Abstract
Background
Finding an aneurysmal bone cyst in the skull is rare and for a neurosurgeon to come across such lesions in the sphenoid bone with orbital extension is even rarer.
Case presentation
We report a case of a 16-year female who presented with a three-month history of headache, proptosis, and deterioration of vision. Pre-operative imaging studies which included NCCT head and MRI brain, suggested the lesion to be an aneurysmal bone cyst of the greater wing of the sphenoid, with extension into the orbit. Intraoperative findings did corroborate with the preoperative imaging findings and were again confirmed later from the histopathology report.
Conclusion
Aneurysmal bone cysts of sphenoid bone with orbital extension, though rare, can be excised completely, without hampering the cosmesis. Being benign, patients can have a prolonged recurrence-free period if the lesion is completely excised.
Similar content being viewed by others
Background
Aneurysmal bone cysts, as a new clinicopathologic entity was first described by Jaffe and Lichtenstein in 1942 [1]. These lesions commonly affect the metaphysis of long bones. Involvement of skull bones is rare (3%) and sphenoid bone aneurysmal bone cysts with orbital extension are even rarer [2, 3]. These handful cases present mostly in their first three decades of life. We report a case of an aneurysmal bone cyst involving the greater wing of sphenoid bone with extension into the lateral orbital wall, which was totally excised without any cosmetic defect.
Case presentation
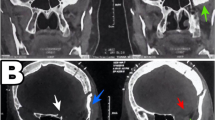
A 16-year girl presented with 3 months history of occasional headache and gradually progressive painless diminution in vision in the right eye. On examination, there was fullness in the right periorbital area with slight proptosis. It was nontender and the overlying skin was normal. Visual acuity was 6/12 in the right eye. There was no evidence of other neurologic deficits. NCCT showed a large heterogeneous lesion in the right anterior middle fossa and herniating anteriorly into the orbit through a defect in the posterior orbital wall. MRI showed a 4.3 × 3.2 × 3.4 cm expansile lytic lesion arising from the greater wing of the sphenoid wing with multiple locules within, showing blood fluid level and enhancement of wall and septa (Fig. 1). Anteriorly it caused the obliteration of the right orbital space resulting in mild proptosis. Medially it compromises the optic nerve canal with compression of the intra-canalicular segment of the optic nerve.
The axial (a) and coronal (b) views of preoperative NCCT head showing a heterogenous lesion, extending anteriorly into the orbit and causing proptosis. Preoperative axial CEMRI (c) and T2 sequence (d) showing an expansile lytic lesion arising from the greater wing of sphenoid wing with multiple locules within, showing blood fluid level and enhancement of wall and septa
We approached this lesion through right frontotemporal craniotomy. Tumour was well defined, encapsulated, involving the greater wing of the sphenoid with extension into the right orbit through the lateral wall. Posteriorly it extended up to the lateral wall of the sphenoid sinus. The lesion was solid cystic, with dark-coloured sanguineous spaces separated by fibrous septa. Gradually the whole lesion was curetted out with meticulous attention to hemostasis. Gross total excision was achieved and without leaving any residual cosmetic defect. In the postoperative period, there was the resolution of proptosis (Fig. 2). Her vision was intact at the time of discharge. Histopathology report did confirm the lesion to be an aneurysmal bone cyst (Fig. 3).
Discussion
Aneurysmal bone cysts of the skull constitute merely 3% of all the ABC cases. They mostly affect the cranial vault and present as palpable mass [4]. Involvement of cranial base is rarely seen and only a handful of spheno-orbital ABC have been reported to date [5]. ABCs arise either as a primary pathology or as a reactionary lesion secondary to various pathologies such as chondroblastoma, fibrous dysplasia, osteoblastoma, giant cell tumor, fibromyxoma, etc. [6].
Bone erosion thinned out cortex and heterogenous mass with multiple fluid levels are frequently seen on computed tomography. MRI demonstrates heterogeneous signal intensities on both T1 and T2 sequences, with multiple fluid levels suggesting hemorrhage with sedimentation. Hypointense peripheral rim with multiple internal septations that show contrast enhancement is a peculiar MRI finding [7, 8]. Though these imaging features are consistent, but not pathognomonic for ABC. Confirmatory diagnosis mandates evidence of histopathologic features like multiple septated fluid-filled spaces, without any endothelial lining. These septations are in fact lined by multinucleated giant cells, myofibroblasts, fibroblasts, and histiocytes [9].
There are various modalities of treatment and each is associated with a different degree of recurrence. En bloc excision and intralesional resection have good outcomes concerning the rate of recurrence. Though en bloc excision achieves the least risk of recurrence, it is associated with the highest degree of morbidity [10]. Intralesional resection with high-speed burr mechanically disrupts the lesion up to the circumscribing healthy bone, thus achieves a local control rate similar to that of en bloc excision. Curettage alone carries a recurrence rate of 20–50% [12]. Although curettage with adjuvant therapies like sclerotherapy, cryotherapy, radiotherapy have been used for peripheral ABC, they can’t be applied for spheno-orbital cases. Preoperative embolization can be used as a surgical strategy to decrease intraoperative blood loss by reducing the vascularity of lesions [13]. Although osteogenic sarcoma is a known complication in patients undergoing adjuvant radiotherapy for extracranial ABC, it has rarely been reported in cranial cases, thus radiotherapy has its role in recurrent cases [14]. In this case, we gained access to the lesion through the right frontotemporal corridor and achieved total excision through intralesional resection. At 15 months of follow-up, she had no recurrence.
Conclusions
Sphenoidal aneurysmal bone cysts constitute a rare clinicopathologic subgroup of ABC of the skull. Though benign, these lesions are locally aggressive and should be considered as a differential diagnosis in younger patients presenting with rapid onset painless proptosis. Intralesional resection with high-speed burr provides a viable option in achieving total resection, without leaving any cosmetic deformity and with a good degree of local disease control.
Availability of data and material
All the information and data that are available, have been shared in the article and are genuine.
Abbreviations
- ABC:
-
Aneurysmal bone cysts
- NCCT:
-
Non-contrast computed tomography
- MRI:
-
Magnetic resonance imaging
References
Jaffe HL. Solitary unicameral bone cyst. Arch Surg. 1942;44(6):1004. https://doi.org/10.1001/archsurg.1942.01210240043003.
Tamimi AF, Nimri C, Huseini M, et al. Aneurysmal bone cyst of the sphenoid bone as an intracranial and orbital space-occupying lesion. Pediatr Neurosurg. 2005;41(5):280–2. https://doi.org/10.1159/000087490.
Cansiz H, Inci E, Erisir F, et al. Aneurysmal bone cyst of the sphenoid bone. J Craniofac Surg. 2002;13(3):411–4. https://doi.org/10.1097/00001665-200205000-00010.
Calliauw L, Roels H, Caemaert J. Aneurysmal bone cysts in the cranial vault and base of skull. Surg Neurol. 1985;23(2):193–8. https://doi.org/10.1016/0090-3019(85)90345-3.
Sheikh BY. Cranial aneurysmal bone cyst “with special emphasis on endovascular management.” Acta Neurochir (Wien). 1999;141:601–10. https://doi.org/10.1007/s007010050349.
Bonakdarpour A, Levy WM, Aegerter E. Primary and secondary aneurysmal bone cyst: a radiological study of 75 cases. Radiology. 1978;126(1):75–83. https://doi.org/10.1148/126.1.75.
Lui YW, Dasari SB, Young RJ. Sphenoid masses in children: radiologic differential diagnosis with pathologic correlation. AJNR Am J Neuroradiol. 2011;32(4):617–26. https://doi.org/10.3174/ajnr.A2144.
Murphey MD, Andrews CL, Flemming DJ, et al. From the archives of the AFIP. Primary tumors of the spine: radiologic pathologic correlation. Radiographics. 1996;16(5):1131–58. https://doi.org/10.1148/radiographics.16.5.8888395.
Ruiter DJ, van Rijssel TG, van der Velde EA. Aneurysmal bone cysts: a clinicopathological study of 105 cases. Cancer. 1977;39(5):2231–9. https://doi.org/10.1002/1097-0142(197705)39:5%3c2231:aid-cncr2820390541%3e3.0.co;2-q.
Mankin HJ, Hornicek FJ, Ortiz-Cruz E, et al. Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol. 2005;23(27):6756–62. https://doi.org/10.1200/JCO.2005.15.255.
Gibbs CP Jr, Hefele MC, Peabody TD, et al. Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr. J Bone Joint Surg Am. 1999;81(12):1671–8. https://doi.org/10.2106/00004623-199912000-00003.
Purohit A, Chopra S, Sinha VD, Dharker SR. Aneurysmal bone cyst of the temporal bone: a case report. Neurol India [serial online] 2002 [cited 2021 Mar 30];50:511. https://www.neurologyindia.com/text.asp?2002/50/4/511/1324.
de Minteguiaga C, Portier F, Guichard JP, et al. Aneurysmal bone cyst in the sphenoid bone: treatment with minimally invasive surgery. Ann Otol Rhinol Laryngol. 2001;110(4):331–4. https://doi.org/10.1177/000348940111000407.
Kumar P, Singh S, Phadke RV, et al. Role of radiotherapy in a recurrent aneurysmal bone cyst of the temporal bone: case report. Neurosurgery. 2006;58(3):E584. https://doi.org/10.1227/01.NEU.0000197487.95078.6F (discussion E584).
Acknowledgements
Not applicable.
Funding
I have not received any funding for the case study.
Author information
Authors and Affiliations
Contributions
DJM has designed, acquired, interpreted the data and then drafted the work. PS did the literature search, designed the work and revised the manuscript. All the authors have read and approved the manuscript and have agreed to be accountable for their contributions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical committee clearance was taken before including this case for study.
Consent for publication
Valid informed written consent of the guardian was taken to publish this case report, as patient was just 16 years old. They were informed that the details of patient will not be disclosed.
Competing interests
There are no financial and non-financial competing interests associated with this case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahakul, D.J., Sharma, P. Greater wing of sphenoid, the home for aneurysmal bone cysts: a case report. Egypt J Neurosurg 36, 28 (2021). https://doi.org/10.1186/s41984-021-00128-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-021-00128-8