Abstract
Background
Tyrosine kinase inhibitors (TKIs) are prescribed as a targeted therapy to treat chronic myeloid leukemia patients. A challenge in clinical practice is that despite excellent efficacy and improved clinical response levels acquired by imatinib, a number of patients receive TKI therapy but have a poor primary response, develop a drug resistance, or relapse after initial success. This inter-individual difference into response has increased the concern in investigating the pharmacogenetics of cancer drugs. This review discusses the influence of various factors, such as BCR-ABL point mutation, efflux and influx transporters, and others, on targeted drug response in CML. Additionally, we focus on how patients can overcome these issues.
Similar content being viewed by others
Background
Chronic myeloid leukemia (CML), as a hematologic malignancy, is a clonal myeloproliferative disorder caused by reciprocal chromosome translocation t(9;22)(q34;q11), well known as the Philadelphia chromosome (Ph+), as the molecular hallmark of CML, leads to forming the breakpoint cluster region and Abelson proto-oncogene1 (BCR-ABL1) fusion gene [1,2,3]. Ph+ chromosome exists within 60–70% of CML patients [4,5,6]. BCR-ABL gene, as an oncogene, can encode the BCR-ABL tyrosine kinase protein. By constitutively activating a tyrosine kinase receptor, it allows ligand-independent stimulation of downstream signaling pathways that affect cell adhesion, DNA repair, survival, and proliferation, which all contribute to leukemia development [7,8,9,10]. Accordingly, an inhibitor of the BCR-ABL such as tyrosine kinase inhibitors (TKIs), should be a selective and effective treatment for CML [11,12,13,14,15]. Despite acceptable results of TKIs in the treatment of CML patients, tyrosine kinase inhibitor (TKI) resistance is the main challenge among these patients [16].
In recent decades, the treatment of cancers with anti-cancer drugs has evolved. Nevertheless, patients treated with identical therapeutic regimens show considerable diversities in drug response and survival results. Therefore, common treatment decision-making strategies that depend solely on the clinical and histopathological factors of disease or environmental agents like age and sex are not completely impressive for every patient [17, 18]. With the advent of human genome sequencing technologies and high-throughput genetic analysis methods, it is undeniable that an individual's genetic structure can influence drug responses, thus increasing attention to carefully examining genetic profiles in the monitoring of cancer patients.
In this study, (1) CML disease and its therapeutic aspects, (2) possible pharmacogenetic markers for predicting the response to TKIs, and (3) strategies to overcome non-response to the treatment of these patients will be discussed. To perform a literature review on chronic myeloid leukemia (CML) and its treatment options, the PubMed and Google Scholar databases were searched using a range of keywords in various combinations. The keywords used include chronic myeloid leukemia, tyrosine kinase inhibitors, imatinib, nilotinib, dasatinib, bosutinib, ponatinib, asciminib, olverembatinib, vodobatinib, treatment failure, BCR-ABL kinase domain mutations, molecular biology, pharmacogenetics, resistance, and personalized medicine. By combining these keywords in different ways, researchers can explore various aspects of CML and its management; these combined keywords include: CML AND tyrosine kinase inhibitors AND treatment failure, BCR-ABL kinase domain mutations AND CML AND personalized medicine, imatinib (other tyrosine kinase inhibitors) AND CML AND pharmacogenetics, imatinib (other tyrosine kinase inhibitors) AND CML AND molecular biology, CML AND imatinib (other tyrosine kinase inhibitors) AND resistance. The search can also focus on emerging therapies such as olverembatinib and vodobatinib, as well as the molecular biology and pharmacogenetics of CML. Other pertinent articles have been chosen amongst the references of retrieved literature.
Chronic myeloid leukemia (CML)
Myeloproliferative disorders refer to a group of hematologic conditions characterized by abnormal growth and proliferation of blood cells. Chronic myeloid leukemia (CML) is one such disorder that results from the malignant transformation of hematopoietic stem cells (HSCs). The occurrence of CML is different depending on the region. It varies from 0.4 per 100,000 persons in some countries to 1.75 per 100,000 in the USA. The incidence relates to age and sex; for instance, CML is a very infrequent disorder among children. In addition, it occurs among men more than women [1, 2]. Furthermore, the median age of people affected is approximately 56 years [3].
Chronic myeloid leukemia is caused by chromosomal translocation of t(9;22), which results in the Ph+ chromosome formation, and BCR-ABL1 gene manufacturing [4]. BCR-ABL plays a critical role in producing the disease by tyrosine kinase activity. During alternative splicing, the BCR-ABL gene is able to produce three types of fusion transcripts with different molecular weights such as P210, P190, and P230 that have constitutively active tyrosine kinase. P210BCR-ABL is more common than the other ones [5]. P210BCR-ABL leads to phosphorylation of various cellular substrates, as a result of activating several downstream signal-transduction cascades such as RAS/MAPK, c-Casitas B lineage lymphoma (c-CBL), PI3- kinase, and Chicken Tumor 10 Regulator of Kinases-like protein (CRKL), Src pathway, and JAK-STAT by p210 BCR-ABL cause the malignant form of the cells. Thereby p210 can control cell differentiation and proliferation [6].
Chronic myeloid leukemia stages divide disease progression into three phases: chronic phase (CP), accelerated phase (AP), and blast phase (BP) [7].
Nearly 90% of patients diagnosed with CML are asymptomatic [8]. Pain or a feeling of fullness below the ribs on the left side can be caused by an enlarged spleen (splenomegaly) [9]. According to the National Comprehensive Cancer Network (NCCN) and European Leukemia Net (ELN) guidelines, the clinical presentation of CML can include the following signs and symptoms: fatigue, weakness, or shortness of breath. These symptoms may be caused by anemia (a low red blood cell count) or by the buildup of abnormal white blood cells in the bone marrow. Unusual bleeding or bruising can be caused by a low platelet count (thrombocytopenia). Rapid weight loss can be caused by the cancer cells taking up space in the bone marrow, making it difficult for normal cells to grow. Recurrent infections can be caused by a low white blood cell count (leukopenia). Skin rashes or itching due to depositing cancer cells in the skin [10,11,12].
Treatment of CML disease
Chronic myeloid leukemia is presented in three phases including: chronic phase (CP), accelerated phase (AP), and blast phase (BP).
CP is the most common and first stage of the disease with a little or no symptoms in the patient but according to studies, the frequency of chronic phase chronic myeloid leukemia (CML) in adults is estimated to be around 85–90% of all cases of CML. In pediatric patients, CML is a rare disease, and the frequency of chronic phase CML is not well established. However, a study published in the journal Cancer in 2020 reports that the incidence of CML in the pediatric population is estimated to be around 1–2% of all childhood leukemias [13,14,15].
Most people in the CP stage respond well to standard treatments such as IMA, nilotinib, dasatinib, or bosutinib [16, 17]. If the patient is resistant to the first line of medication, the dose may be increased, or another TKI may be tried [18]. In the AP, leukemia cells in the body quickly begin to develop symptoms. Also, leukemia cells often acquire new gene mutations that accelerate their growth [19]. Treatment for the AP of CML depends on the medication the patient has already received [20, 21]. If the patient has not received any treatment, the patient will receive TKIs [22]. Most patients respond to IM at this stage, though these responses do not last as long as patients within the CP, so novel drugs such as nilotinib and dasatinib are often used at this stage [23].
In the BP, symptoms and leukemia cells become more abnormal [24]. For patients who have not been previously treated for the blast phase, high-dose IMA may be helpful [25]. Newer TKIs such as bosutinib, nilotinib, and dasatinib show a better effect on BP, and ponatinib may only be used after testing all other TKIs [26].
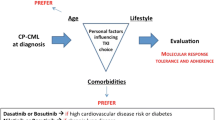
The treatment process in patients depends on their disease phase, their age, other prognostic agents, and the possibility of stem cell donation [27]. Despite the high efficiency of TKIs therapy, patients do not show identical responses to the same treatment [28]. Then, the patient's response to treatment was divided into three categories of optimal response, warning, and failure based on the evaluation of cytogenetic and molecular response [12]. In addition to mutations and overexpressions of BCR-ABL1, inhibition of drug transporter activities, activation of alternative signal pathways, dysfunction of DNA repair and genomic instability, epigenetic abnormalities, persistence of leukemia stem cells (LSCs), and dysfunction of the immune system, drug resistance is a multifactorial process [29, 30].
Tyrosine kinase inhibitors
IMA
imatinib (IMA) (GLEEVEC®) is the most commonly prescribed first-line medication used to treat CML universal [31]. Patients with Ph+CML who have failed interferon-alpha therapy or whose disease has recurred following stem cell transplantation have been included in its indications. For other diseases, the indication of this medicine includes patients with ph+acute lymphoblastic leukemia (ph+ALL), diseases associated with the platelet-derived growth factor receptor (PDGFR) gene rearrangement, aggressive systemic mastocytosis (ASM) without the D816V c-Kit mutation or unknown c-Kit mutation status, chronic eosinophilic leukemia (CEL) who have the FIP1L1-PDGFRα fusion kinase, and HES or CEL who are FIP1L1-PDGFRα fusion kinase negative or unknown, unresectable, recurrent, metastatic dermatofibrosarcoma protuberans (DFSP), and malignant stromal tumors (GIST) [32, 33]. Inhibition of the BCR-ABL protein occurs through binding of IMA to the ATP pocket in the active site, preventing downstream phosphorylation of target proteins [34].
For patients in the chronic phase of CML, the recommended initial dose is 400 mg per day. For patients in the accelerated or blast phase of CML, the recommended initial dose is 600 mg per day. If a patient experiences low levels of white blood cells or platelets, the dose may be held or reduced until the levels return to a safe range. If a patient experiences severe hepatotoxicity or fluid retention, the medication may be held until the issue resolves. Patients with moderate or severe renal impairment should receive a lower dose and should be used with caution [11].
IMA is a highly selective drug against specific molecular targets. IMA, as an inhibitor, can restrain c-KIT, Abl, platelet-derived growth factor receptor (PDGF-R), Abl-related gene (Arg), and finally BCR-ABL activity [31, 35, 36].
An analysis of the outcomes of IMA treatment for chronic myeloid leukemia over a period of 10.9 years showed that 83.3% of patients in the IMA group survived at least 10 years. Most (48.3%) of patients randomly assigned to IMA completed study treatment with IMA, and 82.8% had a complete cytogenetic response. In the first year of treatment, serious adverse events that the investigators considered to be associated with IMA were uncommon [37].
Based on the results of the phase 2 study including patients who were resistant or intolerant to interferon therapy, IMA was the first TKI to receive the approval for the treatment of CML. A complete cytogenetic response (CCyR) rate of 69% was estimated after 12 months of treatment with IM. Patients treated with IMA experienced a better response than those treated with interferon and cytarabine [38, 39]. In the most recent update, an overall survival rate of 83% was estimated at 10 years. Following 5 and 10 years of follow-up, respectively, 31% and 52% of patients assigned to IMA stopped treatment. There were only 4% of patients discontinued treatment due to side effects [40].
Treatment with IMA is mostly well endured with a low occurrence of intense side effects. But, the most common adverse events include mild-to-moderate edema, nausea, muscle cramps, skin rashes, diarrhea, and myelosuppression [41, 42]. There is a possibility of irreversible acute renal injury associated with IM therapy. After discontinuing IMA treatment, the estimated glomerular filtration rate and hemoglobin levels may improve. There has been no report of serious long-term exposure toxicity associated with IMA [43,44,45].
Amplification, or overexpression of BCR-ABL, clonal evolution, and mutations in the P-loop, catalytic domain, and another mutation have been displayed to play a role in primary and secondary resistance against IM, respectively, which will be discussed in the next part. Increased comprehension of the underlying mechanisms of resistance has led to the improvement of novel second-generation TKIs [46].
Nilotinib
Nilotinib (TASIGNA®), as a second-generation TKIs, is designed to dominate the resistance created by IM due to a vast range of mutations (F317L/VLI/C, T315A, and V299L) [33]. Nilotinib compared to IMA: (1) induce faster and deeper molecular responses, (2) the binding site is more lipophilic and therefore has greater potency and selectivity (fits into the ATP-binding site), (3) can bind to the inactive conformation of the ABL kinase domain (KD) [47].
For patients newly diagnosed with the chronic phase of CML, the recommended initial dose is 300 mg twice a day. For patients who are resistant or intolerant to other treatments, the recommended initial dose is 400 mg twice a day. For patients in the blast phase of CML, the recommended initial dose is 400 mg twice a day. If a patient experiences low levels of white blood cells or platelets, the dose may be held or reduced until the levels return to a safe range. If a patient experiences QT interval prolongation, the medication may be held or reduced. If a patient has a history of peripheral arterial occlusive disease or cardiovascular risk factors, nilotinib should be used with caution, and if peripheral arterial occlusive disease is confirmed, nilotinib should be permanently discontinued [11].
In a study, nilotinib was associated with an incidence of 5% for ischemic heart disease, 1.4% for ischemic cerebrovascular disease, and 4.3% for peripheral arterial disease after 6 years, compared with IMA [48].
A study followed patients with newly diagnosed CML in chronic phase for 10 years or more and found that nilotinib had higher rates of molecular response, lower rates of disease progression and CML-related death, and increased eligibility for treatment-free remission (TFR) when compared to IMA [49].
Dasatinib
Dasatinib (SPRYCEL®), as an oral TKIs medicine, shows its benefits in cases where IMA fails because of resistance to specific mutations (Y253H, E255V/K, and F359V/I/C), and it has been reported that dasatinib has more significant activity in inhibiting BCR-ABL than IMA [50, 51]. Also, with a CCyR rate of 98% at 12 months, dasatinib was evaluated as first-line therapy in the treatment of CP CML [52]. Dasatinib can bind to multiple conformations of the ABL kinase and also inhibit PDGFR-A and B, SRC-family kinases (SRC, LCK, YES, FYN) and c-KIT, and ephrin receptor kinase [53].
The initial recommended dose for patients in the chronic phase of CML is 100 mg once daily, while the recommended initial dose for patients in the accelerated or blast phase of CML is 140 mg once daily. National Comprehensive Cancer Network outlines guidelines for adjusting the dose in cases of hematologic and non-hematologic toxicities, as well as rare but serious toxicities such as pulmonary arterial hypertension (PAH). These adjustments include holding or reducing the dose of dasatinib, using growth factors in combination, and using diuretics, supportive care, and steroids to manage fluid retention events and pleural/pericardial effusions. National Comprehensive Cancer Network suggests taking the medication with a meal and large glass of water to prevent gastrointestinal upset and using topical or systemic steroids, dose reduction, dose interruption, or dose discontinuation for rash [11].
Approximately 30% of patients treated with dasatinib develop pleural effusions. In addition, more than 70% of patients experience a recurrence of the pleural effusion once dasatinib is restarted. As a result of dose adjustments based on dasatinib plasma levels, pleural effusion rates can be reduced, while responses are maintained. It is uncommon for dasatinib to cause pulmonary arterial hypertension (PAH), but it may lead to severe and sometimes irreversible complications [42, 54,55,56,57,58].
In a study of patients with chronic CML who had resistance or intolerance to IMA, those who received dasatinib had a high rate of progression-free survival and overall survival. Most adverse events occurred within the first 2 years of treatment, and it was concluded that dasatinib can provide long-term benefits for patients with CML who have resistance or intolerance to IMA [59].
Bosutinib
Bosutinib (Bosulif®) acts as a dual Src and Abl kinases inhibitor. Interestingly, separately lower concentrations of the dual src/abl suppressor are essential to cut BCR-ABL phosphorylation when compared to IMA. Bosutinib has exhibited favorable harboring results in CML patient’ resistance to mutations or intolerance against IMA [60]. In vitro studies showed that bosutinib also repressed 16 of 18 IM-resistant isoforms of BCR-ABL1 kinase [61,62,63,64,65]. The studies found no difference in CCyR between bosutinib and IM even though bosutinib is associated with a higher likelihood of achieving major molecular response (MMR) than IMA [66,67,68,69].
The recommended initial dose for newly diagnosed CML is 400 mg once daily. For CML, AP-CML or BP-CML that has shown resistance or intolerance to prior therapy, the recommended initial dose is 500 mg once daily. Dose adjustments may be made based on hematologic toxicities, such as low levels of white blood cells or platelets. If recovery occurs within 2 weeks, treatment may be resumed at the same dose. If blood counts remain low for more than 2 weeks, the dose may be reduced by 100 mg upon recovery. Doses lower than 300 mg/day have not been evaluated. Non-hematologic toxicities, such as diarrhea or liver transaminase elevation, may also require dose adjustments. Special consideration should be given to patients with preexisting hepatic or renal impairment. If clinically appropriate, bosutinib may be re-escalated to 500 mg once daily [11].
A common side effect of bosutinib is diarrhea. Most of the time, this side effect can be managed by reducing or interrupting the dose [42, 66, 67]. Pleural effusions are generally uncommon in patients who are treated with bosutinib [70]. Long-term exposure to bosutinib has been associated with a decrease in the glomerular filtration rate [71]. A study with the purpose of use of the drug bosutinib in adults with CML who have either been newly diagnosed or have developed resistance or intolerance to other treatments such as IMA followed 284 patients for an average of 5 years and found that at 2 and 5 years, 54% and 40% of patients, respectively, were still receiving treatment with bosutinib. The study found that the drug had a high rate of success in achieving cytogenetic response and complete cytogenetic response and that the majority of adverse events occurred within the first 2 years of treatment. Overall, the study suggests that bosutinib is a viable option for treating CML in patients who have developed resistance or intolerance to other treatments, with durable efficacy and manageable side effects over time [72].
Ponatinib
Ponatinib (ICLUSIG®), as a third-generation kinase inhibitor, is organized to prevail over the T315I mutation. This medicine demonstrated inhibitory operation against native BCR-ABL1 kinase and different ABL1 mutations in different trials. Also, P-loop, β3-, β5- strands and αC- helix are mainly responsible for ponatinib binding [73]. For this reason, ponatinib is recently illustrated for the treatment of CML in each phase of the disease resistant to dasatinib, nilotinib and IMA [74]. More studies have indicated that ponatinib is active on KIT, MEK/ERK kinase 2 (MEKK2), AKT, extracellular signal-regulated kinase (ERK1/2), fibroblast growth factor receptors (FGFRs), rearranged during transfection (RET), and other kinases, and this medicine has been assessed on various cancers in which these kinases play important roles, including ovary, breast, lung, thyroid cancers, neuroblastoma, rhabdoid tumors and in myeloproliferative disorders [75].
The initial recommended dose is 45 mg once daily for patients in the chronic phase of CML and can be reduced to 15 mg once daily upon achieving a certain level of disease response. For patients in the accelerated or blast phase, the recommended initial dose is 45 mg once daily. Dose adjustments are recommended for hematologic and non-hematologic toxicities, such as low blood cell counts or liver enzyme elevations [11].
As a consequence of ponatinib, patients with CP-CML were more likely to experience cardiovascular events, including arterial occlusive events, which were 31% in five years (16% cardiovascular, 13% cerebrovascular, and 14% peripheral arterial vascular events). A reduction in the dose of the drug is recommended for the management of these side effects [76].
Asciminib
Asciminib (SCEMBLIX®) is a selective allosteric inhibitor of BCR-ABL1 that binds to the second myristoyl ABL1 kinase with high intensity, unlike other TKIs [77]. Because the myristoyl domain is not readily found in other kinases, this inhibitor is highly selective for BCR-ABL1. The design logic of asciminib is based on the results obtained in docking, nuclear magnetic resonance (NMR) and crystallographic studies. Among the compounds with specific properties for causing significant curvature at the C-terminus of the second domain, asciminib has been identified [78]. A phase 1a study was conducted with asciminib and nilotinib, dasatinib, or IMA in patients with chronic myeloid leukemia who had become resistant or intolerant to the previous two lines of therapy. Asciminib was combined with nilotinib, IMA or dasatinib in this study to increase the dose of single-agent asciminib. The study included 141 patients with chronic phase CML and nine patients with accelerated phase CML with a mean follow-up of 59 weeks. According to the registration data, 105 patients (70%) had received at least three previous TKIs, mainly IMA (73%), nilotinib (76%) and dasatinib (87%), and 46 patients (31%) had at least one mutation within the BCR-ABL. Following the administration of the drug, 92% of 37 patients without a complete hematologic response achieved one. There was a complete cytogenetic response (CCyR) in 54% of 57 patients without CCyR within 24 weeks. Within six months and twelve months, 37% and 48% of patients achieved MMR, respectively [79]. In a subset of patients with the T315I mutation, those who have been resistant to previous therapies, asciminib, as the first example of an allosteric inhibitor, may offer a promising treatment option as a third-line therapy [80]. Asciminib is a medication that should be taken orally without food. Patients should avoid food 2 h before and 1 h after taking asciminib. The recommended initial dose for CP-CML (previously treated with ≥ 2 TKIs) is 80 mg orally once daily or 40 mg twice daily (at approximately 12-h intervals). For patients with CP-CML with T315I mutation, the recommended initial dose is 200 mg orally twice daily (at approximately 12-h intervals). Dose adjustments should be made for hematologic and non-hematologic toxicities, such as absolute neutrophil count < 1.0 × 109/L, platelets < 50 × 109/L, elevated serum amylase and/or lipase, hypertension, hypersensitivity and cardiovascular toxicity. Drug interactions should be closely monitored with strong CYP3A4 inhibitors, itraconazole oral solution containing hydroxypropyl-β-cyclodextrin, CYP3A4 substrates, CYP2C9 substrates, P-glycoprotein substrates [11].
A study looks at the effectiveness and safety of the drug asciminib in patients with CML who had failed previous treatments. The study included 20 patients with a median age of 60.1 years at the time of diagnosis, and most patients were alive at the time of the survey. The majority of patients had comorbidities, with the most prevalent being cardiovascular, respiratory, and endocrine conditions. The median time from diagnosis to starting asciminib treatment was 9.5 years. Most patients received asciminib as the fourth or fifth line of treatment, and the median BCR-ABL1IS level at the start of treatment was 1.05%. A total of 55% of patients discontinued their previous treatment due to intolerance, 25% due to lack of efficacy, and 25% due to both. Forty-five percentage of patients achieved a MMR at a median duration of 2.2 months. Thirty percentage of patients failed to achieve MMR. Seventy percentage of patients were still receiving asciminib at the time of analysis, for a median duration of 13.4 months. Six patients discontinued treatment for various reasons, including intolerance and disease progression, and one patient required a dose reduction due to side effects [81].
Future TKI drugs
Olverembatinib
As an oral, third-generation BCR-ABL1 TKI, olverembatinib (HQP1341) is being developed to treat CML, ALL, as well as solid tumors including GIST. In addition to inhibiting wild-type and mutant BCR-ABL1 kinases, olverembatinib also inhibits the mutant T315I protein, which confers resistance to all first- and second-generation TKIs. Olverembatinib was approved in China for the treatment of adult patients with CP-CML or AP-CML harboring the T315I mutation in November 2021. In the USA, as of the time this article was written, clinical studies are being conducted on CML and precursor cell ALL, and in China, studies are being conducted on solid tumors, including GIST [68, 82, 83].
Vodobatinib
Vodobatinib is a new drug that is currently being studied in patients with advanced CML who have been intolerant or resistant to some of the TKIs or have other comorbidities that make the use of other TKIs difficult. In vitro studies have demonstrated its efficacy against most BCR-ABL mutations, and it is being investigated as a potential new therapy for CML [68, 84].
How to measure molecular and cytogenetic response
Gold standard method for molecular and cytogenetic response measurement
After talking about the different mechanisms of response to treatment, we answer the question, how to measure the response to treatment?
The monitoring of treatment for chronic myeloid leukemia (CML) is now mainly done using quantitative PCR, which measures the levels of BCR-ABL1. This method is known as the International Scale (IS) [85, 86], and it was found that early response to treatment was an important factor in determining the outcome of treatment. The IS has also defined milestones for deep molecular remission (DMR), with a BCR-ABL1 level of less than 1% being equivalent to complete cytogenetic remission [45, 87, 88]. Cytogenetics is no longer recommended for routine monitoring. It's only used when molecular monitoring is not possible, such as in cases of atypical translocations, atypical transcripts, or additional chromosomal aberrations. If MMR is not reached within 36–48 months, a change in treatment is recommended [12].
It may be necessary to perform molecular testing in patients who fail TKI therapy due to BCR-ABL1 point mutations that disrupt TKI binding. In some cases, hybrid mutations of BCR-ABL1 can be very resistant to first-, second-, and even third-generation TKIs due to their clonal configuration. There is no doubt that Sanger sequencing is the gold standard for screening BCR-ABL1 KD mutants, but it is relatively insensitive [89,90,91,92].
Cytogenetic responses have been evaluated, as accurate and sensitive checking of BCR-ABL1 transcript levels, via RT-qPCR. Estimation of cytogenetic response is usually monitored every three months till MMR is reached and every 3–6 months after that [12]. Fluorescence in situ hybridization (FISH) can be used to evaluate the cytogenetic response in patients as previously described. If the patient responds well to medication and the FISH test is negative at 6 or 12 months of age, or BCR-ABL1 transcripts are less than 1%, the patient is likely to have a complete cytogenetic response (CCyR) [93]. Therefore, the NCCN 2021 guidelines recommend maintaining cytogenetic assessment for diagnosis, failure to achieve response and loss of hematologic or cytogenetic response [94].
Monitoring methods in the future
The gold standard for BCR-ABL1 KD mutant screening is Sanger sequencing, but this technique is relatively weakly sensitive [89,90,91,92]. Considering BCR-ABL1 point mutations, digital PCR (dPCR) are considered alternative method for Sanger sequencing [91]. In a study aimed at quantifying mutations that produce resistance to one or more second-generation TKIs (such as T315I/A, F359V/I/C, V299L, E255K, F317L/V/I/C, E255V, and Y253H), excellent dPCR matching was shown in positive samples for second-generation TKI-resistant mutations. However, next-generation sequencing (NGS) technique stays a better way to diagnose emerging mutations because of its ability to detect the large number of various mutations that can resist to TKIs [95].
A recent study has found that NGS is more effective than traditional methods in detecting these low-level mutations, which can indicate the resistance to TKIs or progression of the disease. Monitoring the kinetics of these mutations through NGS can help identify patients who need to switch to a different TKI or TKI dose and that NGS with a myeloid mutation panel should be considered for patients with no identifiable BCR-ABL1 mutations [96].
The use of machine learning methods to identify the usual types and subtypes of leukemia has been very practical in recent decades. One of the most comprehensive attempts was made ten years ago by using genomic expression profiles to diagnose and classify different types of leukemias by Salah et al. [97]. Artificial intelligence (AI) and machine learning (ML) techniques are also useful for combining large-scale omics information from cancer patients and for exploring gene expression profiles in response to several drugs [98]. In general, this method provides a positive relationship between gene expression and drug activity, allowing the detection of gene purposes for drugs examined. Conversely, a negative correlation between gene expression and measured drug function (e.g., detection of high-level expression of a gene subject to reduced activity of a drug) suggests that like a gene may mediate resistance and hypersensitivity to the drug [99, 100]. Specially, a machine learning model can forecast CML utilization blood cell counts and diagnose CML earlier in the disease course compared to routine medical examinations. The leukemia artificial intelligence (LEAP) program has recently been developed using the decision tree method with extreme gradient boosting (XGBoost) to determinate tree procedure for the optimal therapy advice for TKIs in patients with CP-CML. As a result, the AI method can consistently address the challenges of international data analysis to choose the appropriate TKI with the exact prediction [101, 102].
Mechanisms of drug resistance
The BCR-ABL1 rearrangement in CML patients results in overexpression of ABL1 [103, 104], and the development dependence of CML cells on constitutively activated BCR-ABL tyrosine kinase permits its objecting by TKIs [105]. It is approximated that more than 25% of CML patients will expand resistance to first-line TKI therapy and have to change this, at least once throughout their lifespan [43, 106, 107]. Drug resistance mechanisms in patients as it is shown in Fig. 1 can be divided into two groups: BCR-ABL-independent mechanisms and BCR-ABL-dependent mechanisms [108]. BCR-ABL-dependent mechanisms include mutations of the BCR-ABL kinase domain, mutations outside BCR-ABL kinase domains, compound mutations, amplification or overexpression of BCR-ABL and BCR-ABL-independent mechanisms including activation of alternative pro-survival signaling pathways as a mechanism of resistance, drug influx–efflux activity, clonal evolution, genomic instability, epigenetic modifications, CML stem cells and cytochrome P450 (CYP) isoenzymes polymorphisms [109, 110]. In the following, we are going to explain some of these important mechanisms (Fig. 2).
BCR-ABL-dependent mechanisms, in addition to mutations within the BCR-ABL gene and other proteins, combined mutations, and polymorphisms, overexpression of the BCR-ABL protein, and genomic instability are all contributing factors to this mechanism. Abbreviation SH2, Src homology 2; SH3, Src homology 3; Cap, cysteine-rich secretory proteins; antigen 5; and pathogenesis-related 1 proteins; IRF1, Interferon regulatory factor 1; ALPK2, Alpha Protein Kinase 2; and CYP1B1, cytochrome P450 1B1; ACA, additional chromosomal aberrations; DDR, DNA damage response deregulation
BCR-ABL-dependent mechanisms
Mutations inside the BCR-ABL kinase domain
The successfulness of therapy with TKI is extremely dependent on suitable BCR-ABL1–drug interplay, and one of the most investigated mechanisms is those related to the reactivation of BCR-ABL1 kinase function [30, 111]. Mutations on the fusion gene and overexpression of BCR-ABL1 that interfere with the binding of TKI to targeted kinase may cause resistance [106].
Point mutations within the ABL kinase domain, as the leading cause of TKI resistance, and other domains that control the conformation of this domain prevent the binding of drugs via changing the BCR-ABL confirmation or by preventing the attaching altogether, leading to acquired resistance instead of primary resistance. Mutations can happen at diverse structural subunits of the kinase domain and, based on where mutations happen, are divided into four significant groups, including (1) the P-loop (ATP-binding loop), among 244 and 255 residues; (2) the IMA direct binding site (DBS) between 315 and 317 residues; (3) the C-loop (catalytic domain) between 350 and 363 residues and (4) the A-loop (activation loop) between 381 and 402 residues (Fig. 2). Some other examples of these mutations are listed in Table 1 [94, 106, 112,113,114,115]. The mutations’ manifestation could result from the elective force of preexisting mutant clones, genetic instability derived via BCR-ABL1, and the drug itself, which gently outgrows the drug-sensitive cells [116, 117]. T315I (isoleucine replaces threonine in position 315 of BCR-ABL1), as a gatekeeper mutation, was the first mutation shown in recurred CML patients and reasons the highest level of resistance to all kinds of TKIs and the only TKI approved for clinical use in this situation is ponatinib [118,119,120,121]. Other mutations such as H396P, E255K, F317L, E255V, M351T, Y253F, H396P, and Y253H have also been detected in the ABL kinase domain that conferred different levels of resistance [122,123,124].
Besides T351I, a mutation in the P-loop was the most common case detected within resistant patients [125]. This mutation leads to persuade destabilization of BCR-ABL1 conformation, damaging IMA action also nilotinib function, and association with a further risk of disease progression [125]. Patients with resistance due to mutation in BCR-ABL are identified with the help of Sanger sequencing then therapy is changed [96].
An assessment of the activity of bosutinib, dasatinib and nilotinib against 18 IMA -resistant BCR/ABL mutants was conducted. Based on its results, eight out of 18 mutants showed resistance to bosutinib, ten out of 18 to dasatinib and 13 out of 18 to nilotinib and IMA. In addition to T315I, highly resistant mutants were observed for bosutinib, IMA and nilotinib, whereas dasatinib was highly resistant only to T315I. Despite high resistance to nilotinib in all P-loop mutants, bosutinib and dasatinib showed improved activity patterns, especially in patients who were IMA -resistant. Inactivities were confirmed against the mutation V299L by bosutinib. It is interesting to note that alterations at this position appear to be sensitive to the effects of IMA and nilotinib treatment. The treatment of H396P/R mutations in the activation loop or F359V mutations in the active site is more effective with bosutinib and dasatinib than with nilotinib. However, nilotinib appears to be more effective against F317L than bosutinib or dasatinib. Dasatinib and bosutinib have similar profiles, but are not identical; bosutinib, for instance, has greater activity against Q252H than dasatinib [126].
Mutations outside the BCR-ABL kinase domain
There is a minor and frequent incidence of point mutations outside the kinase domain, but they could have an impact on resistance to TKIs [29]. These domains are included Src homology 2 (SH2), Src homology 3 (SH3), and cysteine-rich secretory proteins, antigen 5, and pathogenesis-related 1 proteins (Cap) domains (Fig. 2). These domains are involved in the auto-inhibition of ABL kinase [127]. Mutations on the SH domain could destroy the BCR-ABL1 structure and therefore disrupt the TKI proficiency [128, 129]. Although mutations in these domains are uncommon, mutations like T212R in the SH2 domain lead to drug resistance [129, 130]. Also, several investigations have announced resistance attainment via malformed splicing of BCR-ABL1; that they are correlated with nucleotides insertion, specifically the maintenance of 35 intronic nucleotides on exon 8–9 of ABL1 [131, 132]. In addition, mutations within and around the myristoylation pocket can cause resistance to asciminib [133,134,135].
Somatic mutations and polymorphisms
In chronic myeloid leukemia, different mutations correlated with response to TKI and/or development to acute phase or blast phase have been described, proposing a role for further mutations in addition to BCR-ABL1 in the progression of CML disorder [136]. It is investigated that within TKI treatment, CML patients gather or lose mutations that impact the patient’s response to TKI [137]. For instance, mutations appeared during the first 6–12 months subsequent to beginning TKI in 37% of CML patients, by good responders having a lower frequency of obtained mutations. Particularly, mutations into TP53 were related to TKI resistance [138]. Also, HLA-E*01:03, interferon regulatory factor 1 (IRF1), alpha protein kinase 2 (ALPK2), and Cytochrome P450 1B1 (CYP1B1) polymorphisms are displayed in CML patients who relapsed [139, 140] (Fig. 2).
Compound mutations
Compound mutations are a common matter within CML treatment, which is the existence of two or more mutations happening in the identical BCR-ABL1 clone [109]. As a result, the interaction among them could lead to resistance [103, 141]. Compound mutations presumably arise sequentially and are different from polyclonal mutations that result from at least two point mutations within the kinase domain of segregate BCR-ABL proteins [142]. Consecutive TKI treatment could be one of the major agents for the continuous enhancement in the occurrence of compound mutations [143].
T315I/E255V or other BCR-ABL1 compound mutations, particularly those including T315I cause resistance to all approved TKIs, including ponatinib [141] (Fig. 2). Some of these compound mutations are shown in Table 1.
Overexpression of BCR-ABL
Gene amplification or upregulation at the transcriptional level is the reason for the BCR-ABL1 overexpression that is only detected in a rare ratio of patients [144, 145]. The expression levels of BCR-ABL1 (both at the mRNA and protein levels) and activity can alter the normal cellular and genetic features and then able to increase disease progression [146, 147].
BCR-ABL1 overexpression causes resistance by escalating the oncoprotein concentration, required to be blocked by TKI [111] (Fig. 2). It is presumed that this overexpression or amplification of BCR-ABL1 leads up to the appearance of point mutations in the kinase domain. For example, CD34-positive CML stem cells that have higher levels of expression of BCR-ABL might show more resistance to IMA and might make more mutations compared with cells expressing BCR-ABL at lower rates [148].
DNA damage repair and genomic instability
Among the factors that have contributed to the evolution of CML, causing TKI resistance and disease transfer from CP-CML to more virulent stages through DNA damage, and genomic instability (such as numerical and structural chromosomal changes and copy number alterations) is DNA damage response deregulation (DDR) [149,150,151]. The patient with CML witnesses genomic instability and DNA damage response (DDR) signaling pathway due to reactive oxygen species (ROS) overproduction, which causes replication pressure and centrosomal dysfunction and eventually prevents apoptosis [147, 151, 152] (Fig. 2). Nevertheless, as well as the DNA lesions, DNA damage repair pathways are activated in Ph-positive cells to reduce DNA damage. These error-prone pathways include alternative non-homologous end joining (NHEJ), single-strand annealing (SSA), and unfaithful homologous recombination repair (HRR) [153,154,155,156,157,158]. In these cells, the generally error-prone HRR promotes point mutations; the NHEJ induces large-scale nucleobase lack, and the vast activity of single-strand annealing (SSA) leads to massive deletions [159]. The mutagenic nucleotide excision repair (NER) is boosted, while the other DNA damage repair pathways are stopped, including mismatch repair and base excision repair (MMR) [160,161,162,163,164,165]. So, as a result, DNA damage repair disturbance in CML directly or indirectly contributes to TKIs resistance and CML progress. Indirect impact mediates genetic instability and the consequent accumulation of point mutations within the ABL1 kinase domain and chromosomal aberrations. In turn, these effects contribute to the prevention of the binding of TKIs, and activation of alternative cellular signaling pathways that also lead to TKI resistance, such as SRC, JAK/STAT, PI3K/AKT and RAS/MAPK pathways [166]. Therefore, upregulation of the NHEJ factors (Poly (ADP-Ribose) Polymerase-1 (PARP1), Werner Syndrome Helicase (WRN), and DNA ligase IIIa), BER genes (methyl-CpG binding domain protein 4 (MBD4) and Nth Like DNA Glycosylase 1 (NTHL1)), DNA damage repair genes (DNA repair protein RAD51 homolog 2 (RAD51L1), Excision repair cross-complementing rodent repair deficiency, complementation group 5 (ERCC5), and Fanconi Anemia complementation group A (FANCA)), and downregulation of the principal NHEJ proteins Artemis and DNA ligase IV can contribute to resistance to treatment with IMA [167,168,169,170,171,172,173]. An example of additional chromosomal abnormalities (ACAs) is 3q26.2 abnormalities that are related to TKI resistance and poor prognosis [174].
BCR-ABL-independent mechanisms
Activation of alternative pro-survival signaling pathways
Survival of CML stem cells does not just rely on BCR-ABL1 function so these cells are not destroyed by TKIs probably because they can also activate some alternative pro-survival signaling pathways, including PI3K/AKT, JAK/STAT, Ras/MAPK, and Src signaling pathways [175, 176]. In these pathways, cells keep on proliferative in spite of effective prevention of the initial oncogenic driver kinase [177]. CML stem cells can also activate autocrine mechanisms to produce mediators like interleukin-3 (IL-3) and granulocyte colony-stimulating factor (G-CSF), and these mediators can act as growth factors for them [178]. The overexpression of Forkhead Box O1 (FOXO1), which is downstream of the PI3K pathway, protein kinase C eta protein (PRKCH), a Protein Kinase C (PKC) and activator of c-RAF (RAF/MEK/ERK) signaling; and Src family kinase (SFK)-LYN also contributes towards BCR-ABL-independent resistance [179,180,181] (Fig. 3).
BCR-ABL-independent mechanisms, a number of mechanisms contribute to this process, such as signaling pathways leading to cell growth, changes in the activity of ABC and other transporters, clonal evolution, polymorphisms of cytochrome p450 isoenzymes, changes in telomere length and telomerase activity, and epigenetic changes. Abbreviations PI3K, phosphoinositide 3-kinase; Akt, protein kinase B, also known as Ak strain transforming (Akt); Ras, rat sarcoma virus; MAPK, mitogen-activated protein kinase; Jak2, janus kinase 2; STAT, signal transducer and activator of transcription; G-CSF, granulocyte colony-stimulating factor; PKC, protein kinase C; SFK, Src family kinase-LYN; IL-3, interleukin 3; CH3 and ME, methyl group; AC, acetyl group FOXO1, forkhead Box O1; PRKCH, protein kinase C eta protein; hOCT1, human organic cation transporter 1; ABC transporters, ATP-binding cassette transporters
Drug influx–efflux activity
Transmembrane transporter proteins through the influx and efflux of the drugs can affect the intracellular concentration of TKIs and the efficiency of BCR-ABL1 inhibition [182, 183]. The expression levels and activity of these transporters are associated with TKIs resistance [184]. Membrane influx pumps, such as human organic cation transporter 1 (hOCT1), and membrane efflux pumps, such as ATP-binding cassette (ABC) transporters, including multidrug-resistant gene product ABC transporter, subfamily B, member 1 (ABCB1) (its other names included P-glycoprotein (P-gp); multidrug resistance protein 1 (MDR1)), the ABC transporter, subfamily G, member 2 (ABCG2) (also known as placenta-specific ABC transporter (ABCP), breast cancer resistance protein (BCRP); mitoxantrone resistance protein (MXR)), and other members of the multiple resistant proteins like ABC transporter, subfamily C (ABCC) (another name contained multidrug resistance-associated protein (MRP)) family, are associated with drug availability in target cells and can act as very potent contributors for resistance to drugs [120, 185, 186]. A number of studies have confirmed increased ABCB1-mediated drug secretion as a feasible mechanism for IMA resistance [28, 187,188,189,190]. Some studies report that ABCB1 can induce resistance to dasatinib rather than nilotinib, while ABCG2 stimulated resistance against both drugs [191]. Eadie et al. [192] demonstrated that nilotinib resistance was only associated with ABCB1 activity and not ABCG2. Despite the fact that nilotinib resistance appears to be related to both ABCB1 and ABCG2 protein expression in diverse studies [193]. Nevertheless, stable clinical links declared between MDR-ABC protein activity and IMA resistance have augmented reports to experiment with the function of frequently inherited variants of ABCG2 and ABCB1 [182] (Fig. 3).
Clonal evolution
BCR-ABL plays an important role in inducing the genomic instability of an amplifying clone [194]. Resistance to TKIs under the pressure of a targeted remedy can be presumed as a dynamic procedure of clonal development and selection of resistant clones [195]. This idea is supported by clinical data, demonstrating that a stop use of TKIs can lead to a significant decrease or even a disappearance of the resistant clone, and the existence of such resistant clones before the start of treatment with TKI may have an impact on the dynamics of the onset of resistance [196, 197]. Clonal evolution is the further mechanism of IMA resistance and is well determined as development after the CP and has been correlated with the obtain of nonrandom chromosomal abnormalities, like additional Ph chromosome, trisomy 8 and chromosome 17 abnormalities, trisomy 19, trisomy 9, point mutations into the coding sequences of RAS, p53, MYC, or rearrangements of retinoblastoma (RB) and p16, within the karyotype of Ph+cells [175, 198] (Fig. 3).
Epigenetic modifications
In hematologic disorders, epigenetic variations such as histone modifications and somatic mutation within regulator genes eventually lead to disease relapse and the enhanced survival of quiescent leukemic stem cells (LSCs) [199, 200]. Overall, it appears that the existence of the BCR–ABL1 oncoprotein is not adequate by itself for CML progression, and the presence of other major modifications, principally epigenetic reprogramming gives rise to malignant LSCs [201, 202]. Also, this factor leads to developing drug resistance [203]. DNA methylation, as the main mechanism for epigenetic control of gene expression, plays an essential role throughout the differentiation of myeloid and lymphoid precursor cells into hematological malignancies [204,205,206]. Indeed, epigenetic patterns define the malignant cell phenotype by affecting the expression of oncogenes and tumor suppressor genes [206, 207]. For example, Hyang-Min Byun and Schoofs et al. show that DNA methylation in CML can arise independently of the genetic background [208, 209]. Changing gene expression profiles caused by epigenetic modifications, such as histone modifications and DNA methylation, can also contribute to the development of drug resistance in CML [210] (Fig. 3).
Cytochrome P450 (CYP) isoenzymes polymorphisms
In the liver, TKIs like IMA are metabolized by cytochrome P450 (CYP) isoenzymes including CYP2D6, CYP3A5, CYP1A2, CYP2C19, CYP1B1, CYP1A1, CYP2C9, and CYP3A4 [211, 212]. The significant IMA metabolite in plasma, CGP74588, is mainly composed of CYP3A4. Studies showed that raised CYP3A activity and generation of the active metabolite CGP74588 is correlated with numerous IMA molecular responses [213] (Fig. 3). Single nucleotide polymorphisms (SNPs) of CYP isoenzymes can result in drug resistance, but no remarkable contribution of CYP3A4/5 variants to TKI efficacy/toxicity has been announced [214].
Telomere length and telomerase activity
Multiple studies have found a correlation between telomere length and response to treatment and progression of the disease in CML patients [215, 216]. In Ph+ peripheral blood leukocytes, telomere length is almost 1 kb shorter than in age-matched controls. Decreased telomere length in CP-CML cells represents that at a specific point in time, BCR-ABL-positive leukemic hematopoietic stem cells underwent more than ten cell divisions compared to their natural polyclonal counterparts (HSC) [217, 218]. Thus, the rate of the telomere shortening during the progression of the disease is 10 to 20 times the rate observed in usual granulocytes [219]. It is also interesting to note that up to a 50-fold increase in telomerase function was detected within more than 50% of patients in the BC phase and was closely related to the attainment of extra cytogenetic aberrations [220] (Fig. 3). Thus, it may be hypothesized that the mechanisms underlying genetic instability in CML, such as aneuploidy, heterozygosity loss and gene amplification, may be immediately due to dysfunctional telomeres and increased telomerase activity [221, 222].
Iwama et al. investigated that within patients treated with interferon-alpha, individuals with lengthy telomeres to therapy beginning experimented with blast crisis remarkably more diminutive than those with shortened telomeres. Also, a considerably higher prevalence of cytogenetic responses and the desired anticipation was reported. It was assumed that expanded telomere length was a demonstrator of an ‘earlier’ phase of CP-CML disease, which returns to preferable response levels [223]. Favored treatment by IMA was discovered to be connected with an expansion in average telomere length [224, 225].
Factors to overcome resistance to treatment
To overcome mutated BCR-ABL1 as a resistance mechanism, second and third generation, TKIs were developed. Nevertheless, even with these new-generation TKIs, some mutations, like T315I, remain resistant to many TKIs [88]. The second generation of TKIs can be connected with decreasing the emergence of BCR-ABL1 mutations [226]. Eide et al. [134] suggested that compound therapy of IMA, especially with asciminib and ponatinib, could be a strategy to manage this type of resistance.
As described in the previous sections, if the patient is resistant to the first generation of TKIs, the second and third generations of this class of medicines will be used [69]. But today, other groups of drugs are used to overcome the resistance of CML; for example, pseudolaric acid B (PAB), as a typical Chinese medicine, through anti-CML activity, is another agent that can control resistance resulting from the mutations BCR-ABL kinase domain [227]. PAB, as a new factor, can obstruct the cell cycle at the G2/M phase and afterward activate the caspase pathway, split the BCR-ABL protein, and impede the BCR-ABL downstream pathways, finally resulting in cell proliferation inhibition, apoptosis, and cytotoxicity [228].
Neferine, as a benzylisoquinoline base alkaloid used in traditional Chinese medicine, is used in compound therapy with IMA for CML patients. This combination therapy can significantly reduce the expression of BCR-ABL protein by inhibiting heat shock protein molecule 90 (Hsp90) expression. As Hsp90 is required for natural BCR-ABL folds, by using Hsp90 inhibitors, such as Neferine, the BCR-ABL and Hsp90 binding is blocked, then BCR-ABL is destroyed by the proteasome pathway, resulting in overcoming the resistance of CML cells with mutations BCR-ABL kinase domain [229,230,231,232]. Asciminib (ABL001), as an allosteric inhibitor, can bind to the myristoylation position and, by conversion the composition of the kinase domain, lead to keeping an inactive form. Asciminib is used to treat TKI resistance due to BCR-ABL mutations and was influential in co-treatment with nilotinib in patients with T315I mutation [109].
ON012380, as a BCR-ABL substrate-binding domain inhibitor, can block ATP-independent cell growth, is the influence in treating T315I mutant cells, and also prevents growth [109].
The fact that epigenetic changes can be pharmacologically manipulated has caused their prosperous use in clinical utilization in many malignancies. Decitabine, as the DNA hypomethylating factor, was tested as the first and second line of thirty percent of CML patients, which elicited a significant number of blood responses but was at the cost of prolonged myeloid suppression. In between IMA-resistant CML patients, Decitabine was examined in composition with further doses of IMA, and 30 to 50% of patients achieved an adequate blood response [233, 234]. Histone deacetylase (HDAC) inhibitors can be used for therapeutic purposes, including benzamides (antinostat), hydroxamate (verostamate), aliphatic acids (phenylbutyrate), electrophilic ketones, and cyclic peptides (romidepsine) [235]. Vorinostat, as a HDAC inhibitor, acts synergistically with TKI to stimulate p21 and p27 expression and restrict BCR-ABL1 levels [236,237,238].
In Chronic myeloid leukemia patients, the upregulation of Programmed death-ligand 1 (PD-L1) is assumed as an immunological runaway process for CML cells. These data recommend that targeting the Programmed cell death protein 1/ programmed cell death ligand 1 (PD-1/PD-L1) pathway may be a successful strategy for eradicating CML cells [84]. Monoclonal antibodies, including pembrolizumab, may interfere with the capacity of cancer cells to grow and extend, and their administration in combination with TKIs may be more effective in treating patients with CML [239].
As well as, co-treatment of arsenic trioxide and interferon (ATO/IFN), as an anti-leukemic, is a factor in overcoming therapeutic resistance via inhibited proliferation of IMA-resistant CML cells and induced apoptosis [240].
Other drugs that have the ability to overcome resistance to treatment with TKIs or alone are mentioned in Table 2.
Importance of personalize medicine in CML
Regardless of improved efficacy and excellent clinical responses got with IMA as a targeted drug, several CML patients taking IMA show an insignificant initial response, progress drug resistance, or undergo recurrence after primary success. These days, resistance to IMA is a challenging issue in clinical practice. There are heterogeneous complex agents for resistance to IMA, including BCR-ABL-independent and BCR-ABL-dependent pathways. Patients remedied with identical therapeutic regimens reveal notable differences in drug response and survival consequences [182, 241]. Hence, conventional treatment option-making strategies that are based only on the clinical and histopathological agents of disease or environmental factors such as sex and age are not entirely impressive for each patient [242, 243]. For this reason, an individual’s genetic structure can influence response to drugs, so creating increased concern in closely exploring genetic profiles within cancer patient meditation. This subject leads to expand investigations focusing on the function of pharmacogenetics in treating cancers [244, 245]. Therefore, by examining SNPs, haplotypes or other heritable mutations, copy number variations (CNVs), and chromosomal alterations through human genome sequencing methods, they have been able to identify genetic factors affecting drug susceptibility and use them to supply prognostic data, predict therapy outcomes, and ameliorate drug impact and safety for specific patients [182, 244, 245].
The earlier sections discussed how pharmacogenetics can predict how well a treatment will work and how well a patient will tolerate it in cases of chronic myeloid leukemia (CML). Different concentrations or types of tyrosine kinase inhibitors (TKIs) can have a big impact on how well the treatment works and how well the patient can tolerate it. The way that TKIs work in the body, as well as genetic variations between individuals, can affect how well the treatment works and if there are any negative side effects. However, the research in this area is limited and conflicting, which makes it difficult to rely on pharmacogenetics. Despite these limitations, the use of TKIs that target BCR-ABL1 has led to better outcomes for CML patients. More research is needed to create personalized treatment plans for CML patients from the moment of diagnosis to the selection of medication.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
References
de la Fuente J, Baruchel A, Biondi A, de Bont E, Dresse M, Suttorp M, et al. International BFMGSGCMLC (2014) Managing children with chronic myeloid leukaemia (CML): recommendations for the management of CML in children and young people up to the age of 18 years. Br J Haematol 167(1):33–47.
Rohrbacher M, Hasford J (2009) Epidemiology of chronic myeloid leukaemia (CML). Best Pract Res Clin Haematol 22(3):295–302
Rohrbacher M, Hasford J (2018) Epidemiology and etiology of chronic myeloid leukemia. In: Wiernik PH, Dutcher JP, Gertz MA (eds) Neoplastic diseases of the blood. Springer, Berlin, pp 9–17
Chereda B, Melo JV (2015) Natural course and biology of CML. Ann Hematol 94(2):107–121
Kuan JW, Su AT, Leong CF, Osato M, Sashida G (2020) Systematic review of normal subjects harbouring BCR-ABL1 fusion gene. Acta Haematol 143(2):96–111
Score J, Calasanz MJ, Ottman O, Pane F, Yeh RF, Sobrinho-Simões MA, Kreil S, Ward D, Hidalgo-Curtis C, Melo JV, Wiemels J (2010) Analysis of genomic breakpoints in p190 and p210 BCR–ABL indicate distinct mechanisms of formation. Leukemia 24(10):1742–1750
Pan S, Chakrabarty SP, Raha S. Progression, detection and remission: evolution of chronic myeloid leukemia using a three-stage probabilistic model. 2022. arXiv:220410504.
Leitner AA, Hochhaus A, Muller MC (2011) Current treatment concepts of CML. Curr Cancer Drug Targets. 11(1):31–43
Ghalesardi OK, Khosravi A, Azizi E, Ahmadi SE, Hajifathali A, Bonakchi H et al (2021) The prognostic importance of BCR-ABL transcripts in chronic myeloid leukemia: a systematic review and meta-analysis. Leuk Res 101:106512
Hehlmann R (2020) The new ELN recommendations for treating CML. J Clin Med. 9(11):3671
https://www.nccn.org/professionals/physician_gls/pdf/cml.pdf.
Hochhaus A, Baccarani M, Silver RT, Schiffer C, Apperley JF, Cervantes F et al (2020) European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia 34(4):966–984
Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M et al (2010) Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 362(24):2260–2270
Hijiya N, Millot F, Suttorp M (2015) Chronic myeloid leukemia in children: clinical findings, management, and unanswered questions. Pediatr Clin 62(1):107–119
Jabbour E, Kantarjian H (2020) Chronic myeloid leukemia: 2020 update on diagnosis, therapy and monitoring. Am J Hematol 95(6):691–709
Jain P, Kantarjian H, Boddu PC, Nogueras-González GM, Verstovsek S, Garcia-Manero G et al (2019) Analysis of cardiovascular and arteriothrombotic adverse events in chronic-phase CML patients after frontline TKIs. Blood Adv 3(6):851–861
Larson RA (2015) Is there a best TKI for chronic phase CML? Blood 126(21):2370–2375
Miller GD, Bruno BJ, Lim CS (2014) Resistant mutations in CML and Ph+ ALL–role of ponatinib. Biol Targets Ther 8:243
O’Dwyer ME, Mauro MJ, Kurilik G, Mori M, Balleisen S, Olson S et al (2002) The impact of clonal evolution on response to imatinib mesylate (STI571) in accelerated phase CML. Blood 100(5):1628–1633
Mukherjee S, Kalaycio M (2016) Accelerated phase CML: outcomes in newly diagnosed vs. progression from chronic phase. Curr Hematol Malig Rep 11(2):86–93
Kantarjian HM, O’Brien S, Cortes JE, Smith TL, Rios MB, Shan J et al (2002) Treatment of Philadelphia chromosome-positive, accelerated-phase chronic myelogenous leukemia with imatinib mesylate. Clin Cancer Res 8(7):2167–2176
Talpaz M, Silver RT, Druker BJ, Goldman JM, Gambacorti-Passerini C, Guilhot F et al (2002) Imatinib induces durable hematologic and cytogenetic responses in patients with accelerated phase chronic myeloid leukemia: results of a phase 2 study. Blood 99(6):1928–1937
Shah NP (2008) Advanced CML: therapeutic options for patients in accelerated and blast phases. J Natl Compr Cancer Netw: JNCCN 6:S31–S36
Assi R, Short N (2020) Blast crisis of chronic myeloid leukemia (CML) a digest for intensivists. In: Nates JL, Price KJ (eds) Oncologic critical care. Springer, Berlin, pp 1135–45
Hehlmann R, Saußele S, Voskanyan A, Silver RT (2016) Management of CML-blast crisis. Best Pract Res Clin Haematol 29(3):295–307
Hehlmann R, Saussele S (2008) Treatment of chronic myeloid leukemia in blast crisis. Haematologica 93(12):1765–1769
Goldman JM (2009) Treatment strategies for CML. Best Pract Res Clin Haematol 22(3):303–313
da Cunha VF, Scheiner MAM, Moellman-Coelho A, Mencalha AL, Renault IZ, Rumjanek VM et al (2016) Low ABCB1 and high OCT1 levels play a favorable role in the molecular response to imatinib in CML patients in the community clinical practice. Leuk Res 51:3–10
Alves R, Gonçalves AC, Rutella S, Almeida AM, De Las RJ, Trougakos IP et al (2021) Resistance to tyrosine kinase inhibitors in chronic myeloid leukemia—from molecular mechanisms to clinical relevance. Cancers 13(19):4820
Apperley JF (2007) Part I: mechanisms of resistance to imatinib in chronic myeloid leukaemia. Lancet Oncol 8(11):1018–1029
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Gattermann N et al (2006) Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med 355(23):2408–2417
Power LA, Coyne JW (2018) ASHP guidelines on handling hazardous drugs. Am J Health Syst Pharm 75(24):1996–2031
Polovich M, Whitford JM, Olsen MM (2014) Chemotherapy and biotherapy guidelines and recommendations for practice. Oncology Nursing Society, Pittsburgh
Iqbal N, Iqbal N (2014) Imatinib: a breakthrough of targeted therapy in cancer. Chemother Res Pract. 2014:1–9
Peng B, Lloyd P, Schran H (2005) Clinical pharmacokinetics of imatinib. Clin Pharmacokinet 44(9):879–894
Capdeville R, Buchdunger E, Zimmermann J, Matter A (2002) Glivec (STI571, imatinib), a rationally developed, targeted anticancer drug. Nat Rev Drug Discov 1(7):493–502
Hochhaus A, Larson RA, Guilhot F, Radich JP, Branford S, Hughes TP et al (2017) Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med 376(10):917–927
Kantarjian H, Sawyers C, Hochhaus A, Guilhot F, Schiffer C, Gambacorti-Passerini C et al (2002) Hematologic and cytogenetic responses to imatinib mesylate in chronic myelogenous leukemia. N Engl J Med 346(9):645–652
Nair P, Wenzel S, Rabe KF, Bourdin A, Lugogo NL, Kuna P et al (2017) Oral glucocorticoid–sparing effect of benralizumab in severe asthma. N Engl J Med 376(25):2448–2458
Gugliotta G, Castagnetti F, Breccia M, Levato L, D’Adda M, Stagno F et al (2015) Long-term outcome of a phase 2 trial with nilotinib 400 mg twice daily in first-line treatment of chronic myeloid leukemia. Haematologica. 100(9):1146
Waller CF (2014) Imatinib mesylate. Recent Results Cancer Res 201:1–25
García-Gutiérrez V, Hernández-Boluda JC (2019) Tyrosine kinase inhibitors available for chronic myeloid leukemia: efficacy and safety. Front Oncol 9:603
Steegmann JL, Baccarani M, Breccia M, Casado L, García-Gutiérrez V, Hochhaus A et al (2016) European LeukemiaNet recommendations for the management and avoidance of adverse events of treatment in chronic myeloid leukaemia. Leukemia 30(8):1648–1671
Sakurai M, Kikuchi T, Karigane D, Kasahara H, Matsuki E, Hashida R et al (2019) Renal dysfunction and anemia associated with long-term imatinib treatment in patients with chronic myelogenous leukemia. Int J Hematol 109(3):292–298
Hochhaus A, Larson RA, Guilhot F, Radich JP, Branford S, Hughes TP et al (2017) Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med 376(10):917–927
Waller CF (2010) Imatinib mesylate. Recent Results Cancer Res 184:3–20
Sacha T, Saglio G (2019) Nilotinib in the treatment of chronic myeloid leukemia. Future Oncol 15(9):953–965
Hochhaus A, Saglio G, Hughes T, Larson R, Kim D, Issaragrisil S et al (2016) Long-term benefits and risks of frontline nilotinib vs imatinib for chronic myeloid leukemia in chronic phase: 5-year update of the randomized ENESTnd trial. Leukemia 30(5):1044–1054
Giles FJ, Abruzzese E, Rosti G, Kim DW, Bhatia R, Bosly A et al (2010) Nilotinib is active in chronic and accelerated phase chronic myeloid leukemia following failure of imatinib and dasatinib therapy. Leukemia 24(7):1299–1301
O’Hare T, Walters DK, Stoffregen EP, Jia T, Manley PW, Mestan J et al (2005) In vitro activity of BCR-ABL inhibitors AMN107 and BMS-354825 against clinically relevant imatinib-resistant Abl kinase domain mutants. Can Res 65(11):4500–4505
Shah NP, Tran C, Lee FY, Chen P, Norris D, Sawyers CL (2004) Overriding imatinib resistance with a novel ABL kinase inhibitor. Science 305(5682):399–401
Cortes JE, Jones D, O’Brien S, Jabbour E, Ravandi F, Koller C et al (2010) Results of dasatinib therapy in patients with early chronic-phase chronic myeloid leukemia. J Clin Oncol 28(3):398
Lindauer M, Hochhaus A (2010) Dasatinib. Recent Results Cancer Res 184:83–102
Vickers NJ (2017) Animal communication: when i’m calling you, will you answer too? Curr Biol 27(14):R713–R715
Hughes TP, Laneuville P, Rousselot P, Snyder DS, Rea D, Shah NP et al (2019) Incidence, outcomes, and risk factors of pleural effusion in patients receiving dasatinib therapy for Philadelphia chromosome-positive leukemia. Haematologica 104(1):93
Rousselot P, Mollica L, Guerci-Bresler A, Nicolini F, Etienne G, Legros L, et al., editors. Dasatinib daily dose optimization based on residual drug levels resulted in reduced risk of pleural effusions and high molecular response rates: final results of the randomized Optim dasatinib trial. Haematologica 99:237–8.
Montani D, Bergot E, Günther S, Savale L, Bergeron A, Bourdin A et al (2012) Pulmonary arterial hypertension in patients treated by dasatinib. Circulation 125(17):2128–2137
Weatherald J, Chaumais M-C, Savale L, Jaïs X, Seferian A, Canuet M et al (2017) Long-term outcomes of dasatinib-induced pulmonary arterial hypertension: a population-based study. European Respiratory Journal. 50(1):1700217
Shah NP, Guilhot F, Cortes JE, Schiffer CA, le Coutre P, Brümmendorf TH et al (2014) Long-term outcome with dasatinib after imatinib failure in chronic-phase chronic myeloid leukemia: follow-up of a phase 3 study. Blood 123(15):2317–2324
Keller G, Schafhausen P, Brümmendorf TH (2010) Bosutinib. Recent Results Cancer Res 184:119–127
Keller-von Amsberg G, Koschmieder S (2013) Profile of bosutinib and its clinical potential in the treatment of chronic myeloid leukemia. Onco Targets Ther 6:99
Puttini M, Coluccia AML, Boschelli F, Cleris L, Marchesi E, Donella-Deana A et al (2006) In vitro and in vivo activity of SKI-606, a novel Src-Abl inhibitor, against imatinib-resistant Bcr-Abl+ neoplastic cells. Can Res 66(23):11314–11322
Rix LR, Rix U, Colinge J, Hantschel O, Bennett K, Stranzl T et al (2009) Global target profile of the kinase inhibitor bosutinib in primary chronic myeloid leukemia cells. Leukemia 23(3):477–485
Golas JM, Arndt K, Etienne C, Lucas J, Nardin D, Gibbons J et al (2003) SKI-606, a 4-anilino-3-quinolinecarbonitrile dual inhibitor of Src and Abl kinases, is a potent antiproliferative agent against chronic myelogenous leukemia cells in culture and causes regression of K562 xenografts in nude mice. Can Res 63(2):375–381
Levinson NM, Boxer SG (2012) Structural and spectroscopic analysis of the kinase inhibitor bosutinib and an isomer of bosutinib binding to the Abl tyrosine kinase domain. PLoS ONE 7(4):e29828
Cortes JE, Kim D-W, Kantarjian HM, Brümmendorf TH, Dyagil I, Griskevicius L et al (2012) Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: results from the BELA trial. J Clin Oncol 30(28):3486
Cortes JE, Gambacorti-Passerini C, Deininger MW, Mauro MJ, Chuah C, Kim D-W et al (2018) Bosutinib versus imatinib for newly diagnosed chronic myeloid leukemia: results from the randomized BFORE trial. J Clin Oncol 36(3):231
Benchikh S, Bousfiha A, El Hamouchi A, Soro SGC, Malki A, Nassereddine S (2022) Chronic myeloid leukemia: cytogenetics and molecular biology’s part in the comprehension and management of the pathology and treatment evolution. Egypt J Med Hum Genet 23(1):1–13
Berman E (2022) How I treat chronic-phase chronic myelogenous leukemia. Blood 139(21):3138–3147
Gjertsen BT, Hochhaus A, Rosti G, Watts JM, Ortí G, le Coutre P et al (2019) Cross-intolerance with bosutinib after prior tyrosine kinase inhibitors in patients with chronic phase chronic myeloid leukemia: BYOND phase 4 study. Blood 134:1639
Cortes JE, Gambacorti-Passerini C, Kim D-W, Kantarjian HM, Lipton JH, Lahoti A et al (2017) Effects of bosutinib treatment on renal function in patients with Philadelphia chromosome-positive leukemias. Clin Lymphoma Myeloma Leuk 17(10):684–95
Gambacorti-Passerini C, Cortes JE, Lipton JH, Kantarjian HM, Kim DW, Schafhausen P et al (2018) Safety and efficacy of second-line bosutinib for chronic phase chronic myeloid leukemia over a five-year period: final results of a phase I/II study. Haematologica 103(8):1298–1307
Tanneeru K, Guruprasad L (2013) Ponatinib is a pan-BCR-ABL kinase inhibitor: MD simulations and SIE study. PLoS ONE 8(11):e78556
Massaro F, Molica M, Breccia M (2018) Ponatinib: a review of efficacy and safety. Curr Cancer Drug Targets 18(9):847–856
Musumeci F, Greco C, Grossi G, Molinari A, Schenone S (2018) Recent studies on ponatinib in cancers other than chronic myeloid leukemia. Cancers 10(11):430
Barbui T, Finazzi G, Falanga A (2013) Myeloproliferative neoplasms and thrombosis. Blood 122(13):2176–2184
Adrián FJ, Ding Q, Sim T, Velentza A, Sloan C, Liu Y et al (2006) Allosteric inhibitors of Bcr-abl–dependent cell proliferation. Nat Chem Biol 2(2):95–102
Jahnke W, Grotzfeld RM, Pelle X, Strauss A, Fendrich G, Cowan-Jacob SW et al (2010) Binding or bending: distinction of allosteric Abl kinase agonists from antagonists by an NMR-based conformational assay. J Am Chem Soc 132(20):7043–7048
Hughes TP, Mauro MJ, Cortes JE, Minami H, Rea D, DeAngelo DJ et al (2019) Asciminib in chronic myeloid leukemia after ABL kinase inhibitor failure. N Engl J Med 381:2315–2326
Breccia M, Colafigli G, Scalzulli E, Martelli M (2021) Asciminib: an investigational agent for the treatment of chronic myeloid leukemia. Expert Opin Investig Drugs 30(8):803–811
Chee LCY, Lee N, Grigg A, Chen M, Schwarer A, Szer J et al (2022) Clinical outcomes of chronic myeloid leukaemia (CML) patients on asciminib through the managed access program (MAP) in Australia. Blood 140(Suppl 1):6800–6802
Cortes JE, Saikia T, Kim D-W, Alvarado Y, Nicolini FE, Khattry N et al (2020) Phase 1 trial of vodobatinib, a novel oral BCR-ABL1 tyrosine kinase inhibitor (TKI): activity in CML chronic phase patients failing TKI therapies including ponatinib. Blood 136:51–52
Dhillon S (2022) Olverembatinib: first approval. Drugs 82(4):469–475
Cortes J, Lang F (2021) Third-line therapy for chronic myeloid leukemia: current status and future directions. J Hematol Oncol 14(1):1–18
Cross N, White H, Müller M, Saglio G, Hochhaus A (2012) Standardized definitions of molecular response in chronic myeloid leukemia. Leukemia 26(10):2172–2175
Cross N, White H, Colomer D, Ehrencrona H, Foroni L, Gottardi E et al (2015) Laboratory recommendations for scoring deep molecular responses following treatment for chronic myeloid leukemia. Leukemia 29(5):999–1003
Baccarani M, Cortes J, Pane F, Niederwieser D, Saglio G, Apperley J et al (2009) Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol 27(35):6041
Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF et al (2013) European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood 122(6):872–884
Soverini S, Bernardi S, Galimberti S (2020) Molecular testing in CML between old and new methods: are we at a turning point? J Clin Med. 9(12):3865
Zabriskie MS, Eide CA, Tantravahi SK, Vellore NA, Estrada J, Nicolini FE et al (2014) BCR-ABL1 compound mutations combining key kinase domain positions confer clinical resistance to ponatinib in Ph chromosome-positive leukemia. Cancer Cell 26(3):428–442
Mughal TI, Psaila B, DeAngelo DJ, Saglio G, Van Etten RA, Radich JP (2021) Interrogating the molecular genetics of chronic myeloproliferative malignancies for personalized management in 2021. Haematologica 106(7):1787–1793
Cumbo C, Anelli L, Specchia G, Albano F (2020) Monitoring of minimal residual disease (MRD) in chronic myeloid leukemia: recent advances. Cancer Manag Res 12:3175–3189
Hehlmann R, Lauseker M, Jung-Munkwitz S, Leitner A, Müller MC, Pletsch N et al (2011) Tolerability-adapted imatinib 800 mg/d versus 400 mg/d versus 400 mg/d plus interferon-a in newly diagnosed chronic myeloid leukemia. J Clin Oncol 29(12):1634–1642
Deininger MW, Shah NP, Altman JK, Berman E, Bhatia R, Bhatnagar B et al (2020) Chronic myeloid leukemia, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 18(10):1385–415
Soverini S, Martelli M, Bavaro L, De Benedittis C, Iurlo A, Galimberti S, et al. Detection of actionable BCR-ABL1 kinase domain (KD) mutations in chronic myeloid leukemia (CML) patients with failure and warning response to tyrosine kinase inhibitors (TKIs): potential impact of next-generation sequencing (NGS) and droplet digital PCR (ddPCR) on clinical decision making. Washington: American Society of Hematology; 2019.
Soverini S, Bavaro L, De Benedittis C, Martelli M, Iurlo A, Orofino N et al (2020) Prospective assessment of NGS-detectable mutations in CML patients with nonoptimal response: the NEXT-in-CML study. Blood 135(8):534–541
Salah HT, Muhsen IN, Salama ME, Owaidah T, Hashmi SK (2019) Machine learning applications in the diagnosis of leukemia: current trends and future directions. Int J Lab Hematol 41(6):717–725
De Las RJ, Alonso-López D, Arroyo MM (2018) Human interactomics: comparative analysis of different protein interaction resources and construction of a cancer protein–drug bipartite network. Adv Protein Chem Struct Biol 111:263–282
Arroyo MM, Berral-González A, Bueno-Fortes S, Alonso-López D, Rivas JDL (2020) Mining drug-target associations in cancer: analysis of gene expression and drug activity correlations. Biomolecules 10(5):667
Lee SI, Celik S, Logsdon BA, Lundberg SM, Martins TJ, Oehler VG et al (2018) A machine learning approach to integrate big data for precision medicine in acute myeloid leukemia. Nat Commun 9(1):42
Hauser RG, Esserman D, Beste LA, Ong SY, Colomb DG Jr, Bhargava A et al (2021) A Machine learning model to successfully predict future diagnosis of chronic myelogenous leukemia with retrospective electronic health records data. Am J Clin Pathol 156(6):1142–1148
Sasaki K, Jabbour EJ, Ravandi F, Konopleva M, Borthakur G, Wierda WG et al (2021) The LEukemia Artificial Intelligence Program (LEAP) in chronic myeloid leukemia in chronic phase: a model to improve patient outcomes. Am J Hematol 96(2):241–250
Radich J (2014) Structure, function, and resistance in chronic myeloid leukemia. Cancer Cell 26(3):305–306
Efficace F, Baccarani M, Breccia M, Alimena G, Rosti G, Cottone F et al (2011) Health-related quality of life in chronic myeloid leukemia patients receiving long-term therapy with imatinib compared with the general population. Blood 118(17):4554–4560
Al-Ali H-K, Heinrich MC, Lange T, Krahl R, Mueller M, Müller C et al (2004) High incidence of BCR-ABL kinase domain mutations and absence of mutations of the PDGFR and KIT activation loops in CML patients with secondary resistance to imatinib. Hematol J 5(1):55–60
Patel AB, O’Hare T, Deininger MW (2017) Mechanisms of resistance to ABL kinase inhibition in chronic myeloid leukemia and the development of next generation ABL kinase inhibitors. Hematol Oncol Clin 31(4):589–612
Melo JV, Barnes DJ (2007) Chronic myeloid leukaemia as a model of disease evolution in human cancer. Nat Rev Cancer 7(6):441–453
Volpe G, Panuzzo C, Ulisciani S, Cilloni D (2009) Imatinib resistance in CML. Cancer Lett 274(1):1–9
Meenakshi Sundaram DN, Jiang X, Brandwein JM, Valencia-Serna J, Remant K, Uludağ H (2019) Current outlook on drug resistance in chronic myeloid leukemia (CML) and potential therapeutic options. Drug Discov Today. 24(7):1355–69
van Erp NP, Gelderblom H, Guchelaar H-J (2009) Clinical pharmacokinetics of tyrosine kinase inhibitors. Cancer Treat Rev 35(8):692–706
Zhao H, Deininger MW (2020) Declaration of Bcr-Abl1 independence. Leukemia 34(11):2827–2836
Soverini S, Colarossi S, Gnani A, Rosti G, Castagnetti F, Poerio A et al (2006) Contribution of ABL kinase domain mutations to imatinib resistance in different subsets of Philadelphia-positive patients: by the GIMEMA Working Party on Chronic Myeloid Leukemia. Clin Cancer Res 12(24):7374–7379
Talati C, Pinilla-Ibarz J (2018) Resistance in chronic myeloid leukemia: definitions and novel therapeutic agents. Curr Opin Hematol 25(2):154–161
Soverini S, Branford S, Nicolini FE, Talpaz M, Deininger MW, Martinelli G et al (2014) Implications of BCR-ABL1 kinase domain-mediated resistance in chronic myeloid leukemia. Leuk Res 38(1):10–20
Kaehler M, Cascorbi I (2021) Pharmacogenomics of impaired tyrosine kinase inhibitor response: lessons learned from chronic myelogenous leukemia. Front Pharmacol 12:1629
Vaidya S, Vundinti BR, Shanmukhaiah C, Chakrabarti P, Ghosh K (2015) Evolution of BCR/ABL gene mutation in CML is time dependent and dependent on the pressure exerted by tyrosine kinase inhibitor. PLoS ONE 10(1):e0114828
Diamond JM, Melo JV (2011) Mechanisms of resistance to BCR–ABL kinase inhibitors. Leuk Lymphoma 52(sup1):12–22
Branford S, Rudzki Z, Walsh S, Parkinson I, Grigg A, Szer J et al (2003) Detection of BCR-ABL mutations in patients with CML treated with imatinib is virtually always accompanied by clinical resistance, and mutations in the ATP phosphate-binding loop (P-loop) are associated with a poor prognosis. Blood 102(1):276–283
Shah NP, Nicoll JM, Nagar B, Gorre ME, Paquette RL, Kuriyan J et al (2002) Multiple BCR-ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia. Cancer Cell 2(2):117–125
An X, Tiwari AK, Sun Y, Ding P-R, Ashby CR Jr, Chen Z-S (2010) BCR-ABL tyrosine kinase inhibitors in the treatment of Philadelphia chromosome positive chronic myeloid leukemia: a review. Leuk Res 34(10):1255–1268
O’Hare T, Shakespeare WC, Zhu X, Eide CA, Rivera VM, Wang F et al (2009) AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell 16(5):401–412
Hochhaus A, Kreil S, Corbin A, La Rosee P, Müller M, Lahaye T et al (2002) Molecular and chromosomal mechanisms of resistance to imatinib (STI571) therapy. Leukemia 16(11):2190–2196
Von Bubnoff N, Schneller F, Peschel C, Duyster J (2002) BCR-ABL gene mutations in relation to clinical resistance of Philadelphia-chromosome-positive leukaemia to STI571: a prospective study. Lancet 359(9305):487–491
Branford S, Rudzki Z, Walsh S, Grigg A, Arthur C, Taylor K et al (2002) High frequency of point mutations clustered within the adenosine triphosphate–binding region of BCR/ABL in patients with chronic myeloid leukemia or Ph-positive acute lymphoblastic leukemia who develop imatinib (STI571) resistance. Blood 99(9):3472–3475
Cang S, Liu D (2008) P-loop mutations and novel therapeutic approaches for imatinib failures in chronic myeloid leukemia. J Hematol Oncol 1(1):1–9
Redaelli S, Piazza R, Rostagno R, Magistroni V, Perini P, Marega M et al (2008) Activity of bosutinib, dasatinib, and nilotinib against 18 imatinib-resistant BCR/ABL mutants. J Clin Oncol 27(3):469–471
Azam M, Latek RR, Daley GQ (2003) Mechanisms of autoinhibition and STI-571/imatinib resistance revealed by mutagenesis of BCR-ABL. Cell 112(6):831–843
Sigl M, Spoerl S, Schnittger S, Meissner J, Rummelt C, Peschel C et al (2013) Imatinib failure and response to dasatinib in a patient with chronic myeloid leukemia in blast crisis and a novel, nine-nucleotide BCR-ABL insertion mutation. Blood Cancer J 3(3):e104-e
Sherbenou DW, Hantschel O, Kaupe I, Willis S, Bumm T, Turaga LP et al (2010) BCR-ABL SH3-SH2 domain mutations in chronic myeloid leukemia patients on imatinib. Blood 116(17):3278–3285
Jabbour EJ, Cortes JE, Kantarjian HM (2013) Resistance to tyrosine kinase inhibition therapy for chronic myelogenous leukemia: a clinical perspective and emerging treatment options. Clin Lymphoma Myeloma Leuk 13(5):515–529
Berman E, Jhanwar S, Hedvat C, Arcila ME, Abdel-Wahab O, Levine R et al (2016) Resistance to imatinib in patients with chronic myelogenous leukemia and the splice variant BCR-ABL135INS. Leuk Res 49:108–112
Marcé S, Cortés M, Zamora L, Cabezón M, Grau J, Millá F et al (2015) A thirty-five nucleotides BCR-ABL1 insertion mutation of controversial significance confers resistance to imatinib in a patient with chronic myeloid leukemia (CML). Exp Mol Pathol 99(1):16–18
Braun TP, Eide CA, Druker BJ (2020) Response and resistance to BCR-ABL1-targeted therapies. Cancer Cell 37(4):530–542
Eide CA, Zabriskie MS, Stevens SLS, Antelope O, Vellore NA, Than H et al (2019) Combining the allosteric inhibitor asciminib with ponatinib suppresses emergence of and restores efficacy against highly resistant BCR-ABL1 mutants. Cancer Cell. 36(4):431–43. E5
Wylie AA, Schoepfer J, Jahnke W, Cowan-Jacob SW, Loo A, Furet P et al (2017) The allosteric inhibitor ABL001 enables dual targeting of BCR–ABL1. Nature 543(7647):733–737
Branford S, Kim DDH, Apperley JF, Eide CA, Mustjoki S, Ong ST et al (2019) Laying the foundation for genomically-based risk assessment in chronic myeloid leukemia. Leukemia 33(8):1835–1850
Fisher K, Wang XQ, Lee A, Morcilla V, de Vries A, Lee E et al (2022) Plasma-derived HIV-1 virions contain considerable levels of defective genomes. J Virol. https://doi.org/10.1128/jvi.02011-21
Stuckey R, López Rodríguez JF, Gómez-Casares MT (2022) Discontinuation of tyrosine kinase inhibitors in patients with chronic myeloid leukemia: a review of the biological factors associated with treatment-free remission. Curr Oncol Rep 24:415–426
Smirnikhina SA, Lavrov AV, Chelysheva EY, Adilgereeva EP, Shukhov OA, Turkina A et al (2016) Whole-exome sequencing reveals potential molecular predictors of relapse after discontinuation of the targeted therapy in chronic myeloid leukemia patients. Leuk Lymphoma 57(7):1669–1676
Vigon L, Luna A, Galan M, Rodriguez-Mora S, Fuertes D, Mateos E et al (2020) Identification of immunological parameters as predictive biomarkers of relapse in patients with chronic myeloid leukemia on treatment-free remission. J Clin Med 10(1):42
Zabriskie MS, Eide CA, Tantravahi SK, Vellore NA, Estrada J, Nicolini FE et al (2014) BCR-ABL1 compound mutations combining key kinase domain positions confer clinical resistance to ponatinib in Ph chromosome-positive leukemia. Cancer Cell 26(3):428–442
Deininger MW, Hodgson JG, Shah NP, Cortes JE, Kim D-W, Nicolini FE et al (2016) Compound mutations in BCR-ABL1 are not major drivers of primary or secondary resistance to ponatinib in CP-CML patients. Blood 127(6):703–712
Kim S-H, Choi SY, Lee S-E, Bang J-H, Byeun J-Y, Park J-E et al (2012) Dynamics and characteristics of BCR-ABL1 multiple mutations in tyrosine kinase inhibitor resistant CML. Blood 120:1677
Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN et al (2001) Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science 293(5531):876–880
Mahon FX, Deininger MW, Schultheis B, Chabrol J, Reiffers J, Goldman JM et al (2000) Selection and characterization of BCR-ABL positive cell lines with differential sensitivity to the tyrosine kinase inhibitor STI571: diverse mechanisms of resistance. Blood 96(3):1070–1079
Gaiger A, Henn T, Horth E, Geissler K, Mitterbauer G, Maier-Dobersberger T et al (1995) Increase of bcr-abl chimeric mRNA expression in tumor cells of patients with chronic myeloid leukemia precedes disease progression. Blood 86:2371–2378
Bavaro L, Martelli M, Cavo M, Soverini S (2019) Mechanisms of disease progression and resistance to tyrosine kinase inhibitor therapy in chronic myeloid leukemia: an update. Int J Mol Sci 20(24):6141
Barnes DJ, Palaiologou D, Panousopoulou E, Schultheis B, Yong AS, Wong A et al (2005) Bcr-Abl expression levels determine the rate of development of resistance to imatinib mesylate in chronic myeloid leukemia. Can Res 65(19):8912–8919
Stetka J, Gursky J, Liñan Velasquez J, Mojzikova R, Vyhlidalova P, Vrablova L et al (2020) Role of DNA damage response in suppressing malignant progression of chronic myeloid leukemia and polycythemia vera: impact of different oncogenes. Cancers 12(4):903
Podszywalow-Bartnicka P, Wolczyk M, Kusio-Kobialka M, Wolanin K, Skowronek K, Nieborowska-Skorska M et al (2014) Downregulation of BRCA1 protein in BCR-ABL1 leukemia cells depends on stress-triggered TIAR-mediated suppression of translation. Cell Cycle 13(23):3727–3741
Popp HD, Kohl V, Naumann N, Flach J, Brendel S, Kleiner H et al (2020) DNA damage and dna damage response in chronic myeloid leukemia. Int J Mol Sci 21(4):1177
Głowacki S, Synowiec E, Szwed M, Toma M, Skorski T, Śliwiński T (2021) Relationship between oxidative stress and imatinib resistance in model chronic myeloid leukemia cells. Biomolecules 11(4):610
Brady N, Gaymes TJ, Cheung M, Mufti GJ, Rassool FV (2003) Increased error-prone NHEJ activity in myeloid leukemias is associated with DNA damage at sites that recruit key nonhomologous end-joining proteins. Can Res 63(8):1798–1805
Cramer K, Nieborowska-Skorska M, Koptyra M, Slupianek A, Penserga ETP, Eaves CJ et al (2008) BCR/ABL and other kinases from chronic myeloproliferative disorders stimulate single-strand annealing, an unfaithful DNA double-strand break repair. Can Res 68(17):6884–6888
Deutsch E, Jarrousse S, Buet D, Dugray A, Bonnet M-L, Vozenin-Brotons M-C et al (2003) Down-regulation of BRCA1 in BCR-ABL–expressing hematopoietic cells. Blood 101(11):4583–4588
Gaymes TJ, Mufti GJ, Rassool FV (2002) Myeloid leukemias have increased activity of the nonhomologous end-joining pathway and concomitant DNA misrepair that is dependent on the Ku70/86 heterodimer. Can Res 62(10):2791–2797
Nowicki MO, Falinski R, Koptyra M, Slupianek A, Stoklosa T, Gloc E et al (2004) BCR/ABL oncogenic kinase promotes unfaithful repair of the reactive oxygen species–dependent DNA double-strand breaks. Blood 104(12):3746–3753
Salles D, Mencalha AL, Ireno IC, Wiesmüller L, Abdelhay E (2011) BCR-ABL stimulates mutagenic homologous DNA double-strand break repair via the DNA-end-processing factor CtIP. Carcinogenesis 32(1):27–34
Skorski T (2012) Genetic mechanisms of chronic myeloid leukemia blastic transformation. Curr Hematol Malig Rep 7(2):87–93
Cramer-Morales K, Nieborowska-Skorska M, Scheibner K, Padget M, Irvine DA, Sliwinski T et al (2013) Personalized synthetic lethality induced by targeting RAD52 in leukemias identified by gene mutation and expression profile. Blood 122(7):1293–1304
Dkhissi F, Aggoune D, Pontis J, Sorel N, Piccirilli N, LeCorf A et al (2015) The downregulation of BAP1 expression by BCR-ABL reduces the stability of BRCA1 in chronic myeloid leukemia. Exp Hematol 43(9):775–780
Piwocka K, Wolanin K, Kusio-Kobialka M, Podszywalow-Bartnicka P (2011) BCR-ABL hits at mitosis; implications for chromosomal instability, aneuploidy and therapeutic strategy. In: Koschmieder S, Krug U (eds) Myeloid leukemia-basic mechanisms of leukemogenesis. IntechOpen, London
Slupianek A, Falinski R, Znojek P, Stoklosa T, Flis S, Doneddu V et al (2013) BCR-ABL1 kinase inhibits uracil DNA glycosylase UNG2 to enhance oxidative DNA damage and stimulate genomic instability. Leukemia 27(3):629–634
Wolanin K, Magalska A, Kusio-Kobialka M, Podszywalow-Bartnicka P, Vejda S, McKenna SL et al (2010) Expression of oncogenic kinase Bcr-Abl impairs mitotic checkpoint and promotes aberrant divisions and resistance to microtubule-targeting agents. Mol Cancer Ther 9(5):1328–1338
Canitrot Y, Falinski R, Louat T, Laurent G, Cazaux C, Hoffmann J-S et al (2003) p210 BCR/ABL kinase regulates nucleotide excision repair (NER) and resistance to UV radiation. Blood 102(7):2632–2637
Yaghmaie M, Yeung C (2019) Molecular mechanisms of resistance to tyrosine kinase inhibitors. Curr Hematol Malig Rep 14(5):395–404
Tobin LA, Robert C, Rapoport AP, Gojo I, Baer MR, Tomkinson AE et al (2013) Targeting abnormal DNA double-strand break repair in tyrosine kinase inhibitor-resistant chronic myeloid leukemias. Oncogene 32(14):1784–1793
Sallmyr A, Fan J, Rassool FV (2008) Genomic instability in myeloid malignancies: increased reactive oxygen species (ROS), DNA double strand breaks (DSBs) and error-prone repair. Cancer Lett 270(1):1–9
Dinis J, Silva V, Gromicho M, Martins C, Laires A, Tavares P et al (2012) DNA damage response in imatinib resistant chronic myeloid leukemia K562 cells. Leuk Lymphoma 53(10):2004–2014
Tipping AJ, Deininger MW, Goldman JM, Melo JV (2003) Comparative gene expression profile of chronic myeloid leukemia cells innately resistant to imatinib mesylate. Exp Hematol 31(11):1073–1080
de Lavallade H, Finetti P, Carbuccia N, Khorashad JS, Charbonnier A, Foroni L et al (2010) A gene expression signature of primary resistance to imatinib in chronic myeloid leukemia. Leuk Res 34(2):254–257
Frank O, Brors B, Fabarius A, Li L, Haak M, Merk S et al (2006) Gene expression signature of primary imatinib-resistant chronic myeloid leukemia patients. Leukemia 20(8):1400–1407
Villuendas R, Steegmann J, Pollan M, Tracey L, Granda A, Fernandez-Ruiz E et al (2006) Identification of genes involved in imatinib resistance in CML: a gene-expression profiling approach. Leukemia 20(6):1047–1054
Wang W, Cortes JE, Lin P, Beaty MW, Ai D, Amin HM et al (2015) Clinical and prognostic significance of 3q26. 2 and other chromosome 3 abnormalities in CML in the era of tyrosine kinase inhibitors. Blood 126(14):1699–706
Picard S, Titier K, Etienne G, Teilhet E, Ducint D, Bernard M-A et al (2007) Trough imatinib plasma levels are associated with both cytogenetic and molecular responses to standard-dose imatinib in chronic myeloid leukemia. Blood 109(8):3496–3499
Yang K, Fu L (2015) Mechanisms of resistance to BCR–ABL TKIs and the therapeutic strategies: a review. Crit Rev Oncol Hematol. 93(3):277–92
Burchert A, Wang Y, Cai D, Von Bubnoff N, Paschka P, Müller-Brüsselbach S et al (2005) Compensatory PI3-kinase/Akt/mTor activation regulates imatinib resistance development. Leukemia 19(10):1774–1782
Jiang X, Lopez A, Holyoake T, Eaves A, Eaves C (1999) Autocrine production and action of IL-3 and granulocyte colony-stimulating factor in chronic myeloid leukemia. Proc Natl Acad Sci 96(22):12804–12809
Wagle M, Eiring A, Wongchenko M, Lu S, Guan Y, Wang Y et al (2016) A role for FOXO1 in BCR–ABL1-independent tyrosine kinase inhibitor resistance in chronic myeloid leukemia. Leukemia 30(7):1493–1501
Wu J, Meng F, Kong L-Y, Peng Z, Ying Y, Bornmann WG et al (2008) Association between imatinib-resistant BCR-ABL mutation-negative leukemia and persistent activation of LYN kinase. J Natl Cancer Inst: JNCI 100(13):926–39
Ma L, Shan Y, Bai R, Xue L, Eide CA, Ou J et al (2014) A therapeutically targetable mechanism of BCR-ABL–independent imatinib resistance in chronic myeloid leukemia. Sci Transl Med. 6(252):252ra121
Nath A, Wang J, Stephanie HR (2017) Pharmacogenetics and pharmacogenomics of targeted therapeutics in chronic myeloid leukemia. Mol Diagn Ther 21(6):621–631
Shugarts S, Benet LZ (2009) The role of transporters in the pharmacokinetics of orally administered drugs. Pharm Res 26(9):2039–2054
Soverini S, Mancini M, Bavaro L, Cavo M, Martinelli G (2018) Chronic myeloid leukemia: the paradigm of targeting oncogenic tyrosine kinase signaling and counteracting resistance for successful cancer therapy. Mol Cancer 17(1):1–15
Pellicano F, Cilloni D, Helgason GV, Messa F, Panuzzo C, Arruga F et al (2009) FOXO transcription factor activity is partially retained in quiescent CML stem cells and induced by tyrosine kinase inhibitors in CML progenitor cells. Blood. https://doi.org/10.1182/blood-2009-06-226621
Gottesman MM (2002) Mechanisms of cancer drug resistance. Annu Rev Med 53(1):615–627
Giles FJ, Kantarjian HM, Cortes J, Thomas DA, Talpaz M, Manshouri T et al (1999) Multidrug resistance protein expression in chronic myeloid leukemia: associations and significance. Cancer Interdiscip Int J Am Cancer Soc. 86(5):805–13
Eadie L, Dang P, Saunders V, Yeung DT, Osborn MP, Grigg AP et al (2017) The clinical significance of ABCB1 overexpression in predicting outcome of CML patients undergoing first-line imatinib treatment. Leukemia 31(1):75–82
Illmer T, Schaich M, Platzbecker U, Freiberg-Richter J, Oelschlägel U, Von Bonin M et al (2004) P-glycoprotein-mediated drug efflux is a resistance mechanism of chronic myelogenous leukemia cells to treatment with imatinib mesylate. Leukemia 18(3):401–408
Bouchet S, Dulucq S, Pasquet J, Lagarde V, Molimard M, Mahon F (2013) From in vitro to in vivo: intracellular determination of imatinib and nilotinib may be related with clinical outcome. Leukemia 27(8):1757–1759
Hegedűs C, Özvegy-Laczka C, Apati A, Magocsi M, Nemet K, Őrfi L et al (2009) Interaction of nilotinib, dasatinib and bosutinib with ABCB1 and ABCG2: implications for altered anti-cancer effects and pharmacological properties. Br J Pharmacol 158(4):1153–1164
Eadie LN, Saunders VA, Hughes TP, White DL (2013) Degree of kinase inhibition achieved in vitro by imatinib and nilotinib is decreased by high levels of ABCB1 but not ABCG2. Leuk Lymphoma 54(3):569–578
Kosztyu P, Bukvova R, Dolezel P, Mlejnek P (2014) Resistance to daunorubicin, imatinib, or nilotinib depends on expression levels of ABCB1 and ABCG2 in human leukemia cells. Chem Biol Interact 219:203–210
Calabretta B, Perrotti D (2004) The biology of CML blast crisis. Blood 103(11):4010–4022
Soverini S, De Benedittis C, Machova Polakova K, Brouckova A, Horner D, Iacono M et al (2013) Unraveling the complexity of tyrosine kinase inhibitor–resistant populations by ultra-deep sequencing of the BCR-ABL kinase domain. Blood 122(9):1634–1648
Hanfstein B, Müller MC, Kreil S, Ernst T, Schenk T, Lorentz C et al (2011) Dynamics of mutant BCR-ABL-positive clones after cessation of tyrosine kinase inhibitor therapy. Haematologica. 96(3):360
Komarova N (2006) Stochastic modeling of drug resistance in cancer. J Theor Biol 239(3):351–366
Danisz K, Blasiak J (2013) Role of anti-apoptotic pathways activated by BCR/ABL in the resistance of chronic myeloid leukemia cells to tyrosine kinase inhibitors. Acta Biochim Pol. 60(4):503–514
Koschmieder S, Vetrie D, editors. Epigenetic dysregulation in chronic myeloid leukaemia: a myriad of mechanisms and therapeutic options. Semin Cancer Biol. 2018;51:180–97
Togasaki E, Takeda J, Yoshida K, Shiozawa Y, Takeuchi M, Oshima M et al (2017) Frequent somatic mutations in epigenetic regulators in newly diagnosed chronic myeloid leukemia. Blood Cancer J. 7(4):e559-e
Meng Z, Li Y-H (2016) One of the mechanisms in blastic transformation of chronic myeloid leukemia: epigenetics abnormality-review. Zhongguo Shi Yan Xue Ye Xue Za Zhi 24(1):250–253
Perrotti D, Jamieson C, Goldman J, Skorski T (2010) Chronic myeloid leukemia: mechanisms of blastic transformation. J Clin Investig 120(7):2254–2264
Azizidoost S, Babashah S, Rahim F, Shahjahani M, Saki N (2014) Bone marrow neoplastic niche in leukemia. Hematology 19(4):232–238
Guillamot M, Cimmino L, Aifantis I (2016) The impact of DNA methylation in hematopoietic malignancies. Trends Cancer 2(2):70–83
Oakes CC, Seifert M, Assenov Y, Gu L, Przekopowitz M, Ruppert AS et al (2016) DNA methylation dynamics during B cell maturation underlie a continuum of disease phenotypes in chronic lymphocytic leukemia. Nat Genet 48(3):253–264
Rosmarin AG, Yang Z, Resendes KK (2005) Transcriptional regulation in myelopoiesis: hematopoietic fate choice, myeloid differentiation, and leukemogenesis. Exp Hematol 33(2):131–143
Baylin SB, Herman JG (2000) DNA hypermethylation in tumorigenesis: epigenetics joins genetics. Trends Genet 16(4):168–174
Byun H-M, Eshaghian S, Douer D, Trent J, Garcia-Manero G, Bhatia R et al (2017) Impact of chromosomal rearrangement upon DNA methylation patterns in leukemia. Open Med 12(1):76–85
Schoofs T, Berdel W, Müller-Tidow C (2014) Origins of aberrant DNA methylation in acute myeloid leukemia. Leukemia 28(1):1–14
Behzad MM, Shahrabi S, Jaseb K, Bertacchini J, Ketabchi N, Saki N (2018) Aberrant DNA methylation in chronic myeloid leukemia: cell fate control, prognosis, and therapeutic response. Biochem Genet 56(3):149–175
Larson RA, Druker BJ, Guilhot F, O’Brien SG, Riviere GJ, Krahnke T et al (2008) Imatinib pharmacokinetics and its correlation with response and safety in chronic-phase chronic myeloid leukemia: a subanalysis of the IRIS study. Blood 111(8):4022–4028
le Coutre P, Kreuzer K-A, Pursche S, v Bonin M, Leopold T, Baskaynak G et al (2004) Pharmacokinetics and cellular uptake of imatinib and its main metabolite CGP74588. Cancer Chemother Pharmacol. 53(4):313–23
Gréen H, Skoglund K, Rommel F, Mirghani RA, Lotfi K (2010) CYP3A activity influences imatinib response in patients with chronic myeloid leukemia: a pilot study on in vivo CYP3A activity. Eur J Clin Pharmacol 66(4):383–386
Jänne PA, Gray N, Settleman J (2009) Factors underlying sensitivity of cancers to small-molecule kinase inhibitors. Nat Rev Drug Discov 8(9):709–723
Estrada N, Xicoy B, García O, Morales-Indiano C, Sagüés M, Boqué C et al (2019) PS1171 telomere length at diagnosis of chronic myeloid leukemia predicts the achievement of deep molecular response to imatinib. HemaSphere 3(S1):532–533
Keller G, Brassat U, Braig M, Heim D, Wege H, Brümmendorf TH (2009) Telomeres and telomerase in chronic myeloid leukaemia: impact for pathogenesis, disease progression and targeted therapy. Hematol Oncol 27(3):123–129
Brümmendorf TH, Holyoake TL, Rufer N, Barnett MJ, Schulzer M, Eaves CJ et al (2000) Prognostic implications of differences in telomere length between normal and malignant cells from patients with chronic myeloid leukemia measured by flow cytometry. Blood 95(6):1883–1890
Drummond MW, Lennard A, Brûmmendorf TH, Holyoake TL (2004) Telomere shortening correlates with prognostic score at diagnosis and proceeds rapidly during progression of chronic myeloid leukemia. Leuk Lymphoma 45(9):1775–1781
Ohyashiki K, Iwama H, Tauchi T, Shimamoto T, Hayashi S, Ando K et al (2000) Telomere dynamics and genetic instability in disease progression of chronic myeloid leukemia. Leuk Lymphoma 40(1–2):49–56
Broccoli D, Young JW, de Lange T (1995) Telomerase activity in normal and malignant hematopoietic cells. Proc Natl Acad Sci 92(20):9082–9086
Ohyashiki JH, Sashida G, Tauchi T, Ohyashiki K (2002) Telomeres and telomerase in hematologic neoplasia. Oncogene 21(4):680–687
Engelhardt M, Mackenzie K, Drullinsky P, Silver RT, Moore MA (2000) Telomerase activity and telomere length in acute and chronic leukemia, pre-and post-ex vivo culture. Can Res 60(3):610–617
Iwama H, Ohyashiki K, Ohyashiki JH, Hayashi S, Kawakubo K, Shay JW et al (1997) The relationship between telomere length and therapy-associated cytogenetic responses in patients with chronic myeloid leukemia. Cancer 79(8):1552–1560
Brümmendorf TH, Ersöz I, Hartmann U, Bartolovic K, Balabanov S, Wahl A et al (2003) Telomere length in peripheral blood granulocytes reflects response to treatment with imatinib in patients with chronic myeloid leukemia. Blood. 101(1):375
Hartmann U, Balabanov S, Ziegler P, Fellenberg J, van der Kuip H, Duyster J et al (2005) Telomere length and telomerase activity in the BCR-ABL-transformed murine Pro-B cell line BaF3 is unaffected by treatment with imatinib. Exp Hematol 33(5):542–549
Hochhaus A, Saglio G, Larson RA, Kim D-W, Etienne G, Rosti G et al (2013) Nilotinib is associated with a reduced incidence of BCR-ABL mutations vs imatinib in patients with newly diagnosed chronic myeloid leukemia in chronic phase. Blood 121(18):3703–3708
Jiang L, Wen C, He Q, Sun Y, Wang J, Lan X et al (2020) Pseudolaric acid B induces mitotic arrest and apoptosis in both imatinib-sensitive and-resistant chronic myeloid leukaemia cells. Eur J Pharmacol 876:173064
Tokarski JS, Newitt JA, Chang CYJ, Cheng JD, Wittekind M, Kiefer SE et al (2006) The structure of dasatinib (BMS-354825) bound to activated ABL kinase domain elucidates its inhibitory activity against imatinib-resistant ABL mutants. Can Res 66(11):5790–5797
An WG, Schulte TW, Neckers LM (2000) The heat shock protein 90 antagonist geldanamycin alters chaperone association with p210bcr-abl and v-src proteins before their degradation by the proteasome. Cell Growth Differ Publ Am Assoc Cancer Res 11(7):355–60
Bhatia S, Diedrich D, Frieg B, Ahlert H, Stein S, Bopp B et al (2018) Targeting HSP90 dimerization via the C terminus is effective in imatinib-resistant CML and lacks the heat shock response. Blood 132(3):307–320
Lu Z, Jin Y, Qiu L, Lai Y, Pan J (2010) Celastrol, a novel HSP90 inhibitor, depletes BCR-ABL and induces apoptosis in imatinib-resistant chronic myelogenous leukemia cells harboring T315I mutation. Cancer Lett 290(2):182–191
Zhang Y, Xiao Y, Dong Q, Ouyang W, Qin Q (2019) Neferine in the lotus plumule potentiates the antitumor effect of imatinib in primary chronic myeloid leukemia cells in vitro. J Food Sci 84(4):904–910
Kantarjian HM, O’Brien S, Cortes J, Giles FJ, Faderl S, Issa JP et al (2003) Results of decitabine (5-aza-2’deoxycytidine) therapy in 130 patients with chronic myelogenous leukemia. Cancer 98(3):522–528
Oki Y, Kantarjian HM, Gharibyan V, Jones D, O’Brien S, Verstovsek S et al (2007) Phase II study of low-dose decitabine in combination with imatinib mesylate in patients with accelerated or myeloid blastic phase of chronic myelogenous leukemia. Cancer 109(5):899–906
Mithraprabhu S, Grigoriadis G, Khong T, Spencer A (2010) Deactylase inhibition in myeloproliferative neoplasms. Investig New Drugs 28(Suppl 1):S50–S57
Di Costanzo A, Del Gaudio N, Migliaccio A, Altucci L (2014) Epigenetic drugs against cancer: an evolving landscape. Arch Toxicol 88(9):1651–1668
Nimmanapalli R, Fuino L, Stobaugh C, Richon V, Bhalla K (2003) Cotreatment with the histone deacetylase inhibitor suberoylanilide hydroxamic acid (SAHA) enhances imatinib-induced apoptosis of Bcr-Abl–positive human acute leukemia cells. Blood 101(8):3236–3239
Fiskus W, Pranpat M, Balasis M, Bali P, Estrella V, Kumaraswamy S et al (2006) Cotreatment with vorinostat (suberoylanilide hydroxamic acid) enhances activity of dasatinib (BMS-354825) against imatinib mesylate–sensitive or imatinib mesylate–resistant chronic myelogenous leukemia cells. Clin Cancer Res 12(19):5869–5878
Hsieh YC, Kirschner K, Copland M (2021) Improving outcomes in chronic myeloid leukemia through harnessing the immunological landscape. Leukemia 35(5):1229–1242
El Eit R, Itani AR, Nassar F, Rasbieh N, Jabbour M, Santina A et al (2019) Antitumor efficacy of arsenic/interferon in preclinical models of chronic myeloid leukemia resistant to tyrosine kinase inhibitors. Cancer 125(16):2818–2828
Ankathil R, Azlan H, Dzarr AA, Baba AA (2018) Pharmacogenetics and the treatment of chronic myeloid leukemia: how relevant clinically? An update. Pharmacogenomics 19(5):475–393
Westbrook K, Stearns V (2013) Pharmacogenomics of breast cancer therapy: an update. Pharmacol Ther 139(1):1–11
Panczyk M (2014) Pharmacogenetics research on chemotherapy resistance in colorectal cancer over the last 20 years. World J Gastroenterol: WJG 20(29):9775
Huang RS, Dolan ME (2010) Approaches to the discovery of pharmacogenomic markers in oncology: 2000–2010–2020. Pharmacogenomics 11(4):471–474
Huang RS, Ratain MJ (2009) Pharmacogenetics and pharmacogenomics of anticancer agents. CA Cancer J Clin 59(1):42–55
Wang Y, Cai D, Brendel C, Barett C, Erben P, Manley PW et al (2007) Adaptive secretion of granulocyte-macrophage colony-stimulating factor (GM-CSF) mediates imatinib and nilotinib resistance in BCR/ABL+ progenitors via JAK-2/STAT-5 pathway activation. Blood 109(5):2147–2155
Gleixner KV, Schneeweiss M, Eisenwort G, Berger D, Herrmann H, Blatt K et al (2017) Combined targeting of STAT3 and STAT5: a novel approach to overcome drug resistance in chronic myeloid leukemia. Haematologica 102(9):1519
Eiring AM, Page BD, Kraft IL, Mason CC, Vellore NA, Resetca D et al (2015) Combined STAT3 and BCR-ABL1 inhibition induces synthetic lethality in therapy-resistant chronic myeloid leukemia. Leukemia 29(3):586–597
Mitchell R, Hopcroft LE, Baquero P, Allan EK, Hewit K, James D et al (2018) Targeting BCR-ABL-independent TKI resistance in chronic myeloid leukemia by mTOR and autophagy inhibition. J Natl Cancer Inst: JNCI 110(5):467–78
Ciarcia R, Damiano S, Montagnaro S, Pagnini U, Ruocco A, Caparrotti G et al (2013) Combined effects of PI3K and SRC kinase inhibitors with imatinib on intracellular calcium levels, autophagy, and apoptosis in CML-PBL cells. Cell Cycle 12(17):2839–2848
Tseng P-H, Lin H-P, Zhu J, Chen K-F, Hade EM, Young DC et al (2005) Synergistic interactions between imatinib mesylate and the novel phosphoinositide-dependent kinase-1 inhibitor OSU-03012 in overcoming imatinib mesylate resistance. Blood 105(10):4021–4027
Chorzalska A, Ahsan N, Rao RSP, Roder K, Yu X, Morgan J et al (2018) Overexpression of Tpl2 is linked to imatinib resistance and activation of MEK-ERK and NF-κB pathways in a model of chronic myeloid leukemia. Mol Oncol 12(5):630–647
Walz C, Sattler M (2006) Novel targeted therapies to overcome imatinib mesylate resistance in chronic myeloid leukemia (CML). Crit Rev Oncol Hematol 57(2):145–164
Yu C, Krystal G, Varticovksi L, McKinstry R, Rahmani M, Dent P et al (2002) Pharmacologic mitogen-activated protein/extracellular signal-regulated kinase kinase/mitogen-activated protein kinase inhibitors interact synergistically with STI571 to induce apoptosis in BCR/ABL-expressing human leukemia cells. Can Res 62(1):188–199
Klejman A, Rushen L, Morrione A, Slupianek A, Skorski T (2002) Phosphatidylinositol-3 kinase inhibitors enhance the anti-leukemia effect of STI571. Oncogene 21(38):5868–5876
Yokota A, Kimura S, Masuda S, Ashihara E, Kuroda J, Sato K et al (2007) INNO-406, a novel BCR-ABL/Lyn dual tyrosine kinase inhibitor, suppresses the growth of Ph+ leukemia cells in the central nervous system, and cyclosporine A augments its in vivo activity. Blood 109(1):306–314
Bixby D, Talpaz M (2009) Mechanisms of resistance to tyrosine kinase inhibitors in chronic myeloid leukemia and recent therapeutic strategies to overcome resistance. ASH Educ Progr Book 2009(1):461–476
Lancet JE, Karp JE (2003) Farnesyltransferase inhibitors in hematologic malignancies: new horizons in therapy. Blood 102(12):3880–3889
Karp JE, editor. Farnesyl protein transferase inhibitors as targeted therapies for hematologic malignancies. Semin Hematol. 2001;38:16–23.
Miyoshi T, Nagai T, Ohmine K, Nakamura M, Kano Y, Muroi K et al (2005) Relative importance of apoptosis and cell cycle blockage in the synergistic effect of combined R115777 and imatinib treatment in BCR/ABL-positive cell lines. Biochem Pharmacol 69(11):1585–1594
Hoover RR, Mahon F-X, Melo JV, Daley GQ (2002) Overcoming STI571 resistance with the farnesyl transferase inhibitor SCH66336. Blood 100(3):1068–1071
Radujkovic A, Schad M, Topaly J, Veldwijk M, Laufs S, Schultheis B et al (2005) Synergistic activity of imatinib and 17-AAG in imatinib-resistant CML cells overexpressing BCR-ABL–Inhibition of P-glycoprotein function by 17-AAG. Leukemia 19(7):1198–1206
Melo JV, Chuah C (2008) Novel agents in CML therapy: tyrosine kinase inhibitors and beyond. ASH Educ Progr Book 2008(1):427–435
Acknowledgements
All those who have collaborated with the authors of this article are greatly appreciated.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EZ did writing-original draft preparation, NN done writing-original draft preparation, SS and HG performed writing—review and editing, AH done visualization, FZ contributed to supervision and validation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zaker, E., Nouri, N., Sorkhizadeh, S. et al. The importance of personalized medicine in chronic myeloid leukemia management: a narrative review. Egypt J Med Hum Genet 24, 31 (2023). https://doi.org/10.1186/s43042-023-00411-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-023-00411-3