Abstract
Background
Vestibular schwannomas (VS) are slowly growing tumor, deriving from the vestibular component of cranial nerve VIII. Primary treatment modalities include microsurgery, radiosurgery, a combination of microsurgery and radiosurgery, and conservative treatment. The management of VS is a matter of debate, particularly in case of small tumors (less than 2 cm in diameter size).
Methods
We performed an institutional retrospective review of a consecutive series of 28 surgically treated patients suffering from VS, operated in our institution. Patients were assigned on the ground of the preoperative imaging in two groups: tumors with major diameter of extra-meatal portion measuring ≥ 3 cm (Group I, 16 patients) and tumors with major diameter < to 3 cm (Group II, 12 patients).
Results
The total amount of 18/28 patients were females; the average age was 60.1 years. The average duration of the preoperative symptoms was 25.2 months, while the average interval between the diagnosis and surgical treatment was 8.68 months. The average preoperative volume was, respectively, for Group I and II tumors of 14.35 cm3 and 3.73 cm3. Age was associated to the duration of the preoperative symptoms (r = − 364; p = 0.044), with the probability to develop a complication (p = 0.031) and preoperative low HB score (r = − 324; p = 0.040). The presence of hypoacusis as preoperative symptom was strongly associated to a lesser postoperative maximum diameter and smaller residual disease (p = 0.014). Group I had a significantly longer hospitalization period in respect to Group II (p = 0.001) that impacted negatively to postoperative performance status (r = 0.368, p = 0.042).
Conclusions
We confirmed the strong association between age and size of the lesion and the clinical results, where larger lesions in older patients are more prone to complications than smaller in young patients. We found that the patients presenting hypoacusis at onset were associate to lesser preoperative FN impairment outlining a possible differential involvement of the CN related to the internal meatus. We also introduce the strong association of Koos grade with postoperative performance status, hospitalization and facial nerve functionality.
Similar content being viewed by others
Introduction
Background
Vestibular schwannomas (VS) are slowly growing, indolent tumors, deriving from the vestibular component of cranial nerve VIII [1]. Primary treatment modalities include microsurgery, radiosurgery and a combination of the two [2,3,4].
By larger VSs, the patient’s quality of life (QoL) can be seriously compromised because of major neurological impairments. Surgery remains the milestone in the management of these tumors, especially where the maximum diameter is over 20 mm, the lesion seriously compresses and possibly dislocates the brainstem (BS) or is cause of severe vestibular symptoms [1, 5,6,7]. Nowadays, in the western countries, thanks to the increased diagnostic means, early detection of VS from systematic request for an magnetic resonance imaging (MRI) by hearing loss and/or tinnitus, the number of tumors detected per year has dramatically increased [3, 8,9,10], and, simultaneously with the mean tumor size steadily decreasing, the optimal management of VS remains a matter of debate, in case of asymptomatic small tumors smaller than 2 cm in diameter size [10], but also in case of oligosymptomatic medium tumors (Grade of Koos 2—from 2 to 3 cm in diameter) [11]. The larger and symptomatic tumors are generally considered for microsurgical excision except in patients suffering from significant comorbidities possibly complicating open surgery [2,3,4, 8,9,10,11]. Because of the debated emergent evidence of efficacy of the radiosurgical treatments, even for larger lesions [4, 9, 10, 12], the optimal management of the medium- and small-sized tumors remains either still unclear and still controversial, especially considering the reported, and probably not completely understood, long-term side effects of the radiation treatment [2, 10]
Purpose of the investigation
In this study, we reviewed a retrospective series of patients suffering from VS, divided in two subgroups according to preoperative diameter of lesion, whose facial nerve (FN) function was evaluated pre- and postoperatively, along with an analysis of the complication rate and functional status changes, in the context of a retrospective single-center single-operator consecutive series of patients.
Patients and methods
Participants and Eligibility
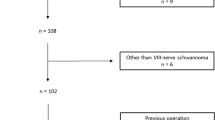
We performed an Institutional retrospective review of a consecutive series of surgically treated patients suffering from VS (Fig. 1), operated on in the Department of Neurosurgery of Policlinico Umberto I of Rome (Università “La Sapienza”) by the Chairman of the Institution and senior author (AS). We collected a total of 28 patients. Histological diagnoses were performed according to the updated version of the WHO guidelines [13]. The patients who were enrolled in the final cohort in the period ranging between January 2013 and December 2017 met the following inclusion criteria:
-
1.
Younger than 75 years old patients,
-
2.
Whose clinical, surgical and radiological records concerning their VS were complete and available for consultation
-
3.
Suffering from no further intracranial or spinal neoplastic, infectious, vascular or inflammatory condition, in order to avoid jeopardization of the functional and neurological results
-
4.
Who did not undergo a previous stereotactic radiosurgery (SRS) or other radiation treatments
All the patients who met the aforementioned inclusion criteria were assigned on the ground of the preoperative imaging to the following subgroups:
Tumors classified as Group I: the major diameter of extra-meatal portion measure ≥ 3 cm, grade III of Koos grading (KG) classifications (mentioned in Table 1 as KG3, 16 patients).
Tumors classified as Group II: the major diameter of extra-meatal portion measure < to 3 cm, grade II of Koos classifications (mentioned in Table 1 as 2, 12 patients).
Patients were preoperatively offered of all the treatment options, including conservative management and SRS, and the surgical indication was confirmed, for each patient, according to the following factors:
-
1.
Age
-
2.
Personal preference of the patient,
-
3.
A preoperative feasible plan for a satisfactory decompression of the compressed nervous structures
-
4.
Neurological symptoms related to the mass, including BS and cranial nerves (CNs) compression,
-
5.
Lesion related dilation of the supratentorial ventricle system
-
6.
For oligo-asymptomatic patients, evidence of significant growth while the patient was included in the follow-up program of our institution.
-
7.
For patients with preserved functional hearing, a durable hearing preservation was the target and therefore played a role in deciding for surgical resection either [11].
For all the included patients, we recorded age, sex, clinical onset (specifically with the first and second presenting symptom—in order of appearance—and the presence/absence of a cochlear, vestibular or facial nerve at the clinical onset), hospitalization length, interval between diagnosis and surgery and preoperative duration of the symptoms.
The FN function was clinically evaluated pre- and postoperatively by means of the standard version of the House–Brackmann scale, extensively validated in the relevant literature [9, 14,15,16]. Vestibular and cochlear dysfunctions were preoperative evaluated, by means of a dichotomous variable (0/1−No/Yes) whenever a clinical history or a diagnostically proven presence of vertigo and/or tinnitus/hypoacusis/anacusis was preoperatively reported.
The extent of the lesion was recorded as follows:
-
1.
Preoperative and postoperative volume of the contrast-enhancing lesion was calculated drawing a region of interest (ROI) in a volumetric enhancing postcontrast study weighted in T1 (a multi-voxel study), conforming to the margins of the contrast-enhancing lesion with software Horos [17].
-
2.
Maximum preoperative and postoperative diameter of the lesion, as measured in slice in which the diameter appeared to the wider in the gadolinium-enhanced T1-weighted pre- and postoperative MRI study.
A focus was on the KPS results as an index of the functional status of the patients: Such parameter was considered, as previously observed demonstrative of QoL [10, 18]. In particular it was recorded in two different moments: 1. before surgery, 2. at 30 day after surgery.
Radiological and surgical protocols
All the patients included underwent a preoperative brain MRI scan, following our institutional protocol, included an high field 3 Tesla volumetric study with the following sequences: T2w, FLAIR, isotropic volumetric T1-weighted magnetization-prepared rapid acquisition gradient echo (MPRAGE) before and after intravenous administration of paramagnetic contrast agent; a constructive interference steady state (CISS) completed the protocol for what concerns the cerebellum pontine angle (CPA).
All the procedures were performed with an infrared-based neuronavigator (Brainlab, Kick® Purely Navigation), in a standard neurosurgical theater, with a standard operative microscope (Leica, model OH4). A standard total intravenous anesthesia protocol has been used. Because of the routinely employed intraoperative neuromonitoring realized with use of stimulating probes in order to “map” the course of the VII CN, no muscle relaxants were administered.
Surgery was in all cases performed through the retrosigmoid approach (RSA) by the senior author (A.S.). The target was a satisfactory resection (GTR/NTR), with decompression of the impaired nervous structures and preservation of both the facial and the cochlear nerve functions, regardless of preoperative hearing status or preoperative facial nerve impairment. All patients were operated in the lateral park-bench position. The FN was monitored by intermittent electrical stimulation of the intracranial FN with the NIM nerve monitoring system (Medtronic Inc., Minneapolis, MN, USA) as well as free facial electromyography (EMG). We also used somatosensory evoked potential monitoring for all patients. Lower cranial nerves were also routinely monitored. Details of the RSA for VS removal have been extensively discussed in the neurosurgical literature. In general, it was intraoperatively judged mandatory to stop tumor excision when the IoN outlined an unquestionable risk for permanent postoperative facial nerve morbidity.
Evaluation of the extent of resection
The extent of resection (EOR) was determined through a comparison between the MR images obtained before surgery and the MRI performed 30 days after surgery. EOR was calculated as a percentage by comparing the preoperative and early postoperative imaging, with the aforementioned software. GTR was defined as a confirmed reduction of the preoperative volume of the tumor of at least 95%; conversely, a near-total resection or subtotal resection was a surgical result of, respectively, a 90–95% and less than 90% resection rate (NTR and STR, respectively).
Follow-up program
A close range dedicated clinical and neuroimaging follow-up program was routinely performed in our institution. This program included:
-
1.
A standard early (maximum 24 h after surgery) postoperative brain CT scan to rule out major and eventually clinically silent complications [19].
-
2.
At approximately one month after surgery (25–35 days), a volumetric brain MRI scan was repeated for a first step follow-up control. When a slowly growing grade I lesion was histologically confirmed, in case of NTR/STR brain MRI scan repeated at three months, whereas in case of GTR it was postoperatively repeated directly at six months after surgery.
For every radiological reevaluation, we performed a complete outpatient clinical and neurological reevaluation. Generally, during this reevaluation, the functional status (as expressed with KPS scores), the neurological conditions in regard to the facial, cochlear and vestibular nerve were accurately recorded. The overall condition of each patient, according to his/her perception of the life, was also recorded, and coded in three-step ordinal variable as 0. worsened, 1. stable and 2. improved. A special focus was also paid on the surgery-related complications experienced by the patients. In particular we recorded the incidence of postoperative hydrocephalus, hematomas, CSF leaks, infections and meningitis.
Statistical methods
The sample was analyzed with SPSS version 18. Comparison between nominal variables have been made with Chi2 test. Continuous variables’ means were compared with one-way, repeated measures, multivariate ANOVA analysis along with contrast analysis and post hoc tests and investigated with Pearson’s bivariate correlation. Threshold of statistical significance was considered p < 0.05.
Potential source of bias and study size
A potential source of bias is expected from exiguity of the sample, which, in regard to the endpoints selected, presents an fair post hoc statistical estimated power (1 − β = 0.76 for age groups and complications incidence, 1 − β = 0.71 and 1 − β = 0.75, respectively, for EOR and status for α 0.05 and effect size 0.8), thus providing reliable conclusions for strong statistical effects.
The study is a historical cohort study (retrospective purely observational, non-sponsored): Outcome and exposure of the patients occurred and consolidated before the start of the study and there is no ethical problem requiring approval of the ethical committee. Before surgical procedure, all the patients gave informed written explicit consent after appropriate information. Data reported in the study have been completely anonymized. No treatment randomization has been performed. This study is consistent with Helsinki declaration of human rights of research.
Results
In a first step, we retrospectively reviewed the clinical, radiological and surgical records of 28 patients operated on by a RSA for the resection of VSs in the period ranging between 2013 and 2017. The total amount of 18/28 patients were females; the average age was 60.1 years ± 13.99. The average duration of the preoperative symptoms was 25.2 months ± 23.4, while the average interval between the diagnosis and surgical treatment was 8.68 months ± 7.97. Preoperatively all the patients included had, respectively, a HB score < 2 and a KPS > 80% in 100% of cases. The average preoperative volume was, respectively, for Group I and II tumors of 14.35 cm3 ± 7.97 and 3.73 cm3 ± 1.46 (Table 1).
The most common presenting symptoms were hearing involvement or loss with a total of 19/28 patients suffering from tinnitus, hypoacusis or cophosis, followed by a total of 11 patients presenting with vertigo (respectively, 67.8% and 39.2%). A total of 13/16 and 11/12 patients belonging to Group I and Group II, respectively, were stable or improved after surgery in regard to KPS (81.25% vs. 91.66%), while a total of 10/16 and 4/12 patients belonging to Group I and Group II, respectively, had a postoperative HB score > 3 after surgery (62.50% vs. 33.33%). The achieved EOR was overcrossing 95% in 78.57% of cases (22/28 patients).
A total of 10/16 and 3/12 patients belonging to Group I and Group II experienced a postoperative complication (62.5% vs. 25.0% p = 0.055—Fig. 2). Three out of the 10 complications of Group I and 1 of the 12 of Group II proved to be stable complications (18.75% vs. 8.33%). In details, fifteen patients postoperative course was uncomplicated, the remaining experienced in 10 cases a transient hydrocephalus, which was in three cases treated with a EVD until resolution of the postoperative edema; in two cases a CSF cutaneous leak which caused a wound problem; in one case the course was extremely benign with a significant tendency to spontaneous resolution; in the remaining case it was necessary to admit the patient in the division to position a 4-day long active lumbar drainage, until complete resolution of the complication. We recorded one case of postoperative FCP postoperative hematoma, a patient who after a period of ICU hospitalization died of pneumonia. The overall mortality rate is 3.57%. No deficit of the lower CN was recorded.
Age
Age was statistically associated to the duration of the preoperative symptoms (r = − 364; p = 0.044), with the probability to develop a complication (p = 0.031) and also with the preoperative HB score (r = − 324; p = 0.040); the elderly, with a longer preoperative duration of symptoms, are a fragile subgroups of patients.
Hypoacusis
The presence of hypoacusis as preoperative symptom was strongly associated to a lesser postoperative maximum diameter and therefore with a smaller residual disease (p = 0.014—Fig. 3). Moreover, patients presenting hypoacusis at onset were associate to lesser preoperative FN impairment (p = 0.018—Fig. 4), thus outlining a possible differential involvement of the CN related to the internal meatus.
Classification of Koos: House–Brackmann, KPS and postoperative complications
HB and KPS showed a strong reciprocal statistical association, both in regard to the pre- and postoperative period outlining that the better preoperative function predicts the better postoperative outcome. Most importantly, the both outcome variables are strongly associated to the personal perception of the QoL of the patient, 30 days after surgery (r = 0.725 p = 0.001), thus highlighting the extreme psychological impact of the FN on the QoL as it is experienced by the patients.
Koos grade 2 or 3 lesion disclosed no significant preoperative KPS and HB scores difference, whereas in the postoperative period, a strong trend toward worse HB outcomes was retrieved in patients suffering from Koos grade 3 lesions (p = 0.069—Fig. 5). Moreover, KG 3 lesion had a significantly longer hospitalization period in respect to the KG 2 counterparts (p = 0.001—Fig. 6) and the longer hospitalization was negatively related, as expected, to postoperative KPS (r = 0.368, p = 0.042).
As already introduced, KG 3 lesions disclosed a trend toward a statistical association with complications in respect to KG 2 lesions (p = 0.055) and thus with outcomes, with a rate of KPS score > 80% of 81.25% versus 91.66% of patients. The incidence of postoperative complications, as a dichotomous variable (1/0 Yes/No), demonstrated a strong association with the postoperative KPS (p = 0.010), the length of hospitalization (p = 0.011, Fig. 7) and interestingly with the preoperative volume of the lesion (p = 0.030, Fig. 8).
Discussion
VS is the most common cerebellopontine angle (CPA) tumor, representing up to 75% of skull base tumors [1]. Several different management approaches were previously advocated, including radiotherapy, observation and periodic control of the tumor, and of course surgery. The “wait and see” option may be suitable under certain circumstances, such as patients in advanced age groups, in poor general health conditions, with small tumors, few or no symptoms or with relatively well preserved hearing [7] but also when the tumor causes no other symptoms, than an auditory function impairment. Because of the increased precocity of the diagnosis, and because, at the diagnosis, patients are extensively informed about the slow growth of the tumor and they suffer, at the beginning, from minimal disturbances, it is increasingly frequent to find patients who prefer to undergo an observation program until the tumor manifests with more significant neurological disturbances (related to the greater tumor sizes), although a greater size of the tumor itself works as a predictor and risk factor for major complications and postoperative facial nerve impairment [1,2,3,4,5].
About the natural history of the conservatively managed VS an overall slow growth rate ranging from 0.66 to 0.78 mm/year has already been reported [5]. Deen et al. [5] analyzed a cohort of patients suffering from conservatively managed VS, and found that none of these patients had spontaneous shrinkage of tumor, rather most continued growing, eventually requiring surgical management. Nakatomi et al. [6] reported that patients with STR would have tumor recurrence at an average of 2.7 years postoperatively.
Although complete removal of the tumor is still to be considered the gold standard, many studies with complete surgical resection of large VS have reported high rates of facial nerve dysfunction (31–57%). For this reason, there is a trend toward STR of the tumor with planned postoperative SRS [4, 8] which, unfortunately, SRS bares its own inherent risks, including tumor swelling and facial neuropathy [3, 9]. Postoperative management of patients with STR depends on the amount of residual tumor and the rate of tumor growth. The goal of our surgery was GTR with preservation of both the facial and the cochlear nerves, regardless of preoperative hearing status.
A surgically induced FN injury is the most common complication of VS surgery. Facial nerve function is considered satisfactory as long as the House–Brackmann grade is 3 or less. The review of 89 articles on facial nerve function reported 78% of preservation with the RSA in tumor size of < 20 mm and 67% in larger tumors [18]. Postoperative facial function is one of the main priorities of VS surgery.
Consistently, the intraoperative facial neuromonitoring has become unavoidable; it enables the nerve integrity to be preserved in the majority of patients [20, 21]. In any case, the preservation of acceptable FN function after surgery is the key concern for most patients with VS.
With the adoption of a functional sparing surgery policy, the functional results on the FN improved considerably, at the price of less radical resections, with a subsequent increased risk of tumor regrowth. Some investigators advocate planned partial resections to minimize the risk for the cranial nerves, leaving significant postoperative tumor residues [9, 16]. Others assert that good postoperative FN outcomes do not depend on the extent of resection if the resection is carried out with a priority given to FN preservation [9, 16, 22]. A negative association between the postoperative clinical results and the size of the tumors has been advocated by several investigators, although in relatively wide surgical series and never unquestionably demonstrated [12, 14, 23]. In general, tumors under 20 mm of diameter, with an outcome of V and VI HB grade, were observed in a low percentage of patients, while the incidence of such results increased notably when the tumor was above this size.
In VS surgery, the adhesion between tumor and facial nerve determines a greater intraoperative manipulation [20]. Dissection of the facial nerve tumor capsule may produce a contusive effect on the nerve fiber thus disrupting the local microcirculation, leading to a transient ischemia leading to a degeneration of the nerve fibers. Such a cascade of events could explain the worsening of the postoperative FN function. For this reason, several authors outlined that the two main anatomical factors determining the possibility to spare the FN are the tumor adhesion or encasement of the FN itself, and the larger size of the tumor [23, 24]. This finding proved to be independent from surgical approach employed, disclosing that for lesions under 30 mm of diameter, the incidence of poor FN outcomes was low, regardless of the surgical approach used.
Our experience confirms the aforementioned findings. In our series, smaller lesions were associated to better clinical outcomes, lesser incidence of complications and shorter hospitalization periods. Therefore, we advocate a timely surgical treatment, either for large lesions determining a significant neurological impairment at diagnosis, and for relatively small VS (KG 2) lesions, in oligo-asymptomatic patients, whose tumors demonstrated an ascertained growth tendency in a radiological follow-up program. The increasing evidence of a negative association between the size of the lesion and the clinical results should always be, in our opinion, an essential part of the preoperative patient information.
Conclusions
Preservation of FN function during resection of vestibular schwannomas (VS) remains one of the key targets to preserve the QoL of the patients. In this study, we confirmed the strong association between age and size of the lesion and the clinical results, where larger lesions in older patients are more prone to complications than smaller in young patients. We found that the patients presenting hypoacusis at onset were associate to lesser preoperative FN impairment outlining a possible differential involvement of the CN related to the internal meatus. We also introduce the strong association of KG with postoperative performance status, hospitalization and facial nerve functionality. In order to improve the clinical results, possibly reducing the complication rate, a surgical indication should be also considered for smaller KG 2 lesions of approximately 20 mm.
Availability of data and materials
At request to the corresponding author, we understand that the corresponding author is the sole contact for the editorial process (including Editorial Manager and direct communications with the office). He is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
Abbreviations
- VS:
-
Vestibular schwannomas
- QoL:
-
Quality of life
- BS:
-
Brainstem
- MRI:
-
Magnetic resonance imaging
- FN:
-
Facial nerve
- AS:
-
Senior author
- SRS:
-
Stereotactic radiosurgery
- ROI:
-
Region of interest
- CPA:
-
Cerebellum pontine angle
- CN:
-
Cranial nerve
- GTR:
-
Gross total resection
- EMG:
-
Electromyography
- EOR:
-
Extent of resection
References
Oh BC, Hoh DJ, Giannota SL. Tumors of the cerebellopontine angle. In: Hanna EY, Demonre F, editors. Comprehensive management of skull base tumors. 1st ed. New York: INFRMA-HC; 2008. p. 339–401.
Akinduro OO, Lundy LB, Quinones-Hinojosa A, Lu VM, Trifiletti DM, Gupta V, Wharen RE. Outcomes of large vestibular schwannomas following subtotal resection: early post-operative volume regression and facial nerve function. J Neurooncol. 2019;143(2):281–8.
Zhang X, Fei Z, Chen YJ, Fu LA, Zhang JN, Liu WP, et al. Facial nerve function after excision of large acoustic neuromas via the suboccipital retrosigmoid approach. J Clin Neurosci. 2005;12:405–8.
Fuentes S, Arkha Y, Pech-Gourg G, Grisoli F, Dufour H, Regis J. Management of large vestibular schwannomas by combined surgical resection and gamma knife radiosurgery. Prog Neurol Surg. 2008;21:79–82.
Deen HG, Ebersold MJ, Harner SG, Beatty CW, Marion MS, Wharen RE, et al. Conservative management of acoustic neuroma: an outcome study. Neurosurgery. 1996;39:260–4.
Nakatomi H, Jacob JT, Carlson ML, Tanaka S, Tanaka M, Saito N, et al. Long-term risk of recurrence and regrowth after gross-total and subtotal resection of sporadic vestibular schwan- noma. J Neurosurg. 2017;1:1–7.
González-Orús Álvarez-Morujo R, Álvarez Palacios I, Martin Oviedo C, Scola Yurrita B, Arístegui Ruiz MA. Conservative management of vestibular schwannoma. Acta Otorrinolaringol Esp. 2014;65:275–82.
Zumofen DW, Guffi T, Epple C, Westermann B, Krahenbuhl AK, Zabka S, et al. Intended near-total removal of Koos grade IV vestibular schwannomas: reconsidering the treatment paradigm. Neurosurgery. 2018;82:202–10.
Van de Langenberg R, Hanssens PE, van Overbeeke JJ, Verheul JB, Nelemans PJ, de Bondt BJ, et al. Management of large vestibular schwannoma. Part I. Planned subtotal resection followed by Gamma Knife surgery: radiological and clinical aspects. J Neurosurg. 2011;115:875–84.
Daniel RT, Tuleasca C, George M, et al. Preserving normal facial nerve function and improving hearing outcome in large vestibular schwannomas with a combined approach: planned subtotal resection followed by gamma knife radiosurgery. Acta Neurochir. 2017;159:1197–211.
Erickson NJ, Schmalz PGR, Agee BS, Fort M, Walters BC, McGrew BM, Fisher WS. Koos classification of vestibular schwannomas: a reliability study. Neurosurgery. 2019;85(3):409–14.
Darrouzet V, Martel J, Enee V, Bebear JP, Guerin J. Vestibular schwannoma surgery outcomes, our multidisciplinary experience in 400 cases over 17 years. Laryngoscope. 2014;114:681–8.
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM, Reifenberger G, Soffietti R, von Deimling A, Ellison DW. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021;23(8):1231–51. https://doi.org/10.1093/neuonc/noab106.
House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93(2):146–7. https://doi.org/10.1177/019459988509300202.
Samii M, Gerganov V, Samii A. Improved preservation of hearing and facial nerve function in vestibular schwannoma surgery via the retrosigmoid approach in a series of 200 patients. J Neurosurg. 2006;105(4):527–35.
Troude L, Boucekine M, Montava M, Lavieille JP, Régis JM, Roche PH. Predictive factors of early postoperative and long-term facial nerve function after large vestibular schwannoma surgery. World Neurosurg. 2019;127:e599–608.
Paglia F, Caporlingua A, Armocida D, Rizzo F, Santoro A, D’angelo L. Preoperative 3D volume reconstruction of the posterior wall of the sphenoid sinus with horos: a free, simple and reliable tool in endoscopic endonasal trans-sphenoidal surgery. Neurocirugia (Astur Engl Ed). 2022;33(5):219–26. https://doi.org/10.1016/j.neucie.2021.04.008.
Sughrue ME, Yang I, Rutkowski MJ, Aranda D, Parsa AT. Preservation of facial nerve function after resection of vestibular schwannoma. Br J Neurosurg. 2010;24:666–71.
Armocida D, Pesce A, Frati A, Miscusi M, Paglia F, Raco A. Pneumoventricle of unknown origin: a personal experience and literature review of a clinical enigma. World Neurosurg. 2019;122:661–4. https://doi.org/10.1016/j.wneu.2018.11.050.
Arístegui Ruiz MÁ, González-Orús Álvarez-Morujo RJ, Oviedo CM, Ruiz-Juretschke F, García Leal R, Yurrita BS. Surgical treatment of vestibular schwannoma. Review of 420 cases. Acta Otorrinolaringol (Engl Ed). 2016;67(4):201–11.
Matthies C, Samii M. Management of vestibular schwannomas (acoustic neuromas): the value of neurophysiology for evaluation and prediction of auditory function in 420 cases. Neurosurgery. 1997;40(5):919–29.
Regis J, Pellet W, Delsanti C, et al. Functional outcome after Gamma Knife surgery or micro- surgery for vestibular schwannomas. J Neurosurg. 2013;119(suppl):1091–100.
Falcioni M, Fois P, Taibah A, Sanna M. Facial nerve function after vestibular schwannoma surgery. J Neurosurg. 2011;115:820–6.
Ben Ammar M, Piccirillo E, Topsakal V, Taibah A, Sanna M. Surgical results and technical refinements in translabyrinthine excision of vestibular schwannomas: the Gruppo Otologico experience. Neurosurgery. 2012;70(6):1481–91. https://doi.org/10.1227/NEU.0b013e31824c010f.
Acknowledgements
In regard to the topics of the present paper, the authors have nothing to disclose. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us. We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property. We further confirm that any aspect of the work covered in this manuscript that has involved either experimental animals or human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Funding
This study was no funded by any association.
Author information
Authors and Affiliations
Contributions
DA was involved in draft manuscript and correspondence, AP contributed to formal analysis and methodology, SC and FM took part in data collection and tables, AF e AS contributed to conceptualization, supervising and main surgical operators.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. This article does not contain any studies with animals performed by any of the authors.
Consent for publication
The patient has consented to the submission of this review article and study to the journal.
Competing interests
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome. We wish to draw the attention of the Editor to the following facts which may be considered as potential conflicts of interest and to significant financial contributions to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Armocida, D., Pesce, A., Ciarlo, S. et al. Predictive factors of facial nerve function after medium/large vestibular schwannoma surgery: relationships between time of surgery, dimensions and size of resection. Egypt J Neurosurg 39, 54 (2024). https://doi.org/10.1186/s41984-024-00319-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-024-00319-z