Abstract
Background
The irrational use of carbapenems in the last years lead to the emergence of carbapenem-resistant Enterobacteriaceae (CRE). This study aimed at determining the prevalence of CRE intestinal carriage among admitted patients in a tertiary care hospital in Egypt, to characterize carbapenemase-producing genes and to identify possible risk factors of CRE colonization. One hundred rectal swabs were collected from patients within 48 h of hospital admission. Culture was done on chromogenic media and then identification and antibiotic susceptibility testing were done using Vitek 2 compact system. Carbapenemase production was confirmed by Rapidec Carba NP test and by multiplex PCR for blaOXA-48-like, blaNDM-like, blaVIM-like, blaIMP-like and blaKPC-like.
Results
A total number of 36 CRE isolates were recovered from 28 patients. Thus, the prevalence of CRE colonization was 28%. Escherichia coli (83%), followed by Klebsiella pneumoniae (17%) were the main species. History of recent hospitalization and prior antibiotic intake were statistically significant risk factors predisposing to CRE colonization. Rapidec Carba NP gave positive results in 29/36 CRE isolates, whereas seven isolates gave negative results; six of them harbored blaOXA-48-like. Overall, the blaOXA-48-like was detected in 24/36 (66.7%), followed by blaNDM-like in 11/36 (30.6%) and lastly blaVIM-like in 1/36 (2.8%).
Conclusions
Our findings confirm that CRE colonization is disseminating in our healthcare facility, a fact that should be considered as possible pathogens causing infections in high risk patients. Strict infection control measures should be applied to all CRE carriers at hospital admission and a proper antimicrobial stewardship program should be followed in clinical settings.
Similar content being viewed by others
Background
The overuse and misuse of carbapenems in the last years resulted in a selective pressure favoring the transfer of resistance genes from chromosomes to plasmids with subsequent dissemination of plasmids between strains, and dissemination of resistant strains between patients leading to the emergence and abrupt spread carbapenem-resistant Enterobacteriaceae (CRE) [1].
Carbapenemase production is the most common mechanism of resistance to carbapenems, which is frequently accompanied by co-existence of other resistance genes to other classes of antibiotics, e.g., aminoglycosides or quinolones [2].
Carbapenemases identified in Enterobacteriaceae belong to three classes of β-lactamases: The Ambler class A, B and D β-lactamases. Klebsiella pneumoniae carbapenemases “KPC”s, are the most clinically common enzymes in Group A [3], Group D includes the oxacillinases (OXA-48-like), whereas the metallo-β-lactamases (Group B) include imipenemase metallo-β-lactamases “IMP”, Verona integron-encoded metallo-β-lactamases “VIM” and New Delhi metallo-β-lactamase “NDM” [4].
The Middle East has been recognized lately as a common reservoir area for NDM-1 [5]. A high prevalence and dissemination of class D carbapenemases was also reported in the Mediterranean countries [6]. Risk factors for carbapenemase producing Enterobacteriaceae (CPE) acquisition include chronic diseases, comorbidities, repeated hospital admissions, or stay in an intensive care unit and prior antimicrobial use [7].
CRE colonization may represent a potential threat to patients as bloodstream invasion through the damaged mucosa may result during severe mucositis in CRE colonized personnel leading to secondary bacteraemia. Moreover, digestive carriers of CRE may represent silent shedders resulting in further dissemination of carbapenemase-producing genes. Therefore, preventing the spread of CRE infection could rely on the accurate detection of both infected patients and colonized carriers [4, 7].
The current study aimed to determine the prevalence of CRE intestinal carriage among admitted patients at Theodor Bilharz Research Institute (TBRI) hospital, a tertiary care hospital, in Giza, Egypt, to characterize carbapenemase-producing genes and to identify possible risk factors of CRE colonization.
Methods
The current study is observational cross-sectional analytic in which rectal swabs were collected from 100 inpatients on the first 48 h of their hospital admission to TBRI hospital in the period from April 2017 to January 2018. Clinical data were recorded including sex, age, departments, duration of hospitalization, presence of chronic diseases or co-morbidities, as well as prior hospital admission through the previous year and prior antibiotic intake through the previous month before admission. A signed informed consent was obtained from each patient contributing in the study.
All rectal swabs were plated directly onto CHROM ID CARBA SMART agar (BioMérieux, France) that enables the selective growth of KPC and MBL CPE on the CARB medium side and OXA-48 CPE on the other OXA side. The cultured plates were then incubated aerobically at 37° for 18–24 h. Recovered colonies were interpreted according to manufacturer’s instructions. Isolates were subcultured on Muller Hinton agar (MHA) for further identification and antibiotic susceptibility testing (AST) using Vitek 2 compact system (BioMérieux, France). AST report included the following antibiotics: carbapenems “ertapenem (ETP), meropenem (MEM) and imipenem(IPM)”, ampicillin (AMP), ampicillin/sulbactam (SAM), cefazolin (CFZ), ceftriaxone (CRO), cefepime (FEP), aztreonam (ATM), amikacin (AK), gentamicin (CN), tobramycin (TOB), ciprofloxacin (CIP), moxifloxacin (MOX), tigecycline (TGC), nitrofurantoin (FT) and trimethoprim/sulfamethoxazole (SXT). Minimum inhibitory concentration (MIC) values were interpreted according to the Clinical Laboratory Standards Institute (CLSI) guidelines. Carbapenem non-susceptible (including resistant and intermediate) isolates (showing MICs; ERT ≥ 1, IPM ≥ 2, MEM ≥ 2) were further confirmed [8]. Epidemiological cut-off points “ECOFFs” released by the European Committee on Antimicrobial Susceptibility Testing were also used as screening cut-off values for carbapenemase producers (MICs; ERT > 0.12, IPM > 1, MEM > 0.12) [9]. Tigecycline and moxifloxacin were interpreted according to EUCAST guidelines [10].
Phenotypic detection of CPE was done by Rapidec Carba NP test (BioMérieux, France). Molecular detection of carbapenemase-producing genes was done using multiplex polymerase chain reaction (PCR) [11]. DNA extraction was done by boiling method. Two multiplex reactions were performed; one for the detection of blaKPC-like, blaOXA-like, and blaNDM-like, and the other for the detection of blaVIM-like and blaIMP-like. PCR cycling conditions included initial denaturation at 94 °C for 10 min, followed by 34 cycles of amplification (94 °C for 30 s, 52 °C for 40 s and 72 °C for 50 s) and lastly a final extension step at 72 °C for 5 min. Detection of amplified PCR products was done on 2% agarose gel electrophoresis.
Results
Study patients included thirty-nine (39%) females and sixty-one (61%) males. Their mean age was 55.7 ± 14.3 years. A total number of 36 CPE isolates were detected on CHROM ID CARBA SMART agar from a total number of 28 patients (28/100; 28%) as eight CPE isolates (8/100; 8%) had both CARB and OXA CPE isolates. Rectal swabs were obtained from different hospital departments; Hepatogastroenterology (HGE) (47%), Intensive Care Units; ICUs (29%) and Urology Department (24%). Most CPE isolates were retrieved from the Urology Department (11/24; 45.8%) with a statistically significant difference (P value 0.035) as shown in Table 1.
Positive swabs cultures on CHROM ID CARBA SMART agar belonged to 15/28 males (53.6%) and 13/28 females (46.4%) with no statistically significant difference (P value 0.342). However, a statistically significant difference was found in patients who were previously hospitalized within the previous 12 months (P value 0.004), as well as in patients who had previous antibiotic intake within the previous month (P value 0.026).
Regarding the presence of co-morbidities, including diabetes mellitus, hypertension, hepatic diseases (hepatitis C virus, cirrhosis or hepatocellular carcinoma), kidney diseases (chronic kidney disease or end stage renal disease), asthmatic bronchitis and neurogenic bladder, no statistically significant difference was found between patients with and without any of those chronic diseases (P value 0.622).
Vitek2 system identification showed that E. coli was the major species identified (30/36; 83%), followed by K. pneumoniae (6/36; 17%). AST interpretation according to CLSI guidelines revealed that 35/36 (97.2%) isolates were resistant to ertapenem, whereas only one isolate (2.8%) was sensitive. Moreover, 29/36 (80.6%) isolates were non-susceptible to imipenem “25 resistant and 4 intermediate” and 7/36 isolates (19.4%) were sensitive. As for meropenem, 28/36 (77.8%) isolates were non–susceptible “27 resistant isolates and only one intermediate isolate” and 8/36 isolates (22.2%) were sensitive [8]. Comparing MIC values of the three carbapenems to the detected carbapenemase-producing genes revealed that all isolates harboring genes showed resistance to at least one carbapenem except for one E. coli isolate that was sensitive to all three carbapenems. This E. coli isolate harbored blaOXA-48.
However, upon applying the ECOFFs screening cut-off values, ertapenem and meropenem MIC values interpretation changed from being sensitive to be “a possible carbapenemase producer”. Also applying ECOFFs breakpoints on all recovered isolates was more sensitive to detect all carbapenemase producers with ertapenem and meropenem (Table 2) [9]
Susceptibility patterns to other antibiotics showed statistically significant difference (P value 0.001) where the highest sensitivity was to tigecycline (83.3%) followed by amikacin and nitrofurantoin. Quinolones, sulphonamides, cephalosporins and aztreonam showed very low patterns of sensitivity while all isolates showed complete resistance to other β-lactams (Table 3).
Rapidec Carba NP gave positive results in only 29 isolates. Seven isolates gave negative results; six of them harbored blaOXA-48-like by multiplex PCR while the seventh isolate was negative by PCR tests.
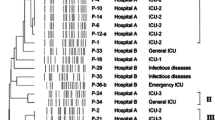
Overall, the blaOXA-48-like was detected in 24/36 (66.7%), followed by blaNDM-like in 11/36 (30.6%) and lastly blaVIM-like in 1/36 (2.8%). All CRE isolates were negative for blaIMP-like or blaKPC-like genes. (Fig. 1 and Table 4).
Multiplex PCR results on agarose gel electrophoresis for blaNDM, blaOXA and blaKPC. A 100 bp DNA ladder. B, C and O: E. coli isolates used as positive controls for blaNDM-like (621 bp), blaOXA-48-like (438 bp) and blaKPC-like (798 bp), respectively. D Negative control. E, G, I and J Isolates positive to blaOXA-48-like. K and L Isolates positive to blaNDM-like. H, M and N Isolates positive to both blaNDM-like and blaOXA-48-like. F An isolate showing a negative PCR result for all tested genes. The left arrow indicates the fragment of molecular size 500 bp
In E. coli, the blaOXA-48-like was mainly detected in 21/30 (70%), followed by blaNDM-like in 7/30 (23.3%), whereas in K. pneumoniae, blaNDM-like was found in 4/6 (66.7%) followed by blaOXA-48-like in 3/6 (50%). Six isolates out of 36 (16.7%) CRE (four E. coli and two K. pneumoniae) harbored two genes (blaNDM-like and blaOXA-48-like) while only one E. coli isolate, 1/36 (2.8%) harbored (blaOXA-48-like and blaVIM-like). Moreover, seven CRE isolates, 7/36 (19.4%) were negative to the five tested genes.
By comparing PCR results to that of Rapidec Carba NP, one isolate was negative by both methods, six isolates were negative by PCR only and another six were negative by Rapidec Carba NP only (Table 4).
Statistical analysis
The data were coded and entered using the statistical package SPSS version 21. The data were summarized using descriptive statistics; number and percentage for qualitative variables, mean and standard deviation for normally distributed quantitative variables. Statistical differences between groups were tested using Chi-Square test for qualitative variables’ comparisons and Independent-Samples T test for quantitative variables which are normally distributed. P values less than or equal to 0.05 were considered statistically significant.
Discussion
The prevalence of carbapenem resistance is increasing indicating a very alarming situation. Eight years ago the emergence of CRE in clinical isolates was reported in two intensive care unit patients in a cancer hospital in Cairo in Egypt [12]. Since then, the frequency increased within few years reaching 62.7% (47/75) in Tanta University Hospitals [13]. More recently, a survey for hospital acquired infections (HAIs) that included 310 ICUs in 72 hospitals across 25 governorates in Egypt showed that 64% of the hospitals had at least one CRE isolate and 47.9% of Enterobacteriaceae isolates were CRE. This rate is higher than estimates reported from other Arab, African or Asian countries. The incidence of CRE HAI was estimated as (3.7/10,000 patient days) which is also much higher than the overall incidence of all CRE (HAI and non-HAI) reported from other countries all over the world; United States (0.1–0.4/10,000 patient-days), Canada (0.2 per 10,000 patient-days) and China (0.4 per 10,000 patient-days) [14].
CRE carriers in rectal swab samples are recognized as a high risk group, as they can spread CRE by intimate contact and via travel [15]. Furthermore, a 6.5% risk of infection with CRE amongst colonized patients has been documented [7]. Therefore, it becomes essential to identify CRE carriers in hospital settings because identifying asymptomatic colonizers and applying contact isolation precautions is mandatory to reduce transmission and to improve patient outcome [16]
The aim of the current study was to determine the frequency of CRE intestinal colonization in patients upon admission to TBRI hospital, assess the genotypic diversity of CPE and to determine the main risk factors related to intestinal colonization with CRE.
Twenty-eight of screened patients gave positive rectal swabs culture on chromogenic agar “CARBA SMART” media yielding 36 CRE isolates. Thus, the prevalence of colonization by CRE was 28%. Studies assessing CRE colonization in Egypt are limited; however, the result of the current study is comparable to a recently published one that was carried in a paediatric ICU in Cairo that showed a prevalence rate of 24% [17]. This was also in agreement with a previous Brazilian study showing a prevalence rate of 30.4% [18]. Higher rate of CRE colonization (52%) was reported among patients admitted to Vietnamese hospitals [19]. On the contrary, this figure was relatively higher than that reported in a rehabilitation Italian hospital (10.2%) and much higher than that reported from outpatient children in Shanghai (3.6%) [15, 20].
Also this was higher than figures obtained from patients in ICUs of two hospitals in Kuwait; 7.8% (25 / 320) at Adan Hospital, and 12.2% (33/270) at Mubarak Al Kabeer Hospital [21].
In a recently published review, Egypt showed the highest prevalence of CRE (28% of 796 isolates) compared to other African countries including Algeria, Libya, Morocco, Mauritania and Tunisia showing a prevalence rate of 2% or less [22]. This high level of resistance in the current study can be attributed to the massive abuse of antibiotics in Egypt [23].
In the current study and following CLSI breakpoints revealed that all the studied isolates harboring carbapenemase-producing genes showed resistance to at least one carbapenem with best sensitivity to ertapenem (97.2%) [8]. However, upon applying the “ECOFFs” screening cut-off values to the three carbapenems, a more sensitive result was obtained covering 100% of CRE with ertapenem and meropenem [9]. This is of much importance to healthcare facilities where screening for CRE to apply prompt infection control contact precautions is of tremendous priority. Moreover, it is worth mentioning that the recent document released by EUCAST in 2017 recommended the use of ertapenem and meropenem to screen for CRE and not imipenem that matches with the finding in this study [24].
The Rapidec Carba NP test is a reliable confirmation tool of CPE isolates, especially NDM producers, with lower sensitivity (as it gave negative results with six OXA-48-like producers) which could be attributed to their weak hydrolytic carbapenemase activity. These findings agree with another study which revealed lower sensitivity with class D Ambler carbapenemase producers [25].
The detection of CPE by Rapidec Carba NP test in six isolates, which were negative by PCR of the tested carbapenem resistance genes, suggested the possibility of the presence of other mechanisms of resistance other than carbapenemase production such as porin loss or over production of ESBLs or of AmpCs. As we tested the main five resistance genes (KPC, NDM, VIM, IMP and OXA-48 genes) only, other uncommon untested resistance genes such as GES, NMC-A, SME, SCF-1, IMI-1 and IMI-2 genes may be involved in resistance to carbapenems.
Understanding factors that predispose to colonization of patients with CRE may help clinicians prevent transmission as well as reduce morbidity and mortality. Previous studies reported that exposure to hospital setting or/and antimicrobial agents might increase the risk of colonization and it would be easier to acquire CRE isolates [15]. In the current study, colonized and non-colonized patients did not significantly differ with respect to gender and associated comorbidities. However, patients colonized with CRE were significantly more likely than non-colonized patients to have a history of recent hospitalization within the previous 12 months, as well as having previous antibiotic intake within the previous month. This also confirms what has been reported lately that among colonized patients, ICU stay is one of the most important patient-related conditions associated with a significant risk of CRE infections, whereas prolonged exposure to broad spectrum antibiotics was among the main modifiable variables involved [7].
The variation in the study population and the epidemiological differences in various geographic regions was reflected in species distribution of CRE as in the present study, E. coli was the major species identified (83%), followed by K. pneumoniae (17%). This was similar to Perry et al. [26] who stated that E. coli was the major species found (47%) among faecal carriers of Enterobacteriaceae with blaNDM-1 at military hospitals in Pakistan. Opposite finding was reported in a Brazilian study where Klebsiella was the sole species identified, and in another study in USA where the majority of recovered isolates were K. pneumoniae (92%) [18, 27]. Other parts of the world showed also different results, where in Taiwan, K. pneumoniae (53.8%) was the main species followed by E. cloacae (30.8%) and lastly E. coli (14.1%) [28].
Although blaNDM is known to be endemic in the Middle East [5] in this study it was the second most common detected gene. While blaOXA-48-like was the main carbapenemase-producing gene (66.7%), mainly in E. coli (70%), blaNDM-like was the following gene (30.6%), mainly in K. pneumoniae (66.7%). Only 2.7% of the isolates harbored blaVIM-like. Similar findings were reported in a recent Egyptian study where blaOXA-48 showed dominance (33%) followed by blaNDM (27%) in CRE isolates from colonized pediatrics age group in ICU. However, both genes were detected mainly in Klebsiella pneumoniae isolates [17]. This finding could be different from the clinical situation in Egypt and in other parts of the world where carbapenem resistance is detected at higher frequencies in K. pneumoniae than in E. coli. In a more recent study, the most common pathogen for CRE cases of HAIs in Egypt was Klebsiella (85.1%), followed by E. coli (10.2%) [14]. Moreover, in a review that compares all multidrug resistant bacteria from different Arab countries, CRE was found in Egypt, as with other countries, more in Klebsiella than in E. coli isolates (40% vs 5%) [22]. Lately our team in TBRI also identified blaNDM as the main carbapenem resistance gene in K. pneumoniae clinical isolates [5]. The blaNDM is known to be endemic in our region with the first report in Cairo in Egypt being reported in 2013 from a K. pneumoniae isolate [12]. Later, it has been described repeatedly from various geographical areas in Egypt [5, 29]. Another Egyptian study reported blaOXA-48 as the dominant carbapenem resistance gene in K. pneumoniae clinical isolates (40.6%) and blaNDM-5 (9.6%) in E. coli [30].
Co-production of OXA-48-like and other carbapenemases (NDM, VIM) leads to the emergence of multidrug resistant strains. In this study, six isolates out of 36 (four E. coli and two K. pneumoniae) harbored two genes (blaNDM-like and blaOXA-48-like) while only one E. coli isolate harbored (blaOXA-48-like and blaVIM-like) genes. Similar co-production of genes was reported previously in several parts of the world [31, 32].
Early detection of CRE colonization allows for early and rapid setting of contact precautions to prevent CRE transmission to other patients. CRE carriage is an important risk factor to be detected rapidly, as this may permit early implementation of appropriate antimicrobial therapy, which is the strongest modifiable predictor for mortality in severe sepsis in CRE infections [16, 21]. Recent report from southeastern Brazil and Vietnam confirmed the importance of active CRE surveillance protocol as subsequent infection with CRE is frequent in hospitalized patients colonized with CRE isolates. However, its effective implementation depends on the appropriate preventive measures and feedback among its team members [19, 33]. Although the current study only enrolled 100 patients, yet we find this significant figure of colonization among the studied subjects is an important threat to public health and should be reported. Further studies including more patients from multiple centers should be considered in the future.
Current treatment options for CRE infections are very limited, as they are resistant to all β-lactam antibiotics as reported in the current study and as previously detected [34]. The highest in vitro sensitivity was shown to glycylclines (tigecycline) in this study followed by aminoglycosides (mainly amikacin and gentamicin) and nitrofurans (nitrofurantoin) which may represent possible treatment options.
Conclusions
Our findings confirm that CRE colonization is disseminating in our healthcare setting. So CRE should be considered clinically as possible pathogens causing infections in high risk patients, especially if proved to be simultaneously colonized by CRE. Applying the ECOFFs screening cut-off is more sensitive to detect all CRE isolates than CLSI. The variation in genes and in species between clinical and colonized isolates may indicate the propensity of CRE strains to acquire genetic materials with rapid spread and inter-species dissemination through horizontal gene transfer. Therefore, strict infection control measures should be followed with all CRE carriers at hospital admission. Rational use of carbapenems should be enforced through national regulations to contain the spread of these superbugs pathogens.
Availability of data and materials
Not applicable.
Abbreviations
- AK:
-
Amikacin
- AMP:
-
Ampicillin
- AST:
-
Antibiotic susceptibility testing
- ATM:
-
Aztreonam
- CFZ:
-
Cefazolin
- CIP:
-
Ciprofloxacin
- CLSI:
-
Clinical Laboratory Standards Institute
- CN:
-
Gentamicin
- CPE:
-
Carbapenemase-producing Enterobacteriaceae
- CRE:
-
Carbapenem-Resistant Enterobacteriaceae
- CRO:
-
Cetriaxone
- Ecoffs:
-
Epidemiological Cut-off points
- ETP:
-
Ertapenem
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- FEP:
-
Cefepime
- FT:
-
Nitrofurantoin
- HAI:
-
Hospital Acquired infections
- ICU:
-
Intensive Care unit
- IMP:
-
Imipenem
- IMP:
-
Imipenemase Metallo-β-Lactamase
- KPC:
-
Klebsiella pneumoniae carbapenemase
- MBL:
-
Metallo-β-lactamase
- MDX:
-
Moxifloxacin
- MEM:
-
Meropenem
- MHA:
-
Mueller Hinton Agar
- MIC:
-
Minimum inhibitory concentration
- NDM:
-
New Delhi Metallo-β-Lactamase
- OXA-48:
-
Oxacillinase
- PCR:
-
Polymerase Chain Reaction
- Sam:
-
Ampicillin/Sulbactam
- SXT:
-
Trimethoprim/Sulfamethoxazole
- TBRI:
-
Theodor Bilharz Research Institute
- TGC:
-
Tigecycline
- TOB:
-
Tobramycin
- VIM:
-
Verona Integron- encoded Metallo-β-Lactamase
References
Martinez-Martinez L, Gonzalez-Lopez JJ (2014) Carbapenemases in Enterobacteriaceae: types and molecular epidemiology. Enferm Infecc Microbiol Clin 32(4):4–9
Leski T, Vora GJ, Taitt CR (2012) Multidrug resistance determinants from NDM-1-producing Klebsiella pneumoniae in the USA. Int J Antimicrob Agents 40:282–284
Queenan AM, Bush K (2007) Carbapenemases: the versatile beta-lactamases. Clin Microbiol Rev 20:440
Nordmann P, Poirel L (2013) Strategies for identification of carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother 68:487–489
Gamal D, Egea P, Elias C, Fernández-Martínez M , Causse M , Pérez-Nadales E et al (2020) High-risk clones and novel sequence type ST4497 of Klebsiella pneumoniae clinical isolates producing different alleles of NDM-type and other carbapenemases from a single tertiary-care centre in Egypt. Int J Antimicrob Agents 56(6): 106164
Nordmann P (2014) Carbapenemase-producing Enterobacteriaceae: overview of a major public health challenge. Med Mal Infect 44(2):51–56
Ambretti S, Bassetti M, Clerici P, Petrosillo N, Tumietto F, Viale P et al (2019) Screening for carriage of carbapenem-resistant Enterobacteriaceae in settings of high endemicity: a position paper from an Italian working group on CRE infections. Antimicrob Resist Infect Control 8:136
CLSI. Clinical and Laboratory Standard Institute. Performance standards for antimicrobial susceptibility testing. 32nd ed. CLSI supplement M100. Clinical and Laboratory Standards Institute, USA, 2022.
EUCAST. The European Committee on Antimicrobial Susceptibility Testing. EUCAST guidelines for detection of resistance mechanisms and specific resistances of clinical and/or epidemiological importance, version 1.0. 2013. http://www.eucast.org/resistance_mechanisms.
EUCAST. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 12.0, 2022. http://www.eucast.org.
Poirel L, Walsh TR, Cuvillier V, Nordmann P (2018) Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 70(1):119–123
Abdelaziz MO, Bonura C, Aleo A, Fasciana T, Mammina C (2013) NDM-1- and OXA-163-producing Klebsiella pneumoniae isolates in Cairo, Egypt, 2012. J Glob Antimicrob Resist 1(4):213–215
Amer WH, Khalil HS, Abd EL Wahab MAA. Risk factors, phenotypic and genotypic characterization of carbapenem resistant Enterobacteriaceae in Tanta University Hospitals, Egypt. Int J Infect Control. 2016;12(i12).
Kotb S, Lyman M, Ismail G, Abd El Fattah M, Girgis SA, Etman A et al . Epidemiology of carbapenem-resistant Enterobacteriaceae in Egyptian intensive care units using national healthcare–associated infections surveillance data, 2011–2017. Antimicrob Resist Infect Control. 2020; 9: 2.
Pan F, Tian D, Wang B, Zhao W, Qin H, Zhang T et al (2019) Fecal carriage and molecular epidemiology of carbapenem-resistant Enterobacteriaceae from outpatient children in Shanghai. BMC Infect Dis 19:678
Richter SS, Marchaim D (2017) Screening for carbapenem-resistant Enterobacteriaceae: who, when, and how? Vir 8(4):417–426
Ghaith DM, Mohamed ZK, Farahat MG, Shahin WA, Mohamed HO (2019) Colonization of intestinal microbiota with carbapenemase-producing Enterobacteriaceae in paediatric intensive care units in Cairo, Egypt. Arab J Gastroenterol 20(1):19–22
Perez LRR, Rodrigues D, Dias CG (2015) Evaluation of phenotypic tests to detect carbapenem-resistant Enterobacteriaceae in colonized patients hospitalized in intensive care units. Braz J Infect Dis 19(4):436–438
Tran DM, Larsson M, Olson L, Hoang NTB, Le NK, Khu DTK et al (2019) High prevalence of colonisation with carbapenem-resistant Enterobacteriaceae among patients admitted to Vietnamese hospitals: risk factors and burden of disease. J Infect 79(2):115–122
Rossini A, Di Santo SG, Libori MF, Tiracchia V, Balice MP, Salvia A (2016) Risk factors for carbapenemase-producing Enterobacteriaceae colonization of asymptomatic carriers on admission to an Italian rehabilitation hospital. J Hosp Infect 92(1):78–81
AlFadhli AH, Jamal WY, Rotimi VO. Prevalence of carbapenem-resistant Enterobacteriaceae and emergence of high rectal colonization rates of blaOXA-181-positive isolates in patients admitted to two major hospital intensive care units in Kuwait. Plos One. 2020.
Moghnieh RA, Kanafani ZA, Tabaja HZ, Sharara SL, Awad LS, Kanj SS (2018) Epidemiology of common resistant bacterial pathogens in the countries of the Arab League. Lancet Infect Dis 18:12
Zakaa El-din M, Samy F, Mohamed A, Hamdy F, Yasser S, Ehab M (2019) Egyptian community pharmacists’ attitudes and practices towards antibiotic dispensing and antibiotic resistance; a cross-sectional survey in Greater Cairo. Curr Med Res Opinion 35(6): 939–946.
EUCAST (2017) The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters, version 7.1. http://www.eucast.org.
Mancini S, Kieffer N, Poirel L, Nordmann P (2017) Evaluation of the Rapidec CARBA NP and β-CARBA tests for rapid detection of carbapenemase-producing Enterobacteriaceae. Diag Microbiol Infect Dis 88(4):293–297
Perry JD, Nagvi SH, Mirza IA, Alizai SA, Hussain A, Ghirardi S et al (2011) Prevalence of faecal carriage of Enterobacteriaceae with NDM-1 carbapenemase at military hospitals in Pakistan, and evaluation of two chromogenic media. J Antimicrob Chemother 66(10):2288–2294
McConville TH, Sullivan SB, Gomez- Simmonds A, Whittier S, Uhlemann AC (2017) Carbapenem-resistant Enterobacteriaceae colonization (CRE) and subsequent risk of infection and 90-day mortality in critically ill patients, an observational study. PLoS One 12(10): e0186195
Tang HJ, Hsieh CF, Chang PC, Chen JJ, Lin YH, Lai CC et al (2016) Clinical significance of community- and healthcare-acquired carbapenem-resistant Enterobacteriaceae isolates. Plos One 11(3): e0151897
Soliman AM, Khalifa HO, Ahmed AM, Shimamoto T, Shimamoto T (2016) Emergence of an NDM-5-producing clinical Escherichia coli isolate in Egypt. Int J Inf Dis 48:46–48
El-Kholy AA, Girgis SA, Shetta MAF, Abdel-Hamid DH, Elmanakhly AR (2020) Molecular characterization of multidrug-resistant Gram-negative pathogens in three tertiary hospitals in Cairo, Egypt. Eur J Clin Microbiol Infect Dis
Zowawi HM, Sartor AL, Balkhy HH, Walsh TR, Al Johani SM, AlJindan RY et al (2014) Molecular characterization of carbapenemase-producing Escherichia coli and Klebsiella pneumoniae in the countries of the Gulf Cooperation Council: dominance of OXA-48 and NDM producers. Antimicrob Agents Chemother 58(6):3085–3090
Yan J, Pu S, Jia X, Xu X, Yang S, Shi J et al (2017) Multidrug resistance mechanisms of carbapenem-resistant Klebsiella pneumoniae strains isolated in Chongqing. China Ann Lab Med 37(5):398–407
Gomides MDA, Fontes AMdS, Silveira AOSM, Matoso DC Ferreira AL, Sadoyama G (2022) The importance of active surveillance of carbapenem-resistant Enterobacterals (CRE) in colonization rates in critically ill patients. PLoS ONE 17(1): e0262554
Morrill HJ, Pogue JM, Kaye KS, LaPlante KL (2015) Treatment options for carbapenem-resistant Enterobacteriaceae infections. Open Forum Infect Dis 2(2): ofv050
Acknowledgements
We acknowledge Theodor Bilharz Research Institute (TBRI), Microbiology Department—Project 99 D for funding this work.
Funding
Theodor Bilharz Research Institute (TBRI), affiliated to ministry of higher education and scientific research, funded this work, as a part of an internal Project No. 99 D. TBRI approved the project idea and supplied all materials and kits required to accomplish the work.
Author information
Authors and Affiliations
Contributions
El-Defrawy I, PI of TBRI internal project 99D from which this study aroused, designed the study, supervised all the work, and contributed in the analysis of the results. Gamal D contributed in research work in addition to supervision of technical work, analysis of the data, and in writing the manuscript. El-Seidi E supervised technical work, analyzed the data, and drafted the manuscript. El-Dabaa E supervised the molecular work and contributed in data analysis. Eissa S supervised the microbiological work and contributed in the analysis of the results. El-Gharbawy R performed the bacterial culture, laboratory work, interpreted the results and performed statistical analysis. All authors critically revised the manuscript, and approved the final version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol of this work was approved by Theodor Bilharz Research Institute (TBRI) institutional review board (FWA00010609). The work has been carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for Experiments in Humans. Each patient or caregivers (for those not able to consent) provided written informed consent. This work was presented as poster in the 29th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in Amsterdam (13–16 April 2019).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Defrawy, I., Gamal, D., El-Gharbawy, R. et al. Detection of intestinal colonization by carbapenem-resistant Enterobacteriaceae (CRE) among patients admitted to a tertiary care hospital in Egypt. Egypt J Med Hum Genet 23, 83 (2022). https://doi.org/10.1186/s43042-022-00295-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-022-00295-9