Abstract
Background
Urinary tract infections represent one of the most frequent hospital and community-acquired infections with uropathogenic Escherichia coli (UPEC) being the main causative agent. The global increase in the emergence of multidrug-resistant (MDR) UPEC necessitates exploring novel approaches. Repurposing natural products as anti-quorum sensing (QS) agents to impede bacterial virulence is gaining momentum nowadays. Hence, this study investigates the anti-QS potentials of carvacrol, cinnamaldehyde, and eugenol against E. coli isolated from urine cultures of Egyptian patients.
Results
Antibiotic susceptibility testing was performed for 67 E. coli isolates and 94% of the isolates showed MDR phenotype. The usp gene was detected using PCR and accordingly, 45% of the isolates were categorized as UPEC. Phytochemicals, at their sub-inhibitory concentrations, inhibited the swimming and twitching motilities of UPEC isolates, with eugenol showing the highest inhibitory effect. The agents hindered the biofilm-forming ability of the tested isolates, at two temperature sets, 37 and 30 °C, where eugenol succeeded in significantly inhibiting the biofilm formation by > 50% at both investigated temperatures, as compared with untreated controls. The phytochemicals were shown to downregulate the expression of the QS gene (luxS) and critical genes related to motility, asserting their anti-QS potential. Further, the combinatory activity of the phytoproducts with five antibiotics was assessed by checkerboard assay. The addition of the phytoproducts significantly reduced the minimum inhibitory concentrations of the antibiotics and generated several synergistic or partially synergistic combinations, some of which have not been previously explored.
Conclusions
Overall, carvacrol, cinnamaldehyde, and eugenol could be repurposed as potential anti-QS agents, which preferentially reduce the QS-based communication and attenuate the cascades of gene expression, thus decreasing the production of virulence factors in UPEC, and eventually, subsiding their pathogenicity. Furthermore, the synergistic combinations of these agents with antibiotics might provide a new perspective to circumvent the side effects brought about by high antibiotic doses, thereby paving the way for overcoming antibiotic resistance.
Similar content being viewed by others
Background
Urinary tract infections (UTIs) are considered among the most contracted bacterial illnesses worldwide throughout the community and hospital settings [1]. They are associated with high mortality and morbidity imposing massive economic and societal burdens [2]. Uropathogenic Escherichia coli (UPEC), the main etiological agent of UTIs, is responsible for more than 80% of UTIs globally [3]. Over the last decades, the problem has escalated with the emergence of a multidrug-resistant (MDR) phenotype among UPEC, featuring an alarming situation [4]. In Egypt, a comparable context is noticed. The easily attainable antibiotics without prescription and their extensive usage in clinical treatment, or as boosters in crop and livestock production, have triggered the emergence of elevated resistance rates among UPEC isolates. This classified Egypt as a country with the highest detected resistance levels compared to its neighboring counterparts in the Arab League [5, 6].
The exceptional ability of the UPEC strains to establish UTI is majorly endorsed by the production of a wide array of virulence factors. These include several adhesins known to increase the colonizing potential of UPEC, as well as an arsenal of weaponries such as toxins, proteases, and siderophores. The iron-chelating compounds secreted by a UPEC strain enable the uropathogen to overcome the restriction of iron availability and to survive inside the nutritionally deficient bladder environment [7]. Moreover, recurrent and difficult-to-treat UTIs are provoked by the UPEC’s capability to form biofilm, a sophisticated defense mechanism creating a sessile bacterial community of cells immersed in a matrix of extracellular polymeric substances creating dormant bacterial repository from which bacteria can re-emerge causing recurrence, thus posing a substantial challenge to physicians [8].
The production of virulence factors in E. coli is fostered and strictly regulated by a cell density-dependent bacterial signaling system. This phenomenon is collectively named quorum sensing (QS) [9, 10]. QS is initiated through the secretion of chemical signaling molecules known as autoinducers. When these autoinducers reach certain thresholds, a signal transduction cascades, and the expression of certain genes is triggered, resulting in a particular change in bacterial behavior. This change may involve antimicrobial resistance (AMR), bacterial bioluminescence, toxin secretion, formation of biofilm, or altered motility [11]. It has been reported that E. coli possesses five major QS systems namely LuxS/autoinducer-2 (AI-2), AI-3/epinephrine/norepinephrine, indole signaling, extracellular death factor, and SdiA QS systems. These QS circuits participate in regulating virulence genes mediating biofilm production, mobility, toxicity, and the production of curli [12].
For decades, the cornerstone strategy for the treatment of UTIs has relied upon the administration of conventional antibiotics such as fosfomycin, nitrofurantoin, sulfamethoxazole/trimethoprim, fluoroquinolones, in addition to aminoglycosides and tetracyclines [7, 13]. However, the rising resistance of UPEC isolates to these routinely used antibiotics is becoming a significant health issue that necessitates a prompt discovery of new alternatives [14]. One of the promising approaches for “disarming” the bacterial virulence is the anti-QS approach. Numerous efforts have been made to create quorum-sensing inhibitors (QSIs) from natural compounds [12, 15]. It has been demonstrated that grape seed extract acts as a natural QSI in E. coli via decreasing flagellar motility and Shiga toxin production, while extracts of broccoli, oregano, rosemary, turmeric, ginger, and basil inhibit the swarming motility of E. coli by impairing the AI-2 QS system [12, 16]. It seems that hijacking QS signaling using QSIs does not only halt bacterial resistance but also tends to disrupt the production of the associated virulence genes without affecting bacterial fitness [11]. Therefore, the anti-QS strategy can be regarded as an attractive alternative that does not exert the classical selective pressure and is able to tackle virulence, especially when used in synergistic combinations with conventional antibiotics [17]. In the current study, we attempted to investigate the ability of some essential phytoproducts, namely carvacrol (CaRV), cinnamaldehyde (CiNN), and eugenol (EG), to suppress the QS-mediated virulence factors such as biofilm formation and motility in UPEC isolated in Egypt. Subsequently, we present an in vitro assessment of the combined effect of these agents with selected antibiotics as a solution to combat the MDR phenotype widely encountered among UPEC isolates.
Results
Identification of the tested isolates and demographic profiles of study subjects
The identity of the 67 isolates collected from the routine laboratory of Alexandria Main University Hospital (AMUH) was confirmed to be E. coli as indicated by the biochemical tests illustrated in Additional file 1. The demographic characteristics of 67 patients (36 males and 31 females) from whom the specimens were isolated showed that UTIs were more prevalent among males in the fifth decade with no incidence in the age group below 20, whereas females showed the highest prevalence in the fourth- and fifth-decade groups (Fig. 1).
Assessment of antibiotic resistance and the effect of the phytochemicals on the growth of E. coli isolates
The susceptibility of 67 E. coli isolates to fifteen antibiotics, selected among the recommended ones for UTIs, was determined using the Kirby–Bauer disk diffusion method. The results showed that a very high percentage of these isolates, reaching 94%, displayed an MDR phenotype, being resistant to at least one agent in three or more chemical classes of antimicrobials (Fig. 2a). More than 70% of the isolates were resistant to amoxicillin/clavulanate, cefepime, cefotaxime, ceftriaxone, imipenem, doxycycline, sulfamethoxazole/trimethoprim, ciprofloxacin, and levofloxacin. The highest percentage of susceptibility was detected to amikacin (94%), followed by meropenem (85%), then colistin (80.5%). None of the isolates was resistant to tigecycline; nevertheless, 22.4% of the isolates were intermediately resistant to it (Fig. 2b). The different antibiotic resistance patterns obtained for the 67 isolates as well as their multiple antibiotic resistance (MAR) indices are represented in Additional file 2. A percentage of 94% of the isolates had a MAR index greater than 0.2 indicating that the organisms were isolated from a region with an upsurge in MDR pathogens. Among the phytochemicals, CiNN exhibited the highest activity level with a minimum inhibitory concentration (MIC) range of 130 to 260 µg/mL, followed by CaRV (MIC range: 250–1000 µg/mL), then EG which yielded an MIC range of 800 to 1600 µg/mL (Additional file 3).
(a) Prevalence of multidrug-resistant (MDR) phenotype, (b) Antibiotic resistance profiles of 67 E. coli isolates. Antibiotics include AK: amikacin, AMC: amoxicillin/clavulanate, CPM: cefepime, CTX: cefotaxime, CTR: ceftriaxone, CIP: ciprofloxacin, CL: colistin, DO: doxycycline, ETP: ertapenem, GEN: gentamicin, IPM: imipenem, LE: levofloxacin, MRP: meropenem, TGC: tigecycline, and COT: sulfamethoxazole/trimethoprim
Antibiotic-antibiotic pairwise correlations
Resistance to two or more antibiotics belonging to the same class is referred to as cross-resistance and is thought to be caused by a similar genetic mechanism. Conversely, associated resistance is defined as resistance to two or more antibiotics belonging to different classes and is deemed to be caused by unrelated mechanisms [18]. To explore the pairwise correlation between different antibiotics used in the current study, the resistance data of the 67 isolates was used to build a correlation matrix based on Pearson correlation coefficient (Fig. 3). The matrix implied that ceftriaxone–cefotaxime, cefepime–amoxicillin/clavulanate, and ceftriaxone–amoxicillin/clavulanate pairs were the most correlated and showed an extremely high significance at p ≤ 0.001. A strong correlation was observed as well among the tested fluoroquinolones (levofloxacin-ciprofloxacin) with Pearson correlation coefficient of 0.905 (p ≤ 0.001).
Correlation matrix showing Pearson’s correlation coefficients (r) calculated based on the resistance profile obtained from 67 E. coli isolates. The dark-colored green, moderately colored green, and light-colored green boxes denote correlations that are significant at p ≤ 0.001, p ≤ 0.01, and p ≤ 0.05, respectively. β-lactams include AMC (amoxicillin/clavulanate), CTR (ceftriaxone), CPM (cefepime), CTX (cefotaxime), ETP (ertapenem), IPM (imipenem), and MRP (meropenem). CIP (ciprofloxacin) and LE (levofloxacin) belong to fluoroquinolones, while COT (sulfamethoxazole/trimethoprim) belongs to the folate pathways antagonists’ class
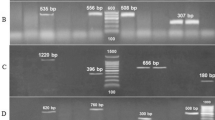
Molecular detection of usp gene
PCR analysis identified an amplicon of 435 bp corresponding to the usp gene which codes for the uropathogenic specific protein in 30/67 of the tested E. coli isolates, thus classifying 45% of the isolates as UPEC. A representative agarose gel showing the PCR amplification of usp gene in some selected E. coli isolates is illustrated in Fig. 4.
Representative agarose gel showing PCR amplification of usp gene in selected E. coli isolates. Lanes 1 and 2 correspond to a DNA molecular marker (100 bp). Lanes 3, 4, 5, and 7 show the amplicon (435 bp) corresponding to usp gene in E1, E2, E3, and E10 isolates, respectively. Lane 6 corresponds to the result of E5, a non-usp-harbouring isolate
Quorum sensing inhibition assays
Inhibition of swimming and twitching motilities
The effect of 0.5XMIC of CaRV, CiNN, and EG on the swimming motility was investigated in 24/30 UPEC isolates that originally exhibited a halo zone diameter of swimming motility of ≥ 40 mm. The isolates were grouped into 3 subgroups, where group 1 included isolates that did not show any suppression by the tested agent, group 2 comprised isolates undergoing an inhibition range of 1–49%, while group 3 encompassed isolates having their swimming motility hindered in the presence of the agents by a value of ≥ 50%. Various inhibition patterns were observed, where EG and CiNN were able to suppress the swimming motility of 14/24 and 12/24 of UPEC isolates, respectively, by a value of ≥ 50%. On the other hand, CaRV showed the least inhibitory effect as it was unable to repress the swimming motility of 16/24 of UPEC isolates (Fig. 5a). To test the inhibitory effect of the phytochemicals on the twitching motility, intermediately motile isolates having twitching zone diameters of 5–20 mm were selected to build Fig. 5b. At concentrations corresponding to their 0.5XMIC, EG possessed the highest inhibitory effect followed by CaRV, then CiNN, where 8/13, 6/13, and 5/13 of UPEC isolates, respectively, had their twitching motility inhibited by a value of ≥ 50%. Representative illustrations showing the inhibition of swimming and twitching motilities by phytochemicals are presented in Fig. 6.
Inhibitive effect of cinnamaldehyde on the swimming motility of E51 isolate showing (a) Control without cinnamaldehyde and (b) Cinnamaldehyde at a concentration equivalent to 0.5XMIC; Inhibition of twitching motility of isolate E63 by eugenol showing (c) Control without eugenol and (d) Eugenol at a concentration corresponding to 0.5XMIC
Impeding the biofilm formation
The inhibitory prospects of 0.5XMIC of CaRV, CiNN, and EG on the biofilm-forming ability were assessed at two temperature sets, 37 and 30 ºC, in isolates showing OD630 above 0.1 (2X ODc). At 37 ºC, EG exhibited the highest suppression level among the tested agents, where it hindered biofilm formation in E51 (initially a strong biofilm-forming isolate) by 75% and in E63 (a moderate biofilm-forming isolate) by 67%, both inhibition values being significant at p < 0.05 (Fig. 7a). For the assay at 30 ºC, 20 UPEC isolates exhibiting strong to moderate biofilm-forming capacity were selected and average biofilm formation was calculated for the control or in the presence of the phytochemicals (Fig. 7b). Eugenol succeeded in significantly inhibiting the biofilm formation by 67% (p < 0.05), followed by CaRV which significantly decreased the biofilm-forming ability by 50%, then CiNN showing a percentage inhibition of 33% as compared with untreated controls (Fig. 7b).
Anti-biofilm activities of carvacrol, cinnamaldehyde, and eugenol at their sub-MICs in: (a) E51 and E63 UPEC isolates experimented at 37 ºC, (b) 20 UPEC isolates investigated at 30 ℃. Data are shown as a mean of three independent experiments with error bars indicating SDs. The p-values indicate the significance at *p < 0.05 vs. non-treated samples
Differential expression levels of genes
qRT-PCR analysis was carried out to assess the ability of CaRV, CiNN, and EG, at their sub-MIC range, to suppress the expression levels of the QS gene (luxS) and the QS-regulated virulence genes. These included the genes coding curli fimbriae (csgA), a crucial component for biofilm formation, a fimbrial adhesin gene, fimA, and fliC, a flagellar gene essential for the motility of UPEC. Four isolates were selected for the transcriptional analysis: E13, E35, E51, and E63 isolates. The selection was based on the isolates evident display of phenotypic expression of biofilm formation and motility. To allow the maximum expression of their virulence factors, E51 and E63 were grown at 37 ºC, while E13 and E35 were subcultured at 30 ºC in the presence and absence of the agents. The phytochemicals commonly altered the expression levels of the tested genes, yet in a variable manner. Carvacrol succeeded in downregulating the major QS gene, luxS, in 100% of the tested isolates with a fold reduction ranging from 1.06 (in E63 isolate) to 1.62 (in E35 isolate). csgA gene was repressed by CaRV in 75% of the isolates and the repression ranged from 1.1- (in E13 isolate) to 1.4-fold (in E35 isolate). fliC gene was downregulated in 75% of the isolates with the highest fold reduction reaching 1.5-fold in E35 isolate and the lowest fold reduction reaching 1.1 in E51 isolate. Carvacrol reduced the expression level of fimA in a single isolate, E51, by 1.2-fold. (Fig. 8a). CiNN repressed the expression levels of csgA and fimA in 100% of the isolates with a fold reduction ranging from 1.3 to 2.6. It reduced the levels of luxS and fliC in 75% of the isolates with a fold reduction ranging from 5.3 to 1.3 (Fig. 8b). The levels of transcripts of luxS and fliC were reduced by an average of 1.46- and 1.76-fold, respectively, in 75% of the isolates by EG and those of csgA were downregulated in 50% of the tested isolates by a fold reduction ranging from 1.67 (in E35 isolate) to 3 (in E35 isolate). An unexpected significant upregulation of fimA gene was noticed upon treatment with CaRV or EG (Fig. 8a and c, respectively).
Relative expression of QS gene (luxS) and QS-regulated virulence genes (csgA, fimA, and fliC) associated with the production of virulence factors in UPEC, following treatment with sub-MICs of (a) Carvacrol, (b) Cinnamaldehyde, and (c) Eugenol. Gene expression was normalized with gapA and represented relative to the expression of genes in the untreated control. The error bars indicate SDs. The p-values indicate the significance of fold decrease at *p < 0.05 and fold increase at +++p < 0.001 and ++++p < 0.0001
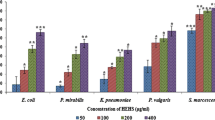
Assessment of the combined activity of phytochemicals and antibiotics by checkerboard assay
The combined effect of CaRV, CiNN, and EG with ciprofloxacin, ceftriaxone, colistin, doxycycline, and tigecycline was investigated against E18, E35, and E63 isolates. These isolates were chosen based on their MDR phenotype, being resistant to 9 antibiotics belonging to 4 different classes. The results in Table 1 are expressed in terms of fractional inhibitory concentration (FIC) index and combinations displaying synergy or partial synergy are referred to as successful ones. The addition of the phytoproducts significantly reduced the MIC of the antibiotic as demonstrated by the fold reduction in the MICs of the used antimicrobials (Additional file 4). Carvacrol generated successful combinations with ceftriaxone, colistin, or doxycycline in 100% of the tested isolates. When combined with tigecycline, CiNN showed partial synergy in 66.6% of the isolates, while EG revealed successful combinations with ciprofloxacin, ceftriaxone, or tigecycline in 100% of the isolates included in the assay.
Discussion
Globally, 150 million UTI cases are reported each year, thus increasing the medical care expenses [19]. Although other bacteria may cause UTIs, UPEC is by far the most predominant pathogen infecting the urinary tract in the United States, Europe, and Latin America [20, 21]. In the current study, 67 E. coli isolates were collected from the urine cultures of patients with UTIs admitted to AMUH from July to October 2018. Demographically, a higher incidence of UTIs in male patients (54%) as compared to their female counterparts (46%) was recorded in this investigation. Although females are known to be at a higher risk group for developing UTIs owing to the anatomical structure of their urinary system [22], other observers found that these infections were more common in males [23]. This could be explained by the higher age group of the patients, exceeding 40 yrs, from whom the samples were collected in this study. In older age, males are at higher risk of catheterization, prostate gland enlargement, and reduced bacteriostatic secretions of the prostate, all representing factors elevating the incidence of UTIs [24].
The treatment of UTIs is usually achieved by a short-term antibiotic regimen, but bacterial resistance to antimicrobials is escalating. A percentage of 94% of the isolates in this study exhibited an MDR phenotype. This elevated incidence rate is in accordance with the rates reported in other parts of Egypt, where MDR E. coli was detected among 96%, 91%, and 95% of the tested isolates in Minia, Dakahlia and Giza, and Cairo, respectively [25,26,27]. MAR indexing method, a useful technique for the evaluation of risk assessment, provides an estimate of the number of bacteria that exhibit antibiotic resistance in the risk area throughout any standard susceptibility testing [28]. A MAR index of > 0.2, a value identical to the one reported by Masoud et al. in 2022 in Egypt [25], was detected for 94% of the isolates in our study. This high MAR index implies the prevalence of persistent pathogens that are resistant to conventional antibiotics at the collection area. Self-medication with the lack of underlying adequate tests, improper antibiotic use, and blind diagnosis are condemned for this extremely high value [29]. More than 85% of the isolates in our collection showed resistance to cephalosporins. These high levels of resistance, endorsed by the World Health Organization report in 2014 are thought to be attributed to their low cost, simple access, and frequent prescription in Egyptian healthcare establishments. While 89.5% and 38.8% of the isolates were resistant to imipenem and ertapenem, respectively, meropenem remained resilient against most of the isolates, with a percentage of susceptibility of 85%. Meropenem is not frequently prescribed in outpatient clinics and is regarded as a last-resort antibiotic in Egyptian hospitals [30]. However, the emergence of carbapenem-resistant E. coli strains is noticed globally necessitating the prudent use of this antibiotic [31]. In addition to meropenem, our results highlight the effectiveness of aminoglycosides, tigecycline, and colistin as treatment options for the eradication of resistant urinary E. coli isolates.
Analyzing the pairwise correlations, highly significant correlations (p ≤ 0.001) were detected among β-lactams pairs and the fluoroquinolones pair (ciprofloxacin-levofloxacin) referring to the phenomenon of cross-resistance. A rational justification by Mohamed et al. [32]. indicated that isolates tend to display similar resistance to antibiotics with related chemical structures. Whereas the correlations detected between the β-lactams-fluoroquinolones and β-lactams-co-trimoxazole pairs refer to associated resistance and are explained by the fact that the implicated resistance genes are co-existing on plasmids that can be easily transferred among bacterial strains [30, 33].
The pathogenicity of a UPEC strain fundamentally depends on the production of virulence factors including adhesins, toxins, siderophores, destructive enzymes, and persistent biofilms that are regulated by its QS mechanism [34]. The last decade has witnessed a revolutionary increase in AMR worldwide, urging the need to discover novel non-antibiotic treatment approaches [35]. In this context, tackling the bacterial QS circuits to constrain virulence has gained attention among researchers, paving the way for novel anti-virulence strategies [12]. The anti-QS approach was pioneered in 2006 by Niu et al. [36]., where the authors demonstrated the CiNN’s ability to impede QS in Vibrio harveyi via modulating the expression of QS genes. Since then, reports emphasizing the anti-QS potentials of different natural phytoproducts and their capacity to attenuate virulence in different microorganisms have surfaced [37,38,39,40]. However, scarce data are available regarding the effect of CaRV, CiNN, and EG on the virulence of MDR UPEC isolates and their mechanism of QS inhibition in these isolates. Hence, the current study focused on evaluating the anti-virulent potential and anti-QS activity of these three phytochemicals against UPEC isolates. We initiated the study by determining the MICs of CaRV, CiNN, and EG, followed by the selection of the sub-MIC ranges to allow the subsequent study of their anti-QS efficacies. Previous observations indicated that subinhibitory concentrations of CaRV, CiNN, and EG inhibited the motility and biofilm-forming ability, traits known to be regulated by QS in E. coli, in a dose-dependent manner [41,42,43]. These observations are consistent with our results, where higher concentrations demonstrated antimicrobial activities of the agents, while lower ones showed anti-QS abilities. Further, we examined the anti-motility impact of the agents against UPEC. Apart from playing a fundamental role in the colonization of the urinary tract and biofilm formation, motility enables UPEC to avoid the wash-out effect of the urine flow, evade the host defense mechanisms, and compete with other pathogens in polymicrobial niches where the advantage is given to motile pathogen [35]. In accordance with previous studies [44, 45], the tested phytochemicals at their sub-MICs succeeded in decreasing the swimming motility of UPEC by a value of ≥ 50%.
Twitching motility is considered one of the prerequisites for biofilm formation [46] and while being studied intensively in other pathogens such as Pseudomonas aeruginosa, P. fluorescens, and Erwinia carotovora [35, 47], to the best of our knowledge, this is the first investigation shedding light on the phenotypic inhibitory effect of the three phytochemicals on the twitching motility in UPEC. The phytoproducts reduced the twitching motility of the tested isolates by ≥ 50%, thus facilitating the hindrance of the succeeding step, biofilm formation.
The biofilm-forming ability of the UPEC isolates was observed to be enhanced at 30℃ when compared to their ability at 37℃. An increased biofilm formation at 30℃ was reported as well by Uhlich et al. [48]. in some E. coli pathotypes. This could be explained by the fact that curli synthesis, an important attribute for biofilm formation, is temperature-dependent and that 30℃ is considered to be the optimum temperature for its expression as reported by Leech et al. [49]. In their study, Leech et al. [49]. demonstrated that the highest expression of csg genes occurred at 30 °C, followed by 28 °C, then at 37 °C. Additionally, other fimbriae that contribute to biofilm formation, such as F9 fimbriae, are known to be optimally expressed at 28℃ [50]. The hazard of biofilm formation by UPEC isolates tends to augment with prolonged catheterization, during which, antibiotic treatment may worsen the situation by imposing selective pressure on the bacteria and leading to the acquisition of more resistance. Since QS circuits adopted by E. coli dominate the transition between the different phases of biofilm formation, an opportunity is created for an intervention using the anti-QS approach [51]. The abrogation of biofilm formation was tested in our study using two temperature sets, 30℃ and 37℃, a parameter not previously explored. The phytoconstituents were shown to hinder the biofilm formation in UPEC isolates at both temperatures demonstrating variable degrees of inhibition, with EG displaying the highest effect. This anti-biofilm effect of the agents at 37℃ is consolidated in the literature by several studies [42, 43, 52, 53].
Motivated by the anti-QS phenotypic results, we pursued to explore the genetic basis of this anti-QS effect, where the differential expression of the virulence-associated genes (fimA, csgA, and fliC) and the QS gene (luxS) were investigated under test and control conditions using qRT-PCR. The phytoproducts caused downregulation of luxS gene in all tested isolates implying that inhibition of the AI-2 system through luxS pathway is a suggested anti-QS mechanism exerted by these compounds. However, CiNN increased the expression level of luxS in a single isolate. This could be explained by the fact that downregulation of other genes engaged in the AI-2 QS system such as pfs, a gene that was not investigated in this study, could have occurred in this particular case [54]. The agents were able, as well, to repress the transcription of the curli fimbriae gene, csgA, a crucial component for biofilm formation, and fliC, a flagellar gene essential for the motility of UPEC. Our results were in accordance with previous reports investigating the expression levels of the abovementioned genes in UPEC or other E. coli pathotypes [41, 52, 55, 56]. Surprisingly, extremely significant upregulation of the fimbrial adhesin gene, fimA, was noticed in some isolates upon treatment with EG or CaRV. This result suggests that bacteria, when encountering unfavorable conditions in the environment, tend to selectively upregulate the expression of a certain gene, which is in this case the fimbrial adhesin gene, fimA, to counteract the suppressing effect exerted on another related gene.
Based on the results of the checkerboard assay, the combinatory effect of CaRV, CiNN, and EG with 5 antibiotics showed partial synergistic interactions in 53%, 33%, and 60% of the generated combinations, respectively. Synergistic combinations were detected, as well, when combining CaRV with ceftriaxone or colistin, and EG with tigecycline or ceftriaxone. Few data are available in the literature regarding the results of these combinations especially in UPEC isolates. Ibrahim and Al Meani [57] reported that combining clove oil, whose major component is EG, enhanced the effect of cefepime, ceftazidime, and ceftriaxone, whereas Vázquez-Ucha et al. [58] detected synergy between thyme oil, the major constituent of which is CaRV, and colistin in Acinetobacter baumannii and Klebsiella pneumoniae. In accordance with our results, a study conducted by Özel et al., in 2022, reported a synergistic interaction of EG with tigecycline in E. coli. The mode of action of CaRV and EG is thought to be due to their lipophilic nature which enables them to accumulate and disintegrate the lipids in the bacterial membrane causing its disruption, energy depletion, and leakage. Whereas CiNN binds to bacterial proteins preventing the action of important bacterial enzymes. Combining these natural compounds with antibiotics constrains bacterial adaptation and restores antibiotic sensitivity by allowing the penetration of the latter [59]. Another reason for the synergetic effect is accounted to the ability of EG and CaRV to disrupt the bacterial cytoplasmic membrane, permeabilize the cell wall, enhance the expression of porins, and downregulate the efflux pumps, thus facilitating the uptake of the antibiotics [60, 61]. Despite being terpenic components of essential oils, the effect of CaRV, CiNN, and EG vary due to the difference in their chemical structure, where the phenolic nature of CaRV and EG tend to exhibit a greater bactericidal effect when compared to aldehydes [62]. Consistent with our findings, CiNN displayed successful combinations with a lower number of antibiotics. The lack of the potentiating effect noted in some interactions can be ascribed to the presence of multiple genes of resistance with variable expressions [59]. The generated synergistic or partially synergistic combinations, some of which have not been previously explored, could provide a new perspective to overcome the side effects brought about by high antibiotic doses and minimize the problem of AMR.
Conclusion
In conclusion, this study sheds light on the anti-QS potential of the phytoconstituents, CaRV, CiNN, and EG. Their combined use with conventional antibiotics succeeded in circumventing antibiotic resistance of MDR UPEC isolates paving the way to novel treatment options for the management of UTIs. Instead of exerting direct selective pressure on the growth of UPEC isolates, these phytochemicals could preferentially reduce the QS-based communication and attenuate the cascades of gene expression decreasing the production of virulence factors, and eventually, subsiding their pathogenicity. We understand and acknowledge the limitations of this study. The combined phytochemicals/antibiotic effect was investigated on a small sample size limiting the statistical significance of synergistic results. Further in vivo validation could have enabled the elucidation of the exact mechanism behind the anti-QS activity of these phytochemicals and their anti-virulent properties.
Methods
Collection and identification of E. coli clinical isolates
Sixty-seven E. coli clinical isolates were collected through the routine laboratory facility of AMUH from the urine cultures of patients admitted to the hospital with UTIs throughout the time duration of July to October 2018. The isolates were preserved as frozen stocks at -20 °C in Luria-Bertani broth (LB, HiMedia, Mumbai, India) containing 20% glycerol and were archived at − 80 °C. Before use, a fresh culture of each of the collected isolates was obtained by cultivation on MacConkey’s and eosin methylene blue agar (Oxoid, Hampshire, UK). Following incubation at 37 °C for 24 h, the isolated colonies were identified by Gram staining and then subjected to standard biochemical tests including triple-sugar iron, indole production, methyl red, Voges Proskauer, citrate utilization, catalase, and urease tests.
Antimicrobial susceptibility testing
The susceptibility of the 67 E. coli isolates to 15 antimicrobials was determined by Kirby-Bauer disk diffusion method using cation-adjusted Mueller–Hinton (CAMH, HiMedia, Mumbai, India) agar. The following antibiotic disks were purchased from HiMedia Laboratories (Mumbai, India) and used for the test: amoxicillin/clavulanate, cefotaxime, ceftriaxone, cefepime, imipenem, meropenem, ertapenem, amikacin, gentamicin, doxycycline, tigecycline, ciprofloxacin, levofloxacin, sulfamethoxazole/trimethoprim, and colistin. The test was carried out according to the Clinical Laboratory Standards Institute (CLSI, 2021) guidelines using Mueller–Hinton agar (HiMedia Laboratories, Mumbai, India) and the results were interpreted in accordance with the breakpoints indicated in CLSI, except for tigecycline and colistin, where EUCAST (2018) and disk manufacturer’s guidelines were applied, respectively, to interpret the results. MAR index, a ratio between the number of antibiotics that an isolate is resistant to and the total number of antibiotics the isolate is exposed to, was calculated for the 67 tested E. coli isolates according to the method described by Masoud et al. [63]. Broth microdilution technique was performed to determine the MICs of the phytochemicals, CaRV (Sigma Aldrich, UK), CiNN (LOBA Chemie, Mumbai, India), and EG (LOBA Chemie, Mumbai, India). Prior to their use, the agents were sterilized using 0.45 μm bacterial filters (Filter-bio-CO., China) and were solubilized in 7.5% dimethyl sulfoxide (DMSO, Fischer Scientific, USA), a concentration which allowed the growth of the isolates as confirmed by the determination of DMSO MIC against all the tested isolates. Serial dilution of CiNN and EG was performed using 7.5% DMSO, while the stock solution of CaRV in 7.5% DMSO was serially diluted in sterile distilled water. The MIC values of the phytochemicals were determined by measuring the absorbance at OD600 after 24 h of incubation using an ELISA microtiter plate reader (BioTek 800 TS, USA) [64].
Molecular detection of usp gene using PCR
The usp gene, coding for the uropathogenic specific protein, is regarded as a pivotal determinant in classifying E. coli strains as UPEC [65]. Therefore, the detection of the gene coding for Usp among the collected isolates was performed using PCR as previously discussed [66]. The following primers, obtained from Bio Basic Inc., Canada were used: usp-forward (5’-ACATTCACGGCAAGCCTCAG-3’) and usp-reverse (5’-AGCGAGTTCCTGGTGAAAGC-3’). The obtained PCR products were separated by gel electrophoresis in the presence of a 100-bp DNA ladder (GeneDireX RTU, Taiwan, yielding 11 fragments: 100–1500 bp). The bands were visualized on a 254 nm UV transilluminator (Entela UVP Upland CA 91,786, USA).
Suppression of quorum sensing-regulated virulence factors by phytochemicals
The ability of CaRV, CiNN, and EG to inhibit the QS-mediated swimming and twitching motilities, as well as the biofilm-forming ability, was investigated in the usp-positive E. coli isolates.
Swimming and twitching motilities assay
Swimming motility was assayed using 0.3% agar plates supplemented with 1% tryptone (Oxoid, Hampshire, UK) and 0.25% NaCl while twitching motility was experimented using LB broth containing 1% agar (B&V Srl, Italy), as previously described [43, 67]. CaRV, CiNN, EG, or DMSO (control) were added to the motility agar plates. The phytochemicals were incorporated at a subinhibitory concentration equivalent to 0.5XMIC of the agent calculated based on the MIC values for each isolate. For the swimming assay, aliquots of 1 µL of UPEC isolates grown to an OD600 of 1.0 were placed at the center of motility plates with or without the tested agents using sterilized micropipette tips. Diameters of swimming halos were measured following incubation at 37 °C for 24 h. In the twitching assay, a colony of each of the tested isolates was deeply stabbed using a sterile toothpick into the prepared plates with or without the phytochemicals in a way to touch the agar–dish interface. After incubation at 37 °C for 48 h, agar was removed and the adhered cells on the dish were stained with 1% (w/v) crystal violet solution. The violet-stained diameters were then accurately measured. E. coli ATCC 8739 and PAO1 were included in the tests as quality control strains.
Crystal violet biofilm formation assay at 30 and 37 °C
The UTIs acquired in hospitals are mostly caused by using urinary catheters. Since the temperature may vary along the length of the catheters, where the collection bag is held at room temperature, the tubing is outside the urinary tract and closer to the skin, while the tip and initial tubing, being inserted in the bladder and the urethra, are subjected to body temperature, 37 °C. This variation in temperatures triggers the concern that UPEC may form biofilm at any part along the catheter. Therefore, the ability of the isolates to form biofilm at 37 ºC and 30 ºC was assessed using the microtiter plate assay as previously described with slight modifications [68]. Briefly, an inoculum of 200 µL of the overnight culture of each of the UPEC strains in nutrient broth (NB, Oxoid, Hampshire, UK) when testing at 37 ºC, or in LB broth when testing at 30 ºC, at an OD600 of 0.05 was introduced into a flat-bottomed 96-well microtiter plate (Sigma-Aldrich, USA) and incubated at 37 or 30 ºC for 48 h. To quantify the formed biofilms, they were stained for 10 min with crystal violet 0.2% (w/v), rinsed three times with distilled water, and extracted with 30% glacial acetic acid (or 95% ethanol in the assay at 30 ºC). Absorbances were measured at 630 nm, and results were expressed as the averages of three replicate wells. Subsequently, isolates that recorded an OD630 above 0.1 (2X ODc) indicating moderate to strong biofilm formation at both temperatures under test were investigated in the presence of the phytoconstituents at concentrations corresponding to 0.5XMIC, where a volume of 100 µL of an overnight culture of each of the UPEC isolates was added to 100 µL of the suitable culture media and incubated for 48 h. The procedure was then followed as mentioned above.
Quantitative real-time PCR assay
For transcriptomic analysis, qRT-PCR was used to investigate the effect of CaRV, CiNN, and EG on the expression levels of the QS gene (luxS) and the virulence genes known to be modulated by QS (csgA, fimA, and fliC). Cultures of selected isolates were grown in LB broth for 48 h in the presence and absence of the agents at concentrations equivalent to 0.5XMIC. Bacterial pellets were harvested by centrifugation at 6000 rpm for 5 min at 4 ºC. Total RNA was extracted from treated and untreated cells using Biozol reagent™ (Bioflux, China) as per the manufacturer’s protocol and its concentration was adjusted by nanodrop (Thermo Fisher, USA). cDNA was synthesized using TOPscript™ RT DryMix (Enzynomics, South Korea) and then was quantified by qPCR using TOPreal™ SYBR® Green Premix (Enzynomics, South Korea) in Rotor-Gene Q Real-Time PCR system (Qiagen, Germany) with the primer pairs described in Online Resource Additional file 5. Each reaction mixture contained 1 µL of cDNA, 10 µL of SYBR® Green Premix, 1 µL of 10 µM of each primer, and 7 µL of nuclease-free water. To normalize the expression levels of the target genes, gapA was used as internal control and the relative gene expression was calculated according to Pfaffl method (2−∆∆Ct) [45]. The experiment was performed in triplicates and the results were denoted in terms of fold change.
Checkerboard assays
The combined activity of CaRV, CiNN, and EG with ceftriaxone, ciprofloxacin, colistin, doxycycline, and tigecycline was analyzed by checkerboard assays against 3 UPEC isolates in 96-well microtiter plates. A volume of 50 µL of two-fold serial dilutions of the tested agents in 30% DMSO was introduced to each well of each row, whereas serial dilutions of the antibiotics were added to each well of each column. An overnight bacterial culture matching the turbidity of 0.5 McFarland was 100-fold diluted in double strength CAMH broth and a volume of 100 µL was inoculated into the checkerboard plates which were then incubated at 37 ºC for 24 h [69]. The FIC index was calculated to investigate the combined effect of the agents and antibiotics using the following equation: FIC of agent = MIC in combination/MIC alone, FIC index = FIC of antibiotic + FIC of phytochemical. For interpretation, an FIC index ≤ 0.5, denoted synergy; 0.5 < FIC index ≤ 0.75, indicated partial synergy; 0.76 < FIC index ≤ 1, designated additive effect; 1 < FIC index ≤ 4, showed an indifferent effect; while an FIC index > 4, referred to antagonism [70].
Statistical analysis
Statistical analyses were carried out using SPSS version 25.0 (SPSS, Chicago, IL). The pairwise correlation analysis of the resistance against selected antibiotics, as well as qRT-PCR results, were evaluated using Pearson’s correlation coefficient. One-way ANOVA followed by Bonferroni testing were conducted for multi-variable comparison. Differences in this study were considered significant at p < 0.05.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- AMUH:
-
Alexandria Main University Hospital
- AMR:
-
antimicrobial resistance
- AI-2:
-
autoinducer-2
- CAMH:
-
cation-adjusted Mueller–Hinton
- CaRV:
-
carvacrol
- CiNN:
-
cinnamaldehyde
- CLSI:
-
Clinical Laboratory Standards Institute
- DMSO:
-
dimethyl sulfoxide
- EG:
-
eugenol
- FIC:
-
fractional inhibitory concentration
- LB:
-
Luria‐Bertani broth
- MIC:
-
minimum inhibitory concentration
- MDR:
-
multidrug-resistant
- NB:
-
nutrient broth
- QS:
-
quorum sensing
- QSIs:
-
quorum sensing inhibitors
- UTIs:
-
urinary tract infections
- UPEC:
-
uropathogenic Escherichia coli
References
Zagaglia C, Ammendolia MG, Maurizi L, Nicoletti M, Longhi C. Urinary tract Infections caused by uropathogenic Escherichia coli strains_new strategies for an old Pathogen. Microorganisms. 2022;10(7):1425.
Rozwadowski M, Gawel D. Molecular factors and mechanisms driving multidrug resistance in uropathogenic Escherichia coli—An update. Genes. 2022;13(8):1397.
Klein RD, Hultgren SJ. Urinary tract Infections: microbial pathogenesis, host–pathogen interactions and new treatment strategies. Nat Rev Microbiol. 2020;18(4):211–26.
Zakaria AS, Edward EA, Mostafa NM. Genomic insights into a colistin-resistant uropathogenic Escherichia coli strain of O23:H4-ST641 lineage harboring mcr-1.1 on a conjugative IncHI2 plasmid from Egypt. Microorganisms. 2021;9(4):799.
Moghnieh RA, Kanafani ZA, Tabaja HZ, Sharara SL, Awad LS, Kanj SS. Epidemiology of common resistant bacterial pathogens in the countries of the Arab League. Lancet Infect Dis. 2018;18(12):e379–e94.
El-Kholy A, El-Mahallawy HA, Elsharnouby N, Abdel Aziz M, Helmy AM, Kotb R. Landscape of multidrug-resistant gram-negative Infections in Egypt: survey and literature review. Infect Drug Resist. 2021;14:1905–20.
Terlizzi ME, Gribaudo G, Maffei ME. UroPathogenic Escherichia coli (UPEC) Infections: virulence factors, bladder responses, antibiotic, and non-antibiotic antimicrobial strategies. Front Microbiol. 2017;8(1664–302X):1566.
O’Rourke K, Cadieux PA. Pathogenic mechanisms of Uropathogens. In: Lange D, Scotland KB, editors. The role of Bacteria in Urology. Cham: Springer; 2019. pp. 23–39.
Chadha J, Harjai K, Chhibber S. Revisiting the virulence hallmarks of Pseudomonas aeruginosa: a chronicle through the perspective of quorum sensing. Environ Microbiol. 2022;24(6):2630–56.
Saeki EK, Kobayashi RKT, Nakazato G. Quorum sensing system: target to control the spread of bacterial Infections. Microb Pathog. 2020;142:104068.
Zhao X, Yu Z, Ding T. Quorum-sensing regulation of antimicrobial resistance in bacteria. Microorganisms. 2020;8(3):425.
Escobar-Muciño E, Arenas-Hernández MMP, Luna-Guevara ML. Mechanisms of inhibition of quorum sensing as an alternative for the control of E. Coli and Salmonella. Microorganisms. 2022;10(5):884.
Bartoletti R, Cai T, Wagenlehner FM, Naber K, Johansen TEB. Treatment of urinary tract Infections and antibiotic stewardship. Eur Urol Supplements. 2016;15(4):81–7.
Ahmed SS, Shariq A, Alsalloom AA, Babikir IH, Alhomoud BN. Uropathogens and their antimicrobial resistance patterns: relationship with urinary tract Infections. Int J Health Sci. 2019;13(2):48–55.
Chadha J, Harjai K, Chhibber S. Repurposing phytochemicals as anti-virulent agents to attenuate quorum sensing-regulated virulence factors and biofilm formation in Pseudomonas aeruginosa. Microb Biotechnol. 2022;15(6):1695–718.
Bai AJ, Rai VR. Quorum sensing inhibitors from phytochemicals and food sources and their potential applications in food quality. In: Shetty K, Sarkar D, editors. Functional foods and biotechnology: Biotransformation and analysis of functional foods and ingredients. CRC Press; 2020. pp. 426–44.
Gopu V, Meena CK, Shetty PH. Quercetin influences quorum sensing in food borne bacteria: In-vitro and in-silico evidence. PLoS ONE. 2015;11(1):e0134684.
Kahlmeter G, Menday P. Cross-resistance and associated resistance in 2478 Escherichia coli isolates from the pan-european ECO·SENS Project surveying the antimicrobial susceptibility of pathogens from uncomplicated urinary tract Infections. J Antimicrob Chemother. 2003;52(1):128–31.
Abu El-Wafa WM, Ibrahim YM. In vitro activity of fosfomycin in double and triple combinations with imipenem, ciprofloxacin and tobramycin against multidrug-resistant Escherichia coli. Curr Microbiol. 2020;77(5):755–61.
Rezatofighi SE, Mirzarazi M, Salehi M. Virulence genes and phylogenetic groups of uropathogenic Escherichia coli isolates from patients with urinary tract Infection and uninfected control subjects: a case-control study. BMC Infect Dis. 2021;21(1):361.
Cheung DA, Nicholson A, Butterfield TR, DaCosta M. Prevalence, co-infection and antibiotic resistance of Escherichia coli from blood and urine samples at a hospital in Jamaica. JIDC. 2020;14(02):146–52.
Ahmad S, Ali F, Qureshi SA, Uzma B, Shakeela Q, Sabir MS, et al. The evaluation of antibiotic susceptibility pattern and associated risk factors of UTI in tertiary care hospital of Peshawar. Pak J Pharm Sci. 2022;35(3):897–903.
Ramalan AS, Joseph FN, Owoseni MC, Ya’aba Y, Chuku A. Prevalence and antibiotic resistance profile of Staphylococcus aureus and Eschericia Coli among patients attending urology clinic of Dalhatu Araf specialist hospital (DASH) Lafia, Nasarawa State, Nigeria. BAJOPAS. 2021;13(1):80–9.
Vasudevan R. Urinary tract Infection: an overview of the Infection and the associated risk factors. J Microbiol Exp. 2014;1(2):42–51.
Masoud SM, Abd El-Baky RM, Aly SA, Ibrahem RA. Prevalence of multidrug resistant Escherichia coli recovered from patients suffering from urinary tract Infections. NRMJ. 2022;6(2):1543–56.
Gawad WE, Helmy OM, Tawakkol WM, Hashem AM. Antimicrobial resistance, biofilm formation, and phylogenetic grouping of uropathogenic Escherichia coli isolates in Egypt: the role of efflux pump-mediated resistance. Jundishapur J Microbiol. 2018;11(2):e14444.
Abdel-Moaty MM, Ws M, Abdel-All SM, El-Hendawy HH. Prevalence and molecular epidemiology of extended spectrum β-lactamase producing Escherichia coli from hospital and community settings in Egypt. J Appl Pharmaceut Sci. 2016;6(1):042–7.
Ayandele AA, Oladipo EK, Oyebisi O, Kaka MO. Prevalence of multi-antibiotic resistant Escherichia coli and Klebsiella species obtained from a tertiary medical institution in Oyo State, Nigeria. Qatar Med J. 2020;2020(1):9.
Iskandar K, Molinier L, Hallit S, Sartelli M, Catena F, Coccolini F, et al. Drivers of antibiotic resistance transmission in low- and middle-income countries from a one health perspective—A review. Antibiotics. 2020;9(7):372.
Mahmoud AT, Salim MT, Ibrahem RA, Gabr A, Halby HM. Multiple drug resistance patterns in various phylogenetic groups of hospital-acquired uropathogenic E. Coli isolated from cancer patients. Antibiotics. 2020;9(3):108.
Patel G, Bonomo R. Stormy waters ahead: global emergence of carbapenemases. Front Microbiol. 2013;4:1–17.
Mohamed NM, Zakaria AS, Edward EA. Genomic characterization of international high-risk clone ST410 Escherichia coli Co-harboring ESBL-encoding genes and blaNDM-5 on IncFIA/IncFIB/IncFII/IncQ1 multireplicon plasmid and carrying a chromosome-borne blaCMY-2 from Egypt. Antibiotics. 2022;11(8):1031.
Shahbazi S, Karam MR, Habibi M, Talebi A, Bouzari S. Distribution of extended-spectrum β-lactam, quinolone and carbapenem resistance genes, and genetic diversity among uropathogenic Escherichia coli isolates in Tehran, Iran. J Glob Antimicrob Resist. 2018;14:118–25.
Bien J, Sokolova O, Bozko P. Role of uropathogenic Escherichia coli virulence factors in development of urinary tract Infection and kidney damage. Int J Nephrol. 2012;2012:681473.
Chadha J, Ravi R, Singh J, Chhibber S, Harjai K. Gentamicin augments the quorum quenching potential of cinnamaldehyde in vitro and protects Caenorhabditis elegans from Pseudomonas aeruginosa Infection. Front Cell Infect Microbiol. 2022;12:899566.
Niu C, Afre S, Gilbert ES. Subinhibitory concentrations of cinnamaldehyde interfere with quorum sensing. Lett Appl Microbiol. 2006;43(5):489–94.
Hong X, Wang Y, Chen S, Zhu J. Efficacy of ten structurally related essential Oil Components on Anti-biofilm and Anti-quorum sensing against Fish spoilers Pseudomonas and Aeromonas. J Aquat Food Prod Technol. 2021;30(4):462–73.
Tapia-Rodriguez MR, Hernandez-Mendoza A, Gonzalez-Aguilar GA, Martinez-Tellez MA, Martins CM, Ayala-Zavala JF. Carvacrol as potential quorum sensing inhibitor of Pseudomonas aeruginosa and biofilm production on stainless steel surfaces. Food Control. 2017;75:255–61.
Lou Z, Letsididi KS, Yu F, Pei Z, Wang H, Letsididi R. Inhibitive effect of eugenol and its nanoemulsion on quorum sensing–mediated virulence factors and biofilm formation by Pseudomonas aeruginosa. J Food Prot. 2019;82(3):379–89.
Li S, Zhou S, Yang Q, Liu Y, Yang Y, Xu N, et al. Cinnamaldehyde decreases the pathogenesis of Aeromonas hydrophila by inhibiting Quorum sensing and Biofilm formation. Fishes. 2023;8(3):122.
Kim YG, Lee JH, Gwon G, Kim SI, Park JG, Lee J. Essential oils and eugenols inhibit biofilm formation and the virulence of Escherichia coli O157:H7. Sci rep. 2016;6:36377.
Kim Y, Kim S, Cho K-H, Lee J-H, Lee J. Antibiofilm activities of cinnamaldehyde analogs against uropathogenic Escherichia coli and Staphylococcus aureus. Int J Mol Sci. 2022;23(13):7225.
Lee JH, Kim YG, Lee J. Carvacrol-rich oregano oil and thymol‐rich thyme red oil inhibit biofilm formation and the virulence of uropathogenic Escherichia coli. J Appl Microbiol. 2017;123(6):1420–8.
Niu C, Gilbert E. Colorimetric method for identifying plant essential oil components that affect biofilm formation and structure. Appl Environ Microbiol. 2004;70(12):6951–6.
Yuan W, Yuk H-G. Effects of sublethal thymol, carvacrol, and trans-cinnamaldehyde adaptation on virulence properties of Escherichia coli O157: H7. Appl Environ Microbiol. 2019;85(14):e00271–19.
Goh SN, Fernandez A, Ang S, Lau W, Ng D, Cheah E. Effects of different amino acids on biofilm growth, swimming motility and twitching motility in Escherichia coli BL21. J Biol Life Sci. 2013;4(2):103–15.
Zhang Y, Kong J, Xie Y, Guo Y, Cheng Y, Qian H et al. Essential oil components inhibit biofilm formation in Erwinia carotovora and Pseudomonas fluorescens via anti-quorum sensing activity. LWT - Food Science and Technology. 2018;92:133-9.
Uhlich G, Chen CY, Cottrell B, Nguyen LH. Growth media and temperature effects on biofilm formation by serotype O157:H7 and non-O157 shiga toxin-producing Escherichia coli. FEMS Microbiol Lett. 2014;354(2):133–41.
Leech J, Golub S, Allan W, Simmons M, Overton T. Non-pathogenic Escherichia coli biofilms: effects of growth conditions and surface properties on structure and curli gene expression. Arch Microbiol. 2020;202(6):1517–27.
Wurpel D, Totsika M, Allsopp L, Hartley-Tassell L, Day C, Peters K, et al. F9 fimbriae of uropathogenic Escherichia coli are expressed at low temperature and recognise Galβ1-3GlcNAc-containing glycans. PLoS ONE. 2014;9(3):e93177.
Henly EL, Norris K, Rawson K, Zoulias N, Jaques L, Chirila PG, et al. Impact of long-term quorum sensing inhibition on uropathogenic Escherichia coli. J Antimicrob Chemother. 2021;76(4):909–19.
Kim Y-G, Lee J-H, Kim S-I, Baek K-H, Lee J. Cinnamon bark oil and its components inhibit biofilm formation and toxin production. Int J Food Microbiol. 2015;195:30–9.
Reichling J. Anti-biofilm and virulence factor-reducing activities of essential oils and oil components as a possible option for bacterial Infection control. Planta Med. 2020;86(08):520–37.
Sharifi A, Nayeri Fasaei B. Selected plant essential oils inhibit biofilm formation and luxS and pfs-mediated quorum sensing by Escherichia coli O157:H7. Lett Appl Microbiol. 2022;74(6):916–23.
Narayanan A, Muyyarikkandy MS, Mooyottu S, Venkitanarayanan K, Amalaradjou MAR. Oral supplementation of trans-cinnamaldehyde reduces uropathogenic Escherichia coli colonization in a mouse model. Lett Appl Microbiol. 2017;64(3):192–7.
Mith H, Clinquart A, Zhiri A, Daube G, Delcenserie V. The impact of oregano (Origanum heracleoticum) essential oil and carvacrol on virulence gene transcription by Escherichia coli O157: H7. FEMS Microbiol Lett. 2015;362(1):1–7.
Ibrahim MO, Al Meani SAL. Detection of plasmid-mediated AMPC β-lactamase genes and evaluation the synergistic effect of clove volatile oil and antibiotics in clinical isolates of klebsiella pneumoniae in Iraq. Biochem Cell Arch. 2019;19(2):4053–61.
Vázquez-Ucha JC, Martínez-Guitián M, Lasarte-Monterrubio C, Conde-Pérez K, Arca-Suárez J, Álvarez-Fraga L, et al. Syzygium aromaticum (clove) and Thymus zygis (thyme) essential oils increase susceptibility to colistin in the nosocomial pathogens Acinetobacter baumannii and Klebsiella pneumoniae. Biomed Pharmacother. 2020;130:110606.
Valcourt C, Saulnier P, Umerska A, Zanelli MP, Montagu A, Rossines E, et al. Synergistic interactions between doxycycline and terpenic components of essential oils encapsulated within lipid nanocapsules against Gram negative bacteria. Int J Pharm. 2016;498(1):23–31.
Dhara L, Tripathi A. The use of eugenol in combination with cefotaxime and ciprofloxacin to combat ESBL-producing quinolone‐resistant pathogenic Enterobacteriaceae. J Appl Microbiol. 2020;129(6):1566–76.
Kachur K, Suntres Z. The antibacterial properties of phenolic isomers, carvacrol and thymol. Crit Rev Food Sci Nutr. 2020;60(18):3042–53.
Bhardwaj M, Singh B, Sinha D, Or V, Vadhana P, Singh S, et al. Evaluation of carvacrol as an antibacterial agent against Escherichia coli isolated from different animal species. J Entomol Zool Stud. 2019;7:911–4.
Masoud SM, Abd El-Baky RM, Aly SA, Ibrahem RA. Co-existence of certain ESBLs, MBLs and plasmid mediated quinolone resistance genes among MDR E. Coli isolated from different clinical specimens in Egypt. Antibiotics. 2021;10(7):835.
Wijesundara NM, Lee SF, Cheng Z, Davidson R, Rupasinghe HPV. Carvacrol exhibits rapid bactericidal activity against Streptococcus pyogenes through cell membrane damage. Sci Rep. 2021;11(1):1487.
Zakaria AS, Edward EA, Mohamed NM. Pathogenicity islands in uropathogenic Escherichia coli clinical isolate of the globally disseminated O25:H4-ST131 pandemic clonal lineage: first report from Egypt. Antibiotics. 2022;11(11):1620.
Ahmed N, Zeshan B, Naveed M, Afzal M, Mohamed M. Antibiotic resistance profile in relation to virulence genes fimH, hlyA and usp of uropathogenic E. Coli isolates in Lahore, Pakistan. Trop Biomed. 2019;36(2):559–68.
Seleem NM, Abd El Latif HK, Shaldam MA, El-Ganiny A. Drugs with new lease of life as quorum sensing inhibitors: for combating MDR Acinetobacter baumannii Infections. Eur J Clin Microbiol. 2020;39(9):1687–702.
Javed S, Mirani ZA, Pirzada ZA. Phylogenetic group B2 expressed significant biofilm formation among drug-resistant uropathogenic Escherichia coli. Libyan J Med. 2021;16(1):1845444.
Wang Y-m, Kong L-c, Liu J, Ma H-x. Synergistic effect of eugenol with Colistin against clinical isolated colistin-resistant Escherichia coli strains. Antimicrob Resist Infect Control. 2018;7(1):1–9.
Abozahra R, Gaballah A, Abdelhamid SM. Prevalence of the colistin resistance gene MCR-1 in colistin-resistant Klebsiella pneumoniae in Egypt. AIMS Microbiol. 2023;9(2):177–94.
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
HAM: Methodology, validation, data curation, and writing - original draft. HMO: Conceptualization, validation, reviewing and editing. ASZ.: Conceptualization, validation, data curation, preparation of figures, writing – reviewing, and editing. NMM: Conceptualization, validation, data curation, writing – review and editing. The first draft of the manuscript was written by NMM and HAM. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The urine samples were collected by the routine laboratory facility of Alexandria Main University Hospital, E. coli isolates were provided anonymously and used in this study. No specimens were collected from patients under the age of 16. The authors did not have any contact with the patients. The informed consent was waived by the Ethics Committee of Alexandria University, Faculty of Medicine which granted the approval for the study under IRB number: 00012098 and the Federal Wide Assurance FWA number: 00018699 (Date: 9/4/2023) (http://www.hhs.gov/ohrp/assurances/index.html).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Morgaan, H.A., Omar, H.M., Zakaria, A.S. et al. Repurposing carvacrol, cinnamaldehyde, and eugenol as potential anti-quorum sensing agents against uropathogenic Escherichia coli isolates in Alexandria, Egypt. BMC Microbiol 23, 300 (2023). https://doi.org/10.1186/s12866-023-03055-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-023-03055-w