Abstract
This paper explores the potential of stem cell therapies in revolutionising stroke recovery, addressing the limitations of current treatments and emphasising regenerative medicine as a promising alternative. Stroke, a leading cause of disability and death worldwide, necessitates innovative approaches due to the temporal constraints and regenerative deficiencies in existing therapeutic modalities. The review explores the diverse mechanisms underlying stem cell-mediated recovery, encompassing neuroprotection, neurogenesis, angiogenesis, modulation of inflammatory responses, and induction of host brain plasticity. We searched prominent databases (PubMed, Scopus, Google Scholar, and Web of Science) from inception to January 2024 for studies on “stem cell therapy” or “regenerative medicine” combined with “stroke recovery” or “cerebrovascular accident”. Studies in humans and animals, published in peer-reviewed journals, and investigating the impact of stem cell therapy on stroke recovery were included. We excluded non-English publications and those lacking sufficient outcome data. Evidence from animal studies demonstrates the efficacy of various stem cell types, while human studies, though limited, contribute valuable insights into safety and potential efficacy. Safety considerations, crucial for successful clinical application, emphasise the need for rigorous preclinical and clinical studies, long-term follow-up data, and ethical standards. Challenges in the field, such as study design heterogeneity, optimising stem cell delivery methods, and identifying subpopulations likely to benefit, require concerted efforts to overcome. Standardising methodologies, refining delivery routes, and personalising interventions based on biomarkers are essential. This review positions stem cell therapies as promising for comprehensive neural tissue recovery following stroke.
Similar content being viewed by others
Introduction
Stroke remains a leading cause of death and disability worldwide, characterized by a sudden interruption of blood flow to the brain [1]. This disruption, often caused by blood clot formation (ischemic stroke) or ruptured blood vessels (hemorrhagic stroke), can lead to permanent brain damage and a decline in physical and cognitive function [1]. According to the World Health Organization (WHO), stroke is the second leading cause of death globally, with an estimated 17.9 million strokes occurring worldwide in 2019 [2]. Furthermore, stroke is a major contributor to disability, with an estimated 5.5 million people dying from stroke each year [2]. The incidence of stroke varies geographically, but it is a significant health burden for all age groups, impacting not just the elderly but also a growing number of younger adults [3].
There are two main stroke categories: ischemic and hemorrhagic [4]. Hemorrhagic strokes, constituting 10–15% of cases, involve bleeding or leaky blood vessels, leading to vessel rupture, toxic effects, and tissue infarction [1]. Ischemic strokes, comprising 87%, result from insufficient blood and oxygen supply, typically due to artery blockage. The clinical impact depends on the stroke's location, type, and severity [1].
Stroke stands as the third most common cause of disability and the second most common cause of death worldwide [3]. It remains a leading cause of disability worldwide, necessitating innovative approaches for effective rehabilitation. Existing stroke therapies vary according to the nature of the stroke [5]. Early thrombolysis with recombinant tissue plasminogen activator (tPA) remains a cornerstone treatment for acute ischemic stroke. Current guidelines recommend tPA administration within 4.5 h of symptom onset, with an extended window up to 6 h being considered in select patients based on advanced imaging techniques [6]. Rehabilitation, antiplatelet therapy, neural repair, and antihypertensive therapy are also employed [7]. In contrast, hemorrhagic stroke therapies involve a reversal of bleeding diatheses, hemostatic therapy, and surgical or endovascular intervention [8,9,10,11]. However, these treatments face limitations, foremost among them being the narrow time window within which they must be administered to yield optimal efficacy, particularly evident in thrombolytic interventions like tPA [12]. The critical importance of prompt intervention is shown by the urgency to dissolve clots and restore blood flow in ischemic strokes [13]. This temporal constraint poses a considerable challenge, as delays in treatment initiation often result in diminished therapeutic effectiveness [14, 15].
Moreover, the existing therapeutic modalities, while proficient in mitigating immediate damage and managing symptoms, notably lack regenerative benefits for the neural tissue affected by stroke [16]. Current interventions predominantly focus on alleviating acute symptoms and preventing further deterioration, leaving a notable gap in restoring damaged neuronal structures and long-term functional recovery [17]. This absence of regenerative potential hinders the realisation of comprehensive rehabilitation in stroke patients, limiting the scope for achieving optimal neurological restoration [18].
These inherent limitations necessitate a shift and a departure from conventional therapeutic approaches. The quest for novel interventions becomes important, as well as seeking strategies that address the immediate consequences of stroke and venture into regenerative medicine. This shift forms the foundation for exploring alternative methodologies, particularly stem cell therapies that promise to mitigate acute damage and foster neuroregeneration and functional recovery [19]. In light of these challenges, exploring stem cell therapies is a promising avenue, offering the potential to transcend current stroke treatments' temporal and regenerative limitations. With their unique ability to differentiate into various cell types and promote tissue repair, stem cells present a novel, innovative approach with significant promise in reshaping stroke recovery [20]. This study aims to critically examine existing evidence, identify gaps, and contribute valuable insights to the ongoing discourse on the applicability of stem cell therapies in stroke rehabilitation.
Methodology
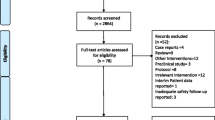
Our study adopts a narrative review design, aiming to evaluate the efficacy of various stem cell therapies in stroke recovery. Table 1. To identify relevant literature, we extensively searched prominent databases, including PubMed, Scopus, Google Scholar and Web of Science, from the inception of available records to January 2024. Our search strategy involved use of keywords ("stem cell therapy" OR "regenerative medicine") AND ("stroke recovery" OR "cerebrovascular accident"), ("neural stem cells" OR "mesenchymal stem cells") AND ("ischemic stroke" OR "hemorrhagic stroke"), and ("embryonic stem cells" OR "induced pluripotent stem cells") AND ("neuroregeneration" OR "brain repair"). Inclusion criteria for our study included studies involving human and animal subjects, published in peer-reviewed journals, and investigating the impact of stem cell therapies on stroke recovery outcomes. Exclusion criteria included non-English publications and those lacking sufficient data on relevant outcomes. Two independent reviewers extracted data from selected studies using a predefined form. The variables of interest included study design, participant demographics, types of stem cells administered, intervention protocols, and primary stroke recovery outcomes.
Stem cell therapies in stroke
Various stem cells from different origins have been identified and investigated for their potential and efficacy in stroke therapy [21]. Table 2. Studies on several types of stem cells, including embryonic stem cells (ESCs), mesenchymal stem cells (MSCs), and induced pluripotent stem cells (iPSCs), have explored their potential for tissue regeneration, maintenance, migration, proliferation, rewiring of neural circuitry, and physical and behavioural rejuvenation [22, 23]. Efforts to utilise stem cells for stroke treatment broadly include ESCs, neural stem cells (NSCs), and mesenchymal stem cells (MSCs) [21]. Other stem cell types being investigated for stroke therapy include bone-marrow stem cells (BMSCs) [21], induced Pluripotent Stem Cells (iPSCs), hematopoietic stem cells (HSCs), human umbilical cord blood cells (HUCBCs), endothelial progenitor cells (EPCs) [24], mononuclear cells (MNCs), and olfactory ensheathing or olfactory glia cells (OEC) [25].
Embryonic stem cells (ESCs)
Unlike other sources of stem cells, human embryonic stem cell (hESCs) lines possess the unique self-renewal ability and the potential to differentiate into any cell type [26]. Derived from the inner mass of blastocysts, hESCs are pluripotent cells capable of differentiating into all body cell types except those of the placenta [19]. Consequently, they represent an ideal cell source for developing cell transplantation strategies in stroke. The regenerative potential of hESCs in stroke is attributed to their ability to generate various neuronal and glial elements that comprise brain tissues, including neurons, astrocytes, and oligodendrocytes [19, 26]. hESCs have been extensively investigated in recent years for generating various types of neurons [27]. ESC-derived mesenchymal stem cells, vascular progenitor cells, and neural progenitor cells have shown beneficial effects without evidence of tumorigenesis [28]. Neuronal progenitor cells derived from ESCs can reduce infarct volume, promote neurogenesis, and enhance functional recovery [29]. Transplanted embryonic neural stem cells have been shown to stimulate the release of angiogenic cytokines, leading to vascular endothelial proliferation within 15 day post-cerebral ischemia [29].
Neural stem/precursor cells (NSCs)
NSCs are multipotent cells primarily located in the subgranular zone of the dentate gyrus of the hippocampus and the subventricular zone of the brain's third ventricle [30]. NSCs can be derived from embryonic, fetal, or adult brain tissue and can differentiate into all cell types necessary for promoting neurological function [31]. These NSCs migrate from the subventricular zone into the rostral migratory stream and subsequently to the olfactory bulb, differentiating into interneurons [32]. NSCs play a significant role in maintaining brain homeostasis and have demonstrated therapeutic potential following neurovascular damage [33]. Transplantation of NSCs has shown efficacy in treating ischemic stroke through various mechanisms, including maintenance of the blood–brain barrier, reduction of neuroinflammation, promotion of neurogenesis and angiogenesis, and ultimately facilitating neurological recovery [34]. Currently, NSCs are a focal point of research for neurobiologists due to their ability to differentiate into various neuronal and glial elements that comprise the central nervous system (CNS), making them promising candidates for restoring neuronal and behavioural deficits associated with various CNS disorders, including stroke [35]. Studies investigating the regenerative potential of rodent or human, embryonic or fetal-derived neural stem/progenitor cells have reported appropriate differentiation of grafted NSCs into neurons and astroglia, as well as functional recovery in stroke models following intracerebral, intracerebroventricular, and intravascular administration [36, 37].
Mesenchymal stem cells
MSCs can traverse the blood–brain barrier and selectively migrate to injured sites, where they mitigate apoptosis, elevate basic fibroblast growth factor levels, and stimulate endogenous cellular proliferation [38]. Studies into the therapeutic application of MSCs for stroke have been prompted by their multilineage differentiation potential, including the ability to generate neuronal-like cells and their immunomodulatory and trophic effects [39, 40]. In vivo studies have shown that MSCs injected peripherally preferentially migrate to damaged areas, correlating with improved recovery in ischemic injury models [41, 42]. In murine stroke models, MSCs treatments have been associated with increased axonal density around ischemic lesions, contributing to axonal remodeling and improved functional recovery [43]. These therapeutic effects are attributed to the secretion of factors that reduce levels of axonal growth inhibitors and promote growth and neurogenesis [41]. MSCs also stimulate stroke recovery by secreting neurotrophic factors such as brain-derived neurotrophic factor (BDNF) and angiogenic mediators [43]. Systemic or peripheral administration of MSCs has been deemed a safe and effective method for stem cell transplantation [43].
Bone-marrow stem cells (BMSCs)
BMSCs express a wide range of angiogenic and arteriogenic cytokines, including placental growth factor (PIGF), basic fibroblast growth factor 2 (bFGF/FGF2), vascular endothelial growth factor (VEGF), insulin-like growth factors (IGFs), and angiopoietin 1 (Ang-1), which play crucial roles in brain plasticity and the restoration of neurological function following stroke [44]. Like NSCs, BMSCs have been investigated for their potential use in stroke therapies due to their ability to differentiate into neural and glial cells in vitro [45]. Subsequent in vivo studies demonstrated that BMSCs, when transplanted intracerebrally into rat stroke models, could migrate to the site of ischemic brain injury and differentiate into neural cells, leading to improved recovery [46]. Further investigations into the migratory capabilities of BMSCs revealed that intra-arterial (IA) and intravenous (IV) administration of BMSCs could result in migration to the brain [47. In rat stroke models, both IA and IV administration of BMSCs led to greater functional recovery, attributed to the accumulation of BMSCs at the site of ischemia [47].
Induced pluripotent stem cells
hiPSCs hold potential for therapeutic applications after ischemic stroke due to their neuroprotective and neuroregenerative properties [48]. Compared to embryonic stem cells (ESCs), iPSCs offer the advantage of avoiding immune rejection and sidestepping the ethical concerns associated with the use of embryonic tissues [49]. Engraftment of iPSCs in a cerebral ischemia model has been shown to reduce infarct volume, improve neurological outcomes, and enhance short-term sensorimotor recovery [50]. iPSCs promise immune reaction-free and personalised stem cell therapy [50].
Hematopoietic stem cells (HSCs)
Administration of HSCs has been shown to reduce ischemic infarct volume in the cerebral cortex of the middle cerebral artery occlusion (MCAO) stroke model [51]. When applied in conjunction with stem cell factor (SCF) and granulocyte-colony stimulating factor (G-CSF) in the hypoxia–ischemia model, HSCs have mitigated atrophy in the ipsilesional cerebral hemisphere [52]. These findings suggest that HSCs hold promise as a valuable source of stem cells and are potential candidates for ameliorating ischemic stroke-induced degeneration. They demonstrate a robust capacity for angiogenesis, as evidenced in diseases like myocardial infarction and limb ischemia, and exhibit the potential for reorganising the vascular network in the brain [51]. However, these cells have a limited capacity for neuronal differentiation and are thus unable to complete the complex restoration process required to repair ischemic stroke-related damage [52].
Human umbilical cord stem cells (HUCBCs)
HUCBCs primarily differentiate into neurons, with a smaller subset capable of differentiating into astrocytes [53]. Treatment with HUCBCs after cerebral ischemia has been shown to reduce neuroinflammation by enhancing the production of interleukin-10 (IL-10) and reducing interferon-gamma (IFN-γ), thereby suppressing T-cell proliferation [54]. Primary intravenous treatment with HUCBCs 24 h after MCAO improved functional recovery and cell migration, suggesting that this timing can be optimal for clinical stroke treatment [55]. Despite the potential of cord blood as a source for cell-based therapies, its application and safety require further confirmation [55].
Endothelial progenitor cells (EPCs)
EPCs are typically generated and maintained in the bone marrow, where they can be mobilised and transferred to injury sites to contribute to blood vessel remodelling and repair [56]. Recent studies have demonstrated that transplantation of EPCs promotes focal angiogenesis and neurogenesis, improves cerebral blood flow, reduces neuronal cell death, decreases infarct volume, and enhances neurobehavioral recovery following ischemia [57, 58]. These characteristics of EPCs suggest their therapeutic potential for treating cerebral ischemia, as they contribute to blood vessel formation and release paracrine trophic factors.
Mononuclear cells (MNCs) and olfactory ensheathing/glial cells (OECs)
One advantage of using mononuclear cells (MNCs) is that they can be obtained from patients without ex-vivo expansion [25]. Olfactory ensheathing cells (OECs) surround olfactory neurons and serve as scavengers of pathogens and debris at the interface between the CNS and the nasal mucosa [59]. In addition, they express neurotrophic factors that support olfactory regeneration [60]. While OECs have been extensively studied in the context of spinal cord injury, research into their potential utility for treating ischemic stroke is still in its early stages [60].
Mechanisms underlying stem cell-mediated recovery in stroke
Neuroprotective effects and enhancement of neurogenesis
Stem cells’ secretory activities in the subacute and chronic phases of stroke promote neuroprotection and neuroregeneration [47, 61, 62]. Transplantation with cellular materials triggers the regeneration of disrupted axons by releasing neurotrophins or inhibiting axon growth cone inhibitors [63]. In addition, spared axons could proliferate to generate newer ones. MSCs, for instance, secrete many neurotrophic factors like BDNF and glial cell line-derived neurotrophic factor (GDNF), which act like a lifeline for neurons, promoting their survival and growth [63]. In addition, SCTs activate the phosphatidylinositol 3-kinase (PI3K)-Akt signalling pathway in neural progenitor cells [64, 65], inducing cell survival, proliferation, migration, and neural cell migration [66, 67]. Different therapies could produce different effects. Bone-marrow mesenchymal cells (BSCs) stimulate the secretion of basic fibroblast growth factor and BDNF from brain parenchymal cells, further activating Akt [68,69,70]. SCTs interact directly with injured neurons, providing support through cell-to-cell communication [69]. They support neuro-recovery by encouraging reinnervation and moderating neuroinflammation. SCT-induced neurogenesis has been shown to facilitate functional recovery with resultant improvements in neurological functions during and after a year of stroke recovery [71]. The acute delivery of stem cells reduces the size of brain lesions, inhibiting cell death in the penumbra [43, 44].
Angiogenesis and vascular repair
Targeted treatment with stem cells has been proposed at the first discovery of increased vascularisation in the penumbra a few days after a stroke [72]. Consequently, treatment with stem cells has been reported to facilitate angiogenesis by stimulating the secretion of potent pro-angiogenic factors like VEGF and VEGFR2, increasing their serum concentration from pre- and during-stroke phases [73]. Angiogenesis by cerebral endothelial cell proliferation contributes to SCT-mediated recovery [55]. In addition, SCTs upregulate the concentration of angiopoietin 1 and Tie2, which induce vessel maturation, stabilisation, and remodelling [74, 75]. In preclinical studies, BMCs have been found to induce the expression of VEGF, angiopoietin 1, and Tie2, which increased angiogenesis and maturation of newly formed vessels [76, 77]. Other angiogenic factors, such as the fibroblast growth factor (FGF), GDNF, and BDNF, and chemoattractant factors, such as SDF-1, stimulate the proliferation of existing endothelial cells and mobilisation of endogenous endothelial progenitors via angiogenesis and vasculogenesis, respectively [77]. Apart from the indirect cell-induced effects reported above, the direct incorporation of stem cells into new blood vessels has also been noted [77]
Modulation of inflammatory responses
Ischemic stroke causes impairment of blood flow to an area of the brain, commonly from an occlusion [1]. This acute episode causes an upregulation of endogenous neuroinflammatory processes, which induces oxidative stress in the affected brain area, forming reactive oxygen species (ROS) [35]. ROS causes tissue damage from vasogenic oedema at infarcted areas with resultant disruption in tissue and fluid ion homeostasis [78]. This cascade induces neuroinflammation responses from injured neurons and supporting cells, which releases inflammatory modulators such as chemokines, cytokines, matrix metalloproteases (MMPs), and cellular adhesion molecules (CAMs) [78, 79]. The use of SCT for stroke suppresses and delays early secondary cell death by inhibiting oxidative stress, mitochondrial impairment, inflammation, and programmed cell death [80]. It also facilitates neuronal healing and reperfusion by activating other regenerative pathways, such as those causing vasculogenesis, neurogenesis, angiogenesis, and synaptogenesis [5, 8]. In addition, MSCs can scavenge free radicals, mitigating oxidative stress and preventing further damage [84[. MSCs and neural progenitor cells can suppress the proliferation of T cells and also modulate T cell induction in vitro by releasing immunosuppressive cytokines and factors [80,81,82]. Down-regulation of inflammatory and immune response genes induced more anti-inflammatory cytokines than pro-inflammatory cytokines after human MSCs were injected into the hippocampus after global ischemia [83].
Induction of host brain plasticity
Induction of host neuroplasticity is another mechanism by which SCTs mediate stroke recovery. Grafted stem cells deliver growth factors like human neural progenitors, promoting both ipsilesional and contralesional plasticity [13]. Neuronal plasticity and motor remapping have been hypothesised as an underlying mechanism for cell-mediated stroke recovery [84]. The same neurotrophic factors stem cells release for neuroprotection also stimulate neuronal growth and plasticity [85]. These factors activate signalling pathways that enhance the brain's ability to form new connections and reorganise existing ones. Plasticity implies increased connections between efferent and afferent fibres at the injury site with other brain parts, synaptogenesis, and the activation of new synapses [77]. SCT with human cord blood cells (HUCBs) and human bone-marrow stromal cells have been reported to induce this endogenous repair mechanism. Human bone-marrow stromal cells have specifically increased synaptophysin expression at the ischemic penumbra in a stroke-recovering brain [85]. NPCs-thrombospondins-mediated synaptogenesis has also been reported as a mechanism [77]. Furthermore, stem cells release exosomes, tiny vesicles containing various biomolecules. These exosomes transfer microRNAs, proteins, and other molecules that directly modulate signalling pathways involved in neuroplasticity, leading to enhanced neuronal connectivity and functional recovery [86].
Current evidence on stem cell use in stroke
Animal studies
The role of stem cell therapy in stroke recovery has been well-studied in animal models. Using different approaches, the studies assessed the efficacy and safety of the different stem cells and investigated their mechanisms of action. See Table 3. Bakreen [87] evaluated the role of a combination therapy comprising human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) and curcumin in a rat stroke model. Their study showed that combination therapy effectively improves neurological outcomes after stroke. The key mechanisms of action identified were anti-inflammatory and anti-oxidant effects. They suggested that the neuroprotective function is achieved through microglia polarisation using the AKT/GSK-3B/B-TrCP/Nrf2 pathway. Likewise, Sunyoung et al. [88] studied the use of a combination of hUCBCs and erythropoietin (EPO) in improving neurological outcomes in patients with subacute stroke, using male Sprague–Dawley rats. They found that the combination therapy of hUCBCs and EPO was more efficacious than either of the therapies used alone. Because of the increased expression of NeuN ( +) cells in the cortex of the animal models after treatment, the authors concluded that the mechanism of action of the stem cell is likely by modulation of neurogenesis and neuroprotection.
Bakreen [87] studied the therapeutic potential of adipose-tissue-derived mesenchymal stem cells in treating ischemic stroke. The study combined the stem cells with experimental rehabilitation and revealed improved behavioural recovery from the combination therapy. However, the study highlighted the need for further research in this area as the exact mechanism of action of the combination therapy is not yet known. Also, Rui He et al. [90] conducted a study using a rat model to evaluate the use of hMSCs in stroke recovery. They evaluated the response to the therapy using a parametric response map (PRM), highlighting its importance in detecting early changes in stroke lesions following therapy. Chi et al. [91] designed a study to evaluate the role of adipose-derived stem cells (ADSCs) in a mouse model of thromboembolism-induced brain infarction. However, the study had a major limitation because, in the experiment, the model did not have infarction.
Shalmali Patkar et al. [89] focused on inhibiting Dax-1 on neurological outcomes in transgenic mice stroke models. Neural stem cells (NSCs) were collected from the hippocampus of the mice. By targeting Dax-1, the level of 17B-estradiol was increased in the NSCs, demonstrating that the inhibition of Dax-1 is associated with improved synaptic neuroplasticity and neurological recovery. Likewise, Song et al. [93] used the influence of magnetic fields in stimulating the migration of human neural stem cells (hNSCs) toward target areas of ischemic brain injury in rat models. They discovered that magnetic fields increased the migration of hNSCs and improved recovery in the rat models. However, the authors noted that caution should be taken in using immortalised stem cells in the human population and suggested further research.
Kaiser et al. [94] studied the effects of nanoparticles with anti-inflammatory and anti-oxidative effects (Tan IIA-NPS) on induced pluripotent stem-cell-derived neural stem cells (iNSCs) using pig models with brain infarction. They found that this combination produced a multimodal enhancement of cell replacement, neuroprotection, and regenerative effects, providing good promise in recovery from ischemic stroke. Du et al. [92] studied the role of intracerebrally injected BMSCs in a rat stroke model and concluded that the administration was safe. However, they suggested optimisation of injection techniques and routes of administration to reduce adverse effects.
Human studies
Mesenchymal stem cells (MSCs)—noted for their safety, likely efficacy, reduced immunogenicity and ease of collection from tissues [100]—were chosen for use by de-Celis Ruiz et al. for the Allogeneic Adipose Tissue–Derived Mesenchymal Stem Cells In Acute Ischemic Stroke (AMASCIS) trial to demonstrate the safety of Adipose-derived MSCs in ischaemic stroke therapy. The trial was designed as a phase IIa, pilot, single-centre, prospective, randomised, double-blind, placebo-controlled clinical trial with a final study sample population of 13 patients—4 of whom received AD-MSCs (at a dose of 1 million cells per kilogram) while 9 were administered placebo. As no adverse effects related to the use of AD-MSCs were noted, the intravenous administration of AD-MSCs within the initial 14 days from symptomatic onset of ischaemic stroke was considered safe. The trial’s secondary outcome sought to demonstrate the efficacy of this therapy. However, no significant difference was observed compared to placebo [101]. See Table 3.
Bhasin et al. [96] utilised autologous mononuclear stem cells (MNCs) instead. They designed a non-randomised controlled observational study to investigate the safety, practicality, and effectiveness of MNC among 24 patients with chronic ischaemic stroke based on a set of defined clinical parameters and radiological imaging. 12 patients received an intravenous dose of 54.6 million cells while the other half received a placebo to be followed up at 24 week post-therapy. Given the absence of aberrant clinical, laboratory, and radiological findings, the trial concluded that autologous MNCs are safe, practical, and tolerable [69].
Based on the finding that plasma-depleted (PD) cord blood products are rich in Granulocyte-Colony Stimulating Factor (GCSF), Endothelial Growth Factor (EGF), Vascular Endothelial Growth Factor (VEGF), Lee et al. hypothesised that the use of PD cytokine products may contribute to brain repair following infarction [102, 103]. A 40-year-old patient with an MRI-confirmed infarct in the right ICA territory was recruited and transfused with umbilical cord blood 8 day post-stroke event with repeated doses of mannitol to facilitate blood–brain barrier entry. The findings from this case showed that the patient experienced an improvement in neurologic capacity, as evidenced by improved NIHSS, Berg Balance, and Barthel index scores [97].
MSCs can also be obtained from Wharton’s jelly and these cells have been demonstrated to have immunomodulating properties and provide neurogenesis-stimulating factors [104, 105]. One study evaluated the safety and likely potency of the serial use of Hospital Exemption-Advanced Therapy Medicinal Product (HE-ATMP), which has Wharton’s Jelly Mesenchymal stem cells (WJMSCs). From a pool of six patients with chronic stroke, the study reported a significant advancement in motor and communication ability with no adverse events reported [98].
Safety considerations
Ensuring the safety of stem cell therapies in stroke recovery is vital. Understanding and mitigating potential adverse effects and complications associated with stem cell therapies is crucial for their successful application in stroke recovery. Common adverse effects include immunological reactions, tumorigenesis, or unintended differentiation into undesired cell types [106, 107]. Rigorous preclinical and clinical studies are essential to identify and address these concerns, emphasising the need for robust safety profiles before widespread clinical implementation.
Moreover. long-term follow-up data are essential to assess stem cell therapies’ sustained safety and efficacy for stroke recovery. Monitoring patients over extended periods allows for identifying delayed adverse effects, assessment of the persistence of therapeutic effects, and understanding the potential for long-term complications. Comprehensive, well-designed longitudinal studies contribute valuable insights into stem cell interventions' safety profile and overall impact.
Furthermore, the ethics of stem cell research in stroke recovery extends to informed consent, patient autonomy, and responsible technology use. Obtaining informed consent from study participants is a cornerstone of ethical stem cell research. In stroke recovery, where individuals are vulnerable due to the severity of their condition, ensuring an understandable, informed consent process is important [2]. Respecting patient autonomy involves providing clear information about the potential risks, benefits, and uncertainties associated with stem cell therapies, allowing individuals to make informed decisions about their participation.
Ethical stem cell research requires a commitment to the equitable treatment of study participants. This involves ensuring access to experimental therapies is based on fair and just criteria, such as medical need and suitability for the study, rather than socioeconomic status or other non-clinical factors. Addressing disparities in access promotes the ethical distribution of the benefits and burdens of research, fostering a more just and inclusive scientific community. Maintaining transparency in stem cell research is crucial for upholding ethical standards. Researchers should communicate openly about study protocols, potential risks, and uncertainties. Transparent reporting of both positive and negative outcomes contributes to the integrity of the research process. Open dialogue with the scientific community, regulatory bodies, and the public fosters trust and ensures that ethical considerations remain at the forefront of stem cell research. Similarly, ethical stem cell research recognises the importance of engaging with the communities affected by stroke and involving stakeholders in the research process. Including diverse perspectives in decision-making enhances the ethical robustness of studies and considers the broader societal implications of stem cell interventions. This engagement helps researchers navigate complex ethical dilemmas and ensures that research benefits are shared equitably among diverse populations. Adherence to established ethical guidelines and regulatory frameworks is non-negotiable. Researchers must engage with institutional review boards (IRBs) and regulatory bodies to ensure their studies comply with ethical standards and legal requirements. Rigorous oversight helps prevent ethical lapses and ensures that study participants' rights, safety, and well-being are prioritised throughout the research.
Challenges and future directions
Addressing heterogeneity in study designs
One of the prominent challenges in stem cell therapies for stroke lies in the heterogeneity of study designs. Existing studies exhibit variations in experimental protocols, including differences in stem cell types, administration methods, and outcome measures [96, 100,101,102]. This heterogeneity makes it challenging to draw conclusions and comparisons across studies. Future directions should emphasise establishing standardised methodologies and ensuring consistency in experimental designs and outcome assessments. Collaboration among researchers to develop a unified framework will enhance the reliability and generalizability of findings, ultimately advancing the understanding of stem cell therapies for stroke.
Optimizing stem cell delivery methods
The optimal delivery method for stem cells in stroke therapy remains an area of ongoing investigation. Various routes, such as intravenous, intra-arterial, and intracerebral administrations, have been explored, each presenting unique advantages and challenges [44, 45]. Considerations, including the blood–brain barrier permeability, cell retention at the target site, and potential immune responses, necessitate further refinement of delivery methods. Future research should focus on identifying the most effective and safe delivery routes, considering factors such as cell type, disease stage, and individual patient characteristics to enhance the precision and efficacy of stem cell therapies.
Identifying subpopulations most likely to benefit
Stem cell therapies in stroke recovery may yield different benefits across all patient populations [39]. Identifying subpopulations most likely to benefit from specific stem cell interventions is critical to advancing personalised medicine in this field. Age, stroke aetiology, comorbidities, and genetic predispositions may influence individual responses to stem cell treatments. Future research directions should prioritise elucidating biomarkers or patient characteristics that can predict positive treatment outcomes. Tailoring stem cell interventions to specific subpopulations based on these factors can enhance treatment efficacy and contribute to developing targeted therapeutic approaches in stroke recovery.
However, the future of this field appears bright. Several ongoing clinical trials are poised to significantly impact stroke treatment protocols. The TOOTH study, for instance, is evaluating the safety and feasibility of using a patient's own dental pulp stem cells to treat chronic stroke [108]. If successful, this approach could pave the way for personalized stem cell therapies tailored to individual needs. Another promising avenue is explored in the J-REPAIR trial [109], which investigates the use of stem cells derived from donors (allogeneic) for treating acute ischemic stroke. This approach, if proven effective, could overcome logistical hurdles associated with autologous therapies and provide a more readily available treatment option. The results of these and other ongoing trials will be crucial for shaping the future of stem cell therapy for stroke recovery.
Limitations and strengths
The review examines the current state of research on stem cell therapies in stroke recovery, encompassing preclinical and clinical studies. The review incorporates recent studies, presenting a current snapshot of the field and including findings from various types of stem cells, enhancing the applicability of the information. The review acknowledges the heterogeneity in study designs across existing research, making it difficult to draw conclusive comparisons. While the review discusses several animal studies, the number of human studies in the current literature needs to be increased.
Conclusion
This review has provided an in-depth exploration of the current landscape of stem cell therapies for stroke recovery. Stroke, a prevalent and debilitating condition, presents significant challenges in terms of limited therapeutic options, especially concerning regenerative potential. While effective in managing acute symptoms, the conventional approaches lack the regenerative benefits necessary for comprehensive neural tissue recovery. Stem cell therapies emerge as a promising avenue, addressing existing stroke treatments’ temporal constraints and regenerative limitations. The mechanisms underlying stem cell-mediated recovery involve multifaceted processes, including neuroprotection, neurogenesis, angiogenesis, modulation of inflammatory responses, and induction of host brain plasticity. The evidence gathered from animal studies highlights the diverse applications of various stem cell types, shedding light on their efficacy in promoting neurological recovery.
Human studies, though limited, contribute valuable insights into the safety and potential efficacy of stem cell interventions. The studies reviewed cover a range of stem cell types, including MSCs derived from different tissues and MNCs. While safety appears promising, further research is warranted to establish the efficacy of these interventions conclusively. Safety considerations are paramount in stem cell therapies, focusing on minimising immunological reactions, tumorigenesis, and unintended differentiation. Long-term follow-up data and ethical considerations, including informed consent and patient autonomy, are crucial to ensure responsible technology use in stem cell research. Challenges in the field, such as the heterogeneity in study designs, optimisation of stem cell delivery methods, and identification of subpopulations most likely to benefit, need concerted efforts to overcome. Standardising methodologies, refining delivery routes, and personalising interventions based on biomarkers are critical steps in advancing the field.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were.
Abbreviations
- tPA:
-
Tissue plasminogen activator
- SCT:
-
Stem cell therapy
- MSCs:
-
Mesenchymal stem cells
- BDNF:
-
Brain-derived neurotrophic factor
- GDNF:
-
Glial cell line-derived neurotrophic factor
- PI3K:
-
Phosphatidylinositol 3-kinase
- Akt:
-
Protein kinase B
- BSCs:
-
Bone-marrow mesenchymal cells
- VEGF:
-
Vascular endothelial growth factor
- VEGFR2:
-
Vascular endothelial growth factor receptor 2
- FGF:
-
Fibroblast growth factor
- SDF-1:
-
Stromal cell-derived factor 1
- ROS:
-
Reactive oxygen species
- MMPs:
-
Matrix metalloproteases
- CAMs:
-
Cellular adhesion molecules
- NPCs:
-
Neural progenitor cells
- HUCBs:
-
Human umbilical cord blood cells
- EPO:
-
Erythropoietin
- PRM:
-
Parametric response map
- ADSCs:
-
Adipose-derived stem cells
- NSCs:
-
Neural stem cells
- NIHSS:
-
National Institutes of Health Stroke Scale
- HE-ATMP:
-
Hospital Exemption-Advanced Therapy Medicinal Product
- WJMSCs:
-
Wharton’s Jelly Mesenchymal Stem Cells
References
Wann LS, Dirksen CD, Hemphill M, et al. Guidelines for the management of ischemic stroke and intracerebral hemorrhage: a guideline for healthcare professionals from the American Stroke Association/American Heart Association. Stroke. 2018;49(e420):e41–210. https://doi.org/10.1161/STR.0b013e318296aeca.
World Health Organization. Stroke. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5298424/. Accessed 9 Sep 2021.
World Health Organization. The global burden of disease study 2019 (GBD 2019) results. https://ghdx.healthdata.org/gbd-2019. Accessed 14 Oct 2020.
Dembele J, Triccas LT, Amanzonwé LER, Kossi O, Spooren A. Bilateral versus unilateral upper limb training in (sub)acute stroke: a systematic and meta-analysis. South Afr J Physiother. 2024;80(1):1985. https://doi.org/10.4102/sajp.v80i1.1985.
Murphy SJ, Werring DJ. Stroke: causes and clinical features. Medicine. 2020;48(9):561–6. https://doi.org/10.1016/j.mpmed.2020.06.002.
The American Stroke Association/American Heart Association Stroke, Wann LS, Dirksen CD, Hemphill M, et al. Guidelines for the management of ischemic stroke and intracerebral hemorrhage: a guideline for healthcare professionals from the American Stroke Association/American Heart Association. Stroke. 2018;49(e420):e41–210. https://doi.org/10.1161/STR.0b013e318296aeca.
Aderinto N, Olatunji G, Abdulbasit MO, Edun M, Aboderin G, Egbunu E. Exploring the efficacy of virtual reality-based rehabilitation in stroke: a narrative review of current evidence. Ann Med. 2023;55(2):2285907. https://doi.org/10.1080/07853890.2023.2285907.
Hong JM, Kim DS, Kim M. Hemorrhagic transformation after ischemic stroke: mechanisms and management. Front Neurol. 2021;12:703258. https://doi.org/10.3389/fneur.2021.703258.
Arba F, Piccardi B, Palumbo V, Biagini S, Galmozzi F, Iovene V, et al. Blood–brain barrier leakage and hemorrhagic transformation: the reperfusion injury in ischemic stroke (RISK) study. Eur J Neurol. 2021;28(9):3147–54. https://doi.org/10.1111/ene.14985.
Li Y, Xia Y, Chen H, Liu N, Jackson A, Wintermark M, et al. Focal low and global high permeability predict the possibility, risk, and location of hemorrhagic transformation following intra-arterial thrombolysis therapy in acute stroke. AJNR Am J Neuroradiol. 2017;38(9):1730–6. https://doi.org/10.3174/ajnr.A5287.
Musmar B, Adeeb N, Ansari J, Sharma P, Cuellar HH. Endovascular management of hemorrhagic stroke. Biomedicines. 2022;10(1):100. https://doi.org/10.3390/biomedicines10010100.
Olatunji G, Kokori E, Isarinade T, Yusuf I, Udojike CI, Abimbola O, et al. Revolutionizing stroke care in Africa: a mini review of the transformative potential of mobile stroke units. Medicine. 2023;102(44): e35899. https://doi.org/10.1097/MD.0000000000035899.
Aderinto N, Olatunji D, Abdulbasit M, Edun M. The essential role of neuroimaging in diagnosing and managing cerebrovascular disease in Africa: a review. Ann Med. 2023;55(2):2251490. https://doi.org/10.1080/07853890.2023.2251490.
Yang L, Qian J, Yang B, He Q, Wang J, Weng Q. Challenges and improvements of novel therapies for ischemic stroke. Front Pharmacol. 2021;12:721156. https://doi.org/10.3389/fphar.2021.721156.
Xie F, Liu H, Liu Y. Adult neurogenesis following ischemic stroke and implications for cell-based therapeutic approaches. World Neurosurg. 2020;138:474–80. https://doi.org/10.1016/j.wneu.2020.02.010.
Hurd MD, Goel I, Sakai Y, Teramura Y. Current status of ischemic stroke treatment: from thrombolysis to potential regenerative medicine. Regen Ther. 2021;18:408–17. https://doi.org/10.1016/j.reth.2021.09.009.
Benedek A, Cernica D, Mester A, Opincariu D, Hodas R, Rodean I, et al. Modern concepts in regenerative therapy for ischemic stroke: from stem cells for promoting angiogenesis to 3D-bioprinted scaffolds customized via carotid shear stress analysis. Int J Mol Sci. 2019;20(10):2574. https://doi.org/10.3390/ijms20102574.
Wagenaar N, de Theije CGM, de Vries LS, Groenendaal F, Benders MJNL, Nijboer CHA. Promoting neuroregeneration after perinatal arterial ischemic stroke: neurotrophic factors and mesenchymal stem cells. Pediatr Res. 2018;83(1–2):372–84. https://doi.org/10.1038/pr.2017.243.
Jiao Y, Liu YW, Chen WG, Liu J. Neuroregeneration and functional recovery after stroke: advancing neural stem cell therapy toward clinical application. Neural Regen Res. 2021;16(1):80–92. https://doi.org/10.4103/1673-5374.286955.
Astarita C, Arora CL, Trovato L. Tissue regeneration: an overview from stem cells to micrografts. J Int Med Res. 2020;48(6):300060520914794. https://doi.org/10.1177/0300060520914794.
Poliwoda S, Noor N, Downs E, Schaaf A, Cantwell A, Ganti L, et al. Stem cells: a comprehensive review of origins and emerging clinical roles in medical practice. Orthop Rev. 2022. https://doi.org/10.52965/001c.37498.
Wang A, Tang Z, Park IH, Zhu Y, Patel S, Daley GQ, Li S. Induced pluripotent stem cells for neural tissue engineering. Biomaterials. 2011;32(22):5023–32. https://doi.org/10.1016/j.biomaterials.2011.03.070.
Farkhondeh A, Li R, Gorshkov K, Chen KG, Might M, Rodems S, et al. Induced pluripotent stem cells for neural drug discovery. Drug Discovery Today. 2019;24(4):992–9. https://doi.org/10.1016/j.drudis.2019.01.007.
Woodruff TM, Thundyil J, Tang SC, Sobey CG, Taylor SM, Arumugam TV. Pathophysiology, treatment, and animal and cellular models of human ischemic stroke. Mol Neurodegener. 2011;6(1):11. https://doi.org/10.1186/1750-1326-6-11.
Kawabori M, Shichinohe H, Kuroda S, Houkin K. Clinical trials of stem cell therapy for cerebral ischemic stroke. Int J Mol Sci. 2020;21(19):7380. https://doi.org/10.3390/ijms21197380.
Locatelli F, Bersano A, Ballabio E, et al. Stem cell therapy in stroke. Cell Mol Life Sci. 2009;66:757–72. https://doi.org/10.1007/s00018-008-8346-1.
Hosseini K, Lekholm E, Ahemaiti A, Fredriksson R. Differentiation of human embryonic stem cells into neuron, cholinergic, and glial cells. Stem Cells Int. 2020;2020:8827874. https://doi.org/10.1155/2020/8827874.
Huang NF, Li S. Mesenchymal stem cells for vascular regeneration. Regen Med. 2008;3(6):877–92. https://doi.org/10.2217/17460751.3.6.877.
Rikhtegar R, Yousefi M, Dolati S, Kasmaei HD, Charsouei S, Nouri M, Shakouri SK. Stem cell-based cell therapy for neuroprotection in stroke: a review. J Cell Biochem. 2019;120(6):8849–62. https://doi.org/10.1002/jcb.28207.
Llorente V, Velarde P, Desco M, Gómez-Gaviro MV. Current understanding of the neural stem cell niches. Cells. 2022;11(19):3002. https://doi.org/10.3390/cells11193002.
Galiakberova AA, Dashinimaev EB. Neural stem cells and methods for their generation from induced pluripotent stem cells in vitro. Front Cell Dev Biol. 2020;8:559464. https://doi.org/10.3389/fcell.2020.00815.
Denoth-Lippuner A, Jessberger S. Formation and integration of new neurons in the adult hippocampus. Nat Rev Neurosci. 2021;22:223–36. https://doi.org/10.1038/s41583-021-00433-z.
Boese AC, Le QE, Pham D, Hamblin MH, Lee JP. Neural stem cell therapy for subacute and chronic ischemic stroke. Stem Cell Res Ther. 2018;9:154. https://doi.org/10.1186/s13287-018-0913-2.
Zhang L, Zhu H, Wang Z. Neural stem cell transplantation therapy for brain ischemic stroke: review and perspectives. World J Stem Cells. 2019;11:817–30. https://doi.org/10.4252/wjsc.v11.i10.817.
Yamaguchi M, Seki T, Imayoshi I, Tamamaki N, Hayashi Y, Tatebayashi Y, et al. Neural stem cells and neuro/gliogenesis in the central nervous system: understanding the structural and functional plasticity of the developing, mature, and diseased brain. J Physiol Sci. 2016;66:197–206. https://doi.org/10.1007/s12576-015-0421-4.
Baker EW, Kinder HA, West FD. Neural stem cell therapy for stroke: a multimechanistic approach to restoring neurological function. Brain Behav. 2019;9: e01214. https://doi.org/10.1002/brb3.1214.
Detante O, Jaillard A, Moisan A, Barbieux M, Favre IM, Garambois K, et al. Biotherapies in stroke. Rev Neurol. 2014;170:779–98. https://doi.org/10.1016/j.neurol.2014.10.005.
Conaty P, Sherman LS, Naaldijk Y, Ulrich H, Stolzing A, Rameshwar P. Methods of mesenchymal stem cell homing to the blood–brain barrier. Methods Mol Biol. 2018;1842:81–91. https://doi.org/10.1007/978-1-4939-8697-2_6.
Chrostek MR, Fellows EG, Crane AT, Grande AW, Low WC. Efficacy of stem cell-based therapies for stroke. Brain Res. 2019;1722:146362. https://doi.org/10.1016/j.brainres.2019.146362.
Corey S, Abraham DI, Kaneko Y, Lee J, Borlongan CV. Selective endovascular cooling for stroke entails brain-derived neurotrophic factor and splenic IL-10 modulation. Brain Res. 2019;1722:146380. https://doi.org/10.1016/j.brainres.2019.146380.
Chen H, Zhou L. Treatment of ischemic stroke with modified mesenchymal stem cells. Int J Med Sci. 2022;19:1155–62. https://doi.org/10.7150/ijms.74161.
Li J, Zhang Q, Wang W, Lin F, Wang S, Zhao J. Mesenchymal stem cell therapy for ischemic stroke: a look into treatment mechanism and therapeutic potential. J Neurol. 2021;268:4095–107. https://doi.org/10.1007/s00415-020-10138-5.
Hsuan Y, Lin H, Chang P, Lin T. Mesenchymal stem cell-based treatments for stroke, neural trauma, and heat stroke. Brain Behav. 2016;6: e00526. https://doi.org/10.1002/brb3.526.
Melaccio A, Reale A, Saltarella I, Desantis V, Lamanuzzi A, Cicco S, et al. Pathways of angiogenic and inflammatory cytokines in multiple myeloma: role in plasma cell clonal expansion and drug resistance. J Clin Med. 2022;11:6491. https://doi.org/10.3390/jcm11216491.
Liu H, Reiter S, Zhou X, Chen H, Ou Y, Lenahan C, et al. Insight into the mechanisms and the challenges on stem cell-based therapies for cerebral ischemic stroke. Front Cell Neurosci. 2021;15:637210. https://doi.org/10.3389/fncel.2021.637210.
Xu K, Lee JY, Kaneko Y, Tuazon JP, Vale F, van Loveren H, et al. Human stem cells transplanted into the rat stroke brain migrate to the spleen via lymphatic and inflammation pathways. Haematologica. 2019;104:1062–73. https://doi.org/10.3324/haematol.2018.206581.
Acosta SA, Tajiri N, Hoover J, Kaneko Y, Borlongan CV. Intravenous bone marrow stem cell grafts preferentially migrate to spleen and abrogate chronic inflammation in stroke. Stroke. 2015;46:2616–27. https://doi.org/10.1161/STROKEAHA.115.009854.
di Val Cervo PR, Besusso D, Conforti P, et al. hiPSCs for predictive modelling of neurodegenerative diseases: dreaming the possible. Nat Rev Neurol. 2021;17:381–92. https://doi.org/10.1038/s41582-021-00465-0.
Thanaskody K, Jusop AS, Tye GJ, Safwani W, Dass SA, Nordin F. MSCs vs. IPSCs: potential in therapeutic applications. Front Cell Dev Biol. 2022;10:1005926. https://doi.org/10.3389/fcell.2022.1005926.
Fernández-Susavila H, Bugallo-Casal A, Castillo J, Campos F. Adult stem cells and induced pluripotent stem cells for stroke treatment. Front Neurol. 2019;10:908. https://doi.org/10.3389/fneur.2019.00908.
Ansari S, Azari H, McConnell DJ, Afzal A, Mocco J. Intraluminal middle cerebral artery occlusion (MCAO) model for ischemic stroke with laser doppler flowmetry guidance in mice. J Vis Exp. 2011;51:2879. https://doi.org/10.3791/2879.
He J, Russell T, Qiu X, Hao F, Kyle M, Chin L, et al. The contribution of stem cell factor and granulocyte colony-stimulating factor in reducing neurodegeneration and promoting neurostructure network reorganization after traumatic brain injury. Brain Res. 2020;1746:147000. https://doi.org/10.1016/j.brainres.2020.147000.
Rizvanov AA, Guseva DS, Salafutdinov II, Kudryashova NV, Bashirov FV, Kiyasov AP, et al. Genetically modified human umbilical cord blood cells expressing vascular endothelial growth factor and fibroblast growth factor 2 differentiate into glial cells after transplantation into amyotrophic lateral sclerosis transgenic mice. Exp Biol Med. 2011;236(1):91–8. https://doi.org/10.1258/ebm.2010.010172.
Liu X, Jia X. Neuroprotection of stem cells against ischemic brain injury: from bench to clinic. Transl Stroke Res. 2023. https://doi.org/10.1007/s12975-023-01163-3.
Chen J, Sanberg PR, Li Y, Wang L, Lu M, Willing AE, et al. Intravenous administration of human umbilical cord blood reduces behavioral deficits after stroke in rats. Stroke. 2001;32(11):2682–8. https://doi.org/10.1161/hs1101.098367.
Zhao X, Liu Q, Li J, Liu L. Endothelial progenitor cells promote tumor growth and progression by enhancing new vessel formation. Oncol Lett. 2016;12(2):793–9. https://doi.org/10.3892/ol.2016.4733.
Xiong Y, Mahmood A, Chopp M. Angiogenesis, neurogenesis and brain recovery of function following injury. Curr Opin Investig Drugs. 2010;11(3):298–308.
Yan F, Li J, Zhang W. Transplantation of endothelial progenitor cells: summary and prospect. Acta Histochem. 2023;125(1):151990. https://doi.org/10.1016/j.acthis.2022.151990.
Hatakeyama M, Ninomiya I, Otsu Y, Omae K, Kimura Y, Onodera O, et al. Cell therapies under clinical trials and polarized cell therapies in pre-clinical studies to treat ischemic stroke and neurological diseases: a literature review. Int J Mol Sci. 2020;21(17):6194. https://doi.org/10.3390/ijms21176194.
Wang J, Zhao J, Li S. Research progress on the therapeutic effect of olfactory ensheathing cell transplantation on ischemic stroke. J Neurorestoratol. 2021;9(2):83–93. https://doi.org/10.26599/JNR.2021.9040012.
Borlongan CV, Glover LE, Sanberg PR, Hess DC. Permeating the blood brain barrier and abrogating the inflammation in stroke: implications for stroke therapy. Curr Pharm Des. 2012;18(25):3670–6.
Lakhan SE, Kirchgessner A, Hofer M. Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med. 2009;7:1. https://doi.org/10.1186/1479-5876-7-1.
Zhang ZG, Chopp M. Neurorestorative therapies for stroke: underlying mechanisms and translation to the clinic. Lancet Neurol. 2009;8(5):491–500. https://doi.org/10.1016/S1474-4422(09)70061-4.
Chen J, Zhang ZG, Li Y, et al. Statins induce angiogenesis, neurogenesis, and synaptogenesis after stroke. Ann Neurol. 2003;53:743–51. https://doi.org/10.1002/ana.10555.
Wang L, Zhang Z, Wang Y, Zhang R, Chopp M. Treatment of stroke with erythropoietin enhances neurogenesis and angiogenesis and improves neurological function in rats. Stroke. 2004;35:1732–7. https://doi.org/10.1161/01.STR.0000128707.49091.30.
Katakowski M, Zhang ZG, Chen J, et al. Phosphoinositide 3-kinase promotes adult subventricular neuroblast migration after stroke. J Neurosci Res. 2003;74:494–501. https://doi.org/10.1002/jnr.10793.
Vojtek AB, Taylor J, DeRuiter SL, et al. Akt regulates basic helix-loop helix transcription factor-coactivator complex formation and activity during neuronal differentiation. Mol Cell Biol. 2003;23:4417–27. https://doi.org/10.1128/MCB.23.12.4417-4427.2003.
Chaudhary LR, Hruska KA. The cell survival signal Akt is differentially activated by PDGF-BB, EGF, and FGF-2 in osteoblastic cells. J Cell Biochem. 2001;81:304–11. https://doi.org/10.1002/jcb.1080.
Alessi DR, Andjelkovic M, Caudwell B, et al. Mechanism of activation of protein kinase B by insulin and IGF-1. EMBO J. 1996;15:6541–51. https://doi.org/10.1002/j.1460-2075.1996.tb01031.x.
Loubinoux I, Demain B, Davoust C, Plas B, Vaysse L. Stem cells and motor recovery after stroke. Ann Phys Rehabil Med. 2014;57(8):499–508. https://doi.org/10.1016/j.rehab.2014.06.003.
Borlongan CV, Hadman M, Sanberg CD, Sanberg PR. Central nervous system entry of peripherally injected umbilical cord blood cells is not required for neuroprotection in stroke. Stroke. 2004;35:2385–9. https://doi.org/10.1161/01.STR.0000143512.99815.80.
Kurozumi K, Nakamura K, Tamiya T, Kawano Y, Ishii K, Kobune M, et al. Mesenchymal stem cells that produce neurotrophic factors reduce ischemic damage in the rat middle cerebral artery occlusion model. Mol Ther. 2005;11:96–104. https://doi.org/10.1016/j.ymthe.2004.09.020.
Slevin M, Krupinski J, Slowik A, Kumar P, Szczudlik A, Gaffney J. Serial measurement of vascular endothelial growth factor and transforming growth factor-beta1 in serum of patients with acute ischemic stroke. Stroke. 2000;31:1863–70. https://doi.org/10.1161/01.STR.31.8.1863.
Yancopoulos GD, Klagsbrun M, Folkman J. Vasculogenesis, angiogenesis, and growth factors: ephrins enter the fray at the border. Cell. 1998;93:661–4. https://doi.org/10.1016/S0092-8674(00)81194-8.
Chen J, Zhang ZG, Li Y, et al. Intravenous administration of human bone marrow stromal cells induces angiogenesis in the ischemic boundary zone after stroke in rats. Circ Res. 2003;92:692–9.
Zacharek A, Chen J, Cui X, et al. Angiopoietin1/Tie2 and VEGF/ Flk1 induced by MSC treatment amplifies angiogenesis and vascular stabilization after stroke. J Cereb Blood Flow Metab. 2007;27(10):1687–701. https://doi.org/10.1038/sj.jcbfm.9600457.
Bliss T, Guzman R, Daadi M, Steinberg GK. Cell transplantation therapy for stroke. Stroke. 2007;38(2):817–26. https://doi.org/10.1161/01.STR.0000255754.28498.8f.
Ceulemans AG, Zgavc T, Kooijman R, Hachimi-Idrissi S, Sarre S, Michotte Y. The dual role of the neuroinflammatory response after ischemic stroke: modulatory effects of hypothermia. J Neuroinflamm. 2010;7(1):1–8.
Iadecola C, Anrather J. The immunology of stroke: from mechanisms to translation. Nat Med. 2011;17(7):796–808.
Bliss TM, Andres RH, Steinberg GK. Optimizing the success of cell transplantation therapy for stroke. Neurobiol Dis. 2010;37(2):275–83.
Einstein O, Fainstein N, Vaknin I, Mizrachi-Kol R, Reihartz E, Grigoriadis N, Lavon I, Baniyash M, Lassmann H, Ben-Hur T. Neural precursors attenuate autoimmune encephalomyelitis by peripheral immunosuppression. Ann Neurol. 2007;61:209–18.
Nasef A, Mathieu N, Chapel A, Frick J, Francois S, Mazurier C, Boutarfa A, Bouchet S, Gorin NC, Thierry D, Fouillard L. Immunosuppressive effects of mesenchymal stem cells: involvement of HLA-G. Transplantation. 2007;84:231–7.
Ohtaki H, Ylostalo JH, Foraker JE, Robinson AP, Reger RL, Shioda S, Prockop DJ. Stem/progenitor cells from bone marrow decrease neuronal death in global ischemia by modulation of inflammatory/immune responses. Proc Natl Acad Sci USA. 2008;105:14638–43.
Waseem A, Saudamini, Haque R, Janowski M, Raza SS. Mesenchymal stem cell-derived exosomes: shaping the next era of stroke treatment. Neuroprotection. 2023;1(02):99–116.
Li Y, Huang J, Wang J, Xia S, Ran H, Gao L, Feng C, Gui L, Zhou Z, Yuan J. Human umbilical cord-derived mesenchymal stem cell transplantation supplemented with curcumin improves the outcomes of ischemic stroke via AKT/GSK-3β/β-TrCP/Nrf2 axis. J Neuroinflamm. 2023;20(1):49.
Hwang S, Choi J, Kim M. Combining human umbilical cord blood cells with erythropoietin enhances angiogenesis/neurogenesis and behavioral recovery after stroke. Front Neurol. 2019;10(10):357.
Bakreen A. Combined adipose tissue-derived mesenchymal stem cell therapy and rehabilitation in stroke: safety, efficacy, and mechanisms underlying repair and recovery. Doctoral dissertation, Itä-Suomen yliopisto 2023.
Sunyoung H, JeeIn C, MinYoung K (2019) Combining human umbilical cord blood cells with erythropoietin enhances angiogenesis/neurogenesis and behavioral recovery after stroke. Front Neurol. https://doi.org/10.3389/fneur.2019.00357
Patkar S, Uwanogho D, Modo M, Tate RJ, Plevin R, Carswell HV. Targeting 17β-estradiol biosynthesis in neural stem cells improves stroke outcome. Front Cell Neurosci. 2022;22(16):917181.
He R, Moisan A, Detante O, Rémy C, Krainik A, Barbier EL, Lemasson B. Evaluation of parametric response mapping to assess therapeutic response to human mesenchymal stem cells after experimental stroke. Cell Transplant. 2017;26(8):1462–71.
Chi K, Fu RH, Huang YC, Chen SY, Lin SZ, Huang PC, Lin PC, Chang FK, Liu SP. Therapeutic effect of ligustilide-stimulated adipose-derived stem cells in a mouse thromboembolic stroke model. Cell Transplant. 2016;25(5):899–912.
Du S, Guan J, Mao G, Liu Y, Ma S, Bao X, Gao J, Feng M, Li G, Ma W, Yang Y, Zhao RC, Wang R. Intra-arterial delivery of human bone marrow mesenchymal stem cells is a safe and effective way to treat cerebral ischemia in rats. Cell Transplant. 2014;23(1_suppl):73–82.
Song M, Kim YJ, Kim YH, Roh J, Kim EC, Lee HJ, Kim SU, Yoon BW. Long-term effects of magnetically targeted ferumoxide-labeled human neural stem cells in focal cerebral ischemia. Cell Transplant. 2015;24(2):183–90.
Kaiser EE, Waters ES, Yang X, Fagan MM, Scheulin KM, Sneed SE, Cheek SR, Jeon JH, Shin SK, Kinder HA, Kumar A. Tanshinone IIA-loaded nanoparticle and neural stem cell therapy enhances recovery in a pig ischemic stroke model. Stem Cells Transl Med. 2022;11(10):1061–71.
de Celis-Ruiz E, Fuentes B, de Leciñana MA, et al. Final results of allogeneic adipose tissue-derived mesenchymal stem cells in acute ischemic stroke (AMASCIS): a phase II, randomized, double-blind, placebo-controlled, single-center, pilot clinical trial. Cell Transplant. 2022;31:9636897221083864.
Bhasin A, Srivastava M, Bhatia R, Mohanty S, Kumaran S, Bose S. Autologous intravenous mononuclear stem cell therapy in chronic ischemic stroke. J Stem Cells Regen Med. 2012;8(3):181–9. https://doi.org/10.46582/jsrm.0803011.
Lee TK, Lu CY, Tsai ST, et al. Complete restoration of motor function in acute cerebral stroke treated with allogeneic human umbilical cord blood monocytes: preliminary results of a phase I clinical trial. Cell Transplant. 2021;30:9636897211067448. https://doi.org/10.1177/09636897211067447.
Milczarek O, Swadźba J, Swadźba P, et al. Comparative analysis of the results of stroke treatment with multiple administrations of Wharton’s jelly mesenchymal stem cells-derived he-ATMP and standard conservative treatment: case series study. Cell Transplant. 2023;32:9636897231195144. https://doi.org/10.1177/09636897231195145.
Phan TG, Ma H, Lim R, Sobey CG, Wallace EM. Phase 1 Trial of Amnion Cell Therapy for Ischemic Stroke. Front Neurol. 2018;9:198. https://doi.org/10.3389/fneur.2018.00198.
Shen LH, Li Y, Chen J, Zhang J, Vanguri P, Borneman J, Chopp M. Intracarotid transplantation of bone marrow stromal cells increases axon-myelin remodeling after stroke. Neuroscience. 2006;137:393–9.
Carmichael ST. Cellular and molecular mechanisms of neural repair after stroke: making waves. Ann Neurol. 2006;59:735.
Vendrame M, Cassady J, Newcomb J, et al. Infusion of human umbilical cord blood cells in a rat model of stroke dose-dependently rescues behavioral deficits and reduces infarct volume. Stroke. 2004;35(10):2390–5. https://doi.org/10.1161/01.STR.0000141681.06735.9b.
Ehrhart J, Sanberg PR, Garbuzova-Davis S. Plasma derived from human umbilical cord blood: potential cell-additive or cell-substitute therapeutic for neurodegenerative diseases. J Cell Mol Med. 2018;22(12):6157–66. https://doi.org/10.1111/jcmm.13898.
Kim DW, Staples M, Shinozuka K, Pantcheva P, Kang SD, Borlongan CV. Wharton’s jelly-derived mesenchymal stem cells: phenotypic characterization and optimizing their therapeutic potential for clinical applications. Int J Mol Sci. 2013;14(6):11692–712. https://doi.org/10.3390/ijms140611692.
Ribeiro CA, Fraga JS, Grãos M, et al. The secretome of stem cells isolated from the adipose tissue and Wharton jelly acts differently on central nervous system derived cell populations. Stem Cell Res Ther. 2012;3(3):18. https://doi.org/10.1186/scrt109.
Bang OY, Lee JS, Lee PH, Lee G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol. 2005;57(6):874–82.
Bhatia V, Gupta V, Khurana D, Sharma RR, Khandelwal N. Randomized assessment of the safety and efficacy of intra-arterial infusion of autologous stem cells in subacute ischemic stroke. AJNR Am J Neuroradiol. 2018;39(5):899–904.
Nagpal A, Kremer KL, Hamilton-Bruce MA, et al. TOOTH (the open study of dental pulp stem cell therapy in humans): study protocol for evaluating safety and feasibility of autologous human adult dental pulp stem cell therapy in patients with chronic disability after stroke. Int J Stroke. 2016;11(5):575–85. https://doi.org/10.1177/1747493016641111.
Suda S, Nito C, Ihara M, et al. Randomised placebo-controlled multicentre trial to evaluate the efficacy and safety of JTR-161, allogeneic human dental pulp stem cells, in patients with Acute Ischaemic stRoke (J-REPAIR). BMJ Open. 2022;12(5): e054269. https://doi.org/10.1136/bmjopen-2021-054269.
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
NA conceptualised the study; all authors were involved in the literature review; GO and EK extracted the data from the reviewed studies; all authors wrote the final and first drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aderinto, N., Olatunji, G., Kokori, E. et al. Stem cell therapies in stroke rehabilitation: a narrative review of current strategies and future prospects. Egypt J Neurol Psychiatry Neurosurg 60, 79 (2024). https://doi.org/10.1186/s41983-024-00851-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-024-00851-7