Abstract
Background
Globalisation of terrorism has led to an increase in the number of injuries from the explosion of improvised explosive devices, with complications resulting from the retained shrapnel. It had been found that a third of those who sustained penetrating spinal cord injuries are from explosions. Retained foreign body in the sacral canal segment is rare, especially shrapnel presenting with urinary incontinence. Moreover, the one who had a dramatic recovery of urinary continence following removal of neglected sacral canal shrapnel. We report a case of a delayed improvement (recovery) in urinary continence following removal of neglected sacral canal shrapnel remotely aided by a pelvic floor exercise.
Case presentation
Our patient was a 14-year-old male who presented with a 3-year history of trauma to the lower back from an Improvised Explosive Device. He was initially associated with difficulty in walking that improved over eight months. However, the urinary incontinence persisted. He was found to be preserved with no neurological deficit in the lower limb. There was a lower back, midline wound, discharging pus. Lumbosacral imaging revealed a sacral (S2) canal Shrapnel. As a case of urinary incontinence from sacral shrapnel, he had the removal of the shrapnel, did well postoperatively, commenced on pelvic floor exercise. He became continence of urine over time.
Conclusions
Retained foreign bodies in the spinal canal are associated with complications that include neurological deficit. Neglected (long-standing) sacral shrapnel with urinary incontinence is rare; moreover, the recovery of the continence with the removal of the shrapnel is aided by the commencement of pelvic floor exercise.
Similar content being viewed by others
Background
Shrapnel gets its name from General Henry Shrapnel of the British Army's Royal Artillery, who, during the Peninsular War, invented an exploding shell that breaks apart and shatter when it is detonated [1]. With the globalisation of terrorism, a significant concern, blast wounds from improvised explosive devices (IEDs) are frequently encountered outside the battlefield, resulting in numerous shrapnel injuries [2].
Following an explosion, gunshot injuries, or motor vehicle accident, penetration and retention of foreign bodies (including shrapnel) are pretty common. Likewise, Blair [3] et al. found that explosives are responsible for a third of those who sustain penetrating injury to the spine.
Foreign bodies in the sacrum are rare. However, there are reports of findings of a nail, wood, and glass [4,5,6], respectively.
Retained foreign body from within the spinal canal may result in complications like a cerebrospinal fluid leak, osteomyelitis, meningitis, migration of the foreign body, and progressive neurologic deficits [7]. Currently, there is a paucity of literature regarding the management and outcome of such injuries due to explosive mechanisms [8, 9]. Common English search engines could not return reports on removing sacral shrapnel and resultant spontaneous recovery of urinary continence. We report a case with urinary incontinence for three (3) years from a retained sacral shrapnel following an IED explosion. He became continence of urine after the surgery with pelvic floor exercise.
Case presentation
We report a 14-year-old boy referred to our facility with a 3-year history of urinary incontinence following trauma to his lower back from an Improvised Explosive Device (IED) explosion. Developed initial difficulty in walking that improved over eight months, currently ambulant. However, he had persistent urinary incontinence and residual low back wound. There was no loss of consciousness, faecal incontinence or feature suggestive of foot drop. Other systems were essentially normal. Medical, family and psychosocial histories are non-contributory.
Examination revealed a preserved but depressed-looking teenager, smelling of urine, afebrile, not pale, with stable vitals. Neurological examination revealed lower limbs muscle power of Medical Research Council (MRC) grade 5/5 in all the muscle groups; the sensation was preserved, with no saddle anaesthesia. Back examination revealed a lower back (sacral area) wound discharging pus, about 3 cm to the right of the midline, mildly tender, no palpable mass, as shown in Fig. 1a below. Digital Rectal Exam (DRE) indicated an excellent sphincter tone. Other systemic examinations were essentially normal.
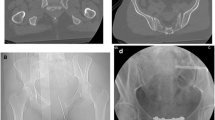
Lumbosacral X-ray revealed an opacity of metallic density (shrapnel) in the Second Sacral (S2) canal, lying diagonally, as shown in Fig. 1b, c below in Fig. 1.
Wound swab Microscopy, Culture and Sensitivity (MCS) was sterile. His packed Cell Volume was 38%, Electrolyte, Urea, Creatinine and urinalysis were normal.
Lumbosacral Computed Tomography Scan (CT scan) with sagittal reconstruction showed a nearly rectangular hyper dense foreign body of metallic density in the spinal canal of S2, with defective dorsum and cauda equina compression as shown in Fig. 2a, b below in Fig. 2.
He was counselled for surgical removal of the shrapnel under general anaesthesia. He was intubated with an "armoured" endotracheal tube, turned prone on bolsters around pressure points, cleaned and draped, exposing the sacral area. The shrapnel’s position was localised with the use of a C-arm fluoroscope. The sacrum was exposed through a midline incision, and a fractured part was found around the shrapnel. After enlarging the fractured entry point, the shrapnel was fully exposed (Fig. 2c) and removed. The removed shrapnel was a dark metal, nearly rectangular, about 30 mm long and 8 mm wide (as in Fig. 2d), as shown in Fig. 2 above.
The discharging sinus was excised, and tissue was sent for microscopy, culture and sensitivity, wound cleaned with dilute hydrogen peroxide (H2O2) and normal saline, wounds closed and dressed. No intra-operative or post-operative cerebrospinal fluid (CSF) leak was observed. He was placed on broad-spectrum antibiotics; the culture result was sterile. The wound healed with no residual infection.
He was commenced on pelvic floor exercise from the third day post-op, wound stitches removed on the tenth day and subsequently discharged home to continue pelvic floor exercise. At the second follow-up (about 8 weeks after the surgery), the patient reported an onset of urinary continence.
Discussion
Blast and gunshot-related injuries are common in countries where war/terrorist activities are prevalent, like in our setting, ravaged by civil-military conflict (Boko Haram terrorists). Such injuries are associated with retained shrapnel or bullets. Long-term complications of retained shrapnel depend on the anatomical location and interaction with the tissues.
Our patient presented with an incomplete spinal cord injury (urinary incontinence only) due to penetrating shrapnel from an IED blast. Such penetrations are said to be a fairly common finding, as reported by Blair [3] from studies in Iraq and Afghanistan, where he found that about one third (1/3) of penetrating spinal injuries are from explosions.
Presentations with a neurological deficit (urinary incontinence) and discharge of pus from the wound are some of the common complications that are likely among others; this agrees with the findings of Bhatoe [10].
Indications for surgical management of penetrating SCI include rapid neurological deterioration, radiographic evidence of spinal cord or nerve root compression, mechanical instability, abscess, cerebrospinal fluid (CSF) leakage, and chronic pain [11, 12].
Like any other metallic foreign body, the diagnosis was made from a plain radiograph and a computed tomography (CT) Scan of the Lumbosacral Spine. Shahlaie [13] had stressed the importance of CT scans in identifying the site, trajectory and planning of surgery.
The shrapnel was removed under general anaesthesia following localisation with fluoroscopy. Studies demonstrated that fluoroscopic image intensifier is a valuable and safe method to detect a foreign body (FB) preoperatively and intraoperatively [14, 15].
After the extraction of the neglected shrapnel and subsequent pelvic floor exercise, he noticed a gradual improvement in his continence, making us presume that he must have improved after the surgical intervention (removal of the shrapnel). The patient’s improvement in urinary continence within two (2) months of removing neglected shrapnel suggest that the surgery might have sped up the process. Though there were few studies on patients that improved clinically after undergoing similar intervention, our patient probably belongs to the 70% of patients that were found to have improved following surgical intervention, as reported by Lawless [16]. However, Lawless [16] found in the second group of his patients that as many as 81% had improved clinically without any form of surgical intervention; this is at variance with our patient who was incontinent for three (3) years before the surgical intervention. Worthy of note is the significant difference in duration of symptoms of his patients upon presentation averaging 2 weeks (early), compared to our patient that presented three (3) years after the injury (late).
Conclusion
Spinal Cord Injury (SCI) due to explosive shrapnel has increased in recent military conflicts. Contributing to this are increasing acts of terrorism, to a much higher degree than in any previous period. Despite recovering from a cauda equina syndrome three (3) years earlier, worthy of note is the persistence of urinary incontinence, which resolved about two (2) months after the removal of the neglected sacral shrapnel, aided probably by an active pelvic floor exercise.
Availability of data and materials
Not applicable.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- CT Scan:
-
Computed tomography scan
- DRE:
-
Digital rectal examination
- FB:
-
Foreign body
- H2O2 :
-
Hydrogen peroxide
- IED:
-
Improvised explosive device
- MCS:
-
Microscopy, culture and sensitivity
- MRC:
-
Medical Research Council
- S2:
-
Sacral 2
- SCI:
-
Spinal cord injury
References
https://www.vocabulary.com/dictionary/shrapnel. Accessed 5 August 2021.
Singh AK, Ditkofsky NG, York JD, et al. Blast injuries: from improvised explosive device blasts to the boston marathon bombing. Radiographics. 2016;36(1):295–307. https://doi.org/10.1148/rg.2016150114.
Blair JA, Patzkowski JC, Schoenfeld AJ, et al. Spinal column injuries among Americans in the global war on terrorism. J Bone Joint Surg Am. 2012;94(18):e1351–9. https://doi.org/10.2106/JBJS.K.00502.
Stern LC, Moore TA. Nail gun injury to the sacrum: case report and review of the literature. Spine. 2011;36:E1778-1780.
Gul S, Dusak A, Songur M, Kalayci M, Acikgoz B. Penetrating spinal injury with a wooden fragment: a case report and review of the literature. Spine. 2010;35:E1534-1536.
Fattahi A, Jahanbakhshi A, Shahivand A, Dastmalchi A. Penetrating sacral injury with a wooden foreign body. Case Rep Med. 2018;2018:1–3. https://doi.org/10.1155/2018/1630864.
Manzone P, Domenech V, Forlino D. Stab injury of the spinal cord surgically treated. J Spinal Disord. 2001;14:264–7.
Janković S, Busić Z, Primorac D. Spine and spinal cord war injuries during the war in Croatia. Mil Med. 1998;163:847–9.
Kang DG, Lehman RA Jr, Carragee EJ. Wartime spine injuries: understanding the improvised explosive device and biophysics of blast trauma. Spine J. 2012;12:849–57.
Bhatoe HS, Singh P. Missile injuries of the spine. Neurol India. 2003;51:507–11.
Kahraman S, Gonul E, Kayali H, Sirin S, Duz B, Beduk A, et al. Retrospective analysis of spinal missile injuries. Neurosurg Rev. 2004;27:42–5.
Klimo P Jr, Ragel BT, Rosner M, Gluf W, McCafferty R. Can surgery improve neurological function in penetrating spinal injury? A review of the military and civilian literature and treatment recommendations for military neurosurgeons. Neurosurg Focus. 2010;28(5):E4. https://doi.org/10.3171/2010.2.FOCUS1036.
Shahlaie K, Chang DJ, Anderson JT. "Nonmissile penetrating spinal injury. Case report and review of the literature. J Neurosurg Spine. 2006;4(5):400–8.
Sencimen M, Bayar GR, Gulses A. Removal of the retained suture needle under C-arm fluoroscopy: a technical note. Dent Traumatol. 2010;26(6):527–9.
Park SS, Yang HJ, Lee UL, Kwon MS, Kim MJ, Lee JH, et al. The clinical application of the dental mini C-arm for the removal of broken instruments in soft and hard tissue in the oral and maxillofacial area. J Craniomaxillofac Surg. 2012;40(7):572–8.
Lawless MH, Lytle EJ, McGlynn AF, Engler JA. Surgical management of penetrating spinal cord injury primarily due to shrapnel and its effect on neurological outcome: a literature review and meta-analysis. J Neurosurg Spine. 2018;28(1):63–71.
Acknowledgements
All the residents in Neurosurgery and Urology of the University of Maiduguri Teaching Hospital.
Funding
None.
Author information
Authors and Affiliations
Contributions
BU—conceptualised, literature search, managed the patient, wrote. BM—literature search, managed the patient, proofread. HMD—literature search, managed the patient, proofread. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and the consent to participate
Ethical approval and the consent to participate were obtained from our Hospitals Ethical committee. The parent and the guardian of the patient had signed an informed consent and agreed for the case report to be published.
Consent for publication
The parent and the guardian of the patient had signed an informed consent and agreed for the case report to be published.
Competing interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Usman, B., Mohammed, B. & Dogo, H.M. Delayed return of urinary continence following the removal of neglected sacral shrapnel. Egypt J Neurosurg 37, 14 (2022). https://doi.org/10.1186/s41984-022-00154-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-022-00154-0