Abstract
Background
Prostatic adenocarcinoma is the most frequent malignancy among elderly men after lung cancer, which has the second incidence and the fourth mortality rate in the Iranian population. The primary objective of this study was to investigate how single-nucleotide polymorphisms of the CDH1 gene (rs16260) and DAB2IP (rs1571801) are associated with the risk of prostate cancer through a multi-stage approach.
Results
In the first stage of the study (58 men), we compared the genotype frequency of polymorphisms rs16260 and rs1571801 in the case group to the control group to determine significant polymorphisms (P value < 0.4). No statistically significant difference was shown between the genotype frequency of rs1571801 in the case and control groups. Thus, rs1571801 polymorphism was eliminated at this stage, and only rs16260 polymorphism evaluated in the next stage. In the second stage, statistical analysis showed a significant difference between genotype frequency of rs16260 (P value = 0.037) in all participants. The effect of rs16260 on prostate cancer was not modified by age or PSA levels. Only the Gleason Score = 7 reveals a significant difference between the risk allele (A) and the allele (C) (rs16260).
Conclusions
According to the results of this study, rs16260 is associated with prostate cancer predisposition and might be used as a potential biomarker in prostate cancer. It should be noted that these results need to be confirmed in a larger population.
Similar content being viewed by others
Background
Prostate cancer primarily occurs in older-aged men. This non-cutaneous neoplasm is the most common type of cancer among men after lung cancer in developing countries [1].Recent reports from GLOBOCAN in 2020 indicate that the Age-Standardized Incidence Rate (ASIR) and Age-Standardized Mortality Rate (ASMR) of prostate cancer were 21.3 and 10.0 per 100,000 populations in Iran. Thus, it has the second incidence rate and the fourth mortality rate [2]. There are numerous diagnostic strategies for clinical examination, such as the digital rectal examination (DRE), PSA measurement, and imaging in the form of transrectal ultrasound-guided scan (TRUS) with a minimum of 10 prostate biopsies and multiparametric magnetic resonance imaging scan (mpMRI) [3]. One of the most common diagnostic methods is prostate-specific antigen-based screening which is recommended alongside DRE. Normal level of PSA is between 0 ng/ml and 4 ng/ml but benign prostatic hyperplasia (BPH), prostatitis, ejaculation, and exercise can increase the PSA level [4, 5]. The PSA is expressed in tissues such as the small intestine, normal prostate epithelium, kidney, and salivary organs, although, there is 100-to-1000fold overexpression in Prostate Cancer patients [6]. Epithelium cells of prostatic acini and ducts play a fundamental role in the secretion of PSA which is an organ-specific enzyme [7].
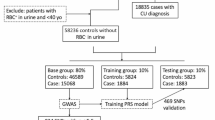
SNPs are among genetic risk factors that occur with a frequency of 1%, which is associated with the susceptibility to prostatic tumorigenesis [8]. One of the most prevalent types of genetic variation for studying genetic differences is SNPs. SNPs are considered as the most useful biomarker for the diagnostic or prognostic of the disease due to their common frequency, low cost genotyping, ease of analysis, and the ability to conduct association studies using statistical and bioinformatics tools [9]. A multi-stage approach is one method for efficient genomic investigations. A smaller number of individuals can be utilized in this method to detect the genotypes of participants. A complete set of SNPs is investigated in a few individuals in the first stage (Participants were chosen from two extremes according to the normal distribution to make the maximum difference) at a liberal P value. SNPs selected in the first phase of investigations are examined in a larger population with a more rigorous P value. Ultimately, only a small number of SNP candidates from the first phase are found to be associated with the relevant feature [10].
E-cadherin, which is composed of 16 coding exons, located on chromosome 16q22.1, is a tumor suppressor gene that encodes an adhesion glycoprotein [11,12,13,14,15]. CDH1 plays a key role in cell polarity, tissue architecture, intercellular adhesion, cell signaling, maintenance of normal tissue morphology, and cellular differentiation [12]. The − 160C/A polymorphism (rs16260) has been identified in the promoter region (the − 160 location) which is linked to the transcriptional start site of E-cadherin. According to studies, the C allele compared with the A allele may increase the level of transcriptional activity between 10 and 68%. Extensive research has proved the mutant allele's affinity for the transcriptional factor is much lower than the wild-type C allele [11]. The results showed that the mutant allele raises the chance of prostate cancer development [16].
DAB2IP gene which is located on chromosome 9q33.1-q33.3, involves in a variety of biological processes such as autophagy, cancer stem cell, epithelial-to-mesenchymal transition (EMT), proliferation and apoptosis [17]. Furthermore, DAB2IP is also implicated in the regulation of Ras-MAPK, ASK-JNK, PI3K-Akt, and nuclear factor-kB (NF-kB) pathways [18]. Decreased DAB2IP expression in prostate epithelial cells is associated with prostate cancer [19]. Rs1571801 has been identified in intron1; 14 kb upstream of exon 2 in the DAB2IP gene is substantially related to an elevated risk of aggressive prostate adenocarcinoma in African American and European populations. Furthermore, numerous researches have revealed the biological role of the DAB2IP gene in aggressive prostate cancer [20]. Epigenetic regulation leads to downregulation of DAB2IP in prostate cancer, which is inversely related to tumor grade and prostate cancer progression [18]. Based on epigenetic or genetic instability observation, the rs1571801 polymorphism may make the DAB2IP gene more susceptible to genetic change or epigenetic regulation in prostate cancer [20].
The current study aimed to evaluate the association between these polymorphisms (rs16260, rs1571801) and prostate cancer susceptibility in the Iranian population using multi-stage approach. The summary of present study has been shown in Fig. 1.
Methods
Study population
For this study, we recruited 127 men with prostate cancer as case and 99 men with BPH as control from the same geographical region. Both groups were referred to Tehran's Hasheminejad Hospital. All the participants in this study have signed a consent form. Each of these two groups was diagnosed with the aid of a specialist doctor and based on PSA levels, digital rectal tests, and prostate biopsies. Patients' clinical information such as age, PSA level, prostate volume, and disease stage was recorded in the checklist. The study was also reviewed by Kharazmi University's ethics committee, and based on the given document, it was approved by the ethics committee with the ID IR.KHU.REC.1400.031. This study was performed in the Laboratory of Molecular Biology and Genetics at Tehran University of Medical Sciences.
Extraction of genomic DNA
EDTA-anticoagulated peripheral blood (3 ml) was collected and stored at − 20 °C. DNA was extracted from blood lymphocytes according to the instruction of the FAVORGENE-Taiwan extraction kit. The quality and quantity of DNA samples were measured after extraction. To determine the quality and quantity of extracted DNA, electrophoresis with 1.5% agarose gel and NanoDrop device were used, respectively. The ratio of 260 to 280 was 1.8. SNP genotyping was done using the Tetra-primer ARMS-PCR technique. Primer1 and the Primer-BLAST-NCBI database were used to design the primers and confirm their correctness, respectively. In this approach, two non-specific external primers and two internal specific primers were used in a reaction to establish the genotype. Allele-specific inner primers differ in the nucleotide sequence at the 3'-end (bold and underlined letters). One is used to identify wild allele, and the other is used to identify mutant allele. Positive control consists of two non-specific external primers (Table 1).
Statistical analysis
Genotype frequency, allele frequency, Hardy–Weinberg equilibrium (HWE), multiplicative, and additive genetic models were evaluated using Chi-squared and Fisher's exact tests with P value < 0.4 in the first stage and P value < 0.05 in the second stage. Odds Ratio (OR) with 95% confidence interval (95%CI) was determined by logistic regression and chi-square test to study the SNPs associated with prostate cancer and Gleason score in the multiplicative and additive models and effect modification. SPSS v.25.0 was used for statistical analysis.
Results
Stage I
Patients characteristics
At this stage, the participants are divided into two groups: the control group, which includes 29 patients with BPH who are the most healthy people, and the case group, which includes 29 prostate adenocarcinoma who are the most unhealthy people. The unhealthiest participants are selected based on Gleason score > 7, positive results of perineural invasion, while the control group (the healthiest) is selected based on PSA < 4. The case group's age range was 55–86 years old, with a mean age of 65.78 ± 9.2, whereas the control group's age range was 47–80 years old, with a mean age of 68.48 ± 9.1.
Statistical analysis
Both polymorphisms with a P value (< 0.4) were analyzed in the first stage. The genotype frequencies of polymorphisms between prostate cancer and the control group are represented in Table 2.
No statistically significant difference was shown between the genotype distribution of rs1571801 in the case and control groups. As estimated by the Chi-square test, case group (P = 0.003) and control group (P = 0.00) for rs1571801 were not in HWE. Thus, the additive genetic model was used to evaluate the association between rs1571801 and prostate cancer. rs1571801 polymorphism was not associated with prostate cancer in the additive genetic model via Fisher's exact test and logistic regression so it was eliminated at this stage (Table 2). Only rs16260 polymorphism is evaluated in the next stage.
Stage II
Patients characteristics
Only the rs16260 polymorphism is evaluated in the second stage. All study participants, including 102 prostate adenocarcinoma and 98 BPH, were evaluated at this stage. The case group's age range was 48–86 years old, with a mean age of 66.26 ± 8.3, the control group's age range was 47–81 years old, with a mean age of 65.32 ± 7.7. The clinical and demographic information of the participants was mentioned in Table 3.
Statistical analysis
At this stage, the statistical analysis was performed for all participants. Significant difference was shown between the genotype frequency of rs16260 in the case and control groups (P = 0.037). Observed and expected frequencies in both case and control groups were examined using Pearson's chi-squared test to evaluate HWE. Case (P value = 0.064) and control (P value = 0.150) groups were in HWE. Therefore, multiplicative and additive genetic models were used to study the association of rs16260 with prostate cancer. Our investigation revealed an association of this polymorphism with prostate adenocarcinoma in the multiplicative genetic model. Furthermore, AC (rs16260) showed an association with prostate cancer in the additive genetic model using CC as a reference genotype, whereas AA (rs16260) did not show an association in this genetic model using CC as a reference genotype (Table 4).
This study investigated the genotype and allele frequency of rs16260, as well as the OR [95%CI] (logistic regression), and P value (Fisher’s exact test) of the risk allele in comparison with the wild allele in three categories of Gleason score. The final results show that there is only a significant difference between the frequency of risk allele (A) and allele (C) in Gleason Score = 7. Besides, no statistically significant difference was revealed between the genotype distribution of rs16260 with the perineural invasion (Table 5).
Effect modification
PSA and age are considered to effect modifications at three levels, there were no differences between the rs16260 polymorphism and prostate cancer at any level (df = 2). Thus, PSA and age were not regarded as effect modifications (Table 6). As a result, the exposure impact (rs16260) is homogeneous across all categories of age and serum PSA level.
Discussion
The most commonly non-cutaneous cancer in men is prostate cancer. After lung cancer in developing countries, this diagnosed non-cutaneous neoplasm is the most prevalent type among men [1]. Recent reports from GLOBOCAN in 2020 indicate that the ASIR and ASMR of prostate cancer were 21.3 and 10.0 per 100,000 populations in Iran [2]. E-cadherin is a tumor suppressor that encodes an adhesion glycoprotein [12, 15]. There is a link between rs16260 in E-cadherin's promoter region (the − 160 position) and the transcriptional start site [11, 13, 15]. Furthermore, multiple investigations have shown that the DAB2IP gene has a biological role in aggressive prostate cancer [20]. Decreased DAB2IP expression in prostate epithelial cells is associated with prostate cancer [19]. In prostate cancer, epigenetic regulation leads to DAB2IP downregulation, which is inversely associated with tumor grade and progression [18]. Rs1571801 has been found in intron 1, 14 kb upstream of exon 2 in the DAB2IP gene is linked to an increased risk of aggressive adenocarcinoma of the prostate in both African American and European populations [20].
In the first stage (59 person) rs1571801 was eliminated since there was no evidence for an association between this polymorphism and prostate cancer in multiplicative and additive genetic models. At this stage, there was a statistically significant difference in the genotype distribution of rs16260 (P = 0.279) in the case and control groups. Consequently, this polymorphism was selected as a candidate SNP for investigations in the second phase. In the second stage, all participants were evaluated to determine the association between rs16260 polymorphism with prostate cancer in both multiplicative and additive genetic models. There is an association between rs16260 in multiplicative genetic model (A vs C) and the additive genetic model with prostate cancer. In Gleason Score = 7, there is a significant difference in the frequency of risk allele (A) and allele (C).
In 2004, the CDH1 (− 160C/A) SNP was shown to be associated with prostate cancer in Swedish men. They identified an association between hereditary prostate cancer and rs16260. As compared to CC genotypes, CA and AA genotypes had a 70% and 150% increased risk of hereditary prostate cancer, respectively. Furthermore, they also discovered evidence that the risk allele did not give an increased risk of sporadic prostate cancer [21].
In 2002, Verhage et al. reported that allele A was associated with a 3.6-fold increased risk of PCa than allele C. Compared to CC genotype, CA genotype of the CDH1 (-160C/A) SNP exhibited an approximately fourfold increased risk of PCa. On the other side, AA genotype was associated with a 1.7-fold increased risk of prostate cancer, which was not statistically significant [22].
Tsukino et al. reported that no statistically significant difference was shown between rs16260 (AA vs CC) (P Value = 0.34) (OR [95%CI] = 1.66 [0.58–4.78]), (CA vs CC) (OR [95%CI] = 1.29 [0.86–1.93]) and prostate cancer, and there is not an association between rs16260 (C vs A) (P Value = 0.17) and prostate cancer [23].
Bo yang et al. reported that The − 160C/A polymorphism has been associated with increased risk of prostate cancer (OR [95%CI] = 1.84 [1.31–2.60] P Value = 0.001 for AA vs CC; OR [95%CI] = 1.18 [1.01–1.38] P Value = 0.04, for CA vs CC; OR [95%CI] = 1.25 [1.07–1.45] P Value = 0.005, in the dominant model AA + CA vs CC; OR [95%CI] = 1.77 [1.27–2.48] P Value = 0.001, and in the recessive model AA vs CC + CA; OR [95% CI] = 1.23 [1.04–1.46] P Value = 0.02 for A vs C) [24].
Pookot et al. investigated the rs16260 in two groups of black men and white men to observe any racial differences and association with prostate cancer. They reported that allele A was associated with a higher relative risk of prostate cancer than allele C in white men (OR [95%CI] = 1.99 [1.29–3.08]). There was no significant association between the allelic frequency of rs16260 and prostate cancer risk in black men (OR [95%CI] = 0.42 [0.22–0.81]). In white men, genotypes AA and CC in comparison with the CC genotype were significantly associated with an increased risk of prostate cancer (OR [95% CI] = 3.04 [1.26–7.32]). In comparison with the CC genotype, the CA and AA genotypes were not associated with an increased risk of prostate cancer in black men (OR [95%CI] = 0.28 [0.12–0.66] for CA vs CC; OR [95%CI] = 0.40 [0.08–2.00] for AA vs CC)) [25].
In 2007, Goto et al. were shown the association of rs16260 and prostate cancer in the Japanese Population. According to their studies, A allele carriers were at higher relative risk for prostate cancer than C only carriers (OR [95%CI] = 1.88 [1.25–2.84] P Value = 0.0023), and in comparison with the CC genotype, the CA and AA genotypes were associated with significantly increased risk of prostate cancer (OR [95%CI] = 9.033 [1.50–172.36] P Value = 0.0434 for AA vs CC; OR [95%CI] = 4.44 [2.82–7.11] P Value < 0.0001 for CA vs CC) [26].
According to research conducted in Bangladesh on CDH1 genetic polymorphisms, there is an association between rs16260 (CA vs CC) (OR [95%CI] = 2.1 [1.1657–3.7830] P Value = 0.0135) and prostate cancer and an association was reported between rs16260 (CA + AA vs CC) (OR [95%CI] = 2.0811 [1.1820–3.6641] P Value = 0.0111) and prostate cancer. No statistically significant difference was shown between rs16260 (AA vs CC) (OR [95%CI] = 1.96 [0.5846–6.5711] P Value = 0.2756) and prostate cancer. In addition, results suggest that there is an association between rs16260 (A vs C) (OR [95%CI] = 1.6901 [1.0740–2.6597] P Value = 0.0233) and prostate cancer [27]. The results of the rs16260 in the present study are consistent with the results of other studies.
Duggan et al. investigated the risk of aggressive prostate cancer in four different groups of people. In comparison with the CC genotype at rs1571801, the CA and AA genotypes exhibited a statistically significant increased risk of aggressive prostate cancer in each of the research groups (OR [95%CI] = 1.50 [1.17–1.93] P Value = 0.0015 in CAPS; OR [95%CI] = 1.29 [1.06–1.57] P Value = 0.0096 in CGEMS; OR [95%CI] = 1.32 [1.07–1.63] P Value = 0.083 in JHH-EA; OR [95%CI] = 1.50 [1.02–2.21] P Value = 0.039 in JHH-AA). In CGEMS samples, they found that the risk allele for rs1571801 was more common in non-aggressive instances than in aggressive ones [19].
Lange et al. found evidence of an association between rs1571801 and the initiation of prostate cancer, but no statistically significant differences between this polymorphism and aggressive adenocarcinoma of the prostate (28). In the present study, rs1571801 does not have an association with prostate cancer that can be because of genetic heterogeneity.
Conclusions
Based on the evidence in this study, we reported that rs16260 is significantly associated with the prostate cancer predisposition, but no statistically significant differences between rs1571801 and adenocarcinoma of the prostate. No association was found between rs16260 and clinical features, although the results indicate that the frequency of the risk allele (A) and allele (C) is significantly different in Gleason Score = 7 (medium-grade-prostate cancer). rs16260 might be used as a potential biomarker in prostate cancer. However, further study in larger populations and in other ethnic groups is required to confirm this study.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASIR:
-
Age-Standardized Incidence Rate
- ASMR:
-
Age-Standardized Mortality Rate
- SCNAs:
-
Somatic copy number alterations
- SNPs:
-
Single nucleotide polymorphisms
- BPH:
-
Benign prostatic hyperplasia
- DRE:
-
Digital rectal examination
- TRUS:
-
Transrectal ultrasound-guided scan
- mpMRI:
-
Multiparametric magnetic resonance imaging scan
- EMT:
-
Epithelial-to-mesenchymal transition
- NF-Kb:
-
Nuclear factor-kB
References
Rawla P (2019) Epidemiology of prostate cancer. World J Oncol 10(2):63
World Health Organization International Agency for Research on Cancer (IARC). GLOBOCAN 2020. Available from: https://gco.iarc.fr/today/data/factsheets/populations/364-iran-islamic-republic-of-fact-sheets.pdf
Nguyen-Nielsen M, Borre M (2016) Diagnostic and therapeutic strategies for prostate cancer. In: Seminars in nuclear medicine, vol 46(6). WB Saunders, pp 484–490
Bernal-Soriano MC, Parker LA, López-Garrigos M, Hernández-Aguado I, Caballero-Romeu JP, Gómez-Pérez L, Alfayate-Guerra R, Pastor-Valero M, García N, Lumbreras B (2019) Factors associated with false negative and false positive results of prostate-specific antigen (PSA) and the impact on patient health: cohort study protocol. Medicine (Baltimore) 98(40):e17451. https://doi.org/10.1097/md.0000000000017451.
Merriel SW, Funston G, Hamilton W (2018) Prostate cancer in primary care. Adv Ther 35(9):1285–1294
Tian JY, Guo FJ, Zheng GY, Ahmad A (2018) Prostate cancer: updates on current strategies for screening, diagnosis and clinical implications of treatment modalities. Carcinogenesis 39(3):307–317
Constantin TV, Mădan VL, Constantin MM, Morariu SH, Braticevici B (2014) The role of prostate-specific antigen in prostate cancer screening. Revista Română de Medicină de Laborator 22(2):275–281
Allemailem KS, Almatroudi A, Alrumaihi F, Almansour NM, Aldakheel FM, Rather RA, Afroze D, Rah B (2021) Single nucleotide polymorphisms (SNPs) in prostate cancer: its implications in diagnostics and therapeutics. Am J Transl Res 13(4):3868
Vallejos-Vidal E, Reyes-Cerpa S, Rivas-Pardo JA, Maisey K, Yáñez JM, Valenzuela H, Cea PA, Castro-Fernandez V, Tort L, Sandino AM, Imarai M (2020) Single-nucleotide polymorphisms (SNP) mining and their effect on the tridimensional protein structure prediction in a set of immunity-related expressed sequence tags (EST) in Atlantic salmon (Salmo salar). Front Genet 27(10):1406
Beikzadeh B, Angaji SA, Abolhasani M (2020) Association study between common variations in some candidate genes and prostate adenocarcinoma predisposition through multi-stage approach in Iranian population. BMC Med Genet 21(1):1
Chang Z, Zhou H, Liu Y (2014) Promoter methylation and polymorphism of E-cadherin gene may confer a risk to prostate cancer: a meta-analysis based on 22 studies. Tumor Biol 35(10):10503–10513
Ma YY, Wu WQ, Liu ZC, Yu XF, Guo K, He QW, Jiang SB, Shao QS, Tao HQ, Huang DS (2016) The CDH1-160C/A polymorphism is associated with breast cancer: evidence from a meta-analysis. World J Surg Oncol 14(1):1–7
Li G, Pan T, Guo D, Li LC (2014) Regulatory variants and disease: the e-cadherin−160C/A SNP as an example. Mol Biol Int 2014:967565. https://doi.org/10.1155/2014/967565
Tan M, Xia S, Zhang Q, Zhu J, Bao E (2013) The-160C> a polymorphism in e-cadherin is associated with the risk of nephrolithiasis. PLoS ONE 8(9):e73109
Qiu LX, Li RT, Zhang JB, Zhong WZ, Bai JL, Liu BR, Zheng MH, Qian XP (2009) The E-cadherin (CDH1) −160 C/A polymorphism and prostate cancer risk: a meta-analysis. Eur J Hum Genet 17(2):244–249
Wang L, Wang G, Lu C, Feng B, Kang J (2012) Contribution of the-160C/A polymorphism in the E-cadherin promoter to cancer risk: a meta-analysis of 47 case-control studies. PLoS ONE 7(7):e40219
Liu L, Xu C, Hsieh JT, Gong J, Xie D (2016) DAB2IP in cancer. Oncotarget 7(4):3766
Wu K, Xie D, Zou Y, Zhang T, Pong RC, Xiao G, Fazli L, Gleave M, He D, Boothman DA, Hsieh JT (2013) The mechanism of DAB2IP in chemoresistance of prostate cancer cells. Clin Cancer Res 19(17):4740–4749
Duggan D, Zheng SL, Knowlton M, Benitez D, Dimitrov L, Wiklund F, Robbins C, Isaacs SD, Cheng Y, Li G, Sun J (2007) Two genome-wide association studies of aggressive prostate cancer implicate putative prostate tumor suppressor gene DAB2IP. J Natl Cancer Inst 99(24):1836–1844
Hsieh JT, Karam JA, Min W (2007) Genetic and biologic evidence that implicates a gene in aggressive prostate cancer. J Natl Cancer Inst 99(24):1823–1824
Jonsson BA, Adami HO, Hägglund M, Bergh A, Göransson I, Stattin P, Wiklund F, Grönberg H (2004) 160C/A polymorphism in the E-cadherin gene promoter and risk of hereditary, familial and sporadic prostate cancer. Int J Cancer 109(3):348–352
Verhage BA, van Houwelingen K, Ruijter TE, Kiemeney LA, Schalken JA (2002) Single-nucleotide polymorphism in the E-cadherin gene promoter modifies the risk of prostate cancer. Int J Cancer 100(6):683–685
Tsukino H, Kuroda Y, Imai H, Nakao H, Qiu D, Komiya Y, Inatomi H, Hamasaki T, Kohshi K, Osada Y, Katoh T (2004) Lack of evidence for the association of E-cadherin gene polymorphism with increased risk or progression of prostate cancer. Urol Int 72(3):203–207
Bo Y, Yi H, Xiaofei W, Hui L, Guoqiang L, Feng L, Weifeng W, Jidong H, Jun O (2015) Effect of E-Cadherin (CDH1)− 160C/A polymorphism on prostate cancer risk: a meta-analysis. bioRxiv 015123. https://doi.org/10.1101/015123
Pookot D, Li LC, Tabatabai ZL, Tanaka Y, Greene KL, Dahiya R (2006) The E-cadherin −160 C/A polymorphism and prostate cancer risk in white and black American men. J Urol 176(2):793–796
Goto T, Nakano M, Ito S, Ehara H, Yamamoto N, Deguchi T (2007) Significance of an E-cadherin gene promoter polymorphism for risk and disease severity of prostate cancer in a Japanese population. Urology 70(1):127–130
Imtiaz H, Afroz S, Hossain MA, Bellah SF, Rahman MM, Kadir MS, Sultana R, Mazid MA, Rahman MM (2019) Genetic polymorphisms in CDH1 and Exo1 genes elevate the prostate cancer risk in Bangladeshi population. Tumor Biol 41(3):1010428319830837
Lange EM, Salinas CA, Zuhlke KA, Ray AM, Wang Y, Lu Y, Ho LA, Luo J, Cooney KA (2012) Early onset prostate cancer has a significant genetic component. Prostate 72(2):147–156
Acknowledgements
Not applicable.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
RA made contribution to conception, DNA extraction, SNP genotyping, scoring, analysis and interpretation of data. ASA and KG made contribution to conception, scoring, analysis and interpretation of data. BB made contribution to conception, analysis and interpretation of data. RR and NB contributed to sampling and medical diagnosis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants were subjected to written consent. The study was approved by Kharazmi University's ethics committee (ID IR.KHU.REC.1400.03).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rahimi, A., Angaji, S.A., Karimi, G. et al. Association study between rs1571801 and rs16260 with prostate adenocarcinoma predisposition in Iranian population. Egypt J Med Hum Genet 24, 33 (2023). https://doi.org/10.1186/s43042-023-00412-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-023-00412-2