Abstract
Background
Graft malposition is a risk factor for failure of anterior cruciate ligament reconstruction. A 70° arthroscope improves visualisation of the medial wall of the lateral femoral condyle without switching portals. We investigated whether the use of this arthroscope affected the accuracy and precision of femoral tunnel placement.
Methods
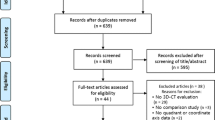
Fifty consecutive adult patients were recruited. Following one withdrawal and two exclusions, 47 patients (30 in group 1 (70° arthroscope), 17 in group 2 (30° arthroscope)) underwent three-dimensional computed tomography imaging using a grid-based system to measure tunnel position.
Results
No difference was found in the accuracy or precision of tunnels (mean position: group 1 = 33.3 ± 6.0% deep–shallow, 27.2 ± 5.2% high–low; group 2 = 31.7 ± 6.9% deep–shallow, 29.0 ± 6.2% high–low; not significant). A post-hoc power analysis suggests a study of 106 patients would be required.
Conclusions
This pilot study suggests that tunnel position is not affected by the arthroscope used. An appropriately powered study could investigate this finding alongside other potential benefits of using a 70° arthroscope for this procedure.
Trial registration
ClinicalTrials.gov, NCT02816606. Registered on 28 June 2016.
Similar content being viewed by others
Background
Graft malposition has been shown to be a major cause of failure in anterior cruciate ligament (ACL) reconstruction [1]. Therefore, a goal for the surgeon is to accurately position the tunnels in relation to either anatomical landmarks or direct measurements [2, 3]. The femoral tunnel is a particular challenge as, when the medial wall of the lateral femoral condyle is viewed from the anterolateral portal using a 30° arthroscope, a foreshortened perspective is achieved [4]. Therefore, many surgeons switch to viewing via the anteromedial portal to confirm placement (prior to tunnel drilling). However, the surgeon then must switch back to the anterolateral portal for drilling or risk over-crowding by viewing through an accessory anteromedial portal. An alternative technique is the use of a 70° arthroscope through the anterolateral portal [4, 5]. This provides a less foreshortened view of the footprint of the ACL that is comparable to the 30° arthroscope view from the anteromedial portal (Fig. 1). Perceived advantages of using the 70° arthroscope are that it prevents the need for switching between portals, it can be maintained whilst the tunnel is drilled, and it gives an improved “bird’s eye” view of the tibial footprint for tunnel placement [4, 5].
Whilst this technique is well described, no previous studies have compared the accuracy of this versus the use of a conventional 30° arthroscope. The aim of this pilot study was to directly compare the femoral tunnel positions achieved using these two arthroscopes (70° via an anterolateral portal and 30° via an anteromedial portal) in a clinical setting. Our primary hypothesis was that there would be no difference between the accuracy of the two techniques. As a pilot study, the additional goal was to inform future work comparing these techniques.
Methods
Patients were recruited as part of a published study comparing flexible and rigid femoral tunnel reamers [6]. Ethical review board approval was additionally received, prior to study commencement, for the present analysis (study number 16/SW/0080). Informed consent for both entry into the trial and the extra imaging required was gained via consultation and a written information pack. The additional radiation exposure for one computed tomography (CT) scan (0.16 mSv) was equivalent to eight chest x-rays or 1 month’s background radiation exposure. The trial was registered with an online trial database.
Patients were randomised on the basis of the reaming system used but not the arthroscope choice. This allocation was based on surgeon preference and availability. Therefore, there were unequal numbers of patients in the study groups. No a priori power analysis was possible due to the lack of published data comparing this variable.
Fifty consecutive adult patients with an isolated ACL injury were recruited to the study. Their demographics are shown in Table 1. Patients under 18 years of age were excluded to ensure skeletal maturity and to allow the use of previously defined measurement techniques. Multi-ligament injuries and revision surgery were also excluded to prevent issues related to tunnel (and fixation) conflict. The final exclusion criterion was inadequate postoperative imaging. One patient was excluded after enrolment due to an unwillingness to attend for postoperative imaging and two patients were excluded due to incomplete posterior blow-out of the tunnel, making measurements of the tunnel aperture centre inaccurate.
In total, there were 31 procedures performed using a 70° arthroscope (group 1) and 18 procedures performed with the 30° arthroscope (group 2) for visualisation. One patient from each group was excluded due to incomplete posterior blow-out preventing accurate assessment of the tunnel centre.
All procedures were performed by the two senior authors (PJS and VIM, both with over 8 years of consultant experience specialising in soft-tissue knee reconstruction). The femoral tunnels were positioned under direct vision (with either arthroscope) using a microfracture awl. For group 1, all viewing was performed via the 70° arthroscope via the anterolateral portal. For group 2, the position of the intended tunnel was first marked, whilst viewing from the anterolateral portal, and then checked (and adjusted) via anteromedial portal viewing. It is routine for our surgeons to mark the tunnel in this way (first via the anterolateral tunnel) using the microfracture awl via the anteromedial portal. However, the acceptance of the tunnel position was made only after verification following switching of the portals. If required, this process was repeated until the intended tunnel position was achieved. Once accepted, a guide wire and cannulated reamer were used to create the tunnel in this position. Each surgeon used both arthroscopic techniques (in approximately equal numbers) throughout the study to avoid this being a potential source of bias to the results. Both surgeons aimed to position the graft within the anteromedial bundle position based on anatomical markers (posterior to the bifurcate ridge and inferior to the intercondylar ridge) and distance from the posterior wall. This position has been shown to be associated with a reduced incidence of graft rupture compared to a mid-bundle position [7]. All patients were reconstructed using autologous hamstring tendon graft with suspensory fixation in the femur. Where additional meniscal or chondral pathology was encountered, this was treated using the same arthroscope as used to position the femoral tunnel. Numbers were too small to compare directly these additional procedures.
Three-dimensional CT (3D-CT) was performed between 3 and 6 months postoperatively. Images were collected using a spiral sequence with 0.625-mm cuts. Surface rendering was applied (Advantage Workstation VolumeShare 7, GE, Waulesha, USA) with manipulation to a standardised position; the medial and lateral femoral epicondyles were overlapped (true lateral position) and the medial condyle was subtracted (in the sagittal plane through the femoral intercondylar notch). Tunnel position measurements were then made using a grid positioned along Blumensaat’s line including the maximal dimensions of the lateral condyle (Fig. 2). This method has been shown to be reliable and valid in previous studies [8, 9]. All measurements were made by the same consultant musculoskeletal radiologist who was blinded to the surgical technique used. Measurements were recorded from the centre of the aperture of the tunnel to the maximal extents of the grid using the conventional deep–shallow (DS) and high–low (HL) measurements and expressed as percentages of the total grid dimensions (Fig. 2).
The accuracy of the tunnel position was calculated in comparison to previously published data defining the anatomical position of the centre of the anteromedial bundle of the ACL using 3D-CT of cadaveric specimens (34.2% (DS); 26.3% (HL)) [10]. This point was defined as the true centre (TC). Trigonometric calculation was then used to define the distance of the aperture centre (AC) of the created tunnel to the defined optimum anatomical position (Fig. 3). The distance was calculated using the following formula: c = √(a2 + b2). The precision of the tunnel position was compared using the standard deviation of the absolute differences recorded. This methodology has previously been used in similar studies [11, 12].
Calculation of difference between centre of tunnel aperture (AC; red square) and anatomical centre of anteromedial bundle (TC; blue triangle) shown on three-dimensional computed tomography reconstructed image; measurements a and b parallel and perpendicular (respectively) to Blumensaat’s line (on expanded view, distance c = √(a2 + b2))
Statistical analysis was performed using SPSS (version 5, IBM, Portsmouth, UK). Continuous data were compared using an unpaired t test. Discreet data were compared using a chi-squared test (with Yate’s correction for small numbers). Precision data were compared using Levene’s test of variance equivalence. Statistical significance was set at P < 0.05. A post-hoc power analysis was performed based on the calculated mean and standard deviations generated by the pilot study (α = 0.05, β = 0.8).
Results
A summary of the results is shown in Table 2. All operated patients attended for postoperative imaging. As mentioned in the methodology, two patients were excluded from the analysis due to the presence of incomplete posterior blow-out of the tunnel (one in each group). Both blow-outs involved only the distal part of the tunnel, affecting the accurate calculation of the tunnel centre (without compromising the suspensory fixation used).
In the remaining 47 patients, there was no significant difference in the position of the tunnels created or the accuracy of placement (distance between TC and AC). When the number of tunnels within 5, 10, and 15% of the absolute dimensions were compared, no difference was demonstrated. There was also no difference in the precision of the two techniques. A graphical display of the tunnel positions is shown in Fig. 4.
Post-hoc power analysis showed that a study with 106 patients (53 in each group) would be required to adequately compare the accuracy of these techniques.
Discussion
The main finding of the study was that there was no difference between arthroscopes in centring a femoral tunnel in a desired position. With equal accuracy and precision, the variation in tunnel position likely reflects the anatomical variation seen in previous studies. The primary hypothesis would therefore have been accepted although a larger study size is required to confidently do so. It is, however, likely that a 70° arthroscope represents a worthwhile alternative to a 30° arthroscope without the additional need for portal switching. We believe this is a technique, with additional benefits, that can be readily adopted. Furthermore, this study informs continued work in this area.
Positioning of the femoral tunnel in ACL reconstruction requires good intra-operative visualisation of either native anatomy or intra-operative measurements. We believe that it is better for the surgeon to individualise tunnel position based on anatomy, but it still remains controversial exactly how the footprint should be identified and where within this the tunnel should be centred [13,14,15]. Our preferred choice of an anteromedial bundle position is increasingly supported by the literature with recent work demonstrating a four-fold reduction in graft failure compared to a mid-bundle position [7].
Quantitative comparison of the accuracy and precision of anatomical tunnel placement is difficult given an accepted variation in both the position of anatomical landmarks and reproducibility of surgical techniques as well as the focus of this study (the arthroscopic visualisation achieved). However, the present study used 3D-CT (shown to be the most accurate method of tunnel measurement) to compare a single defined reconstruction technique [8].
Multiple anatomical and radiological studies suggest that the ACL footprint varies in both position and size [2, 16,17,18] with Luites and Verdonschot reporting variation of 4 mm (in both DS and HL dimensions) about a mean value [19]. Similarly, the accuracy of surgical placement is seen to vary about a planned point. In a study by Hart et al., four different “anatomical” techniques were compared with a mean error in placement of 3–4 mm with each method [20]. Thus, there is variation in both anatomy and surgical accuracy (both in the region of 4 mm) equating to combined errors that may be relatively large (8 mm). While our results reflect these variations (in both anatomy and surgical precision) no difference was seen between the two tested arthroscopes, suggesting visualisation is equivalent.
Alternative proposed techniques (to maximise visualisation) include the use a 30° arthroscope via an accessory anteromedial portal [21, 22] or central viewing portal [23]. We chose to use the 70° arthroscope as it allows for medial portal drilling without over-crowding or additional portal creation, with most surgeons accustomed to using this arthroscope for posterior cruciate reconstruction [4, 5]. Additional benefits have also been described including the improved bird’s-eye view of the tibial footprint during tunnel positioning [5]. We found any required meniscal and chondral work also relatively easy with the 70° arthroscope, although in a less experienced group a greater learning curve may be expected (as seen with other ACL techniques) [24, 25].
Limitations of this study include those inherent to the pilot study design and the methodology used. This study was powered to show a difference in an independent variable (reamer design). The post-hoc calculation suggests that a larger study group may be required to find a difference in tunnel position between these two arthroscopic techniques. The groups were not randomised (and arthroscope choice was largely based on surgeon preference), although the demographics were well matched and the analysis was independent of knee size. The inherent potential for bias is balanced against the pragmatism of such a study. Additionally, the methodology used to define accuracy was based on previous anatomical work that may not reflect every surgeon’s preferred position. An alternative would be to study the ability to position a marker on a pre-defined goal anatomical position (for example, on the bifurcate ridge). This may give a better measure of accuracy and precision. However, conducting such a study would be problematic, with additional pre-operative imaging required outside of a cadaveric setting. The inclusion of two surgeons introduces potential bias in differences of intended tunnel position. Despite both surgeons using the two techniques in roughly equal numbers, as this was not randomised there may be inherent differences between the surgeons that may not be present in a single surgeon series. Finally, the relationship between accurate tunnel position and function or complications could not be investigated. This would require an adequately powered study solely focused on this factor to make valid conclusions. The conclusions from the present study, and recommendations made, are purposefully reserved in light of these limitations.
Conclusion
Both arthroscopic techniques show the ability to position the femoral tunnel in an acceptable position in a clinical group. No difference was found between the techniques reported, suggesting that use of the 70° arthroscope represents a valid alternative that is worthy of consideration given the other described benefits. The importance of accuracy and precision of these techniques could be studied in a larger group with further work focussed on the impact of surgical experience and the functional consequences of potential differences identified. Furthermore, if our findings of equivalence are shown, future work should focus on the other proposed advantages of this technique including tibial tunnel visualisation as well as operative time and ease.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 3D-CT:
-
Three-dimensional computed tomography
- AC:
-
Aperture centre
- ACL:
-
Anterior cruciate ligament
- CT:
-
Computed tomography
- DS:
-
Deep–shallow
- HL:
-
High–low
- TC:
-
True centre
References
Moisala AS, Jarvela T, Harilainen A, Sandelin J, Kannus P, Jarvinen M (2007) The effect of graft placement on clinical outcome of the anterior cruciate ligament reconstruction: a prospective study. Knee Surg Sports Traumatol Arthrosc 15:879–887
Bird JH, Carmont MR, Dhillon M, Smith N, Brown C, Thompson P, Spalding T (2011) Validation of a new technique to determine midbundle femoral tunnel position in anterior cruciate ligament reconstruction using 3-dimensional computer tomography analysis. Arthroscopy 27:1259–1267
Sullivan JP, Matava MJ, Flanigan DC, Gao Y, Britton CL, Amendola A, Wolfe BR (2012) Reliability of tunnel measurements and the quadrant method using fluoroscopic radiographs after anterior cruciate ligament reconstruction. Am J Sports Med 40:2236–2241
Bucher TA, Naim S, Mandalia V (2014) The use of the 70o arthroscope for anatomic femoral and tibial tunnel placement and tunnel viewing in anterior cruciate ligament reconstruction. Arthrosc Tech 3:e79–e81
Mandalia VI, Kosy JD (2016) Anterior cruciate ligament reconstruction with 70-degree arthroscope and flexible reamers—early operative experience. J Arthrosc Joint Surg 3:51–55
Kosy JD, Walmsley K, Anaspure R, Schranz PJ, Mandalia VI (2019) Flexible reamers produce comparable anterior cruciate ligament reconstruction femoral tunnels without the hyperflexion required with rigid reamers: 3D-CT analysis of femoral tunnel morphology in a randomised clinical trial. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05709-7. [Epub ahead of print].
Borton ZM, Yasen SK, Mumith A, Wilson A (2018) Mid-bundle positioning of the femoral socket increases graft rupture in anatomic single bundle anterior cruciate ligament reconstruction. Knee 25:1122–1128
Kosy JD, Mandalia VI (2018) Plain radiographs can be used for routine assessment of ACL reconstruction tunnel position with three-dimensional imaging reserved for research and revision surgery. Knee Surg Sports Traumatol Arthrosc 26:534–549
Lertwanich P, Martins CAQ, Asai AS, Ingham SJM, Smolinski P, Fu FH (2011) Anterior cruciate ligament tunnel position measurement reliability on 3-dimensional reconstructed computer tomography. Arthroscopy 27:391–398
Lee JK, Lee S, Seong SC, Lee MC (2015) Anatomy of the anterior cruciate ligament insertion sites: comparison of plain radiography and three-dimensional computed tomographic imaging to anatomical dissection. Knee Surg Sports Traumatol Arthrosc 23:2297–2305
Luites JWH, Wymenga AB, Blankevoort L, Eygendaal D, Verdonschot N (2013) Accuracy of a computer-assisted planning and placement system for anatomical femoral tunnel positioning in anterior cruciate ligament reconstruction. Int J Med Robot 10:438–446
Sirleo L, Innocenti M, Innocenti M, Civinini R, Carulli C, Matassi F (2018) Post-operative 3D CT feedback improves the accuracy and precision in the learning curve of anatomic ACL femoral tunnel placement. Knee Surg Sports Traumatol Arthrosc 26:468–477
Ilahi OA, Mansfield DJ, Urrea LH 2nd, Qadeer AA (2014) Reliability and reproducibility of several methods of arthroscopic assessment of femoral tunnel position during anterior cruciate ligament reconstruction. Arthroscopy 30:1303–1310
Markatos K, Kaseta MK, Lallos SN, Korres DS, Efstathopoulos N (2013) The anatomy of the ACL and its importance in ACL reconstruction. Eur J Orthop Surg Traumatol 23:747–752
Wolfe BR, Ramme AJ, Britton CL, Amedola A (2014) MOON Knee Group. Anterior cruciate ligament tunnel placement. J Knee Surg 27:309–317
Forsythe B, Kopf S, Wong AK, Martins CA, Anderst W, Tashman S, Fu FH (2010) The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am 92:1418–1426
Kim JG, Chang MH, Lim HC, Bae JH, Ahn JH, Wang JH (2013) Computed tomography analysis of the femoral tunnel position and aperture shape of transportal and outside-in ACL reconstruction: do different anatomic reconstruction techniques create similar femoral tunnels? Am J Sports Med 41:2512–2520
Lorenz S, Elser F, Mitterer M, Obst T, Imhoff AB (2009) Radiologic evaluation of the insertion sites of the 2 functional bundles of the anterior cruciate ligament using 3-dimensional computed tomography. Am J Sports Med 37:2368–2376
Luites JWH, Verdonschot N (2017) Radiographic positions of femoral ACL, AM and PL centres: accuracy of guidelines based on the lateral quadrant method. Knee Surg Sports Traumatol Arthrosc 25:2321–2329
Hart A, Sivakumaran T, Burman M, Powell T, Martineau PA (2018) A prospective evaluation of femoral tunnel placement for anatomical anterior cruciate ligament reconstruction using 3-dimensional magnetic resonance imaging. Am J Sports Med 46:192–199
Logan JS, Elliot RR, Wilson AJ (2012) TransLateral ACL reconstruction: a technique for anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20:1289–1292
Tompkins M, Milewski MD, Brockmeier SF, Gaskin CM, Hart JM, Miller MD (2012) Anatomic femoral tunnel drilling in anterior cruciate ligament reconstruction: use of an accessory medial portal versus traditional transtibial drilling. Am J Sports Med 40:1313–1321
Cohen SB, Fu FH (2007) Three-portal technique for anterior cruciate ligament reconstruction: use of a central medial portal. Arthroscopy 23:325.e1–325.e5
Luthringer TA, Blackmore SA, Singh BC, Strauss EJ (2016) The learning curve associated with anteromedial portal drilling in ACL reconstruction. Phys Sportsmed 44:141–147
Hohmann E, Bryant A, Tetsworth K (2010) Tunnel positioning in anterior cruciate ligament reconstruction: how long is the learning curve? Knee Surg Sports Traumatol Arthrosc 18:1576–1582
Acknowledgements
The authors acknowledge the support of the institutional research and development team in trial design and coordination.
Funding
No external funding or financial support was provided for the work done.
Author information
Authors and Affiliations
Contributions
JDK performed the analysis of results and statistical testing, and prepared and edited the manuscript. JDK also performed the literature review and review board submission required. KW, EAG and SVH ran the study, ensuring completion of surgery, imaging and follow-up. ADS was involved in the statistical analysis of the results and the production of the results and figures for the manuscript. RA performed all of the image manipulation and measurement required on the three-dimensional images. PJS and VIM conceived the study and performed all of the surgery. All authors were involved in the editing and submission of the manuscript (including approval of the final draft).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical review board approval was received prior to study commencement (South West – Cornwall & Plymouth Research Ethics Committee, ref. 16/SW/0080). Informed consent for both entry into the trial and the extra imaging required was gained via consultation and a written information pack.
Consent for publication
Although no identifying information is included, all participants consented to the use of their data for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kosy, J.D., Walmsley, K., Sharma, A.D. et al. A comparison of femoral tunnel placement in ACL reconstruction using a 70° arthroscope through the anterolateral portal versus a 30° arthroscope through the anteromedial portal: a pilot 3D-CT study. Knee Surg & Relat Res 32, 17 (2020). https://doi.org/10.1186/s43019-020-00037-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43019-020-00037-4