Abstract
Background
Aneurysmal subarachnoid hemorrhage (SAH) is a vascular pathology with high morbidity and mortality that requires timely management to reduce the risk of complications. However, the ideal time for aneurysm clipping is still controversial. This study aimed to compare the degree of functional capacity at discharge of patients who underwent surgery for rupture of a cerebral aneurysm at different periods of time until surgery.
Results
132 patients who underwent surgery for SAH due to aneurysm rupture were included. The mean age was 52.5 years and 69.7% of participants were female. At admission, 96.2% were given a score of 1–3 on the World Federation of Neurological Surgeons scale and 79.6% received a score of 1–2 on the Hunt Hess scale. 8.3% of cases underwent surgery within the first 3 days of bleeding. The average time from clinical manifestation to surgical intervention was 7.1 days. At discharge 77.27% of patients presented good functional capacity. After adjusting for confounders, multivariate analysis showed a trend towards increased, albeit not statistically significant, risk in patients undergoing surgery at between 4 and 10 days (RR = 2.95 95% CI 0.80–10.87) and at > 10 days after SAH (RR = 2.65. 95% CI 0.72–9.79).
Conclusions
Despite the trend towards a higher probability of presenting poor functional capacity at discharge in patients undergoing aneurysm clipping more than 3 days after SAH, the differences were not statistically significant. There is a need for prospective randomized studies evaluating the best time to clip aneurysms, since aneurysm clipping is still a routine procedure in many countries.
Similar content being viewed by others
Background
Subarachnoid hemorrhage (SAH) caused by aneurysm rupture is an acute cerebrovascular event in which the bleeding occurs in the subarachnoid space normally occupied by cerebrospinal fluid. Although SAH accounts for only 5% of all cerebrovascular events, this pathology has a lethality rate of up to 50% [1].
SAH affects 6 to 9 per every 100,000 individuals worldwide [2], while in Peru, the incidence rate of SAH was 4.31 cases per 100,000 people [3] in 2018. In addition, in 2019 the Analysis of the Health Situation of Peru cataloged cerebrovascular events as the third most frequent cause of death in this territory [4].
As this pathology progresses, problems including rebleeding and/or vasospasm may occur, making timing crucial for achieving positive clinical and neurological outcomes in the case of a SAH [5]. The likelihood of disability and mortality, which typically manifest at certain time intervals, is increased in patients with SAH [6].
Rebleeding most frequently occurs within the first 24 h after the onset of bleeding, with the first 6 h carrying the highest risk of this consequence [5, 7]. Rebleeding has been associated with a higher likelihood of disability following the cerebrovascular episode [8].
Vasospasm is the constant constriction of intracranial blood vessels that can occur secondary to SAH [9]. The main time frame for the manifestation of this complication is the first 3 weeks after the onset of bleeding, with the fourth through tenth day having the highest risk of cerebral ischemia induced by vasospasm [10].
Early surgery (before day 3) may be desirable in order to prevent these two problems, however early surgery is not always possible. Patients with a poor initial clinical condition (Hunt and Hess score of 4 to 5) typically undergo surgery later since they may present substantial cerebral edema that can worsen cerebral ischemia [11, 12].
On the other hand, early surgery requires rapid medical response, the availability of tomography and angiography for achieving an early diagnosis, and the presence of a team of surgeons who are experts in the field. However, most Peruvian health care facilities typically do not have access to this infrastructure, thereby delaying treatment [13].
The ideal time for definitive surgical management of a ruptured cerebral aneurysm is still controversial [14]. A systematic review and meta-analysis reported high heterogeneity and inconsistency among studies addressing the relationship between neurological outcomes and time to surgery, with no significant differences in having poor clinical and neurological outcomes between those operated within, before or after the 3-day period following the hemorrhage [15]. This review also noted that studies that take into account the level of bleeding as a confounding factor are needed.
Additional research is therefore necessary to better understand the variation in risk among individuals over time until surgery in patients with a ruptured SAH. This study aimed to determine the association between the degree of functional capacity and the bleeding time until surgery in patients with SAH treated in the Vascular Neurosurgery Service of the Hospital Nacional Dos de Mayo in Lima, Peru.
Methods
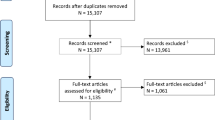
An observational, retrospective cohort study was conducted. The study population consisted of patients diagnosed with ruptured cerebral aneurysms in a referral hospital in Peru between 2018 and 2021.
During the study period all cases of SAH resulting from a ruptured cerebral aneurysm were included. The exclusion criteria were: cases with incomplete data related to the predictor or outcome variable, patients undergoing surgery for an arteriovenous malformation, and patients intervened for unruptured aneurysms.
The sample size was calculated to be 130 cases, with proportions of 0.32 for those with poor functional status at discharge and 0.68 for those with good functional status at discharge when comparing surgical intervention times before and after 3 days [10].
The term bleeding time was used to refer to the time from the recognition of the vascular event to the time of definitive surgical intervention, and the degree of functional capacity was defined by evaluation using the modified RANKIN scale at medical discharge [16]. The variables of age, sex, arterial hypertension, diabetes, obesity, Hunt and Hess scale, WFNS scale, Fisher scale, rebleeding, hydrocephalus, delayed cerebral ischemia, aneurysm size, aneurysm location, presence of additional unruptured aneurysms, and nosocomial infection were also analyzed.
The following cut-off points were used for the variable of bleeding time: 1 to 3 days, 4 to 10 days, and greater than 10 days, with the first period being considered early surgery, the second intermediate surgery, and the last period was considered as late surgery [10].
The modified Rankin scale was reclassified as a poor degree of functional capacity (4–6 points) and a good degree of functional capacity for the functional degree variable at discharge (0–3 points) [16].
A descriptive analysis was performed using absolute and relative frequencies for the categorical variables, while the mean and standard deviation, or median and interquartile range were used for the numerical variables, according to the distribution of normality.
In the bivariate analysis, Chi-square and T-tests were used, as appropriate. In order to avoid sparse data bias, only variables that had at least 10 observations in the category of interest were included in the bivariate and multivariate analyses [17].
Generalized linear models of the Poisson family were used to evaluate the relationship between bleeding time until surgery and functional grade at discharge. These models used log links and robust variances to calculate relative risks (RR) at 95% confidence intervals (95% CI). A p value less than 0.05 was considered significant. The statistical program Stata version 17.0 (Stata Corp, College Station, TX) was used for all analyses.
Results
Of the 158 patients initially identified for inclusion, those diagnosed with a ruptured arteriovenous malformation (n = 7), an unruptured cerebral aneurysm (n = 5), and those with incomplete data on the predictor or outcome variable (n = 14) were excluded. The study included 132 patients who had undergone treatment for aneurysmal SAH. All the patients received surgical clipping.
In the descriptive analysis (Table 1), the mean age was 52.59 years, with a minimum age of 14 years and a maximum of 86 years. Females made up 69.70% (n = 92) of the total number of participants. Arterial hypertension was present in 45.45% (n = 60) of the patients studied. There was no other relevant medical history was reported among the study participants.
At the time of hospitalization, all patients reported headache. On neurological evaluation, 96.21% (n = 127) received a score less than 3 on the WFNS scale, and only 5 patients had a score greater than 3. For the Hunt and Hess scale, 79.55% (n = 105) of patients received a score less than 2, with no patient receiving a score of 5. Furthermore, 56.82% (n = 57) presented a Fisher scale score of 3 to 4. The average time from clinical manifestation to surgical intervention was 7.1 days.
The mean size of the ruptured aneurysm was 5.62 mm, with the posterior communicating artery being the most common site (32.58%; n = 43), followed by the middle cerebral artery (25.76%; n = 34), and the anterior communicating artery (24.24%; n = 32). All the aneurysms registered in this analysis were saccular. In addition, additional unruptured cerebral aneurysms were found in 10.61% (n = 14) of the patients.
The bleeding time to surgery was 1 to 3 days in 8.32% (n = 11) of the patients, 4 to 10 days in 44.71% (n = 59), and greater than 10 days in 46.97% (n = 63). Rebleeding was present in 9.85% (n = 13), and delayed cerebral ischemia was reported in 11.36% (n = 15). A good functional grade at discharge was reported in 77.27% (n = 102) of the patients.
The bivariate analysis (Table 2) showed no significant differences between the degree of functional capacity at discharge and the length of bleeding time, with 18.18% of patients with a poor degree of high functional capacity undergoing surgery within the first 3 days, 23.73% at between 4 and 10 days, and 22.58% after 10 days (p = 0.921).
Furthermore, among patients with a low level of functional capacity at discharge, 44.44% had a high score on the Hunt and Hess scale, while only 17.14% had a score between 1 and 2, with these differences being statistically significant (p = 0.003).
In patients with poor functional capacity at discharge, 46.15% developed rebleeding while 20.17% did not (p = 0.034) and 60% presented delayed cerebral ischemia while 17.9% did not (p = 0.001).
In the crude regression analysis (Table 3), there were no significant differences in relation to the poor degree of functional capacity at discharge, between those undergoing surgery on days 4 to 10 (RR: 1.31; 95% CI 0.34–4 0.98) (p = 0.697) and those intervened after the 10th day (RR: 1.24, 95% CI 0.32–4.75) (p = 0.751), compared to patients undergoing surgery on or before the day 3.
The Hunt and Hess scale score (RR: 2.59; 95% CI 1.43–4.71) (p = 0.002), rebleeding complications (RR: 2.29; 95% CI 1.15–4.56) (p = 0.019) and late cerebral ischemia (RR: 3.34; 95% CI 1.89–5.90) (p < 0.01) were independent risk factors.
The risk of having a poor functional capacity at discharge tended to be higher in patients undergoing surgery at between 4 and 10 days after SAH (adjusted RR: 2.95; 95% CI 0.80–10.87) and after 10 days (adjusted RR: 2.65; 95% CI 0.72–9.79), although these differences were not statistically significant after adjusting for age, gender, hypertension, Hunt and Hess score, Fisher score, rebleeding, delayed cerebral ischemia, aneurysm size, cerebral circulation, and nosocomial infections.
Additionally, it was found that patients presenting delayed cerebral ischemia had a 2.42-fold greater risk of presenting a poor functional grade at discharge compared to those without this complication (adjusted RR: 2.42, 95% CI 1.05–5 0.58) (p = 0.038). A high Hunt and Hess scale score at hospital admission increased the risk of having a poor functional capacity grade at discharge (adjusted RR: 2.44, 95% CI 0.97–6.12) (p = 0.057), although the p-value was marginally significant.
Discussion
Our study found that the average time from clinical manifestation to surgical intervention was 7.1 days, possibly due to the limited access to healthcare services and a weak referral system between health centers in the country. However, our results indicate that performing surgery after the initial 3 days did not significantly increase the risk of a low degree of functional capacity at discharge compared to those who had surgery within the first 3 days. It is important to note that our findings revealed a marginal tendency towards increased risk for those operated on after 3 days. Other studies have reported a higher risk for patients undergoing endovascular treatment after 3 days, indicating that more research is necessary to corroborate our results. Furthermore, aneurysmal clipping remains the primary form of treatment in this country, making our study findings crucial for improving patient outcomes and underscores the importance of addressing the systemic barriers to timely surgical intervention in low- and middle-income countries.
A systematic review found no statistically differences in the global estimates of poor outcome in patients undergoing surgery before and 3 days after SAH. However, the subgroup of patients with a good Hunt and Hess score at hospital admission (less than 3) who underwent early surgery, presented better clinical outcomes and a lower mortality when compared to those undergoing surgery after 3 days. It should be noted that this study only included patients undergoing microsurgery, which differs from the type of surgical intervention performed in our study [15].
Similarly, another systematic review of patients who underwent endovascular treatment found no differences in neurological outcomes between those who underwent surgery before and after the first 3 days following SAH. However, patients undergoing surgery before day 1 had a lower possibility of poor outcomes than those intervened later than the first day after SAH [18].
These two systematic reviews seem to support the assumption that "as soon as feasible" is the optimal time for intervention, particularly for patients in a good initial clinical condition. These scenarios are unfeasible for low- and middle-income countries such as Peru, in which microsurgery and the endovascular methods are only available in specialized hospitals. Additionally, hyper-early surgery (before day 1) would not be feasible in most cases in Peru, since the average time of arrival to hospital of a patient with a cerebrovascular event is 51 h after the onset of the clinical presentation (18).
In relation to the surgical clipping intervention, a systematic review found that early surgery (0 to 3 days) and intermediate surgery (4 to 7 7 days) showed better results than late surgery (after 7 days) in patients in good condition. However, this review had the limitation that the patients were from different cohorts, and thus, the comparisons were indirect [19]. As a result, the optimal time for definitive surgical intervention remains controversial, and prospective randomized studies considering different periods and types of approach are still needed.
There are also some limitations to consider. Despite the fact that four years of surgical interventions were studied, the sample size might be limited. Furthermore, because some confounders had very few observations in the category of interest, they were excluded from the multivariate analysis. However, the adjusted model included the main confounders. Finally, although the Hunt and Hess score was included as a confounder, there were not enough data in the category of interest to present stratified models for this variable.
Conclusion
The ideal time for the definitive treatment of aneurysmal SAH is still controversial. In this study, patients who underwent aneurysm clipping later than the first 3 days after SAH had a lower degree of functional capacity at discharge than those undergoing aneurysm clipping within the first 3 days. However, this difference was not statistically significant.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SAH:
-
Aneurysmal subarachnoid hemorrhage
- WFNS:
-
World Federation of Neurological Surgeons scale
- RR:
-
Relative risk
- CI:
-
Confidence interval
References
van Gijn J, Kerr RS, Rinkel GJE. Subarachnoid haemorrhage. Lancet Lond Engl. 2007;369(9558):306–18. https://doi.org/10.1016/S0140-6736(07)60153-6.
Neifert SN, Chapman EK, Martini ML, Shuman WH, Schupper AJ, Oermann EK, et al. Aneurysmal subarachnoid hemorrhage: the last decade. Transl Stroke Res junio de. 2021;12(3):428–46. https://doi.org/10.1007/s12975-020-00867-0.
Bernabé-Ortiz A, Carrillo-Larco RM. Incidence rate of stroke in Peru. Rev Peru Med Exp Salud Publica. 2021;38(3):399–405. https://doi.org/10.17843/rpmesp.2021.383.7804.
Análisis de Situación de Salud del Perú.pdf. [citado 6 de octubre de 2022]. Disponible en: https://www.dge.gob.pe/portal/docs/asis/Asis_peru19.pdf
Tang C, Zhang TS, Zhou LF. Risk factors for rebleeding of aneurysmal subarachnoid hemorrhage: a meta-analysis. PLoS ONE. 2014;9(6):e99536. https://doi.org/10.1371/journal.pone.0099536.
Jabbarli R, Thiemo DF, Oppong DM, Daniela P, Philipp P, Karsten HW, et al. Risk factors for and clinical consequences of multiple intracranial aneurysms. Stroke. 2018;49(4):848–55. https://doi.org/10.1161/STROKEAHA.117.020342.
Rodríguez DR, Matamoros CES. Resangrado por ruptura aneurismática: epidemiología, factores asociados, fisiopatología y tratamiento. :8. Disponible en: http://revneuro.sld.cu/index.php/neu/article/view/147
Naidech AM, Janjua N, Kreiter KT, Ostapkovich ND, Fitzsimmons BF, Parra A, et al. Predictors and impact of aneurysm rebleeding after subarachnoid hemorrhage. Arch Neurol marzo de. 2005;62(3):410–6. https://doi.org/10.1001/archneur.62.3.410.
Chugh C, Agarwal H. Cerebral vasospasm and delayed cerebral ischemia: review of literature and the management approach. Neurol India febrero de. 2019;67(1):185–200. https://doi.org/10.4103/0028-3886.253627.
Qian Z, Peng T, Liu A, Li Y, Jiang C, Yang H, et al. Early timing of endovascular treatment for aneurysmal subarachnoid hemorrhage achieves improved outcomes. Curr Neurovasc Res febrero de. 2014;11(1):16–22. https://doi.org/10.2174/1567202610666131210104606.
Brilstra EH, Rinkel GJ, Algra A, van Gijn J. Rebleeding, secondary ischemia, and timing of operation in patients with subarachnoid hemorrhage. Neurology. 2000;55(11):1656–60. https://doi.org/10.1212/wnl.55.11.1656.
Dorhout Mees SM, Molyneux AJ, Kerr RS, Algra A, Rinkel GJE. Timing of aneurysm treatment after subarachnoid hemorrhage. Stroke. 2012;43(8):2126–9. https://doi.org/10.1161/STROKEAHA.111.639690.
Davalos LF, Málaga G. Stroke in Peru: a forgotten and unattended prevalent disease. Rev Peru Med Exp Salud Publica. 2014;31(2):400–1.
Cho WS, Kim JE, Park SQ, Ko JK, Kim DW, Park JC, et al. Korean clinical practice guidelines for aneurysmal subarachnoid hemorrhage. J Korean Neurosurg Soc. 2018;61(2):127–66. https://doi.org/10.3340/jkns.2017.0404.005.
Yao Z, Hu X, Ma L, You C, He M. Timing of surgery for aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Int J Surg Lond Engl. 2017;48:266–74. https://doi.org/10.1016/j.ijsu.2017.11.033.
Fernández Sanz A, Ruiz Serrano J, Tejada Meza H, Marta MJ. Validation of the Spanish-language version of the simplified modified Rankin Scale telephone questionnaire. Neurol Barc Ed Impr. 2019. https://doi.org/10.1016/j.nrl.2019.03.003.
Greenland S, Mansournia MA, Altman DG. Sparse data bias: a problem hiding in plain sight. BMJ. 2016;352:i1981. https://doi.org/10.1136/bmj.i1981.
Rawal S, Alcaide-Leon P, Macdonald RL, Rinkel GJE, Victor JC, Krings T, et al. Meta-analysis of timing of endovascular aneurysm treatment in subarachnoid haemorrhage: inconsistent results of early treatment within 1 day. J Neurol Neurosurg Psychiatry. 2017;88(3):241–8. https://doi.org/10.1136/jnnp-2016-314596.
de Gans K, Nieuwkamp DJ, Rinkel GJE, Algra A. Timing of aneurysm surgery in subarachnoid hemorrhage: a systematic review of the literature. Neurosurgery. 2002;50(2):336–40. https://doi.org/10.1097/00006123-200202000-00018.
Acknowledgements
Not applicable.
Author contributions
ALV, CJD, and MAP: contributed to the conception and design of the study. ALV and CJD: contributed to data acquisition. FOGS contributed to analysis and interpretation of data. FOGS and MAP: critical review of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study underwent previous evaluation and obtained approval by the Ethics Committee of Universidad Científica del Sur (No. 388-2021-PRE15) on 25th July, 2020. Further informed consent for the retrospective study was not necessary.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Loconi-Vallejos, A., Jorge-Dejo, C., Azurín-Peña, M. et al. Timing of aneurysm treatment in subarachnoid hemorrhage and grade of functional capacity at discharge: a retrospective cohort study. Egypt J Neurol Psychiatry Neurosurg 59, 89 (2023). https://doi.org/10.1186/s41983-023-00692-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00692-w