Abstract
Background
Spondylodiscitis is infections of the intervertebral disc and adjacent vertebral body with insidious onset. These infections are primarily haematogenous in origin. Early spinal infections after posterior spinal instrumentation usually occur within 3 months after surgery, whereas late infections may occur up to 8 years after surgery but are rare with an incidence of 1.9%.
Case presentation
We describe the case of a 66-year-old woman who complained of febrile back pain and developed late-onset spondylodiscitis 9 years after pedicle screw fixation, which is the longest-onset case. She was treated with surgical instrument removal and thorough debridement of the infected tissue with long-term antimicrobial treatment, with excellent results.
Conclusions
If there is radiculopathy and fever associated with spinal surgery in the history, it should be remembered that evaluation of lumbar spine MRI and acute phase reactions is crucial, and spondylodiscitis should also be considered in the preliminary diagnosis even after 9 years.
Similar content being viewed by others
Background
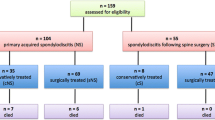
Spondylodiscitis is infections of the intervertebral disc and the adjacent vertebral body with insidious onset [1]. They have a silent clinical course and are therefore difficult to diagnose early [2]. These infections are primarily haematogenous in origin but may also be secondary to tuberculosis or Brucella infections [3]. The lumbar spine is most commonly affected, accounting for 58%, the thoracic spine for 30%, and the cervical spine for 11% [3]. The most commonly detected microorganisms are Staphylococcus aureus and coagulase-negative staphylococci, but despite invasive techniques, aetiologic diagnosis is not always possible [4].
The incidence of iatrogenic spondylodiscitis is increasing with the high number of spinal surgeries and the development of new diagnostic methods. The incidence after lumbar discectomy varies from 0.2 to 4% [4], whereas after posterior spinal fusion and instrumentation, the incidence ranges from 0 to 35% [5].
Early spinal infections after spinal instrumentation usually occur within 3 months of surgery [5, 6], whereas late infections can occur up to 8 years after surgery but are rare, with an incidence of 1.9% of all posterior spinal instrumentation [7]. We present a case of late-onset spondylodiscitis; that occurred 9 years after posterior instrumentation, which is the case that occurs after the longest duration.
Case presentation
A 66-year-old female patient presented with back and right leg pain that had persisted for 1 month. She also complained of night sweats, tremors, and fever that increased up to 39 degrees. It turned out that she had lumbar spinal stenosis and had been operated 9 years ago with bilateral transpedicular screws in the L4 and L5 vertebrae and two rods (Fig. 1). There were no other chronic diseases or previous infections in her medical history. Physical examination revealed restricted range of motion in the proximal muscle groups of both lower extremities, which was due to hyperalgesia. Right lower extremity thigh flexion and extension strength was 3/5; right dorsiflexion and EHL were 4/5.
On blood tests, the patient's white blood cell count was 18,800, with an erythrocyte sedimentation rate of 119 mm/h, a C-reactive protein value of 139.15 mg/dL, and a procalcitonin value of 0.83 ng/mL. Blood cultures were obtained, and tests performed to determine the cause of infection revealed no evidence of Brucella, tuberculosis, or infective endocarditis.
Computed tomography of the lumbar spine revealed pedicle screw fixators at the level of the L4–5 vertebrae. A degenerative vacuum phenomenon was noted in the lumbar intervertebral disc (Fig. 2). Because of the patient's allergy to contrast media, non-contrast-enhanced lumbar spine magnetic resonance imaging (MRI) was performed. In addition to an anterior bone fusion at the L4–5 level, prominent oedematous inflammatory changes were observed in both vertebrae and paravertebral areas (Fig. 3). At the same time, the intervertebral disc was found to be markedly narrowed, so spondylodiscitis was considered as a preliminary diagnosis.
The screws were surgically removed and thorough debridement of the infected tissue was performed (Fig. 4). A specimen from the lumbar region with an open biopsy was sent for pathological and microbiological examination. There was no multiplication in the patient's cultures. Microscopy revealed a strong neutrophilic leukocyte infiltration and palisading epithelioid histiocyte populations. Pathology revealed severe necrosis, inflammatory and focal granulomatous reaction.
She received ampicillin and sulbactam as her first empiric intravenous antibiotherapy. Five days later, treatment with piperacillin–tazobactam was started on the recommendation of the Infectious Diseases Clinic. One week later, antibiotherapy was switched to imipenem and cilastatin sodium. The patient was discharged with an oral antibiotic after intravenous antibiotic treatment was completed for 6 weeks.
Significant regression was observed on lumbar spine MRI scan in the first month of treatment (Fig. 5). It was observed that the pain of the patient, whose spine was immobilized and in whom no additional neurological deficits were noted, regressed with the infection markers. On blood tests at discharge, the patient's white blood cell count was 5940 with a sedimentation rate of 60 mm/h, a C-reactive protein value of 7.95 mg/dL, and a procalcitonin value of less than 0.12 ng/mL.
Conclusions
Infections can occur after all types of spinal surgery [8]. The incidence of iatrogenic spondylodiscitis is increasing with high number of spinal surgeries and the development of new diagnostic methods. In a retrospective study of 6120 cases of posterior spinal fusion and instrumentation, the authors reported 11 patients with postoperative anterior spondylodiscitis [9]. After posterior spinal instrumentation, the incidence ranged from 0 to 35% [5, 10]. Early spinal infections after instrumentation usually occur within 3 months after surgery [5, 6]; whereas late infections can occur up to 8 years after surgery but are rare, with an incidence of 1.9% of all posterior instrumentation [7].
Late-onset spondylodiscitis and psoas abscess 5 years after percutaneous balloon kyphoplasty have been reported [11]. Late tuberculous spondylodiscitis 8 years after discectomy was described by Lotfinia and Vahedi [12]. Besides these long duration periods; no case of spondylodiscitis 9 years after posterior spine surgery has been described so far. Thus, this case demonstrated that the risk of infection persists for up to 9 years after surgery.
The goals of treating spinal infections are to eliminate the microbial pathogen, preserve neurological function, and restore spinal stability and morphology [2, 13, 14]. Antibiotic treatment should be postponed until samples for cultures have been obtained. In the case of negative cultures, intravenous empiric broad-spectrum antibiotic treatment for 6 weeks is recommended for pyogenic spondylodiscitis, and we have adhered to this time period [15].
In addition to conservative treatments, surgical treatment should be considered if symptoms worsen and if inflammatory indicators do not show signs of normalization [16, 17]. In addition, implant infections are considered the main cause of late-onset spinal pain after instrumentation [18, 19]. Biofilm-forming organisms are the main cause of late-onset infections, especially in spondylodiscitis after instrumentation. Therefore, removal of the foreign body is recommended for its eradication, whereas maintaining instrumentation after delayed infection leads to more morbidity and less success [20]. Our patient was treated with surgical instrument removal and thorough debridement of the infected tissue with concomitant long-term antimicrobial treatment, with excellent results.
If there is radiculopathy and fever associated with spinal surgery history, it should be remembered that evaluation of lumbar spine MRI and acute phase reactants is crucial, and spondylodiscitis should also be considered in the preliminary diagnosis even after 9 years.
Availability of data and materials
Not applicable.
Abbreviations
- MRI:
-
Magnetic resonance imaging
References
Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: Update on diagnosis and management. J Antimicrob Chemother. 2010;65(SUPPL. 3):11–24.
Herren C, Jung N, Pishnamaz M, Breuninger M, Siewe J, Sobottke R. Spondylodiscitis: diagnosis and treatment options. Dtsch Arztebl Int. 2017;114(51–52):875–82.
Gentile L, Benazzo F, De Rosa F, Boriani S, Dallagiacoma G, Franceschetti G, et al. A systematic review: characteristics, complications and treatment of spondylodiscitis. Eur Rev Med Pharmacol Sci. 2019;23(2 Suppl):117–28.
Chen S-H, Chen W-J, Wu M-H, Liao J-C, Fu C-J. Postoperative infection in patients undergoing posterior lumbosacral spinal surgery: a pictorial guide for diagnosis and early treatment. Clin Spine Surg. 2018;31(6):225–38.
Weinstein MA, McCabe JP, Cammisa FPJ. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000;13(5):422–6.
Quiñones-Hinojosa A, Jun P, Jacobs R, Rosenberg WS, Weinstein PR. General principles in the medical and surgical management of spinal infections: a multidisciplinary approach. Neurosurg Focus. 2004;17(6):E1.
Wimmer C, Gluch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord. 1998;11(2):124–8.
Gerometta A, Bittan F, Rodriguez Olaverri JC. Postoperative spondilodiscitis. Int Orthop. 2012;36(2):433–8.
Hsieh M-K, Chen L-H, Niu C-C, Fu T-S, Lai P-L, Chen W-J. Postoperative anterior spondylodiscitis after posterior pedicle screw instrumentation. Spine J. 2011;11(1):24–9.
Di Martino A, Papalia R, Albo E, Diaz L, Denaro L, Denaro V. Infection after spinal surgery and procedures. Eur Rev Med Pharmacol Sci. 2019;23(2):173–8.
Alpantaki K, Koutserimpas C, Kofteridis DP, Papastefanou S, Samonis G. Late-onset spondylodiscitis and psoas abscess, 5 years after percutaneous balloon kyphoplasty: a case report. Br J Neurosurg [Internet]. 2019;15:1. https://doi.org/10.1080/02688697.2019.1672856.
Lotfinia I, Vahedi P. Late-onset post-diskectomy tuberculosis at the same operated lumbar level: case report and review of literature. Eur Spine J. 2010;19(SUPPL.2):226–32.
Ryang Y-M, Akbar M. Pyogenic spondylodiscitis: symptoms, diagnostics and therapeutic strategies. Orthopade. 2020;49(8):691–701.
Waheed G, Soliman MAR, Ali AM, Aly MH. Spontaneous spondylodiscitis: review, incidence, management, and clinical outcome in 44 patients. Neurosurg Focus. 2019;46(1):E10.
Rutges JPHJ, Kempen DH, van Dijk M, Oner FC. Outcome of conservative and surgical treatment of pyogenic spondylodiscitis: a systematic literature review. Eur Spine J. 2016;25(4):983–99.
Duarte RM, Vaccaro AR. Spinal infection: state of the art and management algorithm. Eur spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2013;22(12):2787–99.
Skaf GS, Domloj NT, Fehlings MG, Bouclaous CH, Sabbagh AS, Kanafani ZA, et al. Pyogenic spondylodiscitis: an overview. J Infect Public Health [Internet]. 2010;3(1):5–16. https://doi.org/10.1016/j.jiph.2010.01.001.
Gaine WJ, Andrew SM, Chadwick P, Cooke E, Williamson JB. Late operative site pain with isola posterior instrumentation requiring implant removal: infection or metal reaction? Spine (Phila Pa 1976). 2001;26(5):583–7.
Sapkas GS, Mavrogenis AF, Mastrokalos DS, Papadopoulos EC, Papagelopoulos PJ. Postoperative spine infections: a retrospective analysis of 21 patients. Eur J Orthop Surg Traumatol. 2006;16(4):322–6.
Kalfas F, Severi P, Scudieri C. Infection with spinal instrumentation: a 20-year, single-institution experience with review of pathogenesis, diagnosis, prevention, and management. Asian J Neurosurg. 2019;14(4):1181–9.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
OB and YK performed a literature research and analysis of originality of the case. The writing phase was done by the whole team. AYY and IA were supervised. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient included in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kurtulus, Y., Baskurt, O., Yavuz, A.Y. et al. A case of late-onset spondylodiscitis within the longest duration: 9 years after posterior instrumentation. Egypt J Neurosurg 37, 29 (2022). https://doi.org/10.1186/s41984-022-00167-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-022-00167-9