Abstract
The polymorphous low-grade neuroepithelial tumor of young (PLNTY) is considered as one among the low-grade neuroepithelial tumor; as per WHO-2021 classification of Brain Tumors in the fifth edition. The term PLNTY was first coined by Huse in 2016. These morphologically variable tumors are characterized by their oligodendroglioma-like cellular components, infiltrative growth pattern, and Cluster of Differentiation 34 (CD34) immunopositivity. Frequent genetic abnormalities involving mitogen-activated protein kinase pathway constituents like the BRAF proto-oncogene or fibroblast growth receptor 2/3 are harbored by PLNTYs. Radiologically, these are found to be well-circumscribed lesions with calcified and cystic components, affecting primarily temporal lobes. Clinically, they present with seizures/epilepsy in young adults (< 30 years). In the present manuscript we are reporting a case of 37-year-old male, presenting with a gradually progressive headache for 6 months, found to have a left frontal multiloculated cystic lesion with dystrophic calcifications. Based on the distinctive histopathological feature of the oligodendroglioma-like infiltrative lesion showing CD34 immunopositivity, a diagnosis of a polymorphous low-grade neuroepithelial tumor of young was made.
Similar content being viewed by others
Introduction
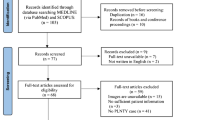
The low-grade neuroepithelial tumors (LGNTs) are an assorted group of epileptogenic lesions encountered in children and young adults. [1, 2] With a varying spectrum of histologic features and glial or glioneuronal differentiation, the traditionally defined subtypes of LGNTs include diffuse astrocytomas, pilocytic astrocytomas, gangliogliomas, pleomorphic xanthoastrocytomas (PXAs), dysembryoplastic neuroepithelial tumors (DNETs), angiocentric gliomas, and oligodendrogliomas. [3] The diagnostic criterion for these LGNTs (especially glioneuronal variants), representing a broad neuropathological spectrum, are not distinct, and hence, impedes proper diagnosis and prognostication. Contrary to these difficulties are the recent advances in the field of molecular diagnostics which have brought about a more accurate system of tumor classification, one based on gene expression profiles and DNA methylation patterns. Incorporating these established molecular advancements, 2021 WHO CNS-5 classification has recognized six new tumor types in the LGNTs alone. [2] Here, we report a rare occurrence of frontal lobe PLNTY in a young man, without any associated seizures/epilepsy.
Case report
A 37-year-old gentleman presented with a history of gradually progressive headache for 6 months. There was no history of seizure episodes. Detailed neurological examination revealed a grossly normal status, except for a positive right-sided pronator drift suggestive of subtle weakness. Fundus examination was normal. The patient had no known comorbidities, with no significant past or family history either. Magnetic resonance imaging (MRI) of the brain showed an intra-axial multilocular cystic lesion with septations involving left frontal white matter, measuring approximately 73 × 52 mm in size (Fig. 1A–D). There was an associated mild perilesional vasogenic edema as well. The fluid content of the lesion was relatively thick as there was incomplete signal suppression on fluid attenuated inversion recovery (FLAIR) sequence. There was no diffusion restriction within the lesion or along its wall, however, there was an eccentric low signal intensity of dense dystrophic calcification along its wall on gradient echo (GRE) sequence. On gadolinium administration, a thin peripheral enhancement was seen along its wall and septations, and an additional eccentric thick focal multilocular pattern enhancement in the region of calcification (Fig. 1). The lesion was seen causing significant mass effect on the left lateral ventricle, especially the frontal horn, with third ventricle compressed, and periventricular ooze of cerebrospinal fluid (CSF) seen. Left basal ganglia was also compressed and displaced. Based on MRI findings, a provisional diagnosis of cystic glioma-intermediate grade was made. Patient was planned for a microsurgical excision of the tumor after undergoing informed written consent as per the operating protocol. A left-sided large fronto-temporal craniotomy was done, and gross total excision of the lesion was achieved. Intraoperatively, the lesion’s cystic portion contained sanguineous fluid, and the tumor capsule was at some parts thick grayish to light brown in color and at other areas it was thin and pale yellow in color. Area of dystrophic calcification was identified and excised. Patient had an unremarkable postoperative hospital stay without any fresh deficits. The collected tumor specimen was sent for detailed histopathological examination and molecular testing. Microscopic sections were studied which showed a tumor exhibiting both infiltrative and compact growth patterns, with predominantly oligodendroglioma-like component (Fig. 2A). The cells had uniformly small and round nuclei with perinuclear haloes, and places exhibiting varying degrees of nuclear pleomorphisms. Intra-nuclear inclusions were also present. Some cells also had astrocytic morphology, and some were ambiguous in appearance. Some cells were fibrillary, spindled, pleomorphic and displayed perivascular pseudo-rosettes. Extensive foci of calcification were also present (Fig. 2B). Areas showing eosinophilic granular bodies and few ganglion cells were also evident. Immunohistochemical analysis of the pathological specimen revealed the following status—Isocitrate dehydrogenase 1 (IDH1)- R132H negative (non-mutant); Glial fibrillary acidic protein (GFAP), S100, synaptophysin positive (Fig. 2C–D); Oligodendrocyte transcription factor 2 (OLIG2) positive (Fig. 2E); CD34 focally positive. Furthermore, the tumor was negative for epithelial membrane antigen (EMA) and thyroid transcription factor 1 (TTF1), with the Mib 1 (Ki-67) proliferation index of 2%. Though the confirmation of genetic alterations involving MAPK pathway constituents (BRAF proto-oncogene or FGFR 2/3) remained pending, the histopathological and other molecular findings conclusively gave the impression of a polymorphous low-grade neuroepithelial tumor of the young (PLNTY), CNS WHO grade 1. Postoperative MRI showed near total excision of the tumor (Fig. 3).
Preoperative axial brain T1WI (A), and T2WI B demonstrates an intra-axial multilocular cystic lesion with septations involving left frontal white matter, measuring approximately 73 × 52 mm in size. Post-contrast T1-weighted axial C cut shows eccentric focal multilocular pattern enhancement around the calcification. Gradient echo (GRE) sequence D confirms the eccentric low signal intensity of dense dystrophic calcification
Microscopic appearance of the tumor. A Image shows a tumor exhibiting an oligodendroglioma-like component predominating (hematoxylin and eosin [H&E]). B Dense calcifications seen within tumor components (H&E). C Immunopositivity demonstrated by the tumor can be seen with synaptophysin and D Glial fibrillary acidic protein—GFAP stains. E Image showing the tumor exhibiting Oligodendrocyte transcription factor 2 (OLIG2) positivity
Discussion
PLNTY is a recently described variant of LGNT, presenting usually as an epileptogenic lesion in young adults. They are characterized by their infiltrative growth pattern, oligodendrocyte-like cells showing CD34 immunopositivity, and evidence of MAPK pathway abnormalities (either BRAF or FGFR2/ FGFR3 mutations). [4] Polymorphous low-grade neuroepithelial tumor of young (PLNTY) is one among them. First described by Huse et al. in 2016, these morphologically variable tumors are characterized by their oligodendroglioma-like cellular components, infiltrative growth pattern, and Cluster of Differentiation 34 (CD34) immunopositivity. [4] To date, only around 50 clinical cases of PLNTY have been described in the literature. [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18] Since Huse et al.’s pioneering work, every single additional case has added valuable input to the wholesome understanding of this rare disease entity. [4] Frequent genetic abnormalities involving mitogen-activated protein kinase (MAPK) pathway constituents like the BRAF proto-oncogene or fibroblast growth receptor 2/3 (FGFR 2/3) are harbored by PLNTYs. Radiologically, these are found to be well-circumscribed lesions with calcified and cystic components, affecting primarily temporal lobes. Clinically, they present with seizures/epilepsy in young adults (< 30 years). [4]
Clinico-radiological characteristics
Though the PLNTY’s age predilection has been reported to be in the range of 2 to 57 years, most cases present under the age of 30 years. [4, 5, 9, 11, 16, 18] It has an equal sex preponderance. Among the 49 cases reported till date, only five of them (including the index case) had non-epileptic clinical presentations like headache, imbalance, and behavioral abnormalities. [3, 4, 6] Such non-epileptic presentations are predominantly associated with extratemporal lesions which account for about one-third of the cases. [3, 4] Radiologically, the important attributes favoring PLNTY have been excellently described by Kurokawa et al. via their systematic analysis. [19] They found PLNTYs to be exclusively supratentorial tumors, with common radiological features as follows—cortical or subcortical masses (95.8%) in the temporal lobe (66.7%); calcification (83.3%); circumscribed margins (72.7%); solid-cystic components (66.6%), and T2-weighted imaging hyperintensity (50.0%). Fei et al. (2022) observed that the epileptic zone identification is critical for every case of PLNTY, and an enlarged surgical resection (vs recommended gross total resection) may provide better postoperative seizure controls. Hence, the identification of epileptic zone and maximum safe resection (under the use of intra-operative adjuncts) have been found to have better outcome as compared to the recommended gross total resection.
Pathological characteristics
PLNTY’s low-grade nature, presence of infiltrating oligodendrocyte-like cells, and its common association with cortical dysplasia are well-established. [15] The diagnostic dilemma of differentiating these tumors from an oligodendroglioma is solved by the exclusive CD34 immunopositivity of the PLNTYs. [4] CD34, a transmembrane phosphor-glycoprotein of early neurulation, is not expressed in mature brain cells. The presence of CD34 has been shown to correspond to drug-resistant epilepsy. Markers of glial differentiation (GFAP and Olig2) may be positive in both tumors. Notably, PLNTYs also lack immunopositivity to markers of neuronal differentiation, like NeuN, which plays a pivotal role in differentiating these from other LGNTs. In every case, the final diagnosis should be arrived upon only after considering the molecular profile, and not on pure histology basis. PLNTYs are known to harbor MAPK pathway alterations in the form of demonstrable BRAF or FGFR2/FGFR3 mutations. [20] On the contrary, their usually mimic, oligodendrogliomas, have IDH mutations and 1p/19q codeletions. Consistent with their low-grade classification, PLNTYs have a Ki-67 labeling index typically less than 5%. BRAF V600E mutations are not unique to PLNTYs alone. They have associations with other LGNTs (like gangliogliomas, PXAs) as well. [20, 21] Alterations in FGFR2/3, belonging to the transmembrane tyrosine kinase receptor family, have been described with several different fusion partners (like FGFR3TACC3, FGFR2-KIAA198, FGFR2-CTNNA3). The result of these fusions is an alteration in the downstream effectors enhancing activation of the MAPK pathway. [20] FGFR3TACC3 fusion (also described in a few glioblastomas) has been reported from the only PLNTY with malignant transformation. [5]
Genetic study
In genetic study mutations in the 52 genes relevant to solid tumors were assessed using next generation sequencing (NGS). The result of genetic study revealed no pathogenic variants of BRAF, IDH1 and IDH2 genes. No fusion identified in NTRK, ALK, RET, FGFR2 and FGFR3 genes.
Conclusions
PLNTY is a recently described rare low-grade epileptogenic tumor of the young. Gross total resection seems to be curative. Only three cases have been reported to date with radiological recurrence during follow-up periods. [4, 5, 17] Adjuvant radiotherapy and chemotherapy were resorted to in the only case of malignant transformation reported. [5] Data on seizure outcomes in PLNTYs need further elaboration.
Availability of data and material
Not applicable.
Abbreviations
- CD34:
-
Cluster of Differentiation 34
- CSF:
-
Cerebrospinal fluid
- FGFR 2/3:
-
Fibroblast growth receptor 2/3
- FLAIR:
-
Fluid-attenuated inversion recovery
- GRE:
-
Gradient echo sequence
- LGNTs:
-
Low-grade neuroepithelial tumor
- MAPK:
-
Mitogen-activated protein
- MRI:
-
Magnetic resonance imaging
- PLNTY:
-
Polymorphous low-grade neuroepithelial tumor of young
References
Bale TA, Rosenblum MK. The 2021 WHO classification of tumors of the central nervous system: an update on pediatric low-grade gliomas and glioneuronal tumors. Brain Pathol. 2023;2022:e13060.
Louis DN, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021;23(8):1231–51.
Riva G, et al. Low-grade neuroepithelial tumor: unusual presentation in an adult without history of seizures. Neuropathology. 2018;38(5):557–60.
Huse JT, et al. Polymorphous low-grade neuroepithelial tumor of the young (PLNTY): an epileptogenic neoplasm with oligodendroglioma-like components, aberrant CD34 expression, and genetic alterations involving the MAP kinase pathway. Acta Neuropathol. 2017;133(3):417–29.
Bale TA, et al. Malignant transformation of a polymorphous low grade neuroepithelial tumor of the young (PLNTY). Acta Neuropathol. 2021;141(1):123–5.
Benson JC, et al. Polymorphous low-grade neuroepithelial tumor of the young as a partially calcified intra-axial mass in an adult. AJNR Am J Neuroradiol. 2020;41(4):573–8.
Bitar M, Danish SF, Rosenblum MK. A newly diagnosed case of polymorphous low-grade neuroepithelial tumor of the young. Clin Neuropathol. 2018;37(4):178–81.
Broggi G, et al. A “polymorphous low-grade neuroepithelial tumor of the young (PLNTY)” diagnosed in an adult. Report of a case and review of the literature. Surg Neurol Int. 2021;12:470.
Chen Y, et al. Polymorphous low-grade neuroepithelial tumor of the young: case report and review focus on the radiological features and genetic alterations. BMC Neurol. 2020;20(1):123.
Fei X, et al. Clinical, radiological, pathological features and seizure outcome with surgical management of polymorphous low-grade neuroepithelial tumor of the young associated with epilepsy. Front Oncol. 2022;12:863373.
Ge R, et al. Clinicopathological features of polymorphous low-grade neuroepithelial tumor of the young. Zhonghua Bing Li Xue Za Zhi. 2020;49(11):1131–5.
Gupta VR, et al. Polymorphous low-grade neuroepithelial tumor of the young: a case report with genomic findings. World Neurosurg. 2019;132:347–55.
Johnson DR, et al. Plenty of calcification: imaging characterization of polymorphous low-grade neuroepithelial tumor of the young. Neuroradiology. 2019;61(11):1327–32.
Lelotte J, et al. Polymorphous low-grade neuroepithelial tumor of the young: case report of a newly described histopathological entity. Acta Neurol Belg. 2020;120(3):729–32.
Palejwala AH, et al. Polymorphous low-grade neuroepithelial tumor of the young: rare tumor and review of the literature. Rare Tumors. 2022;14:20363613221083360.
Sumdani H, et al. Case report of rarely described polymorphous low-grade neuroepithelial tumor of the young and comparison with oligodendroglioma. World Neurosurg. 2019;127:47–51.
Surrey LF, et al. Genomic analysis of dysembryoplastic neuroepithelial tumor spectrum reveals a diversity of molecular alterations dysregulating the MAPK and PI3K/mTOR pathways. J Neuropathol Exp Neurol. 2019;78(12):1100–11.
Tateishi K, et al. BRAF V600E mutation mediates FDG-methionine uptake mismatch in polymorphous low-grade neuroepithelial tumor of the young. Acta Neuropathol Commun. 2020;8(1):139.
Kurokawa M, et al. Neuroradiological features of the polymorphous low-grade neuroepithelial tumor of the young: five new cases with a systematic review of the literature. Neuroradiology. 2022;64(6):1255–64.
Ida CM, et al. Polymorphous low-grade neuroepithelial tumor of the young (PLNTY): molecular profiling confirms frequent MAPK pathway activation. J Neuropathol Exp Neurol. 2021;80(9):821–9.
Srinivasa K, Cross KA, Dahiya S. BRAF alteration in central and peripheral nervous system tumors. Front Oncol. 2020;10: 574974.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
VPJ, RM and VPM performed literature research and analysis of the originality of the case. The writing phase was done by the whole team. VPJ, AA and VPM were supervised. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Yes.
Competing interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Joshi, V., Chougule, M.V., Mudkanna, A. et al. Atypical presentation of polymorphous low-grade neuroepithelial tumor of young (PLNTY): a case report. Egypt J Neurosurg 38, 7 (2023). https://doi.org/10.1186/s41984-023-00192-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-023-00192-2