Abstract
Gastrointestinal colonization of carbapenem-resistant Enterobacteriaceae (CRE) could serve as a reservoir for the transmission of these pathogens in the clinical setting. The aim of this study was to investigate the intestinal carriage of CRE and to analyze risk factors for CRE carriage. Rectal swabs were collected from 95 patients at two Iranian university hospitals. CRE screening was performed using selective media (CHROMagar and MacConkey agar). Polymerase chain reaction (PCR) was used to detect carbapenemase-encoding genes. Clonal relatedness was investigated by pulsed-field gel electrophoresis (PFGE). The rate of carriage of CRE in hospitalized patients was 37.9%. Overall, 54 CRE isolates were identified, of which 47 were carbapenemase-producers. All of the 54 CRE were detected using CHROMagar compared with 52 CRE detected using MacConkey agar. Fifteen patients were colonized by multiple CRE isolates. Three significant risk factors for CRE carriage were detected: intensive care unit (ICU) hospitalization, antibiotic exposure, and mechanical ventilation. bla OXA-48 was the most frequent carbapenemase detected, followed by bla NDM-1 and bla NDM-7. Eleven carbapenemase-producing Enterobacteriaceae (CPE) isolates co-harbored bla NDM-1 and bla OXA-48. Also, six CPE isolates co-harbored bla NDM-7 and bla OXA-48. We did not detect bla KPC, bla GES, bla IMP, or bla VIM. PFGE analysis showed that Escherichia coli clones were diverse, while Klebsiella pneumoniae isolates were divided into four clusters. Cluster I was the major clone carrying bla OXA-48 and bla CTX-M-15 genes. In our study, the carriage rate of CRE was high and the emergence of CPE isolates among patients is alarming. The implementation of adequate preventive measures such as active surveillance is urgently needed to control the spread of CPE in the healthcare setting.


Similar content being viewed by others
References
Nordmann P, Dortet L, Poirel L (2012) Carbapenem resistance in Enterobacteriaceae: here is the storm! Trends Mol Med 18:263–272
Harris PNA, Tambyah PA, Paterson DL (2015) β-lactam and β-lactamase inhibitor combinations in the treatment of extended-spectrum β-lactamase producing Enterobacteriaceae: time for a reappraisal in the era of few antibiotic options? Lancet Infect Dis 15:475–485
Nordmann P (2014) Carbapenemase-producing Enterobacteriaceae: overview of a major public health challenge. Med Mal Infect 44:51–56
Viau R, Frank KM, Jacobs MR, Wilson B, Kaye K, Donskey CJ et al (2016) Intestinal carriage of carbapenemase-producing organisms: current status of surveillance methods. Clin Microbiol Rev 29:1–27
Nordmann P, Naas T, Poirel L (2011) Global spread of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 17:1791–1798
Lascols C, Peirano G, Hackel M, Laupland KB, Pitout JDD (2013) Surveillance and molecular epidemiology of Klebsiella pneumoniae isolates that produce carbapenemases: first report of OXA-48-like enzymes in North America. Antimicrob Agents Chemother 57:130–136
Barguigua A, Zerouali K, Katfy K, El Otmani F, Timinouni M, Elmdaghri N (2015) Occurrence of OXA-48 and NDM-1 carbapenemase-producing Klebsiella pneumoniae in a Moroccan university hospital in Casablanca, Morocco. Infect Genet Evol 31:142–148
Dandachi I, Salem Sokhn E, Najem E, Azar E, Daoud Z (2016) Carriage of beta-lactamase-producing Enterobacteriaceae among nursing home residents in north Lebanon. Int J Infect Dis 45:24–31
Kilic A, Baysallar M (2015) The first Klebsiella pneumoniae isolate co-producing OXA-48 and NDM-1 in Turkey. Ann Lab Med 35:382–383
Nobari S, Shahcheraghi F, Rahmati Ghezlgeh F, Valizadeh B (2014) Molecular characterization of carbapenem-resistant strains of Klebsiella pneumoniae isolated from Iranian patients: first identification of bla KPC gene in Iran. Microb Drug Resist 20:285–293
Zhao ZC, Xu XH, Liu MB, Wu J, Lin J, Li B (2014) Fecal carriage of carbapenem-resistant Enterobacteriaceae in a Chinese university hospital. Am J Infect Control 42:e61–e64
Centers for Disease Control and Prevention (CDC) (2009) Laboratory protocol for detection of carbapenem-resistant or carbapenemase-producing, Klebsiella spp. and E. coli from rectal swabs. CDC, Atlanta, GA. Available online at: https://www.cdc.gov/hai/pdfs/labsettings/klebsiella_or_ecoli.pdf
Pournaras S, Zarkotou O, Poulou A, Kristo I, Vrioni G, Themeli-Digalaki K et al (2013) A combined disk test for direct differentiation of carbapenemase-producing Enterobacteriaceae in surveillance rectal swabs. J Clin Microbiol 51:2986–2990
Adler A, Navon-Venezia S, Moran-Gilad J, Marcos E, Schwartz D, Carmeli Y (2011) Laboratory and clinical evaluation of screening agar plates for detection of carbapenem-resistant Enterobacteriaceae from surveillance rectal swabs. J Clin Microbiol 49:2239–2242
Moran Gilad J, Carmeli Y, Schwartz D, Navon-Venezia S (2011) Laboratory evaluation of the CHROMagar KPC medium for identification of carbapenem-nonsusceptible Enterobacteriaceae. Diagn Microbiol Infect Dis 70:565–567
Clinical and Laboratory Standards Institute (CLSI) (2015) Performance standards for antimicrobial susceptibility testing; Twenty-fifth informational supplement. CLSI document M100-S25. CLSI, Wayne, PA
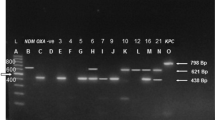
Poirel L, Walsh TR, Cuvillier V, Nordmann P (2011) Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 70:119–123
Doyle D, Peirano G, Lascols C, Lloyd T, Church DL, Pitout JD (2012) Laboratory detection of Enterobacteriaceae that produce carbapenemases. J Clin Microbiol 50:3877–3880
Shahcheraghi F, Nobari S, Rahmati Ghezelgeh F, Nasiri S, Owlia P, Nikbin VS et al (2013) First report of New Delhi metallo-beta-lactamase-1-producing Klebsiella pneumoniae in Iran. Microb Drug Resist 19:30–36
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH et al (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33:2233–2239
Girlich D, Bouihat N, Poirel L, Benouda A, Nordmann P (2014) High rate of faecal carriage of extended-spectrum β-lactamase and OXA-48 carbapenemase-producing Enterobacteriaceae at a university hospital in Morocco. Clin Microbiol Infect 20:350–354
Pantel A, Marchandin H, Prère MF, Boutet-Dubois A, Brieu-Roche N, Gaschet A et al (2015) Faecal carriage of carbapenemase-producing Gram-negative bacilli in hospital settings in southern France. Eur J Clin Microbiol Infect Dis 34:899–904
Papadimitriou-Olivgeris M, Marangos M, Fligou F, Christofidou M, Bartzavali C, Anastassiou ED et al (2012) Risk factors for KPC-producing Klebsiella pneumoniae enteric colonization upon ICU admission. J Antimicrob Chemother 67:2976–2981
Wiener-Well Y, Rudensky B, Yinnon AM, Kopuit P, Schlesinger Y, Broide E et al (2010) Carriage rate of carbapenem-resistant Klebsiella pneumoniae in hospitalised patients during a national outbreak. J Hosp Infect 74:344–349
Tijet N, Richardson D, MacMullin G, Patel SN, Melano RG (2015) Characterization of multiple NDM-1-producing Enterobacteriaceae isolates from the same patient. Antimicrob Agents Chemother 59:3648–3651
Cheng VCC, Chen JHK, Wong SCY, Ho PL, Yuen KY (2016) Gastrointestinal colonization with multiple New Delhi metallo-β-lactamase-producing Enterobacteriaceae isolates in the same patient: a potential challenge in outbreak investigation. J Hosp Infect 92:108–109
Girlich D, Nordmann P, Lécuyer H, Berche P, Marmorat-Khuong A, Gros I et al (2015) Multiple colonization with highly resistant bacteria: carbapenemase-producing Enterobacteriaceae, carbapenemase-producing Pseudomonas aeruginosa, carbapenemase-producing Acinetobacter baumannii, and glycopeptide-resistant Enterococcus faecium. Diagn Microbiol Infect Dis 81:217–218
Karaaslan A, Soysal A, Altinkanat Gelmez G, Kepenekli Kadayifci E, Söyletir G, Bakir M (2016) Molecular characterization and risk factors for carbapenem-resistant Gram-negative bacilli colonization in children: emergence of NDM-producing Acinetobacter baumannii in a newborn intensive care unit in Turkey. J Hosp Infect 92:67–72
Torres-Gonzalez P, Cervera-Hernandez ME, Niembro-Ortega MD, Leal-Vega F, Cruz-Hervert LP, García-García L et al (2015) Factors associated to prevalence and incidence of carbapenem-resistant Enterobacteriaceae fecal carriage: a cohort study in a Mexican tertiary care hospital. PLoS One 10:e0139883
Candevir Ulu A, Kurtaran B, Seza Inal A, Kömür S, Kibar F, Çiçekdemir HY et al (2015) Risk factors of carbapenem-resistant Klebsiella pneumoniae infection: a serious threat in ICUs. Med Sci Monit 21:219–224
Sonnevend Á, Ghazawi AA, Hashmey R, Jamal W, Rotimi VO, Shibl AM et al (2015) Characterization of carbapenem-resistant Enterobacteriaceae with high rate of autochthonous transmission in the Arabian peninsula. PLoS One 10:e0131372
Seiffert SN, Marschall J, Perreten V, Carattoli A, Furrer H, Endimiani A (2014) Emergence of Klebsiella pneumoniae co-producing NDM-1, OXA-48, CTX-M-15, CMY-16, QnrA and ArmA in Switzerland. Int J Antimicrob Agents 44:260–262
Xie L, Dou Y, Zhou K, Chen Y, Han L, Guo X et al (2017) Coexistence of bla OXA-48 and truncated bla NDM-1 on different plasmids in a Klebsiella pneumoniae isolate in China. Front Microbiol 8:133
Al-Marzooq F, Ngeow YF, Tay ST (2015) Emergence of Klebsiella pneumoniae producing dual carbapenemases (NDM-1 and OXA-232) and 16S rRNA methylase (armA) isolated from a Malaysian patient returning from India. Int J Antimicrob Agents 45:445–446
Perry JD, Naqvi SH, Mirza IA, Alizai SA, Hussain A, Ghirardi S et al (2011) Prevalence of faecal carriage of Enterobacteriaceae with NDM-1 carbapenemase at military hospitals in Pakistan, and evaluation of two chromogenic media. J Antimicrob Chemother 66:2288–2294
Panagea T, Galani I, Souli M, Adamou P, Antoniadou A, Giamarellou H (2011) Evaluation of CHROMagar™ KPC for the detection of carbapenemase-producing Enterobacteriaceae in rectal surveillance cultures. Int J Antimicrob Agents 37:124–128
Song W, Hong SG, Yong D, Jeong SH, Kim HS, Kim HS et al (2015) Combined use of the modified Hodge test and carbapenemase inhibition test for detection of carbapenemase-producing Enterobacteriaceae and metallo-β-lactamase-producing Pseudomonas spp. Ann Lab Med 35:212–219
Woodford N, Tierno PM Jr, Young K, Tysall L, Palepou MF, Ward E et al (2004) Outbreak of Klebsiella pneumoniae producing a new carbapenem-hydrolyzing class a beta-lactamase, KPC-3, in a New York medical center. Antimicrob Agents Chemother 48:4793–4799
Nematzadeh S, Shahcheraghi F, Iversen A, Giske CG (2015) Successful international clones of bla CTX-M-15-producing Klebsiella pneumoniae with coexpression of plasmid-mediated quinolone resistance (PMQR) determinants in Tehran hospitals. Diagn Microbiol Infect Dis 83:371–374
Acknowledgments
This research was supported by the Pasteur Institute of Iran. The authors would like to thank the personnel of the Pasture Institute of Iran and the staff of both hospitals for their help. Also, the authors are grateful to Dr. Ehsan Mostafavi for help with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
This project was done based on ethical guidelines as previously approved by the Pasteur institute of Iran (project no: IR.PII.REC.1395.51).
Conflict of interest
No conflicts of interest declared.
Rights and permissions
About this article
Cite this article
Solgi, H., Badmasti, F., Aminzadeh, Z. et al. Molecular characterization of intestinal carriage of carbapenem-resistant Enterobacteriaceae among inpatients at two Iranian university hospitals: first report of co-production of bla NDM-7 and bla OXA-48 . Eur J Clin Microbiol Infect Dis 36, 2127–2135 (2017). https://doi.org/10.1007/s10096-017-3035-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3035-3