Abstract
Introduction
Spheno-orbital meningiomas are characterized by bone invasion with extensive hyperostosis and possible encroachment into the orbit, infra-temporal fossa, and/or the cavernous sinus that render total surgical excision challenging. The surgical technique utilized is a key factor facilitating complete resection and hence improvement of proptosis and accompanying visual symptoms.
Methods
This is a retrospective study of twenty-two patients (including 4 recurrent cases) with meningioma en-plaque, presenting with hyperostosis and proptosis. We describe the surgical approaches used, technique, and extent of resection in addition to postoperative outcome.
Results
In twenty patients, the pterional approach was used, while two patients were operated on via the mini orbito-zygomatic approach. Total resection of the tumor was achieved in 10 cases (45.5%), subtotal in 6 (27.3%), partial in 5 (22.7%), and in 1 case, injury to the internal carotid artery lead to premature termination of surgery. Seventeen patients (77.3%) had improvement of proptosis, 2 (9.1%) had partial improvement, and 2 (9.1%) had no improvement at 3 months of follow-up. Post-operative morbidities include cerebrospinal fluid leak, infection, and hydrocephalus, each occurred in one (4.5%) different case.
Conclusions
Proper drilling of the lateral and superior orbital walls with excision of any intra-orbital soft tissue components is all key points for better surgical resection and clinical regression of proptosis. However, factors such as extension of the hyperostosis to the infra-temporal fossa or medial orbital wall, tumor invasion of the cavernous sinus, or adherence of tumor to the orbital muscles, prevent total excision.
Similar content being viewed by others
Introduction
Spheno-orbital meningiomas (SOM) represent a subgroup of sphenoid ridge meningiomas that are also known as the en-plaque meningiomas account for 20% of intracranial meningiomas [1]. This location is considered to be the third most common location for meningiomas [2, 3]. En-plaque meningiomas with extension into the orbit represent only 2‑9% of meningiomas [4,5,6]. Spheno-orbital meningiomas are diagnosed by their pattern of growth, based on radiographic appearance and not on the basis of their histological morphology [7]. They have a tendency to stimulate bone hyperostosis in neighboring skull bones more than most meningiomas and the extent of hyperostosis is usually not proportionate to the size of the meningioma or the soft tissue component, which usually tends to be small [7, 8]. Due to their special pattern of growth and interosseous extension, SOMs are notoriously known for exhibiting a high rate of recurrence, ranging from 35 to 50% [3, 9]. It is important not to confuse this subtype of meningioma with primary meningiomas arising from the optic nerve sheath, from which they in turn can extend to the sphenoid wing [10].
There is a female preponderance in SOMs as with most meningiomas [6]. The main presenting symptoms are proptosis, visual impairment, and not uncommonly retro-orbital pain. Patients with recurrence of SOMs usually present with optic nerve involvement [3].
Different surgical approaches have been described to resect SOMs [11,12,13,14]. Improvement of proptosis and decompression of the optic nerve should be considered the main goals of surgeries [15, 16].
Extension of SOMs into the cavernous sinus and involvement of the ocular musculature render gross total resection nearly impossible due to the risk of loss of visual function. Some authors prefer subtotal resection with postoperative radiation therapy [17, 18]. There is, however, no general agreement on the usefulness of using radiation therapy for skull base lesions especially with interosseous extension as with spheno-orbital meningiomas [19,20,21].
The surgical technique to ameliorate the visual and cosmetic manifestations is the key, and this is our focus on this study.
Methods
We retrospectively studied and evaluated twenty-two patients with spheno-orbital meningiomas presenting with proptosis who underwent surgical resection. Our single exclusion criterion was absence of proptosis. All the cases studied had hyperostosis and proptosis, with or without soft tumor extension into the orbit. Patient demographics, preoperative clinical condition, radiographic evaluation, surgical technique, extent of surgical resection, and clinical outcome were collated and evaluated. Preoperative imaging in the form of magnetic resonance imaging (MRI) was performed in all cases and 21 of the 22 patients had a preoperative computerized tomography (CT) scan to evaluate the degree of bony involvement, extent of hyperostosis, involvement of orbital walls, and the infra-temporal region. Four out of the 22 cases were recurrent cases (18.2%).
Regarding the surgical technique, we used the classical pterional approach in twenty cases with drilling of the sphenoid ridge. The remaining 2 cases were approached via the mini orbito-zygomatic (OZ) approach. The last is a modification of the pterional approach that allows increasing in the vertical angle and decreasing the depth of the surgical corridor, hence, the amount of brain retraction required. In our case-series, the approach was done using a 2-piece modified orbito-zygomatic craniotomy. Firstly, a pterional craniotomy was performed, followed by drilling of part of the orbital roof and removing the orbital rim using a Gigli saw in a beveled manner to allow easy replacement.
Drilling of the orbital roof and lateral orbital wall was performed in all the cases, including deroofing of the superior orbital fissure. A high-speed drill was used to drill all hyperostotic bone. Extradural drilling of the anterior clinoid process was done in case it is involved by the tumor. Deroofing of the optic canal was done in cases with confirmed optic nerve compression at the canal, to avoid unnecessary extra work that could lead to thermal or mechanical injury to the optic nerve. In cases where there is intraconal tumor, the periorbita is opened for removing any soft tissue tumor component. The invasion into the cavernous sinus was not addressed intraoperatively and we decided to follow the patients up with imaging. The extension of hyperostosis into the infratemporal region presented a limiting factor to drill all the hyperostotic bone.
After finishing the bony work, the dura was opened, and the medial limit of the mass, including the optic nerve and carotid artery, is explored before the soft tissue component of the tumor was resected. Tumor resection was evaluated using the Simpson Grading System [22].
After meticulous tumor resection, a main concern during closure was correct hermetic dural closure. The anterior dura was resected and replaced by either pericranial graft (and/or temporalis fascia), fascia lata, or artificial graft. Resection of the dura stops lateral to the cavernous sinus. Naturally achieving water-tight dural closure was very important to prevent postoperative cerebrospinal fluid (CSF) leak with its associated complications. It is our protocol during surgery not to use fixed retraction; intermittent dynamic retraction was used when needed.
Following tumor resection and dural repair, the superior orbital rim that was initially removed in mini OZ, is fixed in place by drilling small holes in the beveled rim and suturing them.
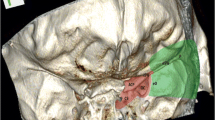
Reconstruction of the drilled orbital roof and lateral wall was not performed, as the orbital rim was preserved in all cases (Figs. 1, 2, and 3).
Right side SOM. Axial CT scan before and after surgery. A 58-year-old female patient operated via the pterional approach. The tumor was extending through the bone and under the temporalis muscle. The invaded pathological bone flap was removed. The tumor was found to invade the dura and the temporal lobe. Anterior clinoidectomy was performed, with drilling of the optic canal. Gross total resection was achieved (Simpson grade I). The dura was resected and reconstructed using a temporalis fascia graft. Regression of the existing proptosis was noted in the immediate postoperative period
Intraoperative picture of the same patient in Fig. 2
Results
The mean age of our patient group was 43.9 years, ranging from 30 to 58. There were 18 (81.8%) de-novo cases and 4 (18.2%) recurrent cases. The main presenting symptom in all cases was proptosis in addition to other manifestations including visual diminution in 11 cases, headache in 6 patients, and temporal fossa swelling in 5 cases. Two patients presented with limited ocular motility and 1 patient presented with seizures (Fig. 4).
With regards to orbital pathology and involvement, all patients had hyperostosis on radiographic evaluation, of which only 12 cases (54.6%) had tumor soft tissue extension into the orbit. Cavernous sinus involvement was present in 3 cases (13.6%) (Fig. 5).
N together with evident radiologic compromise of the optic canal. Removal of the anterior clinoid process (ACP) was done in case of its involvement by the tumor (Fig. 6).
The extent of resection was evaluated using the Simpson Grading System. Total resection (Simpson grades I and II) was achieved in 10 cases (45.5%), near-total resection (Simpson grade III) in 6 cases (27.3%), and partial resection (Simpson grades IV) in 5 cases (22.7%). In one case, the operation was prematurely terminated after injury to the internal carotid artery (ICA) occurred (Fig. 7).
In 17 cases (77.27%), there was complete resolution of proptosis, 2 cases (9.1%) had partial improvement and 2 (9.1%) had no improvement postoperatively after 3 months follow-up. None of the cases developed enophthalmos in the follow-up period (Fig. 8).
Two of our patients developed a postoperative cerebrospinal fluid (CSF) leak, one of which was managed conservatively while the other patient developed late postoperative hydrocephalus that required a ventriculo-peritoneal shunt. Three patients had transient ophthalmic (V1) hyposthesia that recovered within 3 months. One patient had temporary ophthalmoplegia that resolved over 2 months. Although the cavernous sinus was not opened, the affection of the trigeminal and oculomotor nerves could be due to thermal and mechanical effect of drilling of the superior orbital fissure. Two patients died in this series, one from intraoperative carotid injury and the other from late deep venous thrombosis. The carotid injury occurred while removing the hyperostotic bone; a rocking movement resulted in tear in its wall. The injured wall was clipped after opening the dura, but the patient developed infarction and died later in the intensive care unit (ICU) (Fig. 9).
Discussion
Despite the fact that spheno-orbital meningiomas (SOM) with hyperostosis represent only 2‑9% of meningiomas, they still form a challenge to the neurosurgeon to achieve total resection [4,5,6]. Although the soft tissue component of the tumor is usually small, the hyperostotic bone with extension into the orbit, potential cavernous sinus invasion, and extension into infra-temporal region all pose a challenge to total resection [7, 8].
The challenge mainly lies in the fact that the aim of surgery is not only the total resection of the intracranial tumor soft tissue but also the resection of hyperostotic bone that has meningioma cells in its Haversian canals, which are an important site for recurrence. Another important aim is to improve the proptosis and/or visual symptoms that the patients present with. In some cases, resection of the meningioma is not sufficient to achieve this, as the hyperostotic bone is often the cause of the visual involvement. Typically, this occurs in cases with hyperostosis of the anterior clinoid and narrowing of the optic foramen and/or optic canal. In those cases, with hyperostosis of the lateral orbital wall with or without tumor soft tissue extension into the orbit, proptosis is the main clinical manifestation [7, 8].
There are several surgical approaches described for resection of SOM [11,12,13,14]. After using the mini OZ approach (modified OZ) in two cases, we did not see any added benefit from the osteotomy in the orbital rim. Although it does increase the vertical angle, in cases with spheno-orbital meningioma, this is not deemed necessary as the soft tissue component was superficial and small and the excision of the intraorbital part can be achieved without an osteotomy of the orbital rim. Also, drilling of the orbital roof and lateral orbital wall just behind the orbital rim achieves adequate decompression of the periorbita and gives access to the intraorbital soft tissue located lateral and superior to the globe and could be done without removing the orbital rim.
In all patients with visual symptoms and in selected cases where the tumor was extensive and where near-total resection was achieved; optic nerve decompression was done. This was achieved through drilling the roof and lateral walls of the optic canal.
The extent of resection of spheno-orbital meningiomas is variable. In the series of Mirone and Schick and colleagues, the gross total resection was as high as 60‑82%. In other series such as those described by Jaaskelainen and colleagues; gross total resection was achieved in only 50% of cases with hyperostosis, and in 15% of patients with extension into the orbit [5, 23, 24].
In some series, the goal of surgery was the relief of symptoms rather than the gross total resection of the tumor. This was true with Ringel and colleagues, where total resection was achieved in 24% of their patients, with 60% of the sub-totally resected tumors remaining stationary [25].
In our series, described above, we were able to achieve total resection in 47.4% of cases, subtotal resection in 21.1% of cases, and partial resection in 26.3% of cases. The main factor limiting gross total resection was the soft tissue extension into the cavernous sinus, adherence of tumor tissue to the orbital musculature, and infratemporal extension of the hyperostotic bone into the pterygoid plates.
There is still no consensus within the neurosurgical community regarding the reconstruction of the drilled superior and lateral orbital walls after surgical resection of the tumor. Some authors believe it is necessary to perform reconstruction to decrease the occurrence of pulsatile exophthalmos. On the other hand, there is a belief that as long as the orbital floor and orbital margins are not drilled off, there is no need for such reconstruction [23, 26]. As far as our series go, we opted not to perform any reconstruction to the orbital roof or lateral wall. Our bone reconstruction was limited to the fronto-temporal region. Bone reconstruction of the drilled off hyperostotic diseased bone was done in 8 cases (36.36%). None of our patients developed postoperative enophthalmos.
Postoperative complications following resection of SOMs are numerous, including worsening of vision, hemiplegia, ophthalmoplegia, facial numbness, hematomas, and injury to the trigeminal [27, 28]. Two of our patients developed a postoperative CSF leak, one of which was managed conservatively while the other patient developed late postoperative hydrocephalus that required management with a ventriculo-peritoneal shunt. Three patients in our series suffered an injury to the trigeminal nerve manifesting as hypoesthesia of V1 distribution. All of the cases were, however, temporary and had fully recovered by 3 months postoperatively. One patient had temporary ophthalmoplegia that recovered over 2 months.
The reported mortality after resection of SOMs was around 6% with Jaaskelainen and colleagues [24]. The main cause of mortality reported in the literature results from a vascular insult. We had 2 mortalities (9%), with one patient suffering an ICA injury intraoperatively leading to their death 2 weeks postoperatively, the other patient died of a pulmonary embolism in the postoperative period.
The role of irradiation for skull base lesions, especially those with associated hyperostosis, is debatable [19,20,21]. At our center, patients are only referred for radiosurgery treatment when there is tumor left in the cavernous sinus. In general patients with WHO grades II or III meningiomas are also possible candidates for radiosurgery. In all cases where total resection was achieved, including the hyperostotic bone, follow up was done every 3 months for 1 year then yearly afterward. In those patients with residual hyperostotic bone, we chose to follow them up rather than offering them adjuvant radiotherapy.
Conclusions
Adequate and meticulous drilling of the lateral and/or superior orbital walls, excision of any intra-orbital soft tissue components, and removal of all accessible hyperostotic bone are all key points contributing to total resection and regression of proptosis. Factors that render total resection difficult are extension of the hyperostosis into the infra-temporal fossa, medial, or inferior orbital walls. In addition, tumor extension into the cavernous sinus or adherence of tumor to the orbital muscles is recognized challenges to achieve total resection. The main aim of surgery in tumors, where total resection is not possible, remains optic nerve decompression and the hyperostotic orbital walls to treat the proptosis.
Availability of data and materials
Data used and analyzed in this study are available from the authors on reasonable request.
Abbreviations
- ACP:
-
Anterior clinoid process
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computerized tomography
- ICA:
-
Internal carotid artery
- MRI:
-
Magnetic resonance imaging
- OZ:
-
Orbito-zygomatic
- PMMA:
-
Polymethyl metacrylate
- SOM:
-
Spheno-orbital meningioma
References
Al-Mefty O, Abdulrauf SI, Haddad GF. Meningiomas. In: Winn HR, editor. Youmans & Winn Neurological Surgery. 6th ed. Philadelphia: Saunders; 2011. p. 1426–49.
Honig S, Trantakis C, Frerich B, Sterker I, Kortmann RD, Meixensberger J. Meningiomas involving the sphenoid wing outcome after microsurgical treatment - a clinical review of 73 cases. Cent Eur Neurosurg. 2010;71:189–98.
Maroon JC, Kennerdell JS, Vidovich DV, Abla A, Sternau L. Recurrent spheno-orbital meningioma. J Neurosurg. 1994;80:202–8.
Jesus O, Toledo MM. Surgical management of meningioma en plaque of the sphenoid ridge. Surg Neurol. 2001;55:265–9.
Mirone G, Chibbaro S, Schiabello L, Tola S, George B. En Plaque sphenoid wing meningiomas: recurrence factors and surgical strategy in a series of 71 patients. Neurosurgery. 2009;65(Suppl 6):100–8.
Shrivastava RK, Sen C, Costantino PD, Della Rocca R. Sphenoorbital meningiomas: surgical limitations and lessons learned in their long-term management. J Neurosurg. 2005;103:491–6.
Honeybul S, Neil-Dwyer G, Lang DA, Evans BT, Ellison DW. Sphenoid wing meningioma en plaque: a clinical review. Acta Neurochir (Wien). 2001;143:749–58.
Pieper DR, Al-Mefty O, Hananda Y, Buecher D. Hyperostosis associated with meningioma of the cranial base: secondary changes or tumor invasion. Neurosurgery. 1999;44:742–7.
Adegbite AB, Khan MI, Paine KW. The recurrence of intra- cranial meningiomas after surgical treatment. J Neurosurg. 1983;58(1):51–6.
Boulos P, Dumont AS, Mandell JW, Jane JA. Meningiomas of the orbit: contemporary considerations. Neurosurg Focus. 2001;10(5). https://doi.org/10.3171/foc.2001.10.5.6.
Carrizo A, Basso A. Current surgical treatment for sphenoorbital meningiomas. Surg Neurol. 1998;50(6):574–8.
Day JD. Cranial base surgical techniques for large spheno-cavernous meningiomas: technical note. Neurosurgery. 2000;46(3):754–9.
Schepers S, Ioannides C, Fossion E. Surgical treatment of exophthalmos and exorbitism: a modified technique. J Craniomaxillofac Surg. 1992;20(7):313–6.
Seifert V, Dietz H. Combined orbito-frontal, sub- and infratemporal fossa approach to skull base neoplasms. Surgical technique and clinical application. Acta Neurochir (Wien). 1992;114(3–4):139–44.
Talacchi A, DeCarlo A, D’Agostino A, Nocini P. Surgical management of ocular symptoms in spheno-orbital meningiomas. Is Orbital reconstruction really necessary? Neurosurg Rev. 2014;37:301–10.
Scarone P, Leclerq D, Héran F, Robert G. Long-term results with exophthalmos in a surgical series of 30 sphenoorbital meningiomas. J Neurosurg. 2009;111:1069–77.
Pompili A, Derome PJ, Visot A, Guiot G. Hyperostosing meningiomas of the sphenoid ridge: clinical features, surgical therapy, and long-term observations: review of 49 cases. Surg Neurol. 1982;17:411–6.
Barbaro NM, Gutin PH, Wilson CB, Sheline GE, Boldrey EB, Wara WM. Radiation therapy in the treatment of partially resected meningiomas. Neurosurgery. 1987;20:525–8.
Iwai Y, Yamanaka K, Ikeda H. Gamma knife radiosurgery for skull base meningioma: long- term results of low-dose treatment. J Neurosurg. 2008;109:804–10.
Gorman L, Ruben J, Myers R, Dally M. Role of hypofractionated stereotactic radiotherapy in treatment of skull base meningiomas. J Clin Neurosci. 2008;15:856–62.
Wenkel E, Thornton AF, Finkelstein D, Adams J, Lyons S, De La Monte S, et al. Benign meningioma: partially resected, biopsied, and recurrent intracranial tumors treated with combined proton and photon radiotherapy. Int J Radiat Oncol Biol Phys. 2000;48:1363–70.
Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957;20:22–39.
Schick U, Bleyen J, Bani A, Hassler W. Management of meningiomas en plaque of the sphenoid wing. J Neurosurg. 2006;104:208–14.
Jaaskelainen J, Ohman J, Kotilainen P, Munyao N, Randell T, Hernesniemi J. Sphenoidal wing meningioma- outer and middle. In: Kaye AH, PMcl B, editors. Operative Neurosurgery. London: Churchill Livingstone; 2000. p. 587–604.
Ringel F, Cedzich C, Schramm J. Microsurgical technique and result of a series of 63 spheno-orbital meningiomas. Neurosurgery. 2007;60(Suppl 2):214–22.
Leake D, Gunnlaugsson C, Urban J, Marentette L. Reconstruction after resection of sphenoid wing meningiomas. Arch Facial Plast Surg. 2005;7(2):99–103.
Pamir MN, Belirgen M, Ozduman K, Kiliç T, Ozek M. Anterior clinoidal meningiomas: analysis of 43 consecutive surgically treated cases. Acta Neurochir (Wien). 2008;150(7):625–36.
Chaichana KL, Jackson C, Patel A, Miller NR, Subramanian P, Lim M, et al. Predictors of visual outcome following surgical resection of medial sphenoid wing meningiomas. J Neurol Surg B. 2012;73:321–32.
Acknowledgements
Not applicable
Funding
This study is funded by the authors in all aspects (data collection, statistical analysis, and writing the manuscript).
Author information
Authors and Affiliations
Contributions
M. E. collected and analyzed the data and wrote the manuscript. W. N. shared in data collection, analysis, reviewed and prepared the manuscript for publication and is the corresponding author. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work has been accepted by the ethics committee in the Department of Neurosurgery, Faculty of Medicine, Beni-Suef University. Reference number is not applicable. It has been approved on November 2016.
Consent to participate has been approved also by the same committee.
Consent for publication
Informed consent was obtained from patients involved in this study that they will be involved in research.
Competing interests
The authors have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elborady, M.A., Nazim, W.M. Spheno-orbital meningiomas: surgical techniques and results. Egypt J Neurol Psychiatry Neurosurg 57, 18 (2021). https://doi.org/10.1186/s41983-021-00276-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-021-00276-6