Abstract
Background
Pilocytic astrocytomas are the most common primary brain tumors in children. Most of the lesions occur in or near the midline. They are rare in extra-axial locations.
Case presentation
We report a 23-year-old lady who was found to have progressive right-sided sensorineural hearing loss and features of raised intracranial pressure due to a pilocytic astrocytoma of the right cerebellopontine angle. After an extensive Medline search, we could find only three cases of primary extra-axial pilocytic astrocytoma of the cerebellopontine angle (CPA) reported till now.
Conclusion
Even a rare occurrence, primary pilocytic astrocytoma, and in general gliomas, should be kept in mind in the differential diagnosis of CPA lesions.
Similar content being viewed by others
Background
Pilocytic astrocytomas (PA) are the most common primary brain tumors in children. Approximately, 80% of PA occurs in the first two decades of life. Most of the lesions occur in or near the midline. Common locations include the cerebellum, the optic nerve and chiasm, and the hypothalamus. They are rare in extra-axial locations.
After an extensive Medline search, we could find only three cases of primary extra-axial pilocytic astrocytoma of the cerebellopontine angle (CPA) reported till now [1,2,3]. We recently encountered a right CPA pilocytic astrocytoma arising from the eighth cranial nerve, completely separated from the brain stem in a 23-year-old lady. The provisional diagnoses on preoperative neuroimaging included arachnoid cyst versus cystic schwannoma.
Case presentation
A 23-year-old female presented with 1.5 years of progressive right-sided sensorineural hearing loss (SNHL) and features of raised intracranial pressure (ICP) like headache and vomiting for 3 months. Signs of cerebellar compression like dysdiadochokinesia and past pointing were present on the right side. Her tandem gait was impaired with swaying toward the right side. No clinical evidence of any other cranial nerve involvement. She had no features of Neurofibromatosis (NF). Pure tone audiometry showed right-sided severe SNHL.
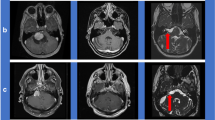
Magnetic resonance (MR) study
The brain MR showed well defined, extra-axial cystic appearing lesion of 29 × 35 × 25 mm seen in the right CPA cistern. The mass is hypointense on T1 and FLAIR, hyperintense on T2 without restricted diffusion and no contrast enhancement. The provisional diagnoses included arachnoid cyst versus cystic schwannoma (Fig. 1).
Surgery
With intraoperative neuromonitoring, a right retromastoid sub-occipital (RMSO) craniotomy was performed. On exposure, there was a completely cystic mass. No solid component was visualized. The arachnoid plane was well preserved all around between the mass and the cerebellum. The mass was arising from the eighth cranial nerve and was completely separated from the brain stem. Under the microscope, a gross total resection was accomplished. The content of the cyst was clear colorless resembling cerebrospinal fluid (CSF).
Pathology
The histopathological examination revealed glial tissue along with a fibro-collagenous cyst wall. The glial tissue appeared mildly cellular showing regimented nuclei focally with few eosinophilic granular bodies and an occasional Rosenthal fiber. The individual cells were elongated with bipolar processes and bland nuclei. No mitosis or necrosis or atypia was seen. Features consistent with pilocytic astrocytoma (Fig. 2).
Postoperative course
Immediately postoperatively, the features of raised ICP were relieved but the hearing loss remained unchanged. There were no new postoperative deficits. At 3 months follow-up, there was a significant improvement in hearing loss and the patient had no other complaints.
Discussion
Pilocytic astrocytomas are the most common primary brain tumors in children. They are classified as WHO grade I tumors because of their benign and slow-growing nature [4]. They represent 85% of cerebellar and 10% of cerebral astrocytomas [5]. Approximately, 15% of patients with Neurofibromatosis type 1 (NF1) develop PA [6].
Peak incidence is between 5 and 15 years of age. Approximately, 80% of PA occurs in patients less than 20 years [7]. There is no sex predilection.
Most of the lesions occur in or near the midline. Common locations include the cerebellum, the optic nerve and chiasm, and the hypothalamus. Less common locations include basal ganglia, brainstem, cerebral hemispheres, and spinal cord [8]. They are rare in extra-axial locations. After an extensive Medline search, we could find only three cases of primary extra-axial pilocytic astrocytoma of the CPA reported till now. Two of them were seen in adults and one in a 12 year old boy. All of them presented with progressive hearing loss and mimicked cystic schwannoma. In all three cases, the tumor was adhered to the cochlear and vestibular nerves. In two of them, the nerves had to be sacrificed for gross total resection, while in one case the mass could be resected without nerve sacrifice. In our case, gross total resection was accomplished without any nerve sacrifice.
Microscopically, PA displays low cellularity with a typical biphasic pattern: compacted bipolar cells with Rosenthal fibers and loose-textured multipolar cells with granular bodies and microcysts.
On Computed Tomography (CT), PAs are typically discrete localized cystic and solid masses located in the posterior fossa. The solid components of these tumors are iso-to slightly hypodense compared with the adjacent brain on non-contrast CT and nearly always enhance following contrast administration. 20–30% of PAs may be entirely solid [9]. Calcification is present in up to 20% [10]. Hemorrhage is rare.
On MR, the solid components of these tumors appear iso-to slightly hypointense relative to grey matter, while the cyst contents are iso-to slightly hyperintense to CSF on T1 weighted images. On T2 weighted images, the solid portions are hyperintense to grey matter. Cyst contents are slightly hyperintense relative to CSF on both T2 weighted images and FLAIR [5]. Peritumoral edema is not usually present. Virtually, all these tumors enhance and enhancement is usually intense but heterogeneous. Cyst wall enhancement may also be seen.
The definitive therapy for PAs is the complete resection of the tumors. The recurrence-free survival rates after gross total resection are higher than 90% [11, 12]. Radiotherapy (RT) can be used as adjuvant treatment in residual tumors or surgically inaccessible tumors such as brainstem/thalamic/optic nerve Pas [13]. However, in young children chemotherapy has been used to delay the need for RT because of well-documented side effects like neurocognitive and neuroendocrine deficits [14, 15].
Conclusions
Pilocytic astrocytomas are rarely seen as primary extra-axial tumors of the cerebellopontine angle. Here, we presented a 23-year-old female with such a lesion who underwent surgical resection of the lesion with postoperative neurological improvement. This case highlights that even if a rare occurrence, primary pilocytic astrocytoma, and in general gliomas, should be kept in mind in the differential diagnosis of CPA lesions.
Abbreviations
- CPA:
-
Cerebellopontine angle
- PA:
-
Pilocytic astrocytomas
- SNHL:
-
Sensorineural hearing loss
- ICP:
-
Intracranial pressure
- CSF:
-
Cerebrospinal fluid
- RT:
-
Radiotherapy
- CT:
-
Computed Tomography
- NF 1:
-
Neurofibromatosis type 1 (NF1)
References
Beutler A, Hsiang J, Moorhouse D, Hansen L, Alksne J. Pilocytic astrocytoma presenting as an extra-axial tumor in the cerebellopontine angle: case report. Neurosurgery. 1995;37:125–8.
Mirone G, Schiabello L, Chibbaro S, Bouazza S, George B. Pediatric primary pilocytic astrocytoma of the cerebellopontine angle: a case report. Childs Nerv Syst. 2009;25:247–51.
Dutta G, Singh D, Singh H, Sachdeva D, Kumar V, Chaturvedi A. Pilocytic astrocytoma of the cerebellopontine angle mimicking vestibular schwannoma: report of a rare entity. Br J Neurosurg. 2017. https://doi.org/10.1080/02688697.2017.1419163.
Louis D, Perry A, Reifenberger G, Deimling A, Branger D, Cavenee W, et al. The 2016 World Health Organization classification of tumors of the central nervous system. Acta Neuropathol. 2016;131(6):803–20.
Koeller KK, Rushing EJ. From the archives of the AFIP: pilocytic astrocytoma: radiologic-pathologic correlation. Radiographics. 2004;24:1693–708.
Listernick R, Ferner R, Liu G, Gurmann D. Optic pathway gliomas in neurofibromatosis-1: controversies and recommendations. Ann Neurol. 2007;61:189–98.
Wallner KE, Gonzales MF, Edwards MSB, Wara WM, Sheline GE. Treatment of juvenile pilocytic astrocytoma. J Neurosurg. 1988;69:171–6.
Sadighi Z, Slopis J. Pilocytic astrocytoma: a disease with evolving molecular heterogeneity. J Child Neurol. 2013;28(5):625–32.
Balogun JA, Rutka JT. Surgery of intracranial gliomas in children. Prog Neurol Surg. 2018;30:204–17.
Halpin S, Kingsley D. Disappearance of cerebral calcification as a sign of tumor growth. AJNR. 1993;14:119–22.
Shaw EG, Wisoff JH. Prospective clinical trials of intracranial low-grade glioma in adults and children. J Neuro-Oncol. 2003;5:153–60.
Fisher PG, Tihan T, Goldthwaite PT, et al. Outcome analysis of childhood low-grade astrocytomas. Pediatr Blood Cancer. 2008;51:245–50.
Kidd EA, Mansur DB, Leonard JR, et al. The efficacy of radiation therapy in the management of grade I astrocytomas. J Neuro-Oncol. 2006;76:55–8.
Massimino M, Spreafico F, Cefalo G, Riccardi R, Tesoro-Tess JD, Gandola L, et al. High response rate to cisplatin/etoposide regimen in childhood low-grade glioma. J Clin Oncol. 2002;20:4209–16.
Silva MM, Goldman S, Keating G, Marymont MA, Kalapurakal J, Tomita T. Optic pathway hypothalamic gliomas in children under three years of age: the role of chemotherapy. Pediatr Neurosurg. 2000;33:151–8.
Acknowledgements
Special thanks to the medical team and patients.
Funding
No funding was available.
Author information
Authors and Affiliations
Contributions
The authors described their own experience and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This case report does not require any ethics committee approval. Consent has been obtained by the patient.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bhradwaj, P., Pandey, S., Kumar, P. et al. Pilocytic astrocytoma of the cerebellopontine angle: a rare case. Egypt J Neurosurg 37, 27 (2022). https://doi.org/10.1186/s41984-022-00169-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-022-00169-7