Abstract
Background
Primary pilocytic astrocytoma of the CPA (Cerebello-pontine angle), in the pediatric age group is an extremely rare entity, with just three cases reported so far. It mostly arises from the root entry zone of the cranial nerves found in this cistern.
Case presentation
A 11-year boy presented with headache, hearing impairment in right ear. Pure tone audiogram and BAER (Brainstem auditory evoked response) suggested retro-cochlear sensori-neural hearing loss. MRI revealed a heterogeneously enhancing extra-axial lesion in the right CPA. Tumor was approached through right retromastoid suboccipital craniotomy. Intraoperatively it seemed to arise from the REZ (root entry zone) of CN VIII and histopathology confirmed it to be pilocytic astrocytoma. We have reported this as only the fourth case and reviewed the already existing literature. In the previous case reports an extensive immunohistochemical analysis was not done and the final diagnosis was not as per the Harlem consensus guidelines.
Conclusion
In this case, we have tried to report the final histopathology in accordance with the 5th edition of WHO classification of CNS tumors. In the current era of molecular diagnosis and layered structural format of reporting a histopathology, this case is the first of its kind and emphasizes the need to consider PA as one of the differentials for lesions in CPA.
Similar content being viewed by others
Background
Pilocytic astrocytoma constitutes 5–10% of primary pediatric tumors and is the most common intrinsic brain tumor in this age group. It is seen mostly in the cerebellum, brainstem, optic pathway, hypothalamus, and rarely in the cerebellopontine angle [1]. Primary pilocytic astrocytoma of CPA (cerebellopontine angle) has been found to arise from the REZ (root entry zone) of the cranial nerves found in this cistern [2, 3]. Such cases in the pediatric population are extremely rare [4,5,6]. With due consent of patient’s guardian we report this case as only the fourth pilocytic astrocytoma of CPA in the pediatric age group and the first of its kind in the era of molecular diagnosis.
Case report
A 11-year boy presented with decreased hearing in the right ear, occasional headache, and vomiting for 4 months. Neurological examination revealed SNHL (sensorineural hearing loss) in the right ear and bilateral papilledema. Although pure tone audiogram confirmed the presence of SNHL in the right ear, he had a serviceable hearing. And, BAER revealed a delay in wave V, thus suggesting a retro-cochlear pathology.
Neuroimaging
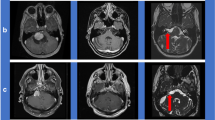
Preoperative MRI, revealed a well-circumscribed extra-axial lesion of in the right CPA, compressing the fourth ventricle, pons, medulla, right cerebellar hemisphere, vermis, and had upstream hydrocephalus (Fig. 1). The lesion showed heterogeneous contrast uptake, with a small focal extension into the right IAC and the right jugular foramen.
Axial (a) and sagittal (b) views of contrast MRI showing a heterogeneously enhancing mass lesion [size 5.0 (TR) × 4.3 (AP) × 5.0 (CC) cm] in the right cerebellopontine angle. Axial T2 image (c) showing an extraaxial lesion in the right cerebellopontine angle, with focal extension into the internal auditory canal
Intraoperative findings
A left ventriculoperitoneal shunt was placed at first, followed by right RMSOC to expose the tumor. EMG was used to map out the course of CN VII. Tumor was encapsulated, grayish white, soft, and was moderately vascular. The central portion of tumor was debulked with the CUSA and as the capsule buckled in, the preserved arachnoidal planes aided in separating it from the cerebellum, brain stem, peduncles, and cranial nerves (V, IX, X). Carefully facial nerve could be dissected away from the tumor mass. However, the tumor was seen to be arising from the CN VIII, almost 1–2 cm away from the surface of the brainstem. The tumor could be excised completely except for a small segment that was adherent to the CN VIII (Fig. 2). The postoperative hospital stay was uneventful and at 18 months of follow-up he is asymptomatic and his hearing was still preserved.
Histopathology
Microscopic examination revealed cells that were ovoid to spindle-shaped, piloid in appearance, arranged in sheets, with no significant nuclear mitosis, atypia, necrosis, and microvascular proliferation. The background showed the presence of eosinophilic granular bodies and Rosenthal fibers. In view of morphology and IHC (Fig. 3) the final diagnosis of pilocytic astrocytoma (WHO grade 1) was made.
a Histopathology slide (using Hematoxylin and eosin stain) shows cells that are spread in sheets, are ovoid to spindled and with no significant nuclear atypia. Many Rosenthal fibers are noted in the background (black arrows). Immunohistochemical analysis showed positivity for GFAP (b), suggesting a glial lineage. IDH1 immunonegative (c), ATRX expression retained (d), p53 expression heterogenous (e). The Ki67 index (2%) was low (f)
Discussion
Excluding NF2, extra-axial lesions in CPA in the pediatric age group are extremely rare. Most of the glial tumors in CPA are due to the secondary exophytic growth of cerebellar and brainstem gliomas. The literature has a handful of cases of gliomas in CPA that are exclusively extra-axial. Most of these have been in the adult population and have either been reported as fibrillary glioma or non-specifically as ‘glioma’ [7, 8]. The source of origin has been the proximal segment of the cranial nerves seen in this anatomical cistern. It is vital to preoperatively differentiate an extra-axial CPA lesion from an intra-axial one as the goal of surgery varies accordingly. In our case, the clinical and radiological findings pointed toward vestibular schwannoma and RMSOC (retro mastoid suboccipital craniotomy) was done to explore the CPA [9]. Intraoperatively we found the lesion to have maintained a good anatomic plane with the brainstem and cerebellum however, it was focally adherent to the glial segment of CN VIII, suggesting it to be the site of origin. In a giant tumor, identification and mapping of the facial nerve using EMG is key to the preservation of its function [10]. Prior ventriculoperitoneal shunt not only relieved the intra-cranial pressure but also aided in preventing retraction injury to the cerebellum.
Panse [11] and Cushing [12] were the first to report cases of fibrillary astrocytomas arising from the root entry zone of CN VIII. Subsequently, many cases of CPA gliomas have been reported and the histological diagnoses have ranged from benign pilocytic astrocytoma to fibrillary astrocytoma to high-grade gliomas like glioblastoma. Specific diagnosis of Primary pilocytic astrocytoma in CPA has commonly been reported in adults [2, 3, 13]. However, only three such cases have been reported in the pediatric age group to date. Over the last decade, the advances in the molecular characteristics of brain tumors have led to the revision of brain tumor taxonomy and inception of immunohistochemical analysis and molecular typing for a comprehensive diagnosis. This case is the first of its kind in the era of molecular diagnosis. Arnautovic et al. [4] and Mirone et al. [5] have reported cases of PA in CPA, arising from the glial segment of CN V, but the final diagnosis was based entirely on the histomorphology. As per the fifth edition of WHO classification of CNS tumors (2021), we have performed all the necessary histological and IHC tests that are recommended for a tumor with glial lineage (Table 1). The final diagnosis was reported in the layered integrated structural format, as per the Harlem consensus guidelines [14].
As the cranial nerves emerge from the brain stem, the REZ is subdivided into: the proximal glial segment (surrounded by the astrocytes and oligodendrocytes), the transitional zone, and the distal peripheral segment (surrounded by Schwann cells). Studies by Skinner and Tarlov showed that the glial segment is longest in CN VIII followed by the sensory division of CN V [15, 16]. Arnautovic et al. have proposed that, longer the glial outgrowth greater is the predisposition to gliomas and hence primary pilocytic astrocytoma of CPA arises most commonly from the CN VIII, followed by CN V [4]. However, dearth of cases has kept this hypothesis under the shadow of debate.
Conclusions
We have reported a rare pediatric case of a giant primary pilocytic astrocytoma of CPA, arising from the root entry zone of CN VIII. It is the largest of such tumors reported till date and certainly expands the differential diagnosis for CPA. Being a tumor with low grade features, its complete excision should be the goal for a recurrence free survival. The contentious topics like the diagnosis and origin of these tumors can be settled only by high degree of suspicion, meticulous analysis of imaging, intraoperative assessment, adequate histo-morphological and immunohistochemical analysis, and of course by increased reporting of such cases.
Availability of data and materials
All the data have been made available to the best of my knowledge.
Abbreviations
- CPA:
-
Cerebello-pontine angle
- PA:
-
Pilocytic astrocytoma
- SNHL:
-
Sensori-neural hearing loss
- CT:
-
Computed tomography
- BAER:
-
Brainstem auditory evoked response
- MRI:
-
Magnetic Resonance Imaging
- IAC:
-
Internal auditory canal
- RMSOC:
-
Rretromastoid suboccipital craniotomy
- CUSA:
-
Cavitron ultrasonic aspirator
- REZ:
-
Root entry zone
- EMG:
-
Electromyography
- GFAP:
-
Glial fibrillary acidic protein
- NF:
-
Neurofibromatosis
- WHO:
-
World Health Organization
- CNS:
-
Central nervous system
- PTA:
-
Pure tone audiogram
- IHC:
-
Immuohistochemistry
- IDH:
-
Isocitrate dehydrogenase
- ATRX:
-
α-Thalassemia mental retardation X-linked protein
- TR:
-
Transverse
- AP:
-
Antero-posterior
- CC:
-
Cranio-caudal
References
Burkhard C, Di Patre PL, Schüler D, Schüler G, Yaşargil MG, Yonekawa Y, et al. A population-based study of the incidence and survival rates in patients with pilocytic astrocytoma. J Neurosurg. 2003;98(6):1170–4.
Beutler AS, Hsiang JK, Moorhouse DF, Hansen LA, Alksne JF. Pilocytic astrocytoma presenting as an extra-axial tumor in the cerebellopontine angle: case report. Neurosurgery. 1995;37(1):125–8.
Francesco F, Maurizio I, Stefano C, Marina S, Ugo S, Massimo S. Trigeminal nerve root entry zone pilocytic astrocytoma in an adult: a rare case of an extraparenchymal tumor. J Neurooncol. 2010;97(2):285–90.
Arnautovic KI, Husain MM, Linskey ME. Cranial nerve root entry zone primary cerebellopontine angle gliomas: a rare and poorly recognized subset of extraparenchymal tumors. J Neurooncol. 2000;49(3):205–12.
Mirone G, Schiabello L, Chibbaro S, Bouazza S, George B. Pediatric primary pilocytic astrocytoma of the cerebellopontine angle: a case report. Childs Nerv Syst. 2009;25(2):247–51.
Zakaria Z, Raja Mohd Rasi RZ, Rahman NAA. Primary pilocytic astrocytoma of the cerebellopontine angle in pediatric patient with neurofibromatosis type 1: a case report. Egypt J Neurosurg. 2022;37(1):28. https://doi.org/10.1186/s41984-022-00168-8.
Kasantikul V, Palmer JO, Netsky MG, Glasscock ME 3rd, Hays JW. Glioma of the acoustic nerve. Arch Otolaryngol. 1980;106(8):456–9.
Gonzalez RA. Differential diagnosis of tumors at the cerebellopontine recess. Bull Johns Hopkins Hosp. 1948;83(3):187–212.
Cohen-Gadol A. Retromastoid craniotomy: an adaptable and panoramic approach to the cerebellopontine angle. World Neurosurg. 2021;147:257–67.
Vivas EX, Carlson ML, Neff BA. Congress of neurological surgeons systematic review and evidence-based guidelines on intraoperative cranial nerve monitoring in vestibular schwannoma surgery. Neurosurgery. 2018;82(2):E44–6.
Panse R. Ein Gliom des Akustikus. Arch Ohr Heilk. 1904;61(251–255):1904.
Cushing H. Tumors of nervus akustikus and syndrome of the cerebellopontine angle. Philadelphia: WB Saunders Co; 1917.
Dutta G, Singh D, Singh H, Sachdeva D, Kumar V, Chaturvedi A. Pilocytic astrocytoma of the cerebellopontine angle mimicking vestibular schwannoma: report of a rare entity. Br J Neurosurg. 2020;34(1):107–9.
Louis DN, Perry A, Burger P, Ellison DW, Reifenberger G, von Deimling A. International society of neuropathology—Haarlem consensus guidelines for nervous system tumor classification and grading. Brain Pathol. 2014;24(5):429–35.
Skinner HA. Some histological features of cranial nerves. Arch Neurol Psych. 1931;25:356–72.
Tarlov IM. Structure of the nerve root. Arch Neurol Psych. 1937;37:1338–55.
Funding
No source of funding for the article.
Author information
Authors and Affiliations
Contributions
ICP has conceptualized and written the manuscript. DJM has helped in collecting the data and compiling it. All authors read and approve the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval has been taken from the ethics committee.
Consent for publication
Has been taken from the patient’s father.
Competing interests
There is no competing of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahakul, D.J., Premsagar, I.C. Primary pilocytic astrocytoma of cerebello-pontine angle in the pediatric age group: literature review and case report. Egypt J Neurosurg 38, 25 (2023). https://doi.org/10.1186/s41984-023-00202-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-023-00202-3