Abstract
Background
Obesity is a health problem defined by surplus body fat accumulation and is one of the leading causes of morbidity and mortality. Earlier studies indicated the influence of brain-derived neurotrophic factor (BDNF) molecular alterations in the development of obesity. One of these variations is the G196A single nucleotide polymorphism (Val66Met; SNP rs6265), which impairs intracellular trafficking and reduces the secretion of BDNF. In this study, we evaluated the possible association of G196A polymorphism of the BDNF gene with body mass index (BMI) among women from the Iranian Azeri Turkish ethnic group. Four hundred eighty-four women including 343 women with obesity or overweight and 141 age-sex and ethnically matched healthy controls were genotyped for G196A SNP of BDNF gene by applying polymerase chain reaction-restriction fragment length polymorphism (PCR–RFLP) method. The association of this polymorphism with BMI was evaluated using analysis of covariance (ANCOVA), and the comparison of alleles and genotypes frequencies between patients (obese and/or overweight participants) and healthy controls was carried out using logistic regression models.
Results
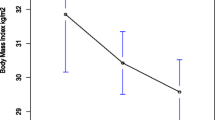
Individuals carrying Met-Met genotype have a significantly lower mean of BMI in comparison to those carrying non-Met/Met polymorphisms (P = 0.0138).
Conclusions
In this study, the association of the Val66Met polymorphism of the BDNF gene with BMI as an obesity trait has been confirmed among the women from the Northwest of Iran.
Similar content being viewed by others
Background
Obesity is one of the important health problems in which excess body fat accumulation can lead to increased mortality and risk of disease, such as metabolic syndrome, type 2 diabetes, stroke, coronary heart disease, liver and gallbladder disease, cancer, osteoarthritis, and sleep disorders [1]. In 1997, obesity was formally recognized as a global epidemic by the World Health Organization (WHO) [2]. According to the WHO, more than 1.9 billion adults (39% of men and 40% of women) were overweight in 2016. Of these, over 650 million adults (11% of men and 15% of women) had obesity and approximately 41 million children under 5 years of age were overweight or obese [3].
The rate of obesity is increasing in both developed and developing countries over the past two decades [4]. In the Middle East, including the Arabian Peninsula, Eastern Mediterranean, Turkey, and Iran, obesity is a notable health issue [5]. In Iran, the prevalence of obesity has reached epidemic proportions and according to a recent study, it was 26.3% in 2008 [6].
As a multifactorial and complex disease, obesity can be influenced by genetic and environmental factors [7]. Several studies have reported some variants in multiple genes that may contribute to gaining weight and distribution of body fat [8]. The contribution of genetic factors in obesity development is estimated to be 40–70% [9].
It has been documented that BDNF belongs to the neurotrophin family of growth factors and supports the survival and differentiation of existing neuronal populations in the peripheral and central nervous systems and synapses through its receptor, tropomyosin-related kinase B (TrkB) [10]. It is abundant in the central nervous system (CNS), especially in the hypothalamus, basal forebrain, cortex, hippocampus, and amygdala, areas that are critical in memory and learning [11]. Recent evidence suggests the effect of BDNF in weight regulation and its association with obesity in multiple types of knockout mouse models [12, 13].
The role of BDNF in the regulation of food absorption [14] and its dose-dependent appetite inhibition and weight loss were already described in previous studies [15].
Earlier studies indicated the involvement of BDNF molecular alterations in the development of obesity and eating disorders (EDs). One of these variations is the G196A single nucleotide polymorphism (Val66Met; SNP rs6265) [16]. rs6265 is a common SNP in the BDNF gene that has been associated with several clinical traits such as anxiety disorders, learning and memory disorders, neurodegenerative disorders including Parkinson’s and Alzheimer’s, obesity, and BMI [17, 18]. This exchange of valine to methionine at codon 66 located at the prodomain of BDNF interferes with the intracellular processing, trafficking, and secretion of BDNF [19].
The goal of this study was to evaluate the possible association of BDNF Val66Met polymorphism with susceptibility to obesity and BMI among women from the Turkish Azeri ethnic group. To the best of our knowledge, this would be the first investigation of the Val66Met polymorphism of BDNF gene in this population.
Methods
Study subjects
Our study included 484 women from the northwest region of Iran, who were divided into three groups: obesity (82 subjects), overweight (261 subjects), and control (141 subjects) groups from 17 to 59 years of age (mean ± SD age, 35.85 ± 9.18). This study was carried out in Tabriz city, the capital of East Azerbaijan Province, located in the Northwest of Iran, from December 2016 to August 2017. Participants were recruited through announcements and flyer distribution in public areas of the city. The inclusion criteria were between the ages of 17 and 60 years and living in Tabriz for at least 5 consecutive years. Also, all contributors in this study were premenopausal and not pregnant or lactating at the time of the study. Subjects who had been participated in weight loss programs during the last 6 months and those suffering from alcoholism, substance addiction, psychotic disorders, or a serious disease such as cardiovascular and endocrine diseases were excluded from the study.
Biological parameters
The patients with light clothing and no shoes were weighed and measured after a 12-h fasting period. Body weight was measured using an electronic scale that was calibrated periodically (SECA Birmingham, UK) with an accuracy of 0.1 kg. Height was measured using a fixed stadiometer to the nearest 0.1 cm. BMI was calculated as a person’s weight in kilograms divided by height in square meter (kg/m2). According to the BMI categories, determined by the World Health Organization in 1997, subjects were classified as obese (BMI ≥ 30.0), overweight (BMI = 25.0–29.9), and normal weight (BMI = 18.5–24.9) [20].
Genotyping
Four milliliters of venous blood samples was collected from all participants in EDTA anticoagulant polypropylene tubes. Written consent to inclusion was obtained from all participants and they were informed of the study. Our protocol was reviewed and approved by the Tabriz University of Medical Science Ethical Committee and assigned with the registry number 1395.1.133 (IR.TBZMED.REC.1397.347).
Genomic DNA from subjects was extracted from peripheral blood leukocytes by the use of simple salting-out procedure. The BDNF Val66Met polymorphism (dbSNP ID rs6265) at position G196A was identified by a polymerase chain reaction-restriction fragment length polymorphism (PCR–RFLP) technique as reported previously [21]. In brief, the 272-bp region of the BDNF gene, including the Val66Met polymorphism site, was amplified by using PCR. The PCR product was overnight digested by the restriction enzyme NlaIII at 37 °C. The genotype was identified by electrophoresis on 8% polyacrylamide gel and stained with ethidium bromide and visualized under ultraviolet light.
Statistical analysis
Statistical analysis was carried out using SAS 9.2 online software and SPSS. The association between Val66Met polymorphism and BMI (comparison of BMI means between genotypes) was evaluated using analysis of covariance (ANCOVA), and the comparison of allele and genotype frequencies between patients (obese or overweight participants or both of them) and healthy controls was carried out using logistic regression models. In this study, we regarded probability values of 0.05 or less as statistically significant. All analyses were adjusted for age.
Results
The baseline phenotypes and Val66Met genotypes of the participants in our study are demonstrated in Table 1. The distribution of BDNF Val66Met (rs6265) genotypes conformed to the Hardy-Weinberg equilibrium (P = 0.5). To characterize the risk of BDNF variant on obesity in this population, we evaluated the risk of being overweight and/or obese according to BDNF genotypes, by use of logistic regression models. Our participants were initially divided into two groups: the control group (BMI < 25) and patients with BMI ≥ 25. A comparison of the allele and genotype frequencies of Val66Met polymorphism between these two groups showed no significant differences (P = 0.465) (Table 2).
Afterward, we performed several analyses and compared allele and genotype frequencies between the following groups: obese participants (BMI ≥ 30) and controls (P = 0.5149), overweight (25 ≤ BMI < 30) participants and controls (P = 0.3054), and obese and overweight individuals (P = 0.3194) (Table 2).
In this cohort, we classified participants into three groups based on their genotypes (A/A, A/G, G/G). A comparison of BMI means among these groups revealed statistically significant differences (P = 0.0470). Individuals carrying AA genotypes in comparison to those carrying non-AA genotypes have statistically significant lower BMI (P = 0.0138) (Table 3).
Discussion
In the present study, we analyzed the possible association between the Val66Met (rs6265) polymorphism of BDNF gene and BMI among 484 women from the Iranian Azeri Turkish ethnic group, and to the best of our knowledge, this is the first survey of this association in Iran. Val66Met polymorphism was detected to be significantly linked with BMI in this study and women with AA (Met-Met) genotype had lower BMI than those with AG (Val-Met) and GG (Val-Val) genotypes. No significant association was observed between genotype and allele frequencies of overweights and controls and between obese and overweight participants.
The prevalence of obesity and correlated morbidities such as coronary heart disease, certain cancers, and type 2 diabetes are ascending, and obesity has become a serious public health issue [1]. Some environmental and lifestyle factors such as lack of physical activity and eating high-fat foods certainly increase the prevalence of obesity worldwide. However, differences in genetic makeup may lead to diversities of body weight in a population sharing the same environment [22]. Brain-derived neurotrophic factor (BDNF), encoded by the BDNF gene, is a member of the neurotrophin family of growth factors that bind to the tyrosine kinase receptor tropomyosin-related kinase B (TrkB) and activate signaling [10]. Haploinsufficient mice in which the BDNF gene has been eliminated demonstrate obesity with hyperactivity and hyperphagia [23].
It has also been reported that conditional deletion of BDNF in mice leads to stimulated longitudinal growth, 80–150% body weight gain, and increased serum of insulin, leptin, cholesterol, and glucose in the blood [13]. Val66Met polymorphism is a common single nucleotide polymorphism in the BDNF gene, which interferes with the intracellular trafficking of BDNF, resulting in the reduced secretion of this protein [19].
Our findings are broadly consistent with the studies carried out on British women populations by Gunstad et al. and Shugart et al. and also with the study on the Korean population reported by Hong et al. [18, 24, 25]. However, in other studies, individuals carrying Met-Met (A/A) or Val-Met (A/G) genotypes had higher mean BMI and also they were more likely obese than those carriers of Val-Val (G/G) genotypes [26,27,28]. These contradictory outcomes could be due to differences in lifestyle, environmental factors, and genetic backgrounds. The current study showing a significant association of Val66Met with BMI is restricted to the female participants from the Iranian Azeri Turkish ethnic group. So, we recommend a larger study including both men and women to characterize the gender differences in this association.
Conclusions
In our study, the association of the Val66Met polymorphism of the BDNF gene with BMI as an obesity trait has been confirmed in the Northwest of Iran women population. Mean BMI was significantly lower in women carrying AA (Met-Met) genotype compared to those with AG (Val-Met) and GG (Val-Val) genotypes (P = 0.0138).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BDNF:
-
Brain-derived neurotrophic factor
- BMI:
-
Body mass index
- PCR–RFLP:
-
Polymerase chain reaction-restriction fragment length polymorphism
- WHO:
-
World Health Organization
References
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH (2009) The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 9(1):88
Caballero B (2007) The global epidemic of obesity: an overview. Epidemiol Rev 29(1):1–5
World Health Organization. Obesity and overweight fact sheet. https://www.who.int. Accessed 1 Apr 2020.
Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E et al (2008) Management of obesity in adults: European clinical practice guidelines. Obes Facts 1(2):106–116
Godwin SM (2006) Globalization, education and Emiratisation: a study of the United Arab Emirates. Electron J Inf Syst Dev Ctries 27(1):1–14
Rashidy-Pour A, Malek M, Eskandarian R, Ghorbani R (2009) Obesity in the Iranian population. Obes Rev 10(1):2–6
Yazdi FT, Clee SM, Meyre D (2015) Obesity genetics in mouse and human: back and forth, and back again. PeerJ 3:e856
Ramachandrappa S, Farooqi IS (2011) Genetic approaches to understanding human obesity. J Clin Invest 121(6):2080–2086
Allison DB, Kaprio J, Korkeila M, Koskenvuo M, Neale MC, Hayakawa K (1996) The heritability of body mass index among an international sample of monozygotic twins reared apart. Int J Obes Relat Metab Disord 20(6):501–506
Acheson A, Conover JC, Fandl JP, DeChiara TM, Russell M, Thadani A et al (1995) A BDNF autocrine loop in adult sensory neurons prevents cell death. Nature 374(6521):450–453
Yamada K, Nabeshima T (2003) Brain-derived neurotrophic factor/TrkB signaling in memory processes. J Pharmacol Sci 91(4):267–270
Lyons WE, Mamounas LA, Ricaurte GA, Coppola V, Reid SW, Bora SH et al (1999) Brain-derived neurotrophic factor-deficient mice develop aggressiveness and hyperphagia in conjunction with brain serotonergic abnormalities. Proc Natl Acad Sci USA 96(26):15239–15244
Rios M, Fan G, Fekete C, Kelly J, Bates B, Kuehn R et al (2001) Conditional deletion of brain-derived neurotrophic factor in the postnatal brain leads to obesity and hyperactivity. J Mol Endocrinol 15(10):1748–1757
Lapchak PA, Hefti F (1992) BDNF and NGF treatment in lesioned rats: effects on cholinergic function and weight gain. Neuroreport 3(5):405–408
Pelleymounter MA, Cullen MJ, Wellman CL (1995) Characteristics of BDNF-induced weight loss. Exp Neurol 131(2):229–238
Thorleifsson G, Walters GB, Gudbjartsson DF, Steinthorsdottir V, Sulem P, Helgadottir A et al (2009) Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat Genet 41(1):18–24
Lu B, Nagappan G, Guan X, Nathan PJ, Wren P (2013) BDNF-based synaptic repair as a disease-modifying strategy for neurodegenerative diseases. Nat Rev Neurosci 14(6):401–416
Gunstad J, Schofield P, Paul RH, Spitznagel MB, Cohen RA, Williams LM et al (2006) BDNF Val66Met polymorphism is associated with body mass index in healthy adults. Neuropsychobiology 53(3):153–156
Bath KG, Lee FS (2006) Variant BDNF (Val66Met) impact on brain structure and function. Cogn Affect Behav Neurosci 6(1):79–85
World Health Organization. Body mass index - BMI. https://www.euro.who.int. Accessed 13 Nov 2020.
Martínez-Ezquerro JD, Rendón-Macías ME et al (2017) Association between the brain-derived neurotrophic factor val66met polymorphism and overweight/obesity in pediatric population. Arch Med Res 48(7):599–608
Wardle J, Carnell S, Haworth CM, Plomin R (2008) Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr 87(2):398–404
Kernie SG, Liebl DJ, Parada LF (2000) BDNF regulates eating behavior and locomotor activity in mice. EMBO J 19(6):1290–1300
Shugart YY, Chen L, Day IN, Lewis SJ, Timpson NJ, Yuan W et al (2009) Two British women studies replicated the association between the Val66Met polymorphism in the brain-derived neurotrophic factor (BDNF) and BMI. Eur J Hum Genet 17(8):1050–1055
Hong KW, Lim JE, Go MJ, Shin YS, Ahn Y, Han BG et al (2012) Recapitulation of the association of the Val66Met polymorphism of BDNF gene with BMI in Koreans. Obesity 20(9):1871–1875
Beckers S, Peeters A, Zegers D, Mertens I, Van Gaal L, Van Hul W (2008) Association of the BDNF Val66Met variation with obesity in women. Mol Genet Metab 95(1-2):110–112
Zhang XY, Zhou DF, Wu GY, Cao LY, Tan YL, Haile CN et al (2008) BDNF levels and genotype are associated with antipsychotic-induced weight gain in patients with chronic schizophrenia. Neuropsychopharmacology 33(9):2200–2205
Akkermann K, Hiio K, Villa I, Harro J (2011) Food restriction leads to binge eating dependent upon the effect of the brain-derived neurotrophic factor Val66Met polymorphism. Psychiatry Res 185(1-2):39–43
Acknowledgements
Not applicable.
Funding
The Center of Excellence for Biodiversity (University of Tabriz) supported us by giving their laboratory to study this association.
Author information
Authors and Affiliations
Contributions
Study design: MB and RM; data collection: HH, MB, RM, and FA; data analysis: AR and HH; manuscript preparation: HH and MB. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors give thanks to all the study participants. Written consent to inclusion was obtained from all participants and they were informed of the study. Our protocol was reviewed and approved by Tabriz University of Medical Science Ethical Committee and assigned with the registry number 1395.1.133 (IR.TBZMED.REC.1397.347).
Consent for publication
Not applicable.
Competing interests
The authors confirm that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Honarmand, H., Bonyadi, M., Rafat, A. et al. Association study of the BDNF gene polymorphism (G196A) with overweight/obesity among women from Northwest of Iran. Egypt J Med Hum Genet 22, 7 (2021). https://doi.org/10.1186/s43042-020-00130-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-020-00130-z