Abstract
Background
Sepsis is one of the leading causes of death in ICU patients. Fluid resuscitation is the main target in septic patients. Proper fluid administration is needed in septic patients to overcome generalized vasodilatation and capillary leak, this capillary leak itself may cause tissue edema and worsen septic patients. On the other hand, vasopressors may improve tissue perfusion or worsen tissue hypoxia. Therefore, predictors for fluid responsiveness are urgently needed. However, many studies have found static indicators useless. That is why dynamic predictors for fluid responsiveness are attracting growing interest to optimize patients.
Our goal is to assess the predictive power of internal jugular vein distensibility index and inferior vena cava collapsibility index for fluid responsiveness in spontaneously breathing septic patients.
Forty adult septic patients were enrolled from a single university teaching hospital’s ICU. We measured the Internal jugular distensibility index (IJV-DI) and Inferior vena cava collapsibility index (IVC-CI) in spontaneously breathing septic patients. Patients were considered responders if they had a change in cardiac index (≥ 15%) after fluid resuscitation with 7 ml/kg crystalloid. The main outcome measure is predictive power of Internal jugular vein distensibility index and Inferior vena cava collapsibility index.
Results
Data from 40 spontaneously breathing septic patients were analyzed. Sixty percent of the patients were fluid responder. The areas under curve of receiver operating characteristic for Internal jugular vein distensibility index and Inferior vena cava collapsibility index to predict fluid responsiveness were 0.96 and 0.97, respectively. IJV-DI (> 17.56%) was predictive of fluid responsiveness with 95.83% sensitivity and 87.5% specificity. IVC-CI (> 35%) was predictive of fluid responsiveness with 95.8% sensitivity and 93.7% specificity.
Conclusions
Both IJV-DI and IVC-CI have near good predictive value for fluid responsiveness in spontaneously breathing septic patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Sepsis is one of the leading causes of death in ICU patients. The main target in septic patients is fluid resuscitation, but optimal fluid resuscitation for each patient is the true question. Proper fluid administration is needed in septic patients to overcome generalized vasodilatation and capillary leak; this capillary leak itself may cause tissue edema and worsen septic patients (Sakr et al., 2017). Vasopressors may be needed to overcome this crucial vasodilatation, but they may also cause tissue hypoperfusion and hypoxia (Wiedemann et al., 2006).
Improving oxygen delivery and hemodynamic optimization by intravenous fluids is a cornerstone in treating septic patients. However, if not monitored, it may be useless or even harmful. This emphasizes the need for an approach to assess who will benefit from fluid administration (Cumpstey et al., 2020).
(Wise et al., 2017) stated that central venous pressure, systolic pressure, and other static predictors are of no value as predictors for fluid responsiveness (Wise et al., 2017). Therefore, it is very important to define noninvasive dynamic tools for fluid resuscitation prediction (Haas et al., 2012).
Our goal is to determine whether the internal jugular vein distensibility index and inferior vena cava collapsibility index are good dynamic predictors for fluid responsiveness or not.
Methods
Ethics
Ethical approval for this study (FMASU MD 262/2019) was provided by the Ethics committee of Ain Shams University Hospital, Abbasia, Cairo, Egypt (Chairperson Prof F. Tash) on 1/9/2019. Written informed consent was obtained from all subjects or their caregivers.
Inclusion criteria
We enrolled 40 spontaneously breathing septic adult patients according to the surviving sepsis campaign (http://www.survivingsepsis.org/Pages/default.aspx, 2019).
Exclusion criteria:
Patients were excluded based on the following:
-
1.
Patients’ refusal
-
2.
Non-echogenicity
-
3.
Mechanical ventilation
-
4.
Severe cardiac conditions
-
5.
Severe respiratory conditions
-
6.
Vein thrombosis
-
7.
Patient on vasopressors or inotropes
-
8.
Morbidly obese patients
-
9.
Patients with acute signs of hemorrhage
-
10.
Evidence of fluid overload
-
11.
Renal dysfunction
Patients’ recruitment
Patients were recruited randomly from critical care units at Ain Shams University Hospitals, on condition that they meet our criteria of inclusion.
Procedure and technique
All hemodynamic measurements (heart rate and mean blood pressure), ultrasound measures IVC-CI (inferior vena cava collapsibility index) and IJV-DI (internal jugular vein distensibility index) and Echo measures COP (cardiac output) and CI (cardiac index) were recorded at the beginning of the study on each patient after a 30-min volume expansion with a 7-ml/kg crystalloid infusion (Ringer Acetate) in the flat supine position. The vivid ultrasound system of GE Healthcare was used for ultrasound and echo measures.
The diameter (D) of aortic annulus was measured using parasternal long-axis view to get the aortic cross-sectional area through the equation = (D2 × 3.14)/4. Then, the aortic cross-sectional area was multiplied by velocity time integral (VTI) (which is the distance a column of blood travels through the aortic annulus with each stroke) to get the stroke volume. It is then multiplied by heart rate to get the cardiac output (Desai & Garry, 2018).
Measuring the velocity time integral was conducted by obtaining the apical five-chamber view (where the proximal aorta, aortic valve, and left ventricular outflow tract come in the view) (Matta et al., 2019). For the best flow estimation, the probe of echo is positioned 15° to the left ventricular outflow tract just near the aortic valve (Miller & Mandeville, 2016).
Patients were considered fluid responders if the change in cardiac index (ΔCI) was ≥ 15% after fluid resuscitation. The cardiac index was calculated by dividing measured cardiac output by body surface area (Guarracino et al., 2014).
The inferior vena cava diameter was estimated through a subcostal view approach using M-mode. The maximum and minimum diameters were measured during expiration and inspiration of the same respiratory cycle. The inferior vena cava collapsibility index was calculated according to the equation (Zhao & Wang, 2016):
The internal jugular vein diameter was estimated by placing the probe transversely on the right internal jugular vein on the right side of the neck, 2 cm above the sternoclavicular joint. It is important not to compress the vein by applying minimal pressure and to record the measurements only when the whole circumference of the vein is visible. Measurements of maximum and minimum diameter were taken during expiration and inspiration of the same respiratory cycle, and the internal jugular vein distensibility index was calculated according to the equation (Guarracino et al., 2014):
Patient-reported outcomes
The primary outcome was to assess the internal jugular vein distensibility index and inferior vena cava collapsibility index as dynamic predictors for fluid responsiveness.
Secondary aim
The secondary aim is to define the predictive value of other tools as predictors of fluid responsiveness, such as
-
1.
Heart rate
-
2.
Cardiac output
-
3.
Mean blood pressure
Statistical analysis
The sample size was calculated using PASS11 program for sample size calculation, a sample of 40 patients achieved 80% power to detect a change in sensitivity from 50 to 80% for IJV distensibility and 99% power to detect a change in sensitivity from 50 to 90% for IVC collapsibility, assuming that the proportion of responders = 50%. The target significance level is 0.05.
Statistical methods
Data were analyzed using the Statistical Package for Social Science (SPSS) version 22.0. Quantitative data were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage.
Results
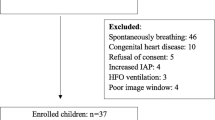
A total of 55 patients were assessed for eligibility. Ten patients did not meet the inclusion criteria, and 5 patients were excluded from the study analysis due to bad echogenicity. The study was conducted on 40 patients; we divided them into two groups (24 responders and 16 nonresponders). All patients were monitored with ECG and noninvasive blood pressure. All measures were recorded in the flat supine position. Patients in our study were considered responders if the increase in the cardiac index is 15% or more after 30 min of fluid resuscitation with 7 ml/kg of crystalloid (Ringer Acetate). Demographic data are shown in the following table (Table 1).
There was no significant difference between responders and nonresponders regarding age, sex, and weight.
After plotting the receiver operating characteristic curve for the predictors of fluid responsiveness, we found that the inferior vena cava collapsibility index had sensitivity and specificity of 95.8% and 93.7%, respectively, for cutoff value > 35%, while the internal jugular vein distensibility index had sensitivity and specificity of 95.83% and 87.5%, respectively, for cutoff value > 17.56% (Table 2).
Moreover, the mean arterial blood pressure showed sensitivity of 75% and specificity of 100% for cutoff value ≤ 52 mmHg, while cardiac output showed sensitivity of 83.3% and specificity of 93.7% for cutoff value ≤ 7.65 l/min. On the other hand, heart rate did not appear to be a tool of value for fluid responsiveness.
The study showed a positive correlation between IVC-CI and IJV-DI and between cardiac output and mean arterial blood pressure. On the other hand, it showed negative correlation between IVC-CI, cardiac output, and mean arterial blood pressure and between IJV-DI, cardiac output, and mean arterial blood pressure (Table 3), Fig. 1.
Discussion
Our findings demonstrate the value of the internal jugular vein distensibility index and the inferior vena cava collapsibility index in predicting fluid responsiveness in spontaneously breathing septic patients.
The main issue facing septic patients is circulatory failure which is often the result of hypovolemia, profound vasodilatation, or both. Therefore, volume expansion may be beneficial in improving tissue perfusion and prognosis or hazardous in causing volume overload and worsening previous cardiac condition or gas exchange. The use of vasopressors may limit vigorous vasodilatation and improve tissue perfusion or cause tissue hypoxia and worsen the condition (Wiedemann et al., 2006).
Static hemodynamic parameters have been found to be of little clinical value by many studies if compared to dynamic parameters in predicting fluid responsiveness (Preisman et al., 2005; Osman et al., 2007). Dynamic predictors for fluid responsiveness are more precise, but some of them are invasive procedures (Theerawit et al., 2016; Guerin et al., 2013).
Ultrasound has become one of the cornerstones of modern ICU. It can be used in daily ICU practice to measure the different dynamic predictors of fluid responsiveness (Theerawit et al., 2016; Orso et al., 2016), such as inferior vena cava collapsibility index (variation of IVC diameter with respiration) (Barbier et al., 2004; Feissel et al., 2004) and internal jugular vein distensibility index to differentiate between fluid responders and nonresponders (Guarracino et al., 2014).
Any pressure or volume change in the intrathoracic systemic venous system is reflected in the extrathoracic system, such as the inferior vena cava and the internal jugular vein (Chiaco et al., 2013).
This observational cross-sectional study has been conducted for 1 year in the ICU. Collected data from 40 patients were analyzed for reaching the final results. We studied IVC-CI and IJV-DI in terms of their reliability and effectiveness as simple bedside noninvasive dynamic tools to define fluid responsiveness in spontaneously breathing septic patients.
Our study demonstrated that changes in the internal jugular vein and the inferior vena cava accompanied with respiration are well-correlated with fluid responsiveness.
Patients in our study were defined as responders when their CI increased by 15% or more after 30 min of fluid resuscitation with 7 ml/kg crystalloid (Ringer Acetate). The responders represented 60% of the cases.
Our study found that the inferior vena cava collapsibility index (IVC-CI) > 35% was a good tool to predict fluid responsiveness with AUC 0.97, revealing sensitivity of 95.8% and specificity of 93.7% with positive predictive value of 95.8 and negative predictive value of 93.7 (p value < 0.001) and 95% confidence interval from 0.861 to 0.999.
Furthermore, our study revealed that the internal jugular vein distensibility index (IJV-DI) > 17.65% was a good predictor for fluid responsiveness with AUC 0.969, revealing sensitivity of 95.83% and specificity of 87.5% with positive predictive value of 92 and negative predictive value of 93.3 (p value < 0.001) and 95% confidence interval from 0.859 to 0.999.
Regarding the inferior vena cava collapsibility index, in line with our study, Caplan et al. (Caplan et al., 2020) (who studied the effect of the site of measurement of IVC readings), confirmed the predictive power of IVC variability of fluid responsiveness in spontaneously breathing septic patients. They collected data from 81 patients. Patients were considered responders with increased SVI (systolic volume index) > 10% after intravenous administration of 500 ml of 4% Gelatin. They found that 4 cm from the right atrium–ivc junction is the best site to measure IVC with AUC 0.85, cutoff value of 33%, sensitivity of 66%, and specificity of 92% (Caplan et al., 2020).
In the same context, Pereira et al. (Pereira et al., 2020) compared pulse pressure variation (ppv) and IVC variation as predictors for fluid responsiveness in surgical patients. They conducted their study on 22 patients and stated that patients with ppv > 13% were considered fluid responsive. They also discovered that IVC variation had strong predictive value with cutoff value > 40%, AUC 0.98, sensitivity of 100%, and specificity of 93.3% for the IVC collapsibility index (Pereira et al., 2020).
Furthermore, Sanchez et al. (Sánchez et al., 2021) collected data from 33 studies conducted on 1352 patients to assess predictors for fluid responsiveness in mechanically ventilated patients at tidal volume ≤ 8 ml/kg. They found that IVC variation strongly predicts fluid responsiveness with AUC 0.86, sensitivity of 77%, and specificity of 87% at cutoff value of 16%. Their low cutoff value could be explained because it was conducted on mechanically ventilated patients, and different calculation equations were used (IVCmax − IVCmin/IVCmin) (Sánchez et al., 2021).
On the other hand, Pinar et al. (Pınar et al., 2020) measured the effectiveness of end-tidal carbon dioxide and inferior vena cava variation to assess fluid responsiveness in 31 spontaneously breathing patients. Patients were considered fluid responsive (15 patients) if cardiac output increased by > 15% after passive leg raising. They discovered that end-tidal carbon dioxide would be a good predictive, while IVC variation did not show a significant difference between responders and nonresponders with AUC 0.50 and 95% CI 0.32–0.69. The decision of the patients who required IV fluid treatment was at the discretion of the treating physicians, thus explaining the discordant results between the studies. Different treatment strategies of the treating physicians can affect the homogeneity of the study population (Pınar et al., 2020).
Moreover, Yao et al. (Yao et al., 2019) in a study on 67 mechanically ventilated patients compared IVC variation and IVC diameter ratio as predictors for fluid responsiveness. They concluded that IVC variation had weak correlation with fluid responsiveness, with AUC 0.68 and 95% CI 0.56–0.81, but they claimed that the reason for their results is the usage of assisted ventilation modalities. In the assisted ventilation modality, there is a variable contribution to inspiration because the unpredictable interplay of ventilator-generated positive pressure and patient-generated negative pressure confusingly influence the IVC. Additionally, because of the lung-protective ventilation strategy, their tidal volume is lower than 8 ml/kg. If the tidal volume is less than 8 ml/kg, it may cause smaller variations in intrathoracic blood volume and pressure, and IVC variation will be smaller. Therefore, these two factors can influence the IVC accuracy in predicting fluid responsiveness (Yao et al., 2019).
Regarding the internal jugular vein distensibility index, our results were confirmed by Haliloğlu et al. (Haliloglu et al., 2017) who collected hemodynamic data from 44 spontaneously breathing septic patients. They found that the IJV collapsibility index was a good predictor for fluid responsiveness with 78% sensitivity and 85% specificity at the cutoff value of 36%. Patients were considered responders with cardiac index increase > 15% after passive leg raising (Haliloglu et al., 2017). Their results are different from ours because of different calculation equations.
Our results are in accordance with the work of Lizuka et al. (Iizuka et al., 2020) who found that IJV variation is a useful predictor for fluid responsiveness when they carried out the study on 27 mechanically ventilated patients with acute circulatory failure. The study found AUC 0.88 and 95% CI 0.75–0.99 with sensitivity of 84% and specificity of 93% at the cutoff value of 11.4%. Patients were considered responsive with 8% increase in stroke volume measured by arterial pulse contour after passive leg raising (Iizuka et al., 2020). Their cutoff value differs from our results because of the usage of mechanical ventilation and different calculation equations.
In the same context, Ma et al. (Ma et al., 2018) confirmed our results stating that IJV is a strong predictor for fluid responsiveness with AUC 0.88, 95% CI 0.78–0.94, sensitivity of 91.2%, and specificity of 82.8% at cutoff value > 12.99%. They collected hemodynamic data from 70 mechanically ventilated post-cardiac surgery patients. Patients were classified as responders when stroke volume increased by > 15% after passive leg raise and intravenous infusion of 500 ml of Gelofusine (Ma et al., 2018). Their cutoff value differs from ours presumably because of mechanical ventilation usage and different calculation equations.
On the other hand, Unluer and Kara (Unluer & Kara, 2013) found that the IJV collapse index was not a useful parameter for the evaluation of hypovolemia in a study performed on 80 volunteers to assess hypovolemia after blood donation. The medians of IJV collapse indices before and after blood donation were 32.74 (95% CI 32.73–39.50) and 38.88 (95% CI 35.54–42.95), respectively. They argued that carotid artery as a pulsatile structure will cause a bias for measurement of IJV diameter, especially in the real traumatized hemorrhagic patient due to tachycardic state. In addition, even a little pressure will cause a great change in the cross-sectional image and diameter of the jugular vein during scanning. In patients with shock, venous scanning becomes more difficult. They also suggested that the longitudinal measure of the internal jugular vein is more accurate and of stronger prediction. Finally, their study was performed on healthy volunteers hemodynamically stable after blood donation who did not normally need fluid resuscitation, while our study was performed on hemodynamically unstable septic patients (Unluer & Kara, 2013).
Limitation
Our observational study has many limitations. The first one is the accuracy of measuring COP (cardiac output) by VTI (velocity time integral). Using TTE (transthoracic echo) necessitates good echogenicity of the patients, so we excluded patients who did not fulfill these criteria. Additionally, using TTE requires skilled personnel, and it was documented that learning this technique is not difficult among critical care doctors (Jozwiak et al., 2014).
The second limitation was the intra-abdominal pressure measure because we did not measure it in our patients. However, we excluded all patients with any expected cause of increased intra-abdominal pressure, like ascites, pregnancy, abdominal malignancy, distension, and acute abdomen.
The third limitation is that the carotid artery as a pulsatile structure will cause a bias for the measurement of IJV diameter. Even a little pressure will cause a great change in the cross-sectional image and diameter of the jugular vein during scanning, especially with tachycardia. The final limitation is that we did not study the prediction of our indices in ventilated patients.
Conclusions
Our results showed that IJV and IVC can be used in the assessment of fluid responsiveness of spontaneously breathing septic patients with sinus rhythm in ICU and they have near predictive value. Both methods are noninvasive and can be performed at the bedside. IJV will be superior on inferior vena cava in cases of abdominal surgery, acute abdomen, or increased intra-abdominal pressure.
Availability of data and materials
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICU:
-
Intensive care unit
- IJV-DI:
-
Internal jugular vein distensibility index
- IVC-CI:
-
Inferior vena cava collapsibility index
- COP:
-
Cardiac output
- CI:
-
Cardiac index
- GE:
-
General electric
- D:
-
Diameter
- VTI:
-
Velocity time integral
- ΔCI:
-
Delta cardiac index
- IVCmax:
-
Maximum Inferior vena cava diameter
- IVCmin:
-
Minimum inferior vena cava diameter
- IJV AP:
-
Internal jugular vein anteroposterior
- IJV:
-
Internal jugular vein
- PASS:
-
Power analysis and sample size software program
- SPSS:
-
Statistical Package for Social Science
- SD:
-
Standard deviation
- ECG:
-
Electrocardiogram
- IVC:
-
Inferior vena cava
- MBP:
-
Mean blood pressure
- HR:
-
Heart rate
- SVI:
-
Systolic volume index
- p value:
-
Probability value
- AUC:
-
Area under curve
- PPV:
-
Pulse pressure variation
- IV:
-
Intravenous
- TTE:
-
Trans thoracic echo
References
Barbier C, Loubières Y, Schmit C, Hayon J, Ricôme JL, Jardin F, Vieillard-Baron A (2004) Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30(9):1740–1746. https://doi.org/10.1007/s00134-004-2259-8
Caplan M, Durand A, Bortolotti P, Colling D, Goutay J, Duburcq T, Drumez E, Rouze A, Nseir S, Howsam M, Onimus T (2020) Measurement site of inferior vena cava diameter affects the accuracy with which fluid responsiveness can be predicted in spontaneously breathing patients: a post hoc analysis of two prospective cohorts. Ann Intensive Care. 10(1):1–0. https://doi.org/10.1186/s13613-020-00786-1.
Chiaco JM, Parikh NI, Fergusson DJ (2013) The jugular venous pressure revisited. Cleveland Clinic J Med 80(10):638–644. https://doi.org/10.3949/ccjm.80a.13039
Cumpstey AF, Grocott MP, Mythen MM (2020) Fluid management and its role in enhanced recovery. In: Perioperative Fluid Management 2020. Springer, Cham, pp 339–363
Desai N, Garry D (2018) Assessing dynamic fluid-responsiveness using transthoracic echocardiography in intensive care. Bja Education. 18(7):218–226. https://doi.org/10.1016/j.bjae.2018.03.005
Feissel M, Michard F, Faller JP, Teboul JL (2004) The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 30(9):1834–1837. https://doi.org/10.1007/s00134-004-2233-5
Guarracino F, Ferro B, Forfori F, Bertini P, Magliacano L, Pinsky MR (2014) Jugular vein distensibility predicts fluid responsiveness in septic patients. Critical Care 18(6):1–8. https://doi.org/10.1186/s13054-014-0647-1
Guerin L, Monnet X, Teboul JL (2013) Monitoring volume and fluid responsiveness: from static to dynamic indicators. Best Practice Res Clin Anaesth 27(2):177–185. https://doi.org/10.1016/j.bpa.2013.06.002
Haas S, Trepte C, Hinteregger M, Fahje R, Sill B, Herich L, Reuter DA (2012) Prediction of volume responsiveness using pleth variability index in patients undergoing cardiac surgery after cardiopulmonary bypass. J Anesthesia 26(5):696–701. https://doi.org/10.1007/s00540-012-1410-x
Haliloglu M, Bilgili B, Kararmaz A, Cinel İ (2017) The value of internal jugular vein collapsibility index in sepsis. Turkish J Trauma Emerg Surg 23(4):294–300. https://doi.org/10.5505/tjtes.2016.04832
Seymour CW, Liu VX, Iwashyna TJ, et al. (2016) Assessment of clinical criteria for sepsis: fo the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):762–774
Iizuka Y, Nomura T, Sanui M, Mochida Y, Aomatsu A, Lefor AK (2020) Collapsibility of the right internal jugular vein predicts responsiveness to fluid administration in patients receiving pressure support ventilation: a prospective cohort study. J Clinic Med Res 12(3):150–156. https://doi.org/10.14740/jocmr4064
Jozwiak M, Monnet X, Cinotti R, Bontemps F, Reignier J, Belliard G (2014) Prospective assessment of a score for assessing basic critical-care transthoracic echocardiography skills in ventilated critically ill patients. Ann Intensive Care. 4(1):1–8. https://doi.org/10.1186/2110-5820-4-12
Ma GG, Hao GW, Yang XM, Zhu DM, Liu L, Liu H, Tu GW, Luo Z (2018) Internal jugular vein variability predicts fluid responsiveness in cardiac surgical patients with mechanical ventilation. Ann Intensive Care 8(1):1–9. https://doi.org/10.1186/s13613-017-0347-5
Matta JL, Kraemer CE, Tuinman PR, van Westerloo DJ (2019) POCUS series: the use of velocity time integral in assessing cardiac output and fluid responsiveness. Netherlands J Critical Care 27(5):196–198
Miller A, Mandeville J (2016) Predicting and measuring fluid responsiveness with echocardiography. Echo Res Practice 3(2):G1–G2. https://doi.org/10.1530/ERP-16-0008
Orso D, Guglielmo N, Federici N, Cugini F, Ban A, Mearelli F, Copetti R (2016) Accuracy of the caval index and the expiratory diameter of the inferior vena cava for the diagnosis of dehydration in elderly. J Ultrasound. 19(3):203–209. https://doi.org/10.1007/s40477-016-0200-y
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, Teboul JL (2007) Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Critical Care Med 35(1):64–68. https://doi.org/10.1097/01.CCM.0000249851.94101.4F
Pereira RM, da Silva AJ, Faller J, Gomes BC, Silva JM Jr (2020) Comparative analysis of the collapsibility index and distensibility index of the inferior vena cava through echocardiography with pulse pressure variation that predicts fluid responsiveness in surgical patients: an observational controlled trial. J Cardiothorac Vasc Anesth 34(8):2162–2168. https://doi.org/10.1053/j.jvca.2020.02.007
Pınar SG, Pekdemir M, Özturan İU, Doğan NÖ, Yaka E, Yılmaz S, Karadaş A, Emir DF (2020) Assessment of end-tidal carbon dioxide and vena cava collapsibility in volume responsiveness in spontaneously breathing patients. Medizinische Klinik-Intensivmedizin und Notfallmedizin. 25:1–7
Preisman S, Kogan S, Berkenstadt H, Perel A (2005) Predicting fluid responsiveness in patients undergoing cardiac surgery: functional haemodynamic parameters including the Respiratory Systolic Variation Test and static preload indicators. Br J Anaesth 95(6):746–755. https://doi.org/10.1093/bja/aei262
Sakr Y, Rubatto Birri PN, Kotfis K, Nanchal R, Shah B, Kluge S, Schroeder ME, Marshall JC, Vincent JL (2017) Higher fluid balance increases the risk of death from sepsis: results from a large international audit. Critical Care Med 45(3):386–394. https://doi.org/10.1097/CCM.0000000000002189
Sánchez JI, Ruiz JD, Fernández JJ, Zuñiga WF, Ospina-Tascón GA, Martínez LE (2021) Predictors of fluid responsiveness in critically ill patients mechanically ventilated at low tidal volumes: systematic review and meta-analysis. Ann Intensive Care 11(1):1–7. https://doi.org/10.1186/s13613-021-00817-5
Theerawit P, Morasert T, Sutherasan Y (2016) Inferior vena cava diameter variation compared with pulse pressure variation as predictors of fluid responsiveness in patients with sepsis. J Crit Care 36:246–251. https://doi.org/10.1016/j.jcrc.2016.07.023
Unluer EE, Kara PH (2013) Ultrasonography of jugular vein as a marker of hypovolemia in healthy volunteers. Am J Emerg Med 31(1):173–177. https://doi.org/10.1016/j.ajem.2012.07.003
Wiedemann HP, Wheeler AP, Bernard GR (2006) Comparison of two fluid-management strategies in acute lung injury. J Vascular Surgery. 44(4):909. https://doi.org/10.1016/j.jvs.2006.08.053
Wise R, Faurie M, Malbrain ML, Hodgson E (2017) Strategies for intravenous fluid resuscitation in trauma patients. World J Surgery 41(5):1170–1183. https://doi.org/10.1007/s00268-016-3865-7
Yao B, Liu JY, Sun YB, Zhao YX (2019) The value of the inferior vena cava area distensibility index and its diameter ratio for predicting fluid responsiveness in mechanically ventilated patients. Shock 52(1):37–42. https://doi.org/10.1097/SHK.0000000000001238
Zhao J, Wang G (2016) Inferior vena cava collapsibility index is a valuable and non-invasive index for elevated general heart end-diastolic volume index estimation in septic shock patients. Med Sci Monit 22:3843–3848. https://doi.org/10.12659/MSM.897406
Acknowledgements
Not applicable.
Funding
No funding. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study supervision was done by BM, WA, RH, and AN. Drafting the article was done by AM. Conception and design were done by AM, BM, WA, RH, and AN. Statistical analysis was done by AM, BM, WA, RH, and AN. Acquisition of data was done by AM. Analysis and interpretation of data was done by AM, BM, WA, RH, and AN. Critical revision of the article was done by BM, WA, RH, and AN. Review of submitted version of manuscript was done by AM, BM, WA, RH, and AN. Administrative/technical/material support was done by AM, BM, WA, RH, and AN. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study (FMASU MD 262/2019) was provided by the Ethics committee of Ain Shams University hospital, Abbasia, Cairo, Egypt (Chairperson Prof F. Tash) on 1/9/2019. Informed written consents to participate in the study were provided by all participants or their legal guardians.
Consent for publication
Not applicable
Competing interests
There were no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsaeed, A.M.R., Nor El-Din, B.M.E., El Taher, W.A.M. et al. Internal jugular vein distensibility variation and inferior vena cava collapsibility variation with fluid resuscitation as an indicator for fluid management in spontaneously breathing septic patients. Ain-Shams J Anesthesiol 14, 26 (2022). https://doi.org/10.1186/s42077-022-00226-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-022-00226-1