Abstract
Background
Idiopathic intracranial hypertension (IIH) is a neurological disorder of unknown etiology and ambiguous pathophysiology due to cerebrospinal fluid dysregulation. This study is designed to evaluate the role of brain magnetic resonance imaging (MRI) and magnetic resonance venography (MRV) in diagnosis of IIH, to clarify the nature and extent of cognitive deficits, and to detect if there is a correlation between radiology, clinical findings, and cognitive dysfunctions in those patients.
Results
The study included 34 patients and 34 age-, sex-, body mass index (BMI)-, and education-matched healthy control subjects. MR brain imaging and Montreal cognitive assessment (MoCA) test were used for both groups. MRI and MRV sensitivity for IIH diagnosis were 85.2% and 85.3% with 100% and 94.1% specificity respectively. 44.1% had cognitive impairment, memory was the most affected domain, followed by attention, abstraction, and orientation with statistically significantly lower total MoCA score (p < 0.005). Domain comparisons reveal a statistically significantly lower memory/delayed recall (p < 0.001) and abstract scores (p < 0.007) in IIH cases versus control subjects. In comparing patients with cognitive impairment (CI) versus those without CI, there were statistically significantly higher CI in low education level, presence of diplopia, hormonal contraceptive use, abnormal MRI brain, papilledema grades, BMI, and opening pressure.
Conclusions
Presence of more than or equal 3 MR imaging findings, bilateral transverse sinus stenosis, and less than or equal 4 combined conduit score increase the specificity and sensitivity of MRI and MRV for IIH diagnosis. IIH had detrimental effect on different cognitive domains especially when patient have low education level, diplopia, papilledema ≥ grade III, high OP ≥ 61.5 cm H2O, and BMI ≥ 34 Kg/m2 with abnormal MRI and MRV findings.
Similar content being viewed by others
Background
Idiopathic intracranial hypertension (IIH) is a neurological disorder of unknown etiology characterized by increased intracranial pressure (ICP) and normal composition of cerebrospinal fluid (CSF) with elevated opening pressure (OP) [1]. The pathophysiology is still ambiguous and supposed to be due to CSF dysregulation [2]. IIH commonly affects obese women in childbearing age; however, it can affect men, children, and non- obese individuals [3]. It has insidious onset with subsequent delayed diagnosis [4].
Neuro-ophthalmic evaluation is essential for diagnosis of IIH patients including headache, visual symptoms, olfactory dysfunction, pulsatile tinnitus, and sixth nerve palsy (6th NP) [5,6,7,8]. Although cognition is not screened routinely during clinical evaluation of IIH, many recent researches were done for assessment of cognitive function and reported cognitive impairment (CI) in these patients [9].
Neuroimaging especially magnetic resonance imaging (MRI) and magnetic resonance venography (MRV) are essential for exclusion of other etiologies of increased ICP and visualize various signs of IIH [10]. Lumbar puncture with elevated OP above 25 cmH2O and normal CSF composition are mandatory to establish a definite diagnosis [11]. Goals of management are to save vision and treat symptoms through medical therapy, surgical procedures, endovascular stenting, and weight loss [12].
The aim of this study was to evaluate the role of brain MRI and MRV in diagnosis of IIH, clarify the extent and nature of cognitive deficits in those patients, and detect if there is correlation between radiology, clinical findings, and cognitive dysfunctions.
Methods
A case control study was carried out in the neurology outpatient clinics and department after approval from Medical Research Ethical Committee. The study included 34 IIH patients (diagnosed according to modified Dandy criteria) [13] and 34 age-, sex-, BMI-, and education-matched healthy control subjects. Written agreement was obtained from all patients and control subjects prior to inclusion in our study. Inclusion criteria of patient group were IIH patients of both sexes, ages ranged from 18 to 50 years, and educated with at least primary level of education. Exclusion criteria were any patients with meningitis, venous sinus thrombosis, papilledema in absence of headache, illiterate, severe visual impairment, and patient with any contraindication to brain MRI.
All patients were subjected to thorough history taking and full clinical and neurological examination focusing on the following: age, sex, weight, and height. Headache was assessed according to onset, duration, frequency, site, severity [according to Numerical Rating Scale (NRS)], characters, and associated symptoms like photophobia, nausea, vomiting, and tinnitus. Visual complaints like visual obscuration, visual loss, diplopia, and blurring of vision were assessed. Ophthalmological examination was done including fundus examination with grading of papilledema [14]. Cognitive assessment was done by using Montreal cognitive assessment (MoCA) test. Past history of drugs causing elevated intracranial pressure especially hormonal contraception.
NRS
Headache severity was evaluated by self-assessment of pain intensity using NRS; it consists 11 points (0–10): 0 point indicates no pain, mild headache (1–3 score), moderate headache (4–7 score), and severe headache (8–10 score) [15, 16].
Cognitive function assessment
The cognitive function assessment was performed using MoCA test which is a rapid, brief, sensitive, and tool that has been considered as an effective tool for diagnosis of mild CI [17]. It consists of 30 items, divided into 7 scales, targeting different cognitive domains. A score of 26 or above was considered normal [18]. BMI calculation was as follows: BMI = weight (Kg)/[height(m)]2 and encompass the following categories: underweight = < 18.5, normal weight = 18.5–24.9, overweight = 25–29.9, and obesity ≥ 30 [19].
MR imaging techniques
Brain MRI was done for both patient and control groups by using a 1.5 T scanner (Siemens, Magnetom aera, Siemens healthcare, Germany). MRI brain was done by using head coil. MRI brain includes axial and sagittal T1-weighted images with repetition time (TR) 400 to 650 ms and echo time (TE) 8 to15 ms. Axial and coronal T2-weighted images were done with repetition time (TR) 4000 to 5500 ms and echo time (TE) 85 to 125 ms. All images were done with 3 mm slice thickness and 1 mm slice gap.
For assessment of optic nerve, optic nerve sheath and the posterior globe flattening axial and coronal T2-weighted turbo spin echo (TSE) sequence images were done by using surface coil along the optic tract (repetition time (TR) 6960 ms, echo time (TE) 99 ms, and slice thickness of 2 mm).
MRV was done for both groups to evaluate dural venous sinus stenosis (SVS) and to exclude dural venous sinus thrombosis (VST) as a cause of idiopathic intracranial hypertension. MRV was done by using two-dimensional time-of-flight (2D TOF) MR venography (repetition time (TR) 23 ms, echo time (TE) 6.5 ms, and slice thickness 2 mm.
Brain MRI and MRV images were assessed by a radiologist with more than 15 years’ experience. The radiologist was blinded to the clinical data of both patient and control groups. Brain MRI images were evaluated for pituitary gland height relative to sellar cavity height, optic nerve sheath diameter, presence or absence of flattening of posterior globe, or optic nerve tortuosity. MRV images were evaluated for transverse sinus thrombosis, stenosis, or hypoplasia [20].
Pituitary gland height was measured in mid-sagittal T1 weighted images by measuring the maximum distance between the sellar floor to the most upper surface of the pituitary gland. Pituitary gland height was classified relative to sella height into 5 grades. Grade 1 (normal appearance) in which there was flat or convex upper part of the pituitary gland, grade 2 (mild decrease of pituitary height) in which the decrease in pituitary gland height was less than one third of sellar cavity height, grade 3 (moderate decrease of pituitary height) in which the decrease in pituitary gland height was more than one third and less than two third of sellar cavity height, grade 4 (severe decrease of pituitary height) in which the decrease in pituitary gland height was more than two thirds of sellar cavity height with concavity of the upper surface of the pituitary gland and grade 5 (empty sella) in which the sellar cavity was enlarged with no detected pituitary gland inside (Figs. 1, 2, 3, and 4) [21].
a–d MRI and MRV of 37 years aged female patient diagnosed with idiopathic increase intracranial tension. a, b Axial T2 scan of left orbit shows tortuosity and grade 2 distention of left optic nerve sheath (white arrows) with flattened left posterior globe (arrowhead). c A mid-sagittal T1 MRI sellar cavity is enlarged with no detected pituitary gland inside grade 5 (empty sella) (blue arrow). d Time of flight MRV shows bilateral transverse sinus stenosis (the left transverse sinus is hypoplastic and also shows stenosis (red arrows)). Combined conduit score was 1 + 1 = 2
a–d MRI and MRV of 23 years aged female patient diagnosed with idiopathic increase intracranial tension. a, b Axial T2 scan of both orbits shows grade 2 distention of both optic nerve sheath (white arrows) with bilateral flattened posterior globe (arrowheads). c A mid-sagittal T1 MRI sellar cavity is enlarged with no detected pituitary gland inside grade 5 (empty sella) (blue arrow). d Time of flight MRV shows bilateral transverse sinus stenosis (red arrows) combined conduit score was 1 + 2 = 3
a–d MRI and MRV of 28 year aged female patient diagnosed with idiopathic increase intracranial tension. a, b Axial T2 scan of both orbits shows tortuosity of right optic nerve, grade 1 distention of both optic nerve sheaths (arrowheads) with flattened right posterior globe (arrow). c A mid-sagittal T1 MRI shows enlarged sellar cavity with no detected pituitary gland inside grade 5 (empty sella) (blue arrow). d Time of flight MRV shows bilateral transverse sinus stenosis (red arrows) combined conduit score was 0 + 1 = 1
a–d MRI and MRV of 44 year aged female patient diagnosed with idiopathic increase intracranial tension. a, b Axial T2 scan of both orbits shows tortuosity of right optic nerve and grade 1 distention of right optic nerve sheath (white arrow) with bilateral flattened posterior globe (arrowheads). c A mid-sagittal T1 MRI with no detected pituitary gland inside grade 5 (empty sella) (blue arrow). d Time of flight MRV shows bilateral transverse sinus stenosis (red arrows) combined conduit score was 0 + 1 = 1
Flattening of posterior globe was evaluated in axial T2-weighted images, and it was diagnosed when there is flattening or loss of convexity of the posterior globe at site of globe and optic nerve junction (Figs. 1, 2, 3, and 4) [22].
Optic nerve sheath diameter was measured in axial T2-weighted images in a plane perpendicular to the optic nerve and 3 mm posterior to the globe. An average value of both right and left optic nerve sheath diameter measurement was taken. Optic nerve sheath distention is graded into 3 grades (0–2). In grade 0, there is no CSF space detected around the optic nerve; in grade 1, the diameter of CSF space around the optic nerve was more than 1 mm and less than 2 mm (Figs. 3 and 4); and in grade 2, the diameter of CSF around the optic nerve was more than 2 mm (Figs. 1 and 2) [23].
Optic nerve tortuosity was evaluated in axial T2-weighted images, and it was diagnosed when there was optic nerve twisting in horizontal or vertical planes (Figs. 1, 3, and 4) [22].
All MRV images were evaluated according to the side of transverse sinus stenosis (unilateral or bilateral) and according to combined conduit score. The diameter of the distal part of superior sagittal sinus was measured and used as reference measurement to diagnose narrowed segment of both transverse/sigmoid junctions. In combined conduit score according to the degree of stenosis we gave a score for each transverse/sigmoid junction from 0 to 4. Score 0 (aplastic segment or gap) was given if there was a flow gap in the transverse/sigmoid junction, score 1 (severe stenosis or hypoplasia) was given if the diameter of conduit segment of transverse sinus was less than 25% of the distal superior sagittal sinus diameter, score 2 (moderate stenosis) was given if the diameter of the conduit segment of transverse sinus was between 26% to 50% of the diameter of distal superior sagittal sinus, score 3 (mild stenosis) was given if the diameter of the conduit segment of transverse sinus was between 51% to 75% of the diameter of distal superior sagittal sinus, and score 4 (normal) was given if the diameter of the conduit segment of transverse sinus was between 76% to 100% of the diameter of distal superior sagittal sinus [23].
The sum of the both right and left sinus score gave the combined conduit score (CCS). Combined conduit score ranged from 0 to 8. In this study, we used score 4 or less as cutoff value for diagnosis of significant transverse sinus stenosis (Figs. 1, 2, 3, and 4) [23].
Lumbar puncture
OP was measured in the lateral decubitus position with stretched legs and without the use of any sedative medications [24]. The patients were given a minimum of 10 min for relaxation before recording the OP [25] withdrawal amount of CSF for microbiology and biochemistry analysis.
For OP ≥ 56 cmH2O (Exposure, X) as a predictor of CI (Response, Y), power analysis was run using PASS 15 Power Analysis and Sample Size Software (2017), NCSS, LLC. Kaysville, Utah, USA, ncss.com/software/pass. A logistic regression of a binary response variable (Y) on a binary independent variable (X) with a sample size of 34 observations (of which 50% are in the group X = 0 and 50% are in the group X = 1) achieves 84% power at a 0.050 significance level to detect an odds ratio of 11.20. A two-sided Wald test is used.
Data were entered and analyzed using IBM-SPSS software (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Data were entered and analyzed using IBM-SPSS software (Version 25.0). Qualitative data were expressed as absolute frequency (N) and percentage (%). Quantitative data were initially tested for normality using Shapiro-Wilk’s test with data being normally distributed if p > 0.050. The presence of significant outliers (extreme values) was tested for by inspecting boxplots. Quantitative data were expressed as mean ± standard deviation (normally distributed). Chi-square or Fisher’s exact test was used to compare categorical data. Quantitative data between the two groups were compared by independent samples t test if normally distributed or Mann-Whitney U test if not. Cochran-Armitage test was run to test the correlation between ordinal independent variable and dichotomous dependent variable. Simple binary logistic regression was run to ascertain the effects of predictor variables on a dichotomous outcome with calculation of crude odds ratios and their 95% CI.
The accuracy of a test to discriminate diseased cases from non-diseased cases was evaluated by receiver operating characteristic (ROC) curve analysis which was done using MedCalc Statistical Software version 18.9.1 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2018). For any of the used tests, the results were considered as statistically significant if p value ≤ 0.050. Appropriate charts were used to graphically present the results whenever needed.
Results
Sociodemographic data
A case control study included two groups (patients and subjects): 34 patients and 34 controlled subjects; both groups were age, sex, BMI, and educationally matched. In the current study, sex distribution among patients included 32 females (94.1%) and 2 males (5.9%). Their age ranged from 19 to 48 year (mean ± SD = 32.8 ± 8.5 years). According to BMI (kg/m2), ideal body weight was 14.7%, overweight was 23.5%, and obese patients were 61.8% (mean ± SD = 31.9 ± 5.2).
Regarding headache, all patients suffered from headache; continuous headache was in 22 patients (64.7%), chronic headache in 8 patients (23.5%), and episodic headache in 4 patients (11.8%). According to site, bi-temporal location was seen in 15 patients (44.1%), global in 13 (38.2%), unilateral in 3 patients, and occipital in 3 patients (8.8% for each). As regards headache characters, 19 patients (55.9%) suffered from compressing type, 9 patients (26.5%) presented with throbbing headache, while 6 patients (17.6%) presented with dull aching headache. According to severity (NRS), in 23 patients (67.6%), the headache was severe; in 8 patients (23.5%), it was moderate; and in 3 patients (8.8%), it was mild. As regards associated symptoms; 12 patients (35.3%) complained from nausea and vomiting, 11 patients (32.4%), suffered from nausea, and 2 patients (5.9%) presented with vomiting. Bilateral tinnitus was in 8 patients while unilateral tinnitus was in 7 patients (Table 1), while there are visual manifestations and papilledema characters (Table 2).
According to MRI and MRV findings, the overall sensitivity of decreased pituitary gland height, flattened posterior globe, optic nerve sheath distention, and optic nerve tortuosity for diagnosis of IIH was 85.2%, 76.4%, 85.2%, and 26.5% respectively and specificity was 91.2%, 100%, 91.1%, and 100% respectively with accuracy of 88.2%, 88.2%, 88.2%, and 63.2% respectively (Tables 3 and 4).
The combination of three or more of these MRI signs increases the sensitivity and specificity to 85.2% and 100% respectively with 92.2% accuracy. The sensitivity and specificity of the use of 4 or less combined conduit score in diagnosis of IIH were 85.3% and 94.1% respectively with 89.7% accuracy. The sensitivity of unilateral, bilateral, and combined (unilateral and bilateral) transverse/sigmoid sinus stenosis in the diagnosis of IIH was 57.9%, 65.2%, and 76.5% respectively, and the specificity was 88.2%, 100%, and 88.2% respectively with an accuracy of 77.3%, 85.7%, and 82.3% respectively (Table 4).
Hormonal contraception was used by 26 (81.25%) out of 32 female patients for a median duration of 6.5 years that ranges from 1 to 25 years (25th percentile = 3, and 75th percentile = 13 years). In education in 34 cases, of the 34 patients, 18 patients (52.9%) received high education level (> 12 years), 15 patients (44.1%) received medium level of education (8–12 years), and only one patient received a low education level (< 8 years).
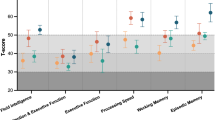
Of the 34 patients, 15 patients (44.1%) had cognitive impairment (MOCA score < 26). Memory was the most affected domain, followed by attention, abstraction, and orientation. In comparison between IIH patients and control subjects, there was a statistically significantly lower total MOCA score in IIH cases versus control subjects (p < 0.005), and cognitive impairment (MOCA< 26) statistically significantly lowered in IIH patients when compared with controlled subjects (p < 0.001). Domain comparisons revealed a statistically significantly lower memory/delayed recall (p < 0.001) and abstract scores (p < 0.007) (Table 5).
There was a statistically significantly higher MOCA score in high education level vs. low education level for all participants, control subjects, and IIH patients (Table 6).
Regarding the differences between those with and without CI, there was a statistically significantly higher low education level, presence of diplopia, hormonal contraceptive use (all cases), abnormal MRI brain (all cases), empty sella turcica (all cases), papilledema grades (right and left), BMI, and opening pressure in those with cognitive impairment (CI) vs. those without CI. Due to small sample size, multivariable logistic regression was not run. A univariate binary logistic regression analysis was performed to ascertain the effect of low education level, presence of diplopia, high OP, higher papilledema grades, and higher BMI on the likelihood that participants will exhibit cognitive impairment. Those with low education level have 4.3 times higher odds to exhibit CI as compared to those with high education level (P = 0.047). Those with diplopia have 10.3 times higher odds to exhibit CI as compared to those without diplopia; those with OP ≥ 56(cmH2O) have 11.2 times higher odds to exhibit CI as compared to those OP < 56 (cmH2O).
For every grade increase in papilledema on the right and left, there is an increase in odds ratios of 5.5 and 6.3, respectively, that participants will exhibit CI; for every increase in BMI by one unit, there is an increase in odds ratio of 1.2 that participants will exhibit CI; and for every increase in OP 1 cmH2O, there is increase in odds ratio of 11 that participants will exhibit CI (Table 7).
Regarding opening pressure (OP), the mean ± SD of OP was 54.1 ± 11.7 cmH2O ranging from 36 to 75 cmH2O and OP at cutoff value ≥ 56 cmH2O showed statistically significantly cognitive impairment (P < 0.001) (Fig. 5).
Discussion
This study exhibited that the majority of IIH occurs mainly in obese female patients (BMI > 30 kg/m2) in childbearing period as mentioned in previous researches [3, 26] that may be attributed to hormonal dysregulation and changes in metabolic neuroendocrine axis in this age [27, 28].
In this study, headache of increased ICP was the core symptom presents in all patients and was the leading cause for asking medical advice as reported in other many studies; however, headache characters were nonspecific in the current study [5, 29]. As regards headache type, continuous headache was the main presenting complaint followed by chronic then episodic type, and this was consistent with Yri and Jensen [30] and inconsistent with Skau and colleagues; they reported that episodic headache was the main presentation followed by continuous type [31]. The main site of headache in the current study was bi-temporal, global, and then unilateral which was concordant with Elbanhawy and colleagues [9]. Bitemporal location, compressing, throbbing, and then dull aching headache were the main characters in this study, but Skau and colleagues found that there is no characteristic quality as regards headache in their study [31].
Severe headache which was associated with nausea and or vomiting with unilateral or bilateral pulsatile tinnitus was presented in the majority of patients. This manifestation coincides with other previous studies [32, 33]. The etiology of pulsatile tinnitus is not completely elucidated, but it is supposed that stenosis in the transverse sinus, which were commonly observed in patients of this study, may produce audible turbulences in blood flow [5, 34].
As regards visual abnormalities in the current study, blurred vision was the main visual complaint; photophobia is where the patient cannot tolerate the light; transient visual obscurations were common and described by the patients of this study as blacking out of vision lasting for seconds and were associated with pasture changes. Bilateral or unilateral sixth palsy due to raised ICP was presented in about one fifth of our patients and was associated with horizontal diplopia. This abnormality was concordant with Mollan and colleagues’ study [35], while Quattrone and colleagues found sixth nerve palsy occurred in about one fourth of cases. Sixth nerve palsy is explained by its longest intracranial course which makes it more susceptible for stretching and also more liable to the mechanical effects as the results of displacement of brain stem backward due to increased ICP [36, 37].
Papilledema was a cornerstone in patients of this study which was detected by fundus examination as in agreement with previous studies [28, 38]; all patients of this study suffered from papilledema; bilateral symmetrical in the majority of patients except 8 patients showed asymmetrical grades between the right and left eye not more than one grade difference; the severity ranged from grade I to grade IV; the majority of patients presented with grade III and then grade II, and this was concordant with the study of Sultan and colleagues [3] who reported the effect of elevated ICP on optic nerve.
The role of MRI and MRV imaging in IIH is to exclude any other causes of increased ICP and search for characteristic imaging signs that can be used for diagnosis of IIH such as empty sella, optic nerve sheath distention, flattened posterior globe, optic nerve tortuosity, and transverse sinus thrombosis [39].
The decrease of the pituitary gland mid-sagittal height was the oldest and the commonest used MR imaging sign for prediction of idiopathic increase intracranial tension [40]. Decrease pituitary gland height in IIH may be caused by arachnocele herniation through the diaphragma sellae [40]. Decrease in pituitary gland height may occur in normal individuals and in various chronic causes of intracranial hypertension like intracranial neoplasm or cerebral venous sinus thrombosis [20].
Many studies concluded that the sensitivity of empty sella in IIH was relatively high which ranged from 65 to 80%, and these were matched with the current study where the sensitivity of decrease the pituitary gland height for diagnosis of IIH was 85.2%. In this study, the specificity of decreased pituitary gland height for diagnosis of IIH was 91.2%, and this was in agreement with many studies who reported that the specificity of empty sella for diagnosis of idiopathic increase intracranial tension ranged from 70 to 100% [10, 20, 41, 42].
Intra-orbital MR imaging signs detected in IIH include optic nerve sheath distention, flattened posterior globe, and optic nerve tortuosity. These signs are proved to be due to increased intracranial CSF pressure in IIH that is conducted to the intra-orbital part of optic nerve leading to increase CSF pressure in the subarachnoid space around the optic nerve [20].
In this study, the sensitivity and specificity of optic nerve sheath distention for diagnosis of IIH were 85.2% and 91.1 respectively, and these were higher than the results of many researches who concluded that optic nerve sheath distention was less sensitive (51%) and only moderately specific (83%) for diagnosis of IIH [2, 20].
In this study, the sensitivity and specificity of flattened posterior globe for diagnosis of IIH was 76.4% and 100% respectively, and these were in agreement with many studies who concluded that the sensitivity of flattened posterior globe for diagnosis of IIH varies between 43 and 85%, and with 98% specificity [10, 20, 41, 42].
In this study, the sensitivity and specificity of optic nerve tortuosity for diagnosis of IIH were 26.5 % and 100% respectively, and these were in agreement with many studies which concluded that the optic nerve tortuosity has low sensitivity (43%) and high specificity (90%) in diagnosis of IIH [10, 20, 41, 42].
In the current study, the presence of 3 or more MRI findings increases the sensitivity and specificity of MRI in diagnosis of idiopathic increase intracranial tension to 85.2 and 100% respectively with an accuracy of 92.2%; this was in agreement with Mallery and his colleagues’ study; they concluded that the combination of any three or more MRI findings is highly specific for diagnosis of idiopathic increase intracranial tension [43].
The main indication of MRV in patients of IIH is exclusion of cerebral venous sinus thrombosis. In these patients, MRV allows the evaluation of transverse/sigmoid sinus patency [44].
In this study according to the side of transverse sinus stenosis, the sensitivity and specificity of bilateral transverse sinus stenosis were higher (65.2% and 100% respectively) in the diagnosis of IIH than the sensitivity and specificity of unilateral transverse sinus stenosis (57.9 and 88.2 respectively) with total sensitivity and specificity of 76.5 and 88.2% respectively. This was in agreement with Farb and colleagues, Riggeal, and his colleagues’ studies; they concluded that the sensitivity and specificity of bilateral transverse sinus stenosis in diagnosis of idiopathic increase intracranial tension using MRV were high (93% and 100% of both studies respectively) [39, 44]. This study was also matched with the study of Mallery and his colleagues which concluded that the sensitivity of transverse sinus stenosis either bilateral or unilateral in diagnosis of IIH was 78% [10]. The study of Samanc and colleagues reported that bilateral transverse venous sinus stenosis is a common finding in intracranial hypertension patients without IIH and also may occur in normal individuals [20].
The study of Morino and his colleagues reported that transverse sinus stenosis either unilateral or bilateral is commonly seen in patients with idiopathic increase intracranial tension. It was still unknown if transverse sinus stenosis occurred as a cause or as a result of increase intracranial CSF pressure, because increased intracranial pressure exerts a compression on the transverse sinus and subsequent venous outflow obstruction. On the other hand, this obstruction caused decreases of the CSF absorption. Also, it was observed that bilateral transverse sinus stenosis stenting can decrease the elevated intracranial pressure. Also, normalization of intracranial pressure can resolve transverse sinus stenosis [40].
In the current study, the sensitivity and specificity of using 4 or less combined conduit score in the diagnosis of idiopathic increase intracranial tension were 85.3% and 94.1% respectively; this was not matched with the study of Ramesh and his colleagues as they concluded that the sensitivity (90%) of combined conduit score in the diagnosis of IIH was higher than its specificity (86.6%). This may be due to the selection of higher CCS cutoff value in the study of Ramesh and his colleagues; so many borderline false positive and false negative values were included in their results [45].
In conclusion, the combination of any three or more MRI findings as regards decreased pituitary gland height, optic nerve sheath distention, flattened posterior globe, and optic nerve tortuosity greatly increased the specificity and sensitivity for diagnosis of idiopathic increase intracranial tension. The presence of MRV findings as regards bilateral transverse sinus stenosis and less than or equal 4 combined conduit score also increased the specificity and sensitivity for the diagnosis of idiopathic increase intracranial tension.
Cognitive affection in patients with IIH has been reported in previous studies [25]. In all studies, apart from the case report by Kaplan and colleagues, 5 testing revealed significant cognitive impairment in patients with IIH especially in memory and verbal tests [46]. CI in patients with IIH occurs as a result of brain dysfunction which could be related to axonal flow as in optic nerve hydrops or impaired function of grey and or white matter of the brain as a result of mechanical compression [47].
In the current study, cognitive impairment (MoCA < 26) was observed in about 44% in the patients and showed to be highly statistically significantly lowered when compared with patients in the control group (P < 0.001) and also when compared with patients and control total MoCA score and percentage (P = 0.005); comparing different cognitive domains, all domains are affected when comparing patients with control subjects especially memory and abstraction which showed to be highly statistically significantly lower than the control (P < 0.001 and P = 0.007 respectively); this is consistent with Yri and colleagues; they found that IIH patients performed significantly worse cognitive function than controls in four of six cognitive domains. Deficits were prominent in reaction time and processing speed, significant impairment in working memory, and significant lower score in cognitive flexibility subset measuring [25].
In this study, comparing patients with cognitive impairment with patients with normal cognitive function, we found that low education level showed statistically significant lower cognitive function when compared with high education level (P = 0.042) which may be attributed to social state; this is consistent with Yri and his colleagues; they found that IIH is a state of socioeconomic consequences especially for young patients of working age [25]. Mollan and his colleagues found that patients living in a low socioeconomic state have a less resources to perform higher education with subsequently increased prevalence of obesity and therefore have increased incidence of IIH [48].
In this study, we found that diplopia had detrimental effect on cognition in which patients with diplopia showed statistically significant cognitive impairment when comparing patients with and without diplopia (P = 0.002); this was consistent with Shipster and his colleagues; they found that many factors have a potential effect, alone or in combination, to cause impairment in neurocognitive function in patients with ICP like diplopia and impaired hearing [49]. Our study showed that patients used contraception had statistically significant cognitive impairment when compared to non-cognitive impairment group (P = 0.004); the explanation is that the hormonal contraception increases the risk of obesity due to effect of progesterone which increases the appetite or facilitates anabolism while estrogen aggravates fat accumulation in adipose tissues and cells [50].
In current study, the cutoff opening pressure was 56 cm H2O in which patients with opening pressure ≥ 56 cm H2O showed statistically significant cognitive impairment when compared to non-cognitive impaired group (P = 0.002). This could be attributed to high pressure that causes mechanical compression with disturbed the function of grey and or white matter of the brain [47, 51]; reduction in cerebral blood flow that occurs in IIH may partly explain cognitive impairment in these patients.
In this study, the patients with increased BMI showed statistically significant cognitive impairment when compared with low BMI (P = 0.025). In the current study, patients with high-grade papilledema showed highly statistically significant cognitive impairment when compared with patients with low-grade papilledema on the right and left eye respectively (P = 0.003, P = 0.001).
We recognize limitations to this study. First, sub-analyses were limited due to small sample size; multivariable logistic regression was not run for the study. Second is the absent follow-up of the patients; lastly is the inability to assess the effect of different lines of treatment on cognition.
Conclusions
The presence of 3 or more characteristic MR imaging findings, bilateral transverse sinus stenosis, and 4 or less CCS increase the specificity and sensitivity of MRI and MRV for the diagnosis of idiopathic increase intracranial tension. IIH had a detrimental effect on different cognitive domains specifically memory/delayed recall, abstraction, and total MoCA score especially when the patient has low education level, diplopia, papilledema ≥ grade III, high OP ≥ 61.5 cm H2O, and BMI ≥ 34 Kg/m2 with abnormal MRI and MRV findings.
Availability of data and materials
The data supporting the results of this article are included within the article.
Abbreviations
- IIH:
-
Idiopathic intracranial hypertension
- ICP:
-
Intracranial pressure
- CSF:
-
Cerebrospinal fluid
- CI:
-
Cognitive impairment
- OP:
-
Opening pressure
- BMI:
-
Body mass index
- 6th NP:
-
Sixth nerve palsy
- MRI:
-
Magnetic resonance imaging
- MRV:
-
Magnetic resonance venography
- NRS:
-
Numerical Rating Scale
- MoCA:
-
Montreal cognitive assessment
- TSE:
-
Turbo spin echo
- TR:
-
Repetition time
- ET:
-
Echo time
- FOV:
-
Field of view
- TA:
-
Time of acquisition
- VSS:
-
Venous sinus stenosis
- VST:
-
Venous sinus thrombosis
- CCS:
-
Combined conduit score
- SD:
-
Standard deviation
- N:
-
Number
- N/V:
-
Nausea and/or vomiting
- IQR:
-
Inter quadratic ratio
- COR:
-
Crude odds ratio
- TP:
-
True positive
- FP:
-
False positive
- TN:
-
True negative
- FN:
-
False negative
- SN:
-
Sensitivity
- SP:
-
Specificity
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- FPOS:
-
Flat posterior optic sclera
- R:
-
Reference category
- CI:
-
Confidence interval
References
Hoffmann J, Mollan SP, Paemeleire K, Lampl C, Jensen RH, Sinclair AJ. European Headache Federation guideline on idiopathic intracranial hypertension. J Headache Pain. 2018;19(1):93. https://doi.org/10.1186/s10194-018-0919-2.
Toscano S, Lo Fermo S, Reggio E, Chisari CG, Patti F, Zappia M. An update on idiopathic intracranial hypertension in adults: a look at pathophysiology, diagnostic approach and management. J Neurol. 2020;27.
Sultan LI, Elnekidy AM, Elfatatry AM, Sayed A. A clinical and radiological study in patients with idiopathic intracranial hypertension. Egypt J Neurol Psychiatry Neurosurg. 2020;56(1):71. https://doi.org/10.1186/s41983-020-00189-w.
Jensen RH, Radojicic A, Yri H. The diagnosis and management of idiopathic intracranial hypertension and the associated headache. TA Neurol Disord. 2016;9(4):317–26. https://doi.org/10.1177/1756285616635987.
Bahnasy WS, El-Heneedy YA, Elhassanien ME, Sharaf AF, Khalid HA. Neuro-ophthalmological biomarkers of visual outcome in newly diagnosed idiopathic intracranial hypertension. Egypt J Neurol Psychiatry Neurosurg. 2019;55(1):26. https://doi.org/10.1186/s41983-019-0081-z.
Fisayo A, Bruce BB, Newman NJ, Biousse V. Over diagnosis of idiopathic intracranial hypertension. Neurol. 2016;86(4):341–50. https://doi.org/10.1212/WNL.0000000000002318.
Mollan SP, Davies B, Silver NC, Shaw S, Mallucci CL, Wakerley BR, et al. Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol Neurosurg Psychiatry. 2018;89(10):1088–100. https://doi.org/10.1136/jnnp-2017-317440.
Khoo KF, Kunte H. Olfactory dysfunction in patients with idiopathic intracranial hypertension. Neurology. 2014;82(2):189.
Elbanhawy IA, Ramzy GM, Basheer MA, Khedr DM. Neurophysiological tests screening cognitive impairment in idiopathic intracranial hypertension patients. Egypt J Neurol Psychiatry Neurosurg. 2018;54(1):7. https://doi.org/10.1186/s41983-018-0010-6.
Ridha MA, Saindane AM, Bruce BB, Riggeal BD, Kelly LP, Newman NJ, et al. MRI findings of elevated intracranial pressure in cerebral venous thrombosis versus idiopathic intracranial hypertension with transverse sinus stenosis. Neuro-ophthalmology. 2013;37(1):1–6. https://doi.org/10.3109/01658107.2012.738759.
Bono F, Salvino D, Tallarico T, Cristiano D, Condino F, Fera F, et al. Abnormal pressure waves in headache sufferers with bilateral transverse sinus stenosis. Cephalalgia. 2010;30(12):1419–25. https://doi.org/10.1177/0333102410370877.
Mollan SP, Markey KA, Benzimra JD, Jacks A, Matthews TD, Burdon MA, et al. A practical approach to, diagnosis, assessment and management of idiopathic intracranial hypertension. Pract Neurol. 2014;14(6):380–90. https://doi.org/10.1136/practneurol-2014-000821.
Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59(10):1492–5. https://doi.org/10.1212/01.WNL.0000029570.69134.1B.
Mollan SP, Hornby C, Mitchell J, Sinclair AJ. Evaluation and management of adult idiopathic intracranial hypertension. Pract Neurol. 2018;18(6):485–8. https://doi.org/10.1136/practneurol-2018-002009.
Dijkers M. Comparing quantification of pain severity by verbal rating and numeric rating scales. J Spinal Cord Med. 2010;33(3):232–42. https://doi.org/10.1080/10790268.2010.11689700.
Loder E, Burch R. Measuring pain intensity in headache trials: which scale to use? International Headache Society. Cephalalgia. 2012;32(3):179–82. https://doi.org/10.1177/0333102411434812.
Abou Elmaaty AA, Flifel MF, Zarad CA. Correlation between brain magnetic resonance imaging, cognitive dysfunction and physical dysability in multiple sclerosis. Egypt J Neurol Psychiatry Neurosurg. 2019;55:54.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Whitehead V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. https://doi.org/10.1111/j.1532-5415.2005.53221.x.
Consultation WHO. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Samanc B, Şahin E, Samanc Y, Ekizoğlu E, Yeşilot N, Çoban O, et al. The contribution of neuroimaging to diagnosis in idiopathic intracranial hypertension. Turk J Neurol. 2019;25(2):58–62. https://doi.org/10.4274/tnd.2018.64497.
Yuh W, Zhu M, Taoka T, Quets JP, Maley JE, Muhonen MG, et al. MR imaging of pituitary morphology in idiopathic intracranial hypertension. J Magn Reson Imaging. 2000;12(6):808–13. https://doi.org/10.1002/1522-2586(200012)12:6<808::AID-JMRI3>3.0.CO;2-N.
Tuncel SA, Yılmaz E, Çağlı B, Tekataş A, Çelik Y, Mehmet Ercüment M, et al. Lumbar opening pressure and radiologic scoring in idiopathic intracranial hypertension: is there any correlation? Pol J Radiol. 2017;82:701–5. https://doi.org/10.12659/PJR.903662.
Guliyeva A, Apaydin M, Beckmann Y, Sezgin G, Gelal F. Migraine or idiopathic intracranial hypertension: magnetic resonance venography and magnetic resonance imaging findings. Neuroradiol J. 2020;33(3):244–51. https://doi.org/10.1177/1971400920919322.
Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81(13):1159–65. https://doi.org/10.1212/WNL.0b013e3182a55f17.
Yri HM, Fagerlund B, Forchhammer HB, Jensen RH. Cognitive function in idiopathic intracranial hypertension: a prospective case–control study. BMJ Open. 2014;4(4):1–9.
Adderley NJ, Subramanian A, Nirantharakumar K, Yiangou A, Gokhale KM, et al. Association between idiopathic intracranial hypertension and risk of cardiovascular diseases in women in the United Kingdom. JAMANeurol. 2019;76:1088–98.
Virdee J, Larcombe SS, Vijay V, Sinclair AJ, Dayan M, Mollan SP. Reviewing the recent developments in idiopathic intracranial hypertension. Ophthalmol Therapy. 2020;9(4):767–81. https://doi.org/10.1007/s40123-020-00296-0.
Chagot C, Blonski M, Machu JL, Bracard S, Lacour JC, Richard S. Idiopathic intracranial hypertension: prognostic factors and multidisciplinary management. J Obes. 2017;2017:1–10. https://doi.org/10.1155/2017/5348928.
Headache Classification Committee of the International Headache Society. The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
Yri HM, Jensen RH. Idiopathic intracranial hypertension: clinical nosography and field-testing of the ICHD diagnostic criteria. A case-control study. Cephalalgia. 2015;35(7):553–62. https://doi.org/10.1177/0333102414550109.
Skau M, Brennum J, Gjerris F, Jensen R. What is new about idiopathic intracranial hypertension? An updated review of mechanism and treatment. Cephalalgia. 2006;26(4):384–99. https://doi.org/10.1111/j.1468-2982.2005.01055.x.
Binder DK, Horton JC, Lawton MT, McDermott MW. Idiopathic intracranial hypertension. Neurosurgery. 2004;54(3):538–51. https://doi.org/10.1227/01.NEU.0000109042.87246.3C.
González-Hernández A, Fabre-Pi O, Díaz-Nicolás S, López-Fernández JC, López-Veloso C, Jiménez-Mateos A. Headache in idiopathic intracranial hypertension. Rev Neurol. 2009;49(1):17–20.
Giuseffi V, Wall M, Siegel PZ, Rojas PB. Symptoms and disease associations in idiopathic intracranial hypertension (pseudotumor cerebri): a case control study. Neurology. 1991;41(2):239. https://doi.org/10.1212/WNL.41.2_Part_1.239.
Mollan SP, Ali F, Hassan-Smith G, Botfield H, Friedman DI, Sinclair AJ. Evolving evidence in adult idiopathic intracranial hypertension: pathophysiology and management. J Neurol Neurosurg Psychiatry. 2016;87(9):982–92. https://doi.org/10.1136/jnnp-2015-311302.
Quattrone A, Bono F, Fera F, Lavano A. Isolated unilateral abducens palsy in idiopathic intracranial hypertension without papilledema. Eur J Neurol. 2006;13(6):670–1. https://doi.org/10.1111/j.1468-1331.2006.01279.x.
Larner AJ. False localizing signs. J Neurol Neurosurg Psychiatry. 2003;74(4):415–8. https://doi.org/10.1136/jnnp.74.4.415.
Smith SV, Friedman DI. The idiopathic intracranial hypertension treatment trial: a review of the outcomes. Hedache. 2017;57(8):1303–10. https://doi.org/10.1111/head.13144.
Riggeal BD, Bruce BB, Saindane AM, Ridha MA, Kelly LP, Newman NJ, et al. Clinical course of idiopathic intracranial hypertension with transverse sinus stenosis. Neurology. 2013;80(3):289–95. https://doi.org/10.1212/WNL.0b013e31827debd6.
Moreno-Ajona D, McHugh JA, Hoffmann J. An update on imaging in idiopathic intracranial hypertension. Front Neurol. 2020;11:453. https://doi.org/10.3389/fneur.2020.00453.
Maralani PJ, Hassanlou M, Torres C, Chakraborty S, Kingstone M, Patel V, et al. Accuracy of brain imaging in the diagnosis of idiopathic intracranial hypertension. Clin Radiol. 2012;67(7):656–63. https://doi.org/10.1016/j.crad.2011.12.002.
Rohr AC, Riedel C, Fruehauf MC, Baalen V, Bartsch T, Hedderich J, et al. MR imaging findings in patients with secondary intracranial hypertension. AJNR Am J Neuroradiol. 2011;32(6):1021–9. https://doi.org/10.3174/ajnr.A2463.
Mallery RC, Rehmani OF, Woo JH, Chen YJ, Reddi S, Salzman KL, et al. Utility of magnetic resonance imaging features for improving the diagnosis of idiopathic intracranial hypertension without papilledema. J Neuroophthalmol. 2019;39(3):299–307. https://doi.org/10.1097/WNO.0000000000000767.
Farb RI, Vanek I, Scott JN, Mikulis DJ, Willinsky RA, Tomlinson G, et al. Idiopathic intracranial hypertension: the prevalence and morphology of sinovenous stenosis. Neurology. 2003;60(9):1418–24. https://doi.org/10.1212/01.WNL.0000066683.34093.E2.
Ramesh R, Peter SB, Kailasanathan N. Significance of transverse sinus stenosis in idiopathic intracranial hypertension patients using contrast enhanced magnetic resonance venogram. IOSR J Dent Med Sci. 2016;15(10):30–41. https://doi.org/10.9790/0853-1510033041.
Kaplan CP, Miner ME, McGregor JM. Pseudotumour cerebri: risk for cognitive impairment? Brain Inj. 1997;11(4):293–303. https://doi.org/10.1080/026990597123601.
Beeri MS, Moshier E, Schmeidler J. Serum concentration of an inflammatory glycotoxin, methylglyoxal, is associated with increased cognitive decline in elderly individuals. Mech Ageing Dev. 2011;132(11-12):583–7. https://doi.org/10.1016/j.mad.2011.10.007.
Mollan SP, Aguiar M, Evison F, Frew E, Sinclair AJ. The expanding burden of idiopathic intracranial hypertension. Eye. 2019;33(3):478–85.
Shipster C, Hearst D, Dockrell JE, Kilby E. Speech and language skills and cognitive functioning in children with Apert syndrome : a pilot study. Int J Lang Commun Disord. 2002;37(3):325–43. https://doi.org/10.1080/13682820210138816.
Sugiharti S, Hadi H, Julia M. Hormonal contraception as a risk factor for obesity. Med J Indones. 2005;14.
Lorberboym M, Lampl Y, Kesler A, Sadeh M, Gadot N. Benign intracranial hypertension: correlation of cerebral blood flow with disease severity. Clin Neurol Neurosurg. 2001;103(1):33–6. https://doi.org/10.1016/S0303-8467(01)00107-X.
Acknowledgements
The authors are grateful to all patients and control subjects for their willingness to participate in this study.
Funding
There is no source of funding for the research.
Author information
Authors and Affiliations
Contributions
AAM, CAZ, TB, and TSE carried out the work. AAM designed the protocol, shared in collecting scientific data, did the statistical analysis, and was responsible for writing the initial draft of the manuscript. TB and TSE shared in collecting the scientific data and shared in writing the initial draft of the manuscript. CAZ shared in the design the protocol and shared in collecting the scientific data. CAZ interpreted the radiology of all patients. All authors read and approved the final version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors obtained permission to conduct this study that was approved from Medical Research Ethical Committee, Institutional Review Board, Mansoura Faculty of Medicine, Mansoura University (code number: R.21.03.1249) All participants gave written informed consent. The procedures followed were in accordance with our protocol. We recruited 34 patients and 34 control subjects from neurology outpatient clinics and neurology department of Mansoura university hospitals.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elmaaty, A.A.A., Zarad, C.A., Belal, T.I. et al. Diagnostic value of brain MR imaging and its correlation with clinical presentation and cognitive functions in idiopathic intracranial hypertension patients. Egypt J Neurol Psychiatry Neurosurg 57, 89 (2021). https://doi.org/10.1186/s41983-021-00338-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-021-00338-9