Abstract
Background
To test the antimicrobial potential of clove essential oil that has been less investigated on antimicrobial-resistant organisms (extended-spectrum β-lactamase-ESBL-producing Escherichia coli), we collected 135 ESBL-producing Escherichia coli strains given that E. coli is the major organism increasingly isolated as a cause of complicated urinary and gastrointestinal tract infections, which remains an important cause of therapy failure with antibiotics for the medical sector. Then, in this study, we evaluated the relationship between the antibacterial potential activity of Syzygium aromaticum essential oil (EOSA) and the expression of antibiotic-resistant genes (SHV-2, TEM-20) in plasmidic DNA on ESBL-producing E. coli using RT-PCR technique.
Results
EOSA was obtained by hydrodistillation. Using Kirby-Baüer method, we found that EOSA presented a smaller media (mean = 15.59 mm) in comparison with chloramphenicol (mean = 17.73 mm). Thus, there were significant differences (p < 0.0001). Furthermore, EOSA had an antibacterial activity, particularly on ECB132 (MIC: 10.0 mg/mL and MBC: 80.0 mg/mL), and a bacteriostatic effect by bactericidal kinetic. We found that the expression of antibiotic-resistant gene blaTEM-20 was 23.52% (4/17 strains) and no expression of blaSHV-2. EOSA presented such as majority compounds (eugenol, caryophyllene) using the GC–MS technique.
Conclusions
Plant essential oils and their active ingredients have potentially high bioactivity against a different target (membranes, cytoplasm, genetic material). In this research, EOSA might become an important adjuvant against urinary and gastrointestinal diseases caused by ESBL-producing E. coli.
Similar content being viewed by others
Background
The importance of extended-spectrum β-lactamase-producing Enterobacteriaceae (especially, E. coli and K. pneumoniae) lies in the increased human antimicrobial-resistant organisms (AROs). Additionally, they arise as main causes of urinary tract and bloodstream infections in both developed and developing countries (Pitout 2012; Domaracký et al. 2007; Pana and Zaoutis 2018).
The extended-spectrum beta-lactamases (ESBLs) are classified as a group of enzymes that cause resistance to the oxyiminocephalosporins (i.e., cefotaxime, ceftazidime, cefepime) and the monobactams (i.e., aztreonam). However, they do not produce resistance to the cephamycins (i.e., cefoxitin, cefotetan) nor to the carbapenems (i.e., imipenem, meropenem, doripenem, ertapenem) (Pitout and Laupland 2008). The majority of ESBLs are classified by Ambler, where the class A includes the SHV or TEM types. These types have evolved from parent enzymes such as TEM-1, TEM-2 and SHV-1 (Sawa et al. 2020).
Additionally, a higher prevalence of AROs is troublesome for the medical sector (due to complications such as chemotherapy, surgery) because infections increase patient mortality and morbidity. These issues remain as an important cause of therapy failure with antibiotics and have serious infection-control-related consequences according to the World Health Organization (WHO) (Seale et al. 2017).
The latter suggests other therapeutic options, mainly of natural origin (i.e., mineral, vegetable and animal) that were the main sources of active compounds; however, with the development of organic chemistry, the preference for synthetic products were above those of natural origin (Wright 2019). In this instance, out of the 252 substances that are considered basic and essential, only 11% are of plant origin (World Health Organisation 2001, 2013).
Clove has gained much attention among other spices, due to its antimicrobial and antioxidant activities (Batiha et al. 2020; Shan et al. 2005; Shrivastav et al. 2019) to help alleviating toothache, inflammation and gastrointestinal disorders (El-Shouny et al. 2020; Santin et al. 2011; Oluwasina et al. 2019). Some studies mentioned the antibacterial potential activity of clove. The first study refers that clove's phenolic extract (Syzygium aromaticum) has antibacterial activities against the growth of S. aureus and E. coli in a concentration range of 50–100 μg/mL (El-Maati et al. 2016). The second study mentions that Syzygium aromaticum seeds contain eugenol (component with antimicrobial activity) with a minimum inhibitory concentration (MIC) of 0.06 mg/mL, which affect the membrane permeability, and increase oxidative stress enzymes such as catalase and superoxide dismutase (Ajiboye et al. 2016).
The synergistic activity of essential oils (EOs) in combination with antibiotics has beneficial potential that allows to minimize the side effects (Gündüz et al. 2009; Langeveld et al. 2014). This interaction has the potential pro to reduce the concentration of EOs needed to obtain an effective antimicrobial activity and minimize the negative sensory impact (Nazer et al. 2005; Vuuren et al. 2009).
Recent studies demonstrate the antibacterial activity of clove on multidrug-resistant strains. However, multidrug-resistant strains are mostly confirmed with phenotypic screening (Shrivastav et al. 2019; Faujdar et al. 2020) but barely using RT-PCR technique. In this study, we evaluate the relationship between the antibacterial potential activity of EOSA and the expression of antibiotic-resistant genes (SHV-2, TEM-20) in plasmidic DNA on ESBL-producing E. coli using RT-PCR technique.
Methods
Plant material
Syzygium aromaticum L. seeds were bought from a grocery store located in the municipality of El Oro de Hidalgo, State of Mexico, with geographical coordinates 19° 48′03 "N 100° 07′53" W in November–December 2017. The botanical authentication of the specimen was performed by M.D. Maria E. Lopez-Villafranco, curator at the IZTA Herbarium, in FES Iztacala of the Autonomous University of Mexico. The specimen was properly labeled with its voucher IZTA 2818.
Preparation of essential oil of Syzygium aromaticum L. (EOSA)
Dried flower buds of S. aromaticum (236.2 g) were ground with mortar and stood in distilled water approximately for 12 h. The obtention of essential oil was performed using hydrodistillation method (Dominguez 1985). Furthermore, EOSA were dissolved in Müeller Hinton Broth (BD Bioxon) to evaluate antibacterial activity.
Microorganism culture and maintenance
Collection and maintenance
In total, 135 ESBL-producing E. coli strains were collected from clinical isolates and identified by culture media, biochemical tests and antibiograms. These strains were identified as ESBL by the automated equipment VITEK ® 2 Compact (BioMerieux, Germany) in the Bacteriology Laboratory of a Health Center in Mexico. ESBL-producing E. coli strains were sampled from July to December 2017, and they were kept in Nutritious Agar (Bioxon, State of Mexico, Mexico) and refrigeration under 4° C for their conservation.
Criteria selection of strains
During the first selection, the total of samples (n = 135) were evaluated using Kirby-Baüer method (i.e., inhibition halos); the samples were analyzed using the statistically significant difference between strains with an inhibition halo greater or equal than 21 mm and control (chloramphenicol), were selected by minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) evaluations and using antibiotic-resistant genes by RT-PCR technique. The last selection considered the strains with expression of antibiotic-resistant genes, and the higher concentration of EOSA by CMB was selected by bactericidal kinetic.
Pre-treatment for antibacterial activity
The bacterial inoculum of ESBL-producing E. coli strains was incubated in 10 mL of Müeller Hinton Broth overnight at 37 °C. The colonies were adjusted to turbidity comparable to the McFarland standard (1.5 × 108 CFU/mL) using disk diffusion agar method by the Kirby-Baüer (Vanden Berghe et al. 1991; CLSI 2015).
Evaluation of the antibacterial activity of EOSA
To evaluate the antibacterial potential of EOSA, disks of 5 mm diameter (Whatman No. 5) were impregnated with 10 μL of EOSA and 25 μg of chloramphenicol. This component was used as positive control above the microbial pre-treatment suspensions on plates of Müeller Hinton Agar plates (BD Bioxon), which were previously striated using Kirby-Baüer method and methods of Martinez-Elizalde et al. (Vanden Berghe et al. 1991; CLSI 2015; Martinez-Elizalde et al. 2015).
The minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) were estimated using the broth dilution method. The assay tubes of pre-treatment microbial suspension were transferred to fresh tubes in concentration of 105 CFU/mL on Müeller Hinton Broth with the concentrations of EOSA at levels between 0.875 and 80 mg/mL. The MIC values were defined as the lowest concentration that prevented visible bacterial growth overnight at 37 °C.
The bactericidal kinetic assay was performed using the appropriate concentrations of EOSA (corresponding to MIC50, MIC and MBC) (Lennette et al. 1981).
Bacteria DNA extraction
The DNA extraction was performed by the alkaline lysis method (Birnboim 1983). The bacteria grew previously in Luria broth overnight, and then 3 mL of bacteria was centrifuged in 2 fractions at 9500 rad/s for 5 min. For this method, three solutions were used: 1) solution I (50 mM glucose, 25 mM Tris–Cl (pH 8.0), 10 mM EDTA (pH 8.0); 2) solution II (0.2 N NaOH, 1% SDS prepared on the same day and added from concentrated solution); and 3) solution III (60 mL of 5 M sodium acetate, 11.5 mL of glacial acetic acid, 28.5 mL of H2O).
The process of DNA extraction is described below: The first step consisted to resuspend the bacterial bottom in 100 μL of solution I. Secondly, 200 μL of solution II was added to the mixing of previous step by inversion and incubated on ice for 3 min. In the last step, 150 μL of solution III was added, followed by an incubation on ice for 3 min, and a centrifugation at 9500 rad/s for 5 min. The supernatant was removed in a fresh tube, and 420 μL of chloroform-phenol-isoamyl alcohol was added, mixing both by inversion. Then, the mix was centrifuged at 9500 rad/s for 5 min. The aqueous phase (upper) was separated in a new tube, and 1 mL of absolute ethanol was added. The supernatant was discarded, and the pellet was washed with cold 70% ethanol, allowing to dry at room temperature for 5 min and resuspending in 50 μL of sterile deionized H2O.
Detection of bacteria resistance genes
A RT-PCR was done to detect antibiotic-resistant genes, and 5 μL of the supernatant obtained in the extraction of DNA was used with two pairs of oligonucleotides (IDT): blaTEM-20 (F: GAT AAC ACT GCG GCC AAC TT and R: TTG CCG GGA AGC TAG AGT AA) and blaSHV-2 (F: CTT TCC CAT GAT GAG CAC CT and R: CGC TGT TAT CGC TCA TGG TA) in a concentration of 12.5 uM. The RT-PCRs (Techne-TC-512) were evaluated using the kit of Master Mix PCR M7502 (Promega) (Araujo Díaz and Salas Asencios 2008).
For the TEM-20 gene, the PCR steps are described next: a denaturation of 5 min at 97 °C, 30 cycles of 1 min at 94 °C, followed by a banding during 1 min at 56 °C (except for the blaSHV gene that requires 54 °C for banding). After that, an extension for 1 min at 72 °C is followed by 10 min at 72 °C of final extension. The PCR products were visualized on 1.5% agarose gels (Merck, Germany), in 1X TEB with ethidium bromide staining. Through this process, a 5X colorless molecular weight marker buffer of 100–2000 bp DNA was used (Bioline, USA) (Araujo Díaz and Salas Asencios 2008).
Analysis of the Chemical Composition by GC–MS
Then, 1μL of EOSA was injected into the equipment. A 6850 Network GC System chromatograph from Agilent Technologies coupled to a 5975C VL MSD mass spectrometer with a triple-axis detector, of the same brand, equipped with an RTX capillary column 30 m long, 0.25 mm internal diameter and 0.25 μm thick (dimethylpolysiloxane (95%) and phenyl polysiloxane (5%)).
The injection mode used was a Split, with radius 80:1 and running flow 37 cm/seg. The temperature of the oven was programmed as follows: initial temperature of 70 °C for 2 min, after which, it was increased at a rate of 8 °C/min until reaching 270 °C and then at 10 °C/min during 6 min. The total time was 75 min, and the higher temperature used was 290 °C. The mass spectra were obtained by electronic impact with ionization energy of 70 electron volts (eV) and detected in a mass range from 35 to 600 m/z. Helium was used as the entraining gas, while the identification of individual components in EOSA was made by GC–MS.
Separated compounds were identified using the chemical library and the database of the NIST library and the PubMed Compound of the National Center of Biotechnology Information (NCBI) (NIST 2016; US National Library of Medicine 2017).
Statistical analysis
All experiments were done three times; however, inhibition halos experiments were done under a completely randomized design, and they were expressed as the mean ± standard deviation (mm). Inhibition halos data were studied using the factorial analysis of variance (ANOVA) with a Tukey–Kramer multiple comparison test (P < 0.05) using the R-project Core-Team (2017).
Results
EOSA had a yield of 6.35% and a density of 1.16 g / mL.
Evaluation of the antibacterial activity of EOSA
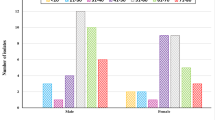
Using Kirby-Baüer method, we found that EOSA presented a smaller media (mean = 15.59 mm), in comparison with chloramphenicol (mean = 17.73 mm). Thus, there were significant differences (F0.05,1,134 = 371.02, p < 0.0001). Furthermore, we found 18 samples with statistically significant differences. They showed an inhibition halo similar to control (chloramphenicol) that were selected by MIC, MBC evaluation and expression of antibiotic-resistant genes by RT-PCR technique (Table 1).
By dilution method, we found that strain 132 had the lowest MIC and the higher MBC (10.0 mg/mL and 80.0 mg/mL), respectively. Then, this strain was selected by bactericidal kinetic, and we found that EOSA had bacteriostatic effect (Fig. 1).
Bactericidal kinetic of ESBL-E. coli (ECB132) exposed to EOSA. The concentrations were: 1/2 MIC: 5 mg/mL; MIC: 10 mg/mL; MBC: 80 mg/mL. CFU: colony-forming unit; hours (h); control (chloramphenicol); MIC: minimum inhibitory concentration; MBC: minimum bactericidal concentration. For kinetic curve the times measured were 0, 2, 4, 6, 8, 12 h with a decrease of bacteria except for MBC at 6 h until 24 h an increasing of bacteria survival in comparison with control
The concentrations were: 1/2 MIC: 5 mg/mL; MIC: 10 mg/mL; MBC: 80 mg/mL. CFU: colony-forming unit; hours (h); control (chloramphenicol); MIC: minimum inhibitory concentration; MBC: minimum bactericidal concentration. For kinetic curve the times measured were 0, 2, 4, 6, 8, 12 h with a decrease of bacteria except for MBC at 6 h until 24 h an increasing of bacteria survival in comparison with control.
Detection of bacteria resistance genes
Using plasmid DNA extraction and RT-PCR technique, we found that ESBL-E. coli strains had the expression of antibiotic-resistant gene blaTEM-20 in a 23.52% (4/17 strains) and no expression of blaSHV-2 (Table 2).
Analysis of the chemical composition by GC–MS
GC–MS analysis revealed the presence of two majority terpene compounds (eugenol and caryophyllene) in EOSA (Fig. 2).
The majority compounds of EOSA are eugenol (77.322%, Tr = 8.728) and caryophyllene (16.77% Tr = 9.305).
Discussion
We found that EOSA had an antibacterial activity on ESBL-producing E. coli; particularly, ECB132 had a bacteriostatic effect until 12 h. In the same way, this antibacterial activity of S. aromaticum (i.e., ethanolic, methanolic extracts) has been observed on strains ATCC such as E. coli, P. aeruginosa, S. aureus (Ajiboye et al. 2016) and a bacteriostatic effect on K. pnemoniae (Lawal 2019). Therefore, the clove mechanism of action has been described altering the permeability of the membrane, causing oxidative stress enzymes (i.e., catalase and superoxide dismutase) (Ajiboye et al. 2016). For instance, we believe that of a single dose some metabolites of S. aromaticum were gradually released over time until their completely released. Otherwise, a single dose in combination or sequential antimicrobial treatments (Paterson et al. 2016) to daily dose, could produce multidrug-resistant bacteria caused by MIC variation on the time, thus considered the antimicrobial dosing in critical change to prevent the bacterial resistance (Kim et al. 2014). Alternatively, natural products need a encapsulation (i.e., biomolecular capping in green synthesis process nanoparticles) to prevent the compounds volatilization and reduce the toxicity and concentration (Roy et al. 2019).
On the other hand, our EOSA had a yield of 6.35%. Yield difference can be influenced by the harvesting season, the geographical origin (Nana et al. 2015) and extraction method that involves the particle size of ground cloves on the yield (Guan et al. 2007).
The EOSA studied in this research contains eugenol and caryophyllene as major compounds, and these we believe that had the antimicrobial activity on ESBL-producing E. coli. Most of the earlier studies reported inhibitory potential of herbal compounds against antibiotic-resistant ATCC strains, and there are not enough studies with antibiotic resistance clinical strains and their gene expression. Similarly, the antibacterial activity of clove compounds is well known: 1) eugenol on ESBL-QR E. coli (quinolone resistant) has demonstrated a synergistic interaction with cefotaxime, and ciprofloxacin (MIC = 0.91–7.34 µg/mL), and shrinkage of cell surfaces with reduced cytoplasm among in others ESBL-QR strains (Dhara and Tripathi 2020). And 2) caryophyllene as β-caryophyllene was able to alter membrane permeability and integrity of B. cereus, leading to membrane damage and intracellular content leakage, which eventually caused cell death (MIC = 2.5% –v/v–) (Moo et al. 2020).
ESBL-producing E. coli clinical strains, evaluated in this study, had the expression of antibiotic-resistant gene blaTEM-20 in a 23.52% (4/17 strains) and no expression of blaSHV-2. In this sense, the incidence of antibiotic-resistant genes in ESBL-E. coli in the health sector is increasingly concerning, for example, 84% blaSHV and 85% blaTEM were found in a Hospital in Guatemala (Herrera García et al. 2019). Furthermore, from outpatients in Tabriz, Iran could be carriers of ESBL-E. coli with resistant genes, 2% of blaSHV and 4% of blaTEM (Dizage 2019). However, the combination between natural compounds and antibiotics (i.e., eugenol-cefotaxime) represents an important management to suppress the synthesis at transcript level in antibiotic-resistant genes (i.e., acrB) (Dhara and Tripathi 2020).
Therefore, EOSA could be a potential such as adjuvant to combat certain infections caused by multidrug-resistant bacteria (i.e., ESBL-E. coli).
Conclusions
In our study the EOSA was obtained by hydrodistillation and had an antimicrobial activity in ESBL-producing E. coli strains, particularly a bacteriostatic effect. The 23.52% of these strains expressed antimicrobial-resistant gene (blaTEM-20) in plasmid DNA until 12 h of a single dose. Therefore, EOSA could be a potential adjuvant, mainly to combat certain infections related to ESBL-producing E. coli. Then, the perspectives to the future researches could be to demonstrate and elucidate the mechanism of action for the different secondary metabolites. The latter will allow to innovate new therapeutic alternatives as adjuvants, to investigate the effect of diverse cells or microorganisms, and their possible suppression of antibiotic-resistant genes.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- AROs:
-
Antimicrobial-resistant organisms
- ATCC:
-
American Type Culture Collection
- DNA:
-
Deoxyribonucleic acid
- ECBx:
-
Number of extended-spectrum β-lactamase-producing strain isolated
- EOs:
-
Essential oils
- EOSA:
-
Syzygium aromaticum Essential oil
- ESBL:
-
Extended-spectrum β-lactamase-producing strain
- FES:
-
Facultad de Estudios Superiores
- GC–MS:
-
Gas chromatography–mass spectrometry
- IDT:
-
Integrated DNA Technologies
- MBC:
-
Minimum bactericidal concentration
- MIC:
-
Minimum inhibitory concentration
- n:
-
Total number of extended-spectrum β-lactamase-producing strain isolated for experiment
- NIST/NCBI:
-
PubMed Compound of the National Center of Biotechnology Information
- QR:
-
Quinolone resistant
- RT-PCR:
-
Reverse transcription polymerase chain
- SD:
-
Standard deviation
- SHV-2:
-
TEM-20
- arcB:
-
Antibiotic-resistant genes
- Tr:
-
Time retention
- WHO:
-
World Health Organization
References
Ajiboye TO, Mohammed AO, Bello SA, Yusuf II, Ibitoye OB, Muritala HF et al (2016) Antibacterial activity of Syzygium aromaticum seed: Studies on oxidative stress biomarkers and membrane permeability. Microb Pathog 95:208–215
Araujo Díaz J, Salas Asencios R (2008) Actividad antimicrobiana de plantas. Rev Científica del Sur
Batiha G, Alkazmi L, Wasef L, Biomolecules AB-, 2020 undefined. Syzygium aromaticum L.(Myrtaceae): Traditional uses, bioactive chemical constituents, pharmacological and toxicological activities. mdpi.com [Internet]. [cited 2020 Jun 30]; Available from: https://www.mdpi.com/2218-273X/10/2/202
Birnboim HC (1983) A rapid alkaline extraction method for the isolation of plasmid DNA. Methods Enzymol 100:243–255
CLSI (2015) M45. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria, Proposed Guideline. Guidelines CLSI
Dhara L, Tripathi A (2020) The use of eugenol in combination with cefotaxime and ciprofloxacin to combat ESBL producing quinolone resistant pathogenic Enterobacteriaceae. J Appl Microbiol
Dizage JL (2019) Study of antibiotic susceptibility pattern and frequency of extended spectrum β-lactamases genes TEM and SHV in urinary tract isolates of Escherichia coli and Klebsiella pneumoniae in Tabriz [Internet]. Vol. 19, Archive of SID Journal of Ardabil University of Medical Sciences. 2019 [cited 2020 Jul 5]. Available from: www.SID.ir
Domaracký M, Rehák P, Juhás Š, Koppel J (2007) Effects of selected plant essential oils on the growth and development of mouse preimplantation embryos in vivo. Physiol Res 56:97–104
Dominguez XA (1985) Quinonas. In: Métodos de investigación fitoquímica
El-Maati MFA, Mahgoub SA, Labib SM, Al-Gaby AMA, Ramadan MF (2016) Phenolic extracts of clove (Syzygium aromaticum) with novel antioxidant and antibacterial activities. Eur J Integr Med 8:494–504
El-Shouny WA, Ali SS, Hegazy HM, Abd Elnabi MK, Ali A, Sun J (2020) Traditional herbal medicine against cagA and vacA toxin genes-producing drug resistant Helicobacter pylori. J Tradit Complement Med. 10:366–377
Faujdar S, Bisht D, Sharma A (2020) Antibacterial activity of Syzygium aromaticum (clove) against uropathogens producing ESBL, MBL, and AmpC beta-lactamase: Are we close to getting a new antibacterial agent? J Fam Med Prim Care 9:180
Guan W, Li S, Yan R, Tang S, Quan C (2007) Comparison of essential oils of clove buds extracted with supercritical carbon dioxide and other three traditional extraction methods. Food Chem 101:1558–1564
Gündüz GT, Gönül ŞA, Karapinar M (2009) Efficacy of myrtle oil against Salmonella Typhimurium on fresh produce. Int J Food Microbiol 130:147–150
Herrera García M, Arévalo Valdez C, Velásquez Porta T (2019) Detección de los genes de β-lactamasas blaTEM, blaSHV y blaCTX-M en aislamientos de Escherichia coli comunitarios. revistasguatemala.usac.edu.gt [Internet]. 2019 [cited 2020 Jul 5]. http://revistasguatemala.usac.edu.gt/index.php/qyf/article/view/939
Kim S, Lieberman TD, Kishony R (2014) Alternating antibiotic treatments constrain evolutionary paths to multidrug resistance. Proc Natl Acad Sci U S A 111:14494–14499
Langeveld WT, Veldhuizen EJA, Burt SA (2014) Synergy between essential oil components and antibiotics: a review. Crit Rev Microbiol 40:76–94
Lawal G (2019) Phytochemical screening and in vitro bacteriostatic effects of Syzigium aromaticum (Clove) Extracts on Clinical Bacterial Isolates [Internet]. Vol. 7, JOBIMB. 2019 [cited 2020 Jul 5]. http://journal.hibiscuspublisher.com/index.php/JOBIMB/index
Lennette E, Truant J, Spaulding C, Abella C. Manual de microbiología clínica. 1981 [cited 2020 Jul 13]; http://www.sidalc.net/cgi-bin/wxis.exe/?IsisScript=LIBRO.xis&method=post&formato=2&cantidad=1&expresion=mfn=014876
Martinez-Elizalde KS, Jimenez-Estrada M, Flores CM, Hernandez LB, Rosas-Lopez R, Duran-Diaz A et al (2015) Evaluation of the medicinal properties of Cyrtocarpa procera Kunth fruit extracts. BMC Complement Altern Med 15:1–7
Moo CL, Yang SK, Osman MA, Yuswan MH, Loh JY, Lim WM, et al (2020) Antibacterial activity and mode of action of β-caryophyllene on Bacillus cereus. Polish J Microbiol
NIST (2016) NIST Standard reference database number 69. NIST Chemistry WebBook
Nana WL, Eke P, Fokom R, Bakanrga-Via I, Begoude D, Tchana T et al (2015) Antimicrobial activity of syzygium aromaticum and zanthoxylum xanthoxyloides essential oils against phytophthora megakarya. J Phytopathol 163:632–641
Nazer AI, Kobilinsky A, Tholozan JL, Dubois-Brissonnet F (2005) Combinations of food antimicrobials at low levels to inhibit the growth of Salmonella sv. Typhimurium: a synergistic effect? Food Microbiol. 22:391–398
Oluwasina OO, Ezenwosu IV, Ogidi CO, Oyetayo VO (2019) Antimicrobial potential of toothpaste formulated from extracts of Syzygium aromaticum, Dennettia tripetala and Jatropha curcas latex against some oral pathogenic microorganisms. AMB Express 9(1):20
Pana ZD, Zaoutis T (2018) Treatment of extended-spectrum β-lactamase-producing enterobacteriaceae (ESBLS) infections: What have we learned until now? version 1 referees: 2 approved. F1000Research 7:1347
Paterson IK, Hoyle A, Ochoa G, Baker-Austin C, Taylor NGH (2016) Optimising antibiotic usage to treat bacterial infections. Sci Rep 6:1–10
Pitout JDD (2012) Extraintestinal pathogenic Escherichia coli: A combination of virulence with antibiotic resistance. Front Microbiol 3:9
Pitout JD, Laupland KB (2008) Extended-spectrum β-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis 8:159–166
Roy A, Bulut O, Some S, Mandal AK, Yilmaz MD (2019) Green synthesis of silver nanoparticles: Biomolecule-nanoparticle organizations targeting antimicrobial activity. RSC Adv 9:2673–2702
Santin JR, Lemos M, Klein-Júnior LC, Machado ID, Costa P, De Oliveira AP et al (2011) Gastroprotective activity of essential oil of the Syzygium aromaticum and its major component eugenol in different animal models. Naunyn Schmiedebergs Arch Pharmacol 383:149–158
Sawa T, Kooguchi K, Moriyama K (2020) Molecular diversity of extended-spectrum β-lactamases and carbapenemases, and antimicrobial resistance. J Intensive Care 8:13
Seale AC, Gordon NC, Islam J, Peacock SJ, Scott JAG (2017) AMR surveillance in low and middle-income settings–a roadmap for participation in the Global Antimicrobial Surveillance System (GLASS). Wellcome Open Res 2:92
Shan B, Cai YZ, Sun M, Corke H (2005) Antioxidant capacity of 26 spice extracts and characterization of their phenolic constituents. J Agric Food Chem 53:7749–7759
Shrivastav A, Sharma R, Shrivastava N, Gautam V, Jain S (2019) Study of inhibitory potential and percent inhibition of oil of Syzygium aromaticum and leaves of Ocimum sanctum on ESBL enzyme from Escherichia coli in broilers of Jabalpur. Indian J Pharmacol 51:337
US National Library of Medicine - National Institutes of Health. Home - PMC - NCBI. www.ncbi.nlm.nih.gov. 2017
Vanden Berghe DA, Vlietinck AJ, Dey DM, Harborne JB (1991) Screening methods for antibacterial and antiviral agents from higher plants. In: Assays for bioactivity
Van Vuuren SF, Suliman S, Viljoen AM (2009) The antimicrobial activity of four commercial essential oils in combination with conventional antimicrobials. Lett Appl Microbiol 48:440–446
World Health Organisation (2001) Legal status of traditional medicine and complementary/alternative medicine: a worldwide review. World Health Organisation, Geneva
World Health Organization (WHO) (2013) WHO traditional medicine strategy 2014–2023. World Heal Organ, Geneva
Wright GD (2019) Unlocking the potential of natural products in drug discovery. Microb Biotechnol 12:55–57
Acknowledgements
To the Master of Pharmaceutical Sciences and Technology from Autonomous University of the State of Mexico; National Autonomous University of Mexico, FES Iztacala, UBIPRO, and the ISSEMyM Medical Center of Toluca for providing the bacterial strains to perform this research with protocol number ISSEMYM 031/17.
Funding
Authors acknowledge the funding granted by the National Council of Science and Technology National Science to the main author of this paper under the protocol number: MCYTF-0518.
Author information
Authors and Affiliations
Contributions
The authors equally contributed in all the article parts. The authors wrote, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mejía-Argueta, E.L., Santillán-Benítez, J.G., Canales-Martinez, M.M. et al. Antimicrobial activity of Syzygium aromaticum L. essential oil on extended-spectrum beta-lactamases-producing Escherichia coli. Bull Natl Res Cent 44, 201 (2020). https://doi.org/10.1186/s42269-020-00458-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-020-00458-x