Abstract
Purpose
A better understanding of total knee arthroplasty (TKA) candidate expectations within the perioperative setting will enable clinicians to promote patient-centered practices, optimize recovery times, and enhance quality metrics. In the current study, TKA candidates were surveyed pre- and postoperatively to elucidate the relationship between patient expectations and length of stay (LOS).
Material and methods
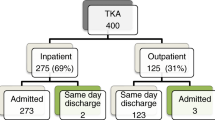
This is a prospective study of patients undergoing TKA between December 2017 and August 2018. Patients were electronically administered surveys regarding their discharge plan 10 days pre-/postoperatively. All patients were categorized into three cohorts based on their LOS: 1, 2, and 3+ days. The effect of preoperative discharge education on patient postoperative satisfaction was evaluated.
Results
In total, 221 TKAs were included, of which 83 were discharged on postoperative day (POD) 1, 96 on POD-2, and 42 POD-3+. Female gender, increasing body mass index (BMI), and surgical time correlated with increased LOS. Preoperative discussions regarding LOS occurred in 84.62% (187/221) of patients but did correlate with differences in LOS. However, patients discharged on POD-1 were more inclined to same-day surgery preoperatively. Patients discharged on POD-3+ were found to be more uncomfortable regarding their discharge during the preoperative phase. Multivariable regressions demonstrated that preoperative discharge discussion was positively correlated with home discharge.
Conclusion
Physician-driven discussion regarding patient discharge did not alter patient satisfaction or length of stay but did correlate with improved odds of home discharge. These findings underscore the importance of patient education, shared decision-making, and managing patient expectations.
Similar content being viewed by others
Background
Total knee arthroplasty (TKA) is one of Medicare’s largest contributors to surgical expenditures—from 2002 to 2013, TKA total hospital costs tripled to $12 billion [1]. During this time period, average hospital costs per TKA were reported to increase only 52.4% ($7849) within the same time period [1]. The increase in total hospital costs has therefore been attributed to its rapid growth in overall demand and utilization [2,3,4]. As reported by the Healthcare Cost and Utilization Project (HCUP), it has been estimated that 700,100 inpatient TKAs were performed in 2012 alone, sustaining its position as the most common inpatient surgical procedure in the USA [5]. Despite a recent slowing in TKA volume, it is estimated that 935,000 TKAs will be performed per annum by 2030 [4].
Under the current payment models, healthcare organizations have shifted their focus from volume-based care to a system of value-based and quality-driven care [6,7,8,9,10,11]. In doing so, substantially greater emphasis has been placed on improving hospital operating efficiency, improving patient safety and satisfaction, and reducing care variability. One specific area of focus has been securing timely discharges as an initiative to reduce per-episode-of-care expenditures for TKA [6,7,8,9,10,11].
Recent literature has emphasized the value of shared decision-making with preoperative patients as a model to educate patients about their perioperative care, improve patient satisfaction, and reduce episode-of-care costs. The “DECISIONS” study by Zikmund-Fisher et al. highlighted the need for orthopedic surgeons to better understand, communicate, and manage patient expectations in the perioperative setting [12]. For orthopedic surgeons, indications for TKA were discussed in only 76% of patient encounters, and patient treatment preferences were discussed in only 72% of surgical cases [12]. As medicine continues to transition away from its paternalistic roots and incentivizes a more patient-centric approach, patient education and the incorporation of patient care preferences will be paramount [12].
In a previous multicenter study evaluating patient satisfaction following total hip arthroplasty (THA), physician-initiated discussion of patient discharge was correlated with shorter lengths of stay (LOS) and improved patient satisfaction [13]. By implementation of Standardized Care Pathways (SCPs) set forth by the Centers for Medicare and Medicaid Services (CMS), institutions have successfully reduced the LOS while maintaining the current quality of care; however, there continues to be a paucity of studies evaluating the effects of SCPs on patient-perceived effects, expectations, and satisfaction [6, 7]. Patient education and expectations are common components of many of the current pathways and education programs and have encountered a wide range of results [14,15,16,17]. Furthermore, as patient-reported outcomes (PROs) and the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores become an integral component of future alternative payment models (APMs), the importance of patient satisfaction and shared decision-making becomes synonymous with healthcare organization and physician reimbursement [8,9,10,11, 18].
The primary objective of our study is to evaluate the effect of preoperative, physician-initiated shared decision-making regarding hospital LOS and its effect on postoperative patient satisfaction for patients undergoing TKA. We hypothesize that preoperative shared discussion will enhance postoperative patient satisfaction and outcomes.
Materials and methods
This is a prospective observational study of TKA candidates between December 2017 and August 2018 at a single, urban, academic healthcare organization. As part of our institution’s standard of care practices, all patients scheduled for total joint arthroplasty were enrolled in a commercially available electronic patient rehabilitation application (EPRA) (Force Therapeutics; New York, NY). Briefly, EPRA is a digital, customizable episode-of-care management tool designed to provide patients with pre- and postoperative educational materials in the form of text, videos, and short quizzes, while also acting as a communication portal between patients and healthcare providers. Moreover, the EPRA platform can push and email custom and validated patient-reported outcome (PRO) surveys to the patient’s smart device or computer, allowing physicians to better track the progress of their patients. Given the platform capabilities, we designed a novel survey to assess the effects of managing patient expectations on patient discharge satisfaction, as assessed by patient-reported “comfort” (Table 1).
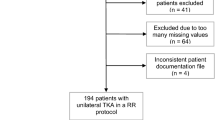
All patients were electronically administered surveys regarding their discharge planning 10 days pre- and postoperatively via push notifications and emails. Patient demographics, surgical factors, and hospital-reported LOS were queried from our institution’s electronic data warehouse, Epic Caboodle (Verona, WI), utilizing Microsoft SQL Server Management Studio (Redmond, WA). Missing patient data were manually chart-checked via our electronic health record (EHR) system, Epic Hyperspace (Verona, WI). Patients were categorized into three cohorts on the basis of their actual hospital LOS based on calendar day: 1 day, 2 day, and 3+ days. Patients discharged on postoperative day (POD) 0 were excluded from the study owing to limited sample size (n = 6) but retained in our tables for descriptive purposes only. It was noted that two surgeons had only contributed a single patient each to the study. To minimize potential bias, their respective two patients were excluded from the study. The remaining surgeons contributed equally to the study (range 44–63 patients each).
All data transformations and statistical analyses were performed using the Anaconda (version 5.3.0; Anaconda Inc., Austin, TX) distribution of Python (version 3.6.6; Python Software Foundation, https://www.python.org). Libraries utilized in this study included pandas, numpy, scipy, statsmodels, patsy, and their respective library dependencies. Statistical analyses of univariable continuous outcomes were performed utilizing one-way analysis of variance (ANOVA) testing, while categorical variables were tested utilizing χ2 tests. Multivariable logistic regression was performed to evaluate what factors effect patient discharge comfort, as well as a separate multivariable linear regression to evaluate what factors may affect actual inpatient LOS. A p-value of < 0.05 was deemed significant.
Results
Patient demographics
In total, 221 elective, primary TKAs were performed by four surgeons within the study period (Table 1). Eighty-three (37.56%) TKAs were discharged on POD-1, 96 (43.44%) were discharged on POD-2, and 42 (19.00%) were discharged on POD-3 or later. Assessment of patient demographics demonstrated that female gender (female gender prevalence: POD-1 discharge 48.19%, POD-2 discharge 62.50%, POD-3+ discharge 76.19%; p < 0.01), increasing BMI [average BMI ± 1 standard deviation (SD): POD-1 discharge 30.09 ± 6.24 kg/m2, POD-2 discharge 31.27 ± 6.59 kg/m2, POD-3+ discharge 33.88 ± 8.25 kg/m2; p < 0.05] and insurance type (commercial versus Medicare insurance: POD1 discharge 56.63% versus 39.76%, POD2 discharge 55.21% versus 36.46%, POD1 discharge 28.57% versus 57.14) were correlated with longer LOS cohorts. While nonsignificant, patients who were categorized as “single, divorced, or widowed” were more prevalent in extended LOS cohorts (POD-1 discharge 43.37%, POD-2 discharge 41.67%, POD-3+ discharge 61.90%; p = 0.07). Age (p = 0.91), race (p = 0.83), smoking status (p = 0.53), and surgical time (p = 0.26) were similar between cohorts (Table 2).
Survey validity and administration
To assess our patient population’s understanding of their inpatient stay, patients were asked the duration of their LOS in a postoperative survey and these values were compared with their actual LOS (Table 3). Patient-reported LOS was correct in 96.38% of surveys (21/221) patients; denoted by ‡ in Table 3). All surveys were provided 10 ± 9 days before and 9 ± 2 days after their day of discharge.
Preoperative survey
Discussions regarding a patient’s LOS was reported in 84.62% (187/221 patients) of preoperative patient encounters and was equally distributed among the cohorts (p = 0.57). With regard to preoperative estimated LOS, as reported by patients, only 42.53% (94/221 patients; denoted by † in Table 3) were provided accurate estimates of their expected LOS.
Across all cohorts, 43.98% of patients reported feeling “very comfortable,” and 39.82% of patients reported feeling “somewhat comfortable,” with the preoperative discharge plans. Moreover, patients in cohorts with longer LOS were less likely to feel “very comfortable” with their discharge plan preoperatively [“very comfortable”: POD-1 discharge 55.42% (46/83 patients), POD-2 discharge 40.62% (39/96 patients), POD-3+ discharge 28.57% (12/42 patients); < 0.01], and were also less likely to have enrolled in a same-day discharge (SDD) program if provided the opportunity [“very likely” or “likely”: POD 1 discharge 62.65% (52/83 patients), POD-2 discharge 28.13% (27/96 patients), POD-3+ discharge 14.29% (6/42 patients); < 0.0001].
Postoperative survey
Postoperatively, patients generally reported an increase in their comfort with their discharge planning (Table 3). In total, 53.85% (119/221 patients) of patients reported being “very comfortable,” up from the 43.89% preoperatively. Meanwhile, only 1.36% of patients felt very uncomfortable regarding their discharge, substantially less than the 7.24% preoperatively. Cohorts with longer LOS were less likely to elicit “very comfortable” responses [“very comfortable”: POD-1 discharge 60.24% (50/83 patients), POD-2 discharge 54.17% (52/96 patients), POD-3+ discharge 40.48% (17/42 patients)], but these findings were not statistically significant (p = 0.09). When surveyed about LOS duration, 84.62% (187/221) of patients were satisfied, similar among the groups (p = 0.13).
Preoperative factors affecting discharge
To evaluate whether preoperative discharge discussions improved patient comfort at discharge, a χ2 test was performed, which was nonsignificant (p = 0.39). A follow-up multivariable logistic regression was performed (Table 4). Postoperative patient-reported comfort with their discharge plan was separated into binary outcomes: “comfortable” and “uncomfortable.” No significant correlation was found between preoperative discharge discussion and postoperatively surveyed discharge comfort (p = 0.80).
A secondary multivariable linear regression analysis of patient factors affecting inpatient LOS was performed (Table 5). The presence or absence of a preoperative discussion was not found to significantly alter inpatient LOS (β = −0.01; 95% CI 0.30–2.42; p = 0.95). Conversely, male gender (β = 0.34; 95% CI 0.10–0.59; p < 0.05), Medicare payor type (β = 0.56; 95% CI 0.06–1.05; p < 0.001), and worker’s compensation/no-fault payor type (β = 1.75; 95% CI 0.80–2.71; p < 0.001) were all significantly correlated with increased inpatient LOS to varying degrees. Current smoker was correlated with a shorter length of stay (β = −0.24; 95% CI −0.47 to 0.01; p < 0.05).
Finally, a multivariable logistic regression evaluating the effect of preoperative discharge discussions on discharge disposition was performed (Table 6). As 98.19% (217/221) patients were discharged home, regression convergence was not possible for race, smoking status, and insurance type. Race, smoking, and worker’s compensation/no fault (three patients) were excluded from the analysis. Preoperative discussions were found to significantly increase likelihood of home discharge compared with a skilled nursing facility (OR 3.87; 95% CI 1.05–14.20; p < 0.05). Similarly, increasing age was correlated with increased odds for home discharge (OR 1.07; 95% CI 1.00–1.15; p < 0.05). Conversely, single, divorced, or widowed marital status was correlated with increased odds of subacute nursing facility discharge (OR 0.24; 95% CI 0.06–094; p < 0.05).
Discussion
TKA remains a major driver of Medicare surgical expenditures [1], and length of stay is a major driver of inpatient costs [19, 20]. Nationally, implementation of Standardized Care Pathways (SCPs) set forth by CMS has resulted in decreased LOS for patients undergoing TKA [6, 7]. Care pathways are an evidence-based multidisciplinary approach that includes preoperative education; these pathways have been implemented with success and reductions in hospital expenditures by several groups [6, 21, 22]. Patient-reported outcomes, especially patient satisfaction metrics, are increasingly being incorporated into reimbursement models as metrics of success. Physicians’ ability to influence patient expectations of postoperative course and disposition may be a means to not only improve reimbursement and metrics of success but better engage patients and increase comfort with their care. In our study, 83% of patients were very comfortable or somewhat comfortable with their preoperative discharge plan, which increased to 89% being very comfortable or somewhat comfortable postoperatively. Eighty-four percent of patients received preoperative discussion regarding length of stay and discharge disposition. This is higher than previously published in reports of orthopedic surgeons [12].
Despite the initiation of preoperative counseling, it remains difficult to accurately inform patients of their exact LOS. Our data demonstrate that 42.5% (9/221 patients) were provided accurate estimates of their expected LOS. In a recent meta-analysis, Shah et al. found increasing age, female gender, BMI ≥ 30 kg/m2, and American Society of Anesthesiology (ASA) score > 2 to increase LOS [23]. In our study, female gender and worker’s compensation insurance were associated with increased length of stay on multivariate analysis. Female gender has been associated with increased length of stay by several authors [24,25,26]. Proposed explanations include increased pain and increased severity of arthritis prior to intervention and decreased social support at home. The number of patients with the primary payor of worker’s compensation or no fault included in this study was small, only three of the total 221 patients and likely not generalizable. Worker’s compensation claim status has been a risk factor for decreased satisfaction in other orthopedic conditions [27,28,29].
In this prospective observational study, preoperative discussions regarding patient discharge nonsignificantly trended toward improved patient comfort toward discharge during the postoperative phase, but there was no perceivable effect on LOS. The effect of preoperative education in knee replacement was examined in a Cochrane review in 2014 by McDonald et al., who at that time found an almost 2-day reduction in length of stay for patients undergoing TKA who received preoperative education [30]. Pamilo et al. also found a significant decrease in length of stay and an increased proportion of discharges to home without an increase in revisions, manipulations, mortality, or readmissions [31]. While patients were counseled by both a surgeon and nurse, it is presumed that an institution-wide adoption of a “fast track” program was the primary driver of reduced LOS. Husted and colleagues stressed the importance of counseling both the patient and their family, providing both written and verbal information regarding length of stay when implementing and organizing a fast-track program [25, 32]. We therefore hypothesize that an institutional adoption of patient counseling regarding discharge is more effective than surgeon-driven counseling in isolation.
When compared with commercial payor types, Medicare and worker’s compensation/no fault was significantly correlated with increasing LOS. In a case–control by Halawi et al., Medicare insurance type was significantly correlated with 4.42 greater odds for inpatient LOS > 2 days when compared with commercial payor types, which was attributed primarily to the CMS’s inpatient-only status of TKA at the time of their study [33]. The effect is further substantiated when compared with Medicaid payor types, which demonstrated 3.88 greater odds for > 2 days LOS for Medicare patients.
Smoking was correlated with a shorter LOS by 0.24 days when compared with nonsmokers on multivariable linear regression. A previous study at our institution demonstrated a 0.15-day (2.47 versus 2.62 days; p = 0.56) decrease in LOS for patients who completed our 4–6-week preoperative smoking cessation program when compared with continued smokers [34]. In a randomized control trial in Denmark by Moller et al., smoking cessation was also demonstrated to decrease inpatient length of stay (11 days versus 13 days) [35].
In recent years, the LOS for TKA has declined from weeks to days [1]; in our study, most patients were discharged on POD-1 or 2. Further reductions in LOS may have diminishing financial returns. However, preoperative discussions do help set patient expectations and identify patients with barriers to discharge, including reduced social support [32]. Discharge destination impacts both quality measures and cost. Our study found that patients receiving preoperative discussion were significantly more likely to be discharged to home than a subacute nursing facility. In a retrospective review of 372 patients undergoing consecutive total joint arthroplasty, Halawi and colleagues found that age, caregiver support at home, and patient expectation of discharge destination were the only significant predictors of discharge destination. Among the variables examined, patient expectation was the most important predictor (p < 0.001). Their group has begun to incorporate discharge destination determination in the preoperative clinic visit leading to a subjective appreciation of decreased LOS [36]. Patients’ readiness for discharge is a complex interplay of physiologic, psychologic, and social factors [37]. In a study of total hip arthroplasty (THA) recipients, Heine et al. found the main concern of patients prior to discharge was feeling safe at home, which included both patients’ personal confidence in their abilities and support of family [38]. Both of these components may be addressed pre- and postoperatively. Our study assessed feelings of comfort with the discharge plan; while most patients were very comfortable or somewhat comfortable, a proportion of patients noted a level of discomfort in their plan. Targeted intervention regarding the lack of comfort in these patients may provide a method to decrease the length of stay and increase patient satisfaction.
Paradoxically, older patients in our study demonstrated an increased rate of home discharge based on our multivariable linear regression. This contradicts previous studies demonstrating that older and more geriatric patients are more likely to experience longer LOS and discharge to skilled nursing facilities [39]. At our institution, discharge to skilled nursing facilities is mostly secondary to limited social support (living alone) and/or home environmental factors, particularly walkups and stairs. It is therefore hypothesized that our increased discharge rate to facilities in comparably younger patients may be skewed by factors such as younger patients living alone and/or in higher walkup housing, while older patients may have accommodated themselves in homes with limited stairs, elevator access, and/or living with family support or in assistive living. It is also conceivable our results may be the result of a type II error.
We found patients who were single or divorced trended toward discharge to a facility rather than home. Literature regarding the association of social support and discharge destination is mixed. Slover et al. found no association between pain-catastrophizing behavior or social support with length of stay or discharge disposition [26]. Weaver et al. found that females undergoing TKA were less likely to be married than their male counterparts, and not being married was associated with longer LOS in both males and females [40]. Napier et al. cited social reasons as the most common cause for delayed discharge in patients undergoing THA or TKA and recommended preoperative agreement regarding discharge plan prior to admission for arthroplasty [41]. As marital status remains a proxy for social support, surgeons and the multidisciplinary teams involved in planning patients’ preoperative discharge destination should inquire about the patient’s social setting to ensure safe and timely discharge.
The relationship between shared decision-making and measurable quality improvement is difficult to objectively assess within the clinical setting. Our investigation did not find a significant reduction in LOS among patients having preoperative discharge discussions. However, these patients were more likely to be discharged home with improved patient comfort. Physicians and other members of the care team should be encouraged to discuss LOS and discharge disposition with TKA candidates with the goal of improving patient satisfaction, readiness for discharge, and the preoperative identification of any healthcare barriers.
Conclusion
While the results of our study indicate that physician-driven discussion regarding patient discharge does not alter patient satisfaction or length of stay, it did correlate with improved odds of home discharge. These findings underscore the importance of patient education, shared decision-making, and managing patient expectations. Future studies are needed to evaluate what key components of the physician–patient interaction may address underlying patient anxieties and/or hesitations for shorter LOS and home discharge. Additional studies investigating potential financial savings and the economic impact of these simple physician–patient interactions are also warranted.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TKA:
-
Total knee arthroplasty
- THA:
-
Total hip arthroplasty
- HCUP:
-
Healthcare Cost and Utilization Project
- LOS:
-
Length of stay
- SCPs:
-
Standardized Care Pathways
- CMS:
-
Centers for Medicare and Medicaid Services
- PROs:
-
Patient-reported outcomes
- HCAHPS:
-
Hospital Consumer Assessment of Healthcare Providers and Systems
- APM:
-
Alternative payment models
- EPRA:
-
Electronic patient rehabilitation application
- EHR:
-
Electronic health records
- SDD:
-
Same-day discharge
- POD:
-
Postoperative day
References
Molloy IB, Martin BI, Moschetti WE, Jevsevar DS (2017) Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Jt Surg 99(5):402–407
Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR (2012) Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991–2010. JAMA 308(12):1227–1236
Williams SN, Wolford ML, Bercovitz A (2015) Hospitalization for total knee replacement among inpatients aged 45 and over: United States, 2000–2010. NCHS Data Brief 210:1–8
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. J Bone Jt Surg 100(17):1455–1460
Fingar KR, Stocks C, Weiss AJ, Steiner CA. Most frequent operating room procedures performed in U.S. hospitals, 2003–2012: Statistical Brief #186. 2006
Iorio R, Clair AJ, Inneh IA, Slover JD, Bosco JA, Zuckerman JD (2016) Early results of medicare’s bundled payment initiative for a 90-day total joint arthroplasty episode of care. J Arthroplasty 31(2):343–350
Dundon JM, Bosco J, Slover J, Yu S, Sayeed Y, Iorio R (2016) Improvement in total joint replacement quality metrics: year one versus year three of the bundled payments for care improvement initiative. J Bone Jt Surg Am 98(23):1949–1953
Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R. Total knee arthroplasty: improving outcomes with a multidisciplinary approach. http://www.ncbi.nlm.nih.gov/pubmed/29416347
Cizmic Z, Novikov D, Feng J, Iorio R, Meftah M (2019) Alternative payment models in total joint arthroplasty under the Affordable Care Act. JBJS Rev 7(3):e4
Novikov D, Cizmic Z, Feng JE, Iorio R, Meftah M (2018) The historical development of value-based care: how we got here. J Bone Jt Surg Am 100(22):e144
Anoushiravani AA, Iorio R (2016) Alternative payment models: from bundled payments for care improvement and comprehensive care for joint replacement to the future? Semin Arthroplasty 27(3):151–162
Zikmund-Fisher BJ, Couper MP, Singer E, Levin CA, Fowler FJ, Ziniel S et al (2010) The DECISIONS study: a nationwide survey of United States adults regarding 9 common medical decisions. Med Decis Making 30:20–34
Padilla JA, Feng JE, Anoushiravani AA, Hozack WJ, Schwarzkopf R, Macaulay WB (2019) Modifying patient expectations can enhance total hip arthroplasty postoperative satisfaction. J Arthroplasty 34(7S):S209–S214
Jones S, Alnaib M, Kokkinakis M, Wilkinson M, St Clair Gibson A, Kader D (2011) Pre-operative patient education reduces length of stay after knee joint arthroplasty. Ann R Coll Surg Engl 93(1):71–75
Huang S-W, Chen P-H, Chou Y-H (2012) Effects of a preoperative simplified home rehabilitation education program on length of stay of total knee arthroplasty patients. Orthop Traumatol Surg Res 98(3):259–264
Moulton LS, Evans PA, Starks I, Smith T (2015) Pre-operative education prior to elective hip arthroplasty surgery improves postoperative outcome. Int Orthop 39(8):1483–1486
Kearney M, Jennrich MK, Lyons S, Robinson R, Berger B (2011) Effects of preoperative education on patient outcomes after joint replacement surgery. Orthop Nurs 30(6):391–396
Anoushiravani AA, Nunley RM (2017) Gainsharing strategies, physician champions, getting physician buy in. J Arthroplasty 32(6):1723–1727
Olthof M, Stevens M, Bulstra SK, van den Akker-Scheek I (2014) The association between comorbidity and length of hospital stay and costs in total hip arthroplasty patients: a systematic review. J Arthroplasty 29(5):1009–1014
Healy WL, Ayers ME, Iorio R, Patch DA, Appleby D, Pfeifer BA (1998) Impact of a clinical pathway and implant standardization on total hip arthroplasty: a clinical and economic study of short-term patient outcome. J Arthroplasty 13(3):266–276
Siddiqi A, White PB, Mistry JB, Gwam CU, Nace J, Mont MA et al (2017) Effect of bundled payments and health care reform as alternative payment models in total joint arthroplasty: a clinical review. J Arthroplasty 32(8):2590–2597
McLawhorn AS, Buller LT (2017) Bundled payments in total joint replacement: keeping our care affordable and high in quality. Curr Rev Musculoskelet Med 10(3):370–377
Shah A, Memon M, Kay J, Wood TJ, Tushinski DM, Khanna V et al (2019) Preoperative patient factors affecting length of stay following total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 34(9):2124-2165.e1
Ponnusamy KE, Naseer Z, El Dafrawy MH, Okafor L, Alexander C, Sterling RS et al (2017) Post-discharge care duration, charges, and outcomes among medicare patients after primary total hip and knee arthroplasty. J Bone Jt Surg Am 99(11):e55
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 79:168–173
Edusei E, Grossman K, Payne A, Perez B, Inneh I, Nelson C et al (2017) Impact of social support and pain coping ability on length of stay and discharge disposition following hip and knee arthroplasty: a prospective study. Bull Hosp Jt Dis 75(2):137–139
Kim KC, Lee W-Y, Shin HD, Han S-C, Yeon K-W (2018) Do patients receiving workers’ compensation who undergo arthroscopic rotator cuff repair have worse outcomes than non-recipients? Retrospective case–control study. J Orthop Surg 26(3):230949901880250
Tufescu TV, Buckley R (2001) Age, gender, work capability, and worker’s compensation in patients with displaced intraarticular calcaneal fractures. J Orthop Trauma 15(4):275–279
Morris BJ, Haigler RE, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB (2015) Workers’ compensation claims and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg 24(3):453–459
McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A (2014) Preoperative education for hip or knee replacement. In: McDonald S (ed) Cochrane database of systematic reviews. Wiley, Chichester
Pamilo KJ, Torkki P, Peltola M, Pesola M, Remes V, Paloneva J (2018) Fast-tracking for total knee replacement reduces use of institutional care without compromising quality. Acta Orthop 89(2):184–189
Husted H (2012) Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop Suppl 83(346):1–39
Halawi MJ, Stone AD, Gronbeck C, Savoy L, Cote MP (2019) Medicare coverage is an independent predictor of prolonged hospitalization after primary total joint arthroplasty. Arthroplasty Today 5(4):489
Herrero C, Tang A, Wasterlain A, Sherman S, Bosco J, Lajam C et al (2020) Smoking cessation correlates with a decrease in infection rates following total joint arthroplasty. J Orthop 21:390
Møller AM, Villebro N, Pedersen T, Tønnesen H (2002) Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 359(9301):114–117
Halawi MJ, Vovos TJ, Green CL, Wellman SS, Attarian DE, Bolognesi MP (2015) Patient expectation is the most important predictor of discharge destination after primary total joint arthroplasty. J Arthroplasty 30(4):539–542
Fenwick AM (1979) An interdisciplinary tool for assessing patients’ readiness for discharge in the rehabilitation setting. J Adv Nurs 4(1):9–21
Heine J, Koch S, Goldie P (2004) Patients’ experiences of readiness for discharge following a total hip replacement. Aust J Physiother 50(4):227–233
Cheung A, Fu H, Cheung MH, Chan WKV, Chan PK, Yan CH et al (2020) How well do elderly patients do after total knee arthroplasty in the era of fast-track surgery? Arthroplasty 2(1):1–6
Weaver F, Hynes D, Hopkinson W, Wixson R, Khuri S, Daley J et al (2003) Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty 18(6):693–708
Napier RJ, Spence D, Diamond O, O’Brien S, Walsh T, Beverland DE (2013) Modifiable factors delaying early discharge following primary joint arthroplasty. Eur J Orthop Surg Traumatol 23(6):665–669
Acknowledgements
N/A.
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Contributions
J.F., A.A., J.M., W.P., and V.S. equally contributed to this work, which included data collection, analysis, and manuscript preparation. R.S. and W.M. oversaw the conceptualization of the project and made final edits prior to submission. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was conducted upon receiving approval from the institutional review board (IRB). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Consent to publish was obtained from all individual participants included in the study.
Competing interests
J.F., A.A., J.M., W.P., and V.S. have nothing to disclose. R.S. is a paid consultant for Intellijoint and Smith&Nephew and holds stock options in Gauss Surgical and PSI. W.M. holds stock options in OrthoAlign.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Feng, J.E., Anoushiravani, A.A., Morton, J.S. et al. Preoperative Patient Expectation of Discharge Planning is an Essential Component in Total Knee Arthroplasty. Knee Surg & Relat Res 34, 26 (2022). https://doi.org/10.1186/s43019-022-00152-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43019-022-00152-4