Abstract
Background
It has been noticed that failure of composite resin restorations can be attributed to either of the two following causes: fracture or secondary caries. For that reason, it is mandatory to formulate a restorative material with antibacterial effect. An octenidine dihydrochloride (OCT) has been assessed as an alternative to antimicrobial material, such as chlorhexidine due to their higher microbicidal effect and less cytotoxicity.
Objective
Current study aimed to add different concentrations of octenidine dihydrochloride into experimental flowable resin composite and evaluate its antibacterial activity over different periods of time to provide the manufacturers with more precise information.
Methods
A flowable resin composite material mix was formulated. Octenidine dihydrochloride antibacterial material was then added separately to the formulated mix at 1% wt. and 1.5% wt. concentration, respectively. Antibacterial activity was assessed against Streptococcus mutans using agar diffusion test and compared to a commercial resin composite.
Results
It showed that by increasing the percentage of incorporated octenidine dihydrochloride (1% and 1.5%), respectively, the antibacterial efficacy against the Streptococcus mutans increased. Results of this study also showed the time had a significant decrease in the antibacterial effect.
Conclusions
It can be concluded that by the incorporation of octenidine dihydrochloride (1% and 1.5%), respectively, the antibacterial efficacy against the Streptococcus mutans increased. Time had a significant decrease in the antibacterial effect of OCT.
Similar content being viewed by others
Background
Dental caries is a common oral disease coming from pathogenic bacteria that causes dental hard tissues damage. The different treatment modalities of dental caries can include removal of decayed dental tissues and restoring them with various types of restorations, such as metal alloys, resin composites, and ceramics (Saiprasert et al. 2023).
The scientific advances in restorative dental materials, have made resin composites one of the most used materials worldwide for different classes of restorations. Mechanical and chemical properties of resin composites can be altered to suit a wider range of uses by altering several factors (AlSahafi et al. 2022). Flowable composite resins with improved mechanical and chemical characteristics have been widely used in the clinical practice. These resin composites having less inorganic fillers and a higher percentage of resinous components are high flow materials that aid in preserving the seal of the restoration’s margins. However, their low elastic modulus and minimal stress contraction are challenged during stress increase (Harp et al. 2022).
As dental caries is a transmissible infection initiated by cariogenic microorganisms, trials to make an antibacterial restorative material turn out to be an appealing issue in dental biomaterials.
Recently, octenidine dihydrochloride has been used as a mouthwash and as an antiseptic agent to treat wounds and skin burns. Prior research has demonstrated that octenidine dihydrochloride and chlorhexidine were equally effective at combating microorganisms causing dental plaque. Octenidine dihydrochloride has been examined as replacements to chlorhexidine due to their higher antimicrobial effect and less toxic effects (Liang et al. 2020).
This study was conducted to evaluate the antibacterial effect of various concentrations of octenidine dihydrochloride across varying time periods in an experimental flowable resin composite. The null hypothesis is that the addition of octenidine dihydrochloride (OCT) to the experimental composite resin had the capability to increase the antibacterial efficacy against the Streptococcus mutans.
Methods
The materials chemical name, description, batch number, and their manufacturers are listed in Table 1.
Streptococcus mutans was provided from the European Culture Collection Center (Belgium, Europe). The Herculite Ultra Flowable, by Kerr, was used as the commercially available flowable resin composite.
Resin matrix preparation
The flowable resin matrix was formulated by the following:
-
Blending Bis-phenol A-glycidyl Methacrylate (Bis-GMA) with Tri-ethylene Glycol Di-methacrylate (TEGDMA) in 70:30 ratio by weight % (Niedźwiedź et al. 2023).
-
The photo-initiator powder system was prepared by adding camphorquinone powder: ethyl 4-di-methyl-amino-benzoate powder in a ratio 1:1.
-
The powder of prepared photo-initiator was gently added to the prepared resin matrix in a dark container.
-
The prepared mixture of resin matrix and powder was stirred steadily on a magnetic stirrer by a small magnet for 2 h to secure homogenous mixture and thorough monomers dissolution (Fidalgo-Pereira et al. 2022).
Drops of acetic acid were added to ethanol solution in a small beaker to decrease the pH to 3 or 4 by using a pH meter for monitoring (Jenway, 3505, UK). A 3% by wt of tri-methoxy-silane was applied to the adjusted ethanol solution and then blended in a beaker using a magnetic stirrer for one hour (Moharam et al. 2018).
Sintering of the silicon di-oxide nanopowder was done at 1300 °C for 20 min using a sintering electric furnace (TEGRA SPEED, Teknik Dental, Turkey). The sintered particles aggregated as white clusters and were ground manually by using mortar and pestle. The ground particles were then sieved using a stainless-steel sieve (400 mesh) (Moharam et al. 2022).
Sintered silicone dioxide nanoparticles were added in the formulated silane coupling agent and blended for two hours by stirring with the magnetic stirrer. The prepared solution was centrifuged at temperature of 25 °C for 30 min, with 6000 rpm speed using a centrifugal machine (Laborzentrifugen GmbH Sigma 3-16-KL, Germany). The nanosilica particles were precipitated at the tube bottom after centrifugation. The final precipitate was rinsed off using ethanol, and then mixing was performed in a vortex mixer (Stuart, SA7, UK) at speed 1800 rpm to secure homogenization of the mix. Centrifugation was performed for the mixture for 5 min by the apparatus of centrifugation. This procedure was done for three times, and the extra ethanol was rinsed off (Meshram et al. 2019).
The final precipitate was then left to dry in a Petri dish using an drying furnace (FD 23, 20L, BINDER, Germany). The operating temperature was continually kept for 60 min at 105 °C (Souza et al. 2023). The Petri dish was then placed in a desiccator for 10 min after removal from the furnace and sealed with foil.
The octenidine dihydrochloride particles were added to the previously silanized silica fillers at concentration of 1% wt. and 1.5% wt to prepare group 3 and 4, respectively. These concentrations were chosen according to a pilot study that was observed prior to the current test.
The prepared mixture of salinized silica nanofillers together with the antibacterial particles was added to the formulated resin matrix. The un-cured resin composite was then placed in a dark tinted bottle and kept in a dark place over-night.
Four groups were tested as follows:
-
Group 1 commercial resin composite.
-
Group 2 experimental resin composite without octenidine dihydrochloride.
-
Group 3 experimental resin composite containing octenidine dihydrochloride 1%
-
Group 4 experimental resin composite containing octenidine dihydrochloride 1.5%
Evaluation of the antibacterial activity using agar disc diffusion test
Resin composite discs specimens were prepared by packing the uncured mix into a sterile Teflon mold with dimensions (5mm X 5mm) (Abou ElReash et al. 2019). Then, in accordance with the manufacturer's instructions, the uncured mix was light cured using a light cure unit with a tip diameter of 10 mm (Premium Plus light cure C02-D, Premium Plus-UK, England) with an irradiance of 2500 mW cm2 on normal mode for 20 s via each side of the mold. After removing the specimens from the molds, any excess cured resin was removed and cut using silicon carbide paper grit with a size of P800 μm.
Streptococcus mutans, a facultatively anaerobic, gram-positive bacterial strain, was used in this investigation. Giza, Egypt's Food Technology Research Institute, donated the Streptococcus mutans. Streptococcus mutans has the American Type Culture Collection (ATCC) number 35668.
In order to achieve a high growth concentration of roughly 106 CFU/mL, the antibacterial test was carried out in a sterilized brain–heart infusion (B-H-I) utilizing inoculation loop broth that was incubated for 24 h at 37 °C under anaerobic conditions (Hernandes et al. 2014).
Colonies were selected the day before the test and grown in 5 ml broth medium at 35–37 °C for 16–18 h. One hundred microliters of the diluted culture was distributed uniformly across the media plate. With a diameter of 5 mm and a depth of 3 mm, a total of 16 bacterial wells were produced and divided into 16 plates containing bacterial strains.
After polymerization, specimens of resin composite discs were inserted into the bacterial wells using a pair of tweezers that had been flame-sterilized. In order to facilitate the growth of bacterial cultures, plates were incubated for 24 h at 37 °C in an incubator (Fisher Scientific isotemp incubator model 655d, USA).
Positive results were scored when a zone of inhibition was observed around the specimens. The inhibitory zone was measured by the shortest distance in (mm) from the specimen outer margin to the microbial growth initial point. The measurements were taken at 30, 60, and 90 days.
Results
At 30 days, the highest mean inhibition zones were recorded in groups 3 and 4, while no inhibition zones were recorded in groups 1 and 2. Among the four tested groups, ANOVA test showed a significant difference (Table 2).
At 60 and 90 days, the highest mean inhibition zones were recorded in group 3, followed by group 4, while no inhibition zones were recorded in groups 1 and 2. Among the four tested groups, ANOVA test showed a significant difference (Table 2). There was no significant difference between tested groups 3and 4 using Tukey’s post hoc test (Table 3).
Comparison at different times within the same group
Groups 1 and 2 showed no inhibition zones throughout the study and recorded a constant value (0) as shown in (Table 4).
In Group 3 the mean inhibition zones measurements increased significantly at 30 days and then decreased significantly at 60 and 90 days. The time effect on group 3 was significant, as shown in (Table 4).
In Group 4 the mean inhibition zone measurements increased significantly at 30 days; afterward, time decreased significantly at 60 days, followed by another significant decrease at 90 days. The time effect on group 4 was significant (Table 4).
Discussion
Secondary caries can be described as a lesion occurring at the margins of an existing restoration, which is caused mainly by Streptococcus mutans bacteria.
A simple method to provide materials for dental restorations with bactericidal activity, is by adding an antibacterial additive to the material. These additives can subsequently be liberated in an aqueous environment, to eliminate the damaging bacteria.
Different antibacterial agents such as triclosan, benzalkonium chloride, silver particles, antibacterial pre-polymerized resin fillers, and chlorhexidine have been introduced in both commercial and experimental dental resin composites (Ezzeldin et al. 2019).
However, studies showed that incorporating antibacterial additives directly into commercial resin composites showed minimal antibacterial activity after curing, as the amount leached out was close to the minimal inhibitory concentration needed for bacterial inhibition. Consequently, to obtain an antibacterial composite resin, the additive might be either dissolved in the monomers or mixed with the inorganic fillers. Therefore, this study was aimed to add a recent antimicrobial particles (octenidine dihydrochloride) to an experimental resin composite (Chum et al. 2019).
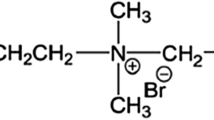
Octenidine dihydrochloride (OCT) is an antibacterial material currently utilized as a mouth wash and for managing skin burns. OCT is a member of the bipyridines, having two cationic functional parts for each molecule, and displaying wide anti-microbial effect on different types of bacteria, fungi, and many viral types (Uzer Celik et al. 2016).
The agar diffusion test was used to assess the antibacterial effect in this study, as it is a broadly applied in vitro way for evaluation of the antibacterial effect of dental restorative materials. The benefit of this way is that the anti-microbial out turn of drugs can be discovered by stimulating the microbial segregates with anti-microbial prepared discs with no modification in the biochemical drug characteristics. It also gives chance for direct comparisons of restorative materials against the tested microorganisms, demonstrating the material which has the more capability to remove bacteria in the local micro-environment (Esenlik et al. 2016).
In the agar diffusion method, the growth inhibition zones are related to the toxic effect of the material applied against the bacteria besides the diffusion ability of the material in the culture media (Stencel et al. 2018).
Results of the current study revealed that by incorporation of octenidine dihydrochloride (1% and 1.5%), respectively, the antibacterial efficacy against Streptococcus mutans increased; this was in accordance with (Uzer Celik et al. 2016) who evaluated the effect of several antimicrobial agents in vitro such as (CHX) chlorhexidine di-gluconate, (PHBM) polyhexamethylene biguanide, and (OCT) octenidine dihydrochloride on pathogenic microorganisms by adding their (M-I-C) minimum inhibitory concentration and (M-B-C) minimum bactericidal concentration. They stated that OCT had an effective antimicrobial effect against the tested bacteria. This can be explained by the fact that octenidine dihydrochloride interferes with cellular walls and membranes which means that it exhibits both fungicidal and bactericidal outcomes. It also interacts with cell wall polysaccharides of microorganisms, bombards the enzymatic structures nearby, terminates cell biological function, and results in cytoplasmic membrane leakage.
Furthermore, OCT appears to be highly effective by means of prolonged antiadhesive activity on bacteria, which might be the cause of its antibacterial activity. This was supported by Uzer Celik et al. (2016) and Stencel et al. (2018).
Additionally, the stated results of this research can be explained by the fact that OCT is a member of the bipyridines, having two cationic functional parts for each molecule, and displaying wide antimicrobial properties on different microorganisms (Malhotra et al. 2016).
Results showed that time had a significant decrease in the antibacterial effect of OCT. In group 4, the antibacterial activity was 2.08 at 30 days. At 60 days the antibacterial activity was 1.6, while at 90 days it was 0.61. Similarly, in group 3, at 30 days the antibacterial activity was 2.08; then, it decreased to 1.7 at 60 days and further decreased to 1.35 at 90 days.
The decline in the antibacterial effect by time can be due to a drop in the rate of release or a drop in the amount of residual material. This was agreed with (Joon et al. 2020).
The component release seems larger at first and then decreases by time; the reduction in the release rate shows that the outer layer constituents are dissolved or washed-out inside the water. Moreover, the constituents inside the resin are discharged with difficulty since the resin constituents restrain such movements. Commonly, the curative agents of dental biomaterials when discharged display a reduction in the rate of release. The water inside the mouth penetrates the resin matrix; the agent in the adhesive dissolves and scatters in smaller concentrations. By time, the agent is released and separated from a deeper layer of the matrix, which means that diffusion time to the exterior environment increases, while the release rate decreases (Joon et al. 2020).
Within the constraints of this study, octenidine dihydrochloride was found to be beneficial when added to flowable resin composites. Additional researches are suggested to demonstrate its impact on hardness, radio-opacity, color stability, and working time. Research on the antibacterial effect of octenidine dihydrochloride on a larger variety of cariogenic bacterial species both in vitro and in vivo is also advised. To be more precise, in order to replicate the release of these antimicrobials in the oral cavity, future studies should design their experiments more carefully, considering teeth and restorations as substrates for biofilm formation under a dynamic and constant flow of saliva.
Conclusions
The addition of octenidine dihydrochloride (OCT) to the experimental composite resin had the capability to increase the antibacterial efficacy against the Streptococcus mutans. Incorporation of OCT with 1% and 1.5% showed the same significant antibacterial effect at 30 and 60 days. However, at 90 days the 1% (OCT) showed better results than the 1.5%. These results were radically higher upon comparison with the commercially available resin composite. Time had a significant effect on reduction of the OCT antibacterial effect.
Availability of data and materials
Data are available under reasoning demand.
Abbreviations
- OCT:
-
Octenidine dihydrochloride
- Bis-GMA:
-
Bis-phenol-A glycerolatedimethacrylate
- TEGDMA:
-
Tri-ethylene glycol di-methacrylate
References
AbouElReash A, Hamama H, Eldars W, Lingwei G, El-Din AM, Xiaoli X (2019) Antimicrobial activity and pH measurement of calcium silicate cements versus new bioactive resin composite restorative material. BMC Oral Health 19(1):235
AlSahafi R, Wang X, Mitwalli H, Alhussein A, Balhaddad AA, Melo MAS, Oates TW, Sun J, Xu HK, Weir MD (2022) Novel antibacterial low-shrinkage-stress resin-based cement. Dent Mater 38(11):1689–1702
Chum JD, Lim DJZ, Sheriff SO, Pulikkotil SJ, Suresh A, Davamani F (2019) In vitro evaluation of octenidine as an antimicrobial agent against Staphylococcus epidermidis in disinfecting the root canal system. Restor Dent Endod 44(1):1–7
Esenlik E, UzerÇelik E, Bolat E (2016) Efficacy of a casein phosphopeptide amorphous calcium phosphate (CPP-ACP) paste in preventing white spot lesions in patients with fixed orthodontic appliances: a prospective clinical trial. Eur J Paediatr Dent 17(4):274–280
Ezzeldin N, Elshishtawy H, El Borady O, Mohamed M (2019) Comparative evaluation of the antibacterial activity of glass ionomer restoration incorporated with different metal oxides nanoparticles on oral Streptococcus mutans. Egy Dent J 65(3213):3220
Fidalgo-Pereira R, Carpio D, Torres O, Carvalho O, Silva F, Henriques B, Özcan M, Souza JCM (2022) The influence of inorganic fillers on the light transmission through resin-matrix composites during the light-curing procedure: an integrative review. Clin Oral Investig 26(9):5575–5594
Harp YS, Montaser MA, Zaghloul NM (2022) Flowable fiber-reinforced versus flowable bulk-fill resin composites: Degree of conversion and microtensile bond strength to dentin in high C-factor cavities. J Esthet Restor Dent 34(4):699–706
Hernandes NM, Catelan A, Soares GP, Ambrosano GM, Lima DA, Marchi GM, Martins LR, Aguiar FH (2014) Influence of flowable composite and restorative technique on microleakage of class II restorations. J Investig Clin Dent 5(4):283–288
Joon A, Khetarpal A, Dahiya S (2020) Comparitive evaluation of antimicrobial efficacy of 0.1% octenidine dihydrochloride, 2% chlorhexidine and 2% chitosan against E. faecalis within the dentinal tubules. IP Indian J Conserv Endodont 5(4):192–199
Liang J, Liu F, Zou J, Xu HHK, Han Q, Wang Z, Li B, Yang B, Ren B, Li M, Peng X, Li J, Zhang S, Zhou X, Cheng L (2020) pH-Responsive antibacterial resin adhesives for secondary caries inhibition. J Dent Res 99(12):1368–1376
Malhotra A, Bali A, Bareja R (2016) Anti-bacterial efficacy of Octenidine as a mouthwash. Int J Pharma Sci Res 7(1):340
Meshram P, Meshram V, Palve D, Patil S, Gade V, Raut A (2019) Comparative evaluation of microleakage around Class V cavities restored with alkasite restorative material with and without bonding agent and flowable composite resin: An in vitro study. Indian J Dent Res 30(3):403–407
Moharam LM, Salem HN, Elgamily HM (2018) The effect of incorporating different concentrations of chlorhexidine digluconate on the degree of conversion of an experimental adhesive resin. J Clin Exp Dent 10(4):e371–e377
Moharam LM, Salem HN, Hassan SN (2022) Effect of açai berry extract application on the bond strength to the bleached enamel using an experimental etch-and-rinse adhesive. J Clin Exp Dent 14(12):e1015–e1023
Niedźwiedź MJ, Demirci G, Kantor-Malujdy N, El Fray M (2023) Influence of photoinitiator type and curing conditions on the photocuring of soft polymer network. Materials (Basel) 16(23):7348
Saiprasert P, Tansakul C, Pikulngam A, Promphet P, Naorungroj S, Ratanasathien S, Aksornmuang J, Talungchit S (2023) Novel hydrolytic resistant antibacterial monomers for dental resin adhesive. J Dent 135:104597
Souza LVS, Pavanello L, Picolo MZD, Kury M, Matos ICRT, Cogo-Müller K, Esteban Florez FL, Cavalli V (2023) Mechanical and antibacterial properties of an experimental flowable composite containing Nb2O5and NF_TiO2 nanoparticles. J Mech Behav Biomed Mater 143:105919
Stencel R, Kasperski J, Pakieła W, Mertas A, Bobela E, Barszczewska-Rybarek I, Chladek G (2018) Properties of experimental dental composites containing antibacterial silver-releasing filler. Materials (Basel) 11(6):1031
UzerCelik E, Tunac AT, Ates M, Sen BH (2016) Antimicrobial activity of different disinfectants against cariogenic microorganisms. Braz Oral Res 30(1):e125
Acknowledgements
The authors extend their sincere gratitude to all of their teachers and colleagues at the National Research Center.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MM completed the practical work, gathered the information, and made significant contributions to the manuscript's composition. TS wrote the text, completed the statistical analysis, and produced the final edit. The final writing, editing, plagiarism check, and submission were completed by HNS. Before submitting, each author has read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mansour, M., Salah, T. & Salem, H.N. The effect of octenidine dihydrochloride on the antibacterial activity of a formulated resin composite: an in vitro study. Bull Natl Res Cent 48, 46 (2024). https://doi.org/10.1186/s42269-024-01201-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-024-01201-6