Abstract
Background data
Post spinal surgery infection is not uncommon. It is considered as one of the most annoying complication following surgery on the spine. The major burdens of post spinal surgery infection are time and money consuming. Infections have a considerable effect on post-operative morbidity and mortality.
Purpose
The aim of this study was to identify the possible risk factors, preventive measures, diagnostic tools and the ideal management procedures.
Study design
Retrospective study.
Patients and methods
This is a retrospective study which was carried out on 35 patients operated upon (either primary or revision) for variable spinal lesions from 2006 till 2016 and complicated by post spinal surgery infection. No patient was operated upon for primary pre-existing spinal infection or congenital lesions. Patients were operated upon by same surgeon in the same hospital. On presentation, the patients were diagnosed to have post-operative infection by clinical examination, laboratory and radiological investigations. All patients were re-admitted to the hospital where the proper management was done.
Results
Most of cases were associated with pre-operative risk factors and intra or post-operative complications. Cervical disc prolapse (8 patients) was the most common lesion in the cervical region group, whereas lumbar disc prolapse (12 patients) was the most common lesion in lumbar group. Six patients suffered from complications (durotomy in 5 patients and right common iliac artery injury in one patient). Superficial infection was encountered in 12 patients and deep infection was diagnosed in 19 patients, whereas combined infection was diagnosed in 4 patients. Surgical management that needed general anesthesia was provided to 22 patients whereas conservative management was provided to 13 patients. Out of 35 cases, only one patient died from the complications of infection.
Conclusion
Post spinal surgery infection is a devastating complication that needs multi-modalities for prevention and control. Neutralization of the pre-operative risk factors can dramatically reduce the post-operative infections. Once diagnosed, the patients with infection must be hospitalized and extensive management should be applied.
Similar content being viewed by others
Introduction
Post spinal surgery infection is not uncommon and is considered as one of the most annoying complication following surgery on the spine. It ranged from 0 to 17% [1, 2]. Many risk factors may predispose to the development and worsening of post-operative infection. Patient’s related factors are diabetes, rheumatoid, obesity, renal failure, old age, alcohol addiction, pre-operative epi-dural steroid injection and smoking. These form the most important risk factors [3,4,5]. Pre-operative knowledge about these factors, especially if treatable, can greatly modify the post-operative results. Intraoperative complications, foreign body implantation, excessive tissue devascularization, haemorrhage, dural injury, esophageal perforation and prolonged procedures can result in post-operative infection [6, 7]. The major burdens of post spinal surgery infection are time and money consuming effects. Infections have a considerable effect on post-operative morbidity and mortality [8]. Recently, post spinal surgery infection was subtyped into superficial, deep and organ space infection. Infections of the skin and subcutaneous tissues are considered as superficial infections which may occur within 1 month from surgery and associated with infected discharge which gives positive results on cultures. Infections of the fascia and muscles are the targets of deep infection with infected discharge or abscess formation. Infections deep to the muscles are considered as organ space infection with psoas abscess, discitis, spondylitis, or epi-dural abscess formation [9]. The gold standard is to prevent post-operative infection but if it occurs, early diagnosis and ideal management are mandatory to achieve a good recovery. Early diagnosis depends on clinical evaluation, laboratory and radiological investigations [10]. The aim of this study was to identify the possible risk factors, preventive measures, diagnostic tools and the ideal management procedures.
Materials and methods
This is a retrospective study which was carried out on 35 patients operated upon (either primary or revision) for variable spinal lesions from 2006 till 2016 and complicated by post spinal surgery infection. No patient was operated upon for primary pre-existing spinal infection or congenital lesions. On presentation, the patients were diagnosed to have post-operative infection by clinical examination, laboratory and radiological investigation. All patients were re-admitted to the hospital even those with superficial infections for fear of spread of infection to the deep layers where the urgent management was done. During the hospital stay, the patients were followed up laboratory and radiological investigations. The laboratory investigations included complete blood picture, blood sugar, culture and sensitivity from the wound, renal and liver function tests and C-reactive protein. The radiological investigations included plain X-ray, CT scan and MRI. After complete healing of infection, the patients were followed up for at least 6 months after discharge from the hospital for fear or recurrence of infection. Summary of the clinical data of cervical, dorsal and lumbar patients was categorized in Tables 1, 2 and 3 respectively.
Results
As regard:
The level of affection: 13 patients had cervical lesions, 4 had dorsal lesions and 18 had lumbar affection.
The age ranged from 22 to 76 years with mean of 52.7 years.
The sex: The patients were 20 males and 15 females.
Pre-operative risk factors were evident in 27 patients. Diabetes (in 12 patients) and obesity (in 8 patients) were the most common risk factors.
Primary lesion: cervical disc prolapse (8 patients) was the most common lesion in the cervical region group, whereas lumbar disc prolapse (12 patients) was the most common lesion in lumbar group.
Duration and type of operation: ranged from 45 to 200 min. Discectomy either cervical or lumbar (20 patients) was the most common operative technique in the infected group.
Intra-operative complications: 6 patients suffered from complications (durotomy in 5 patients and right common iliac artery injury in one patient).
Foreign body implantation: was done in 19 patients. Cages, plates and screws were the most common foreign body implanted.
Post-operative complications: were observed in 13 patients. Esophageal perforation was the most dangerous and devastation complication and was faced after tracheostomy.
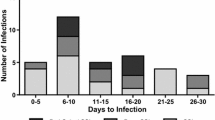
Lucid interval (between the primary surgery and the diagnosis of infection): ranged from 5 days to 4 months.
Type of infection: superficial infection was encountered in 12 patients and deep infection was diagnosed in 19 patients, whereas combined infection occurred in 4 patients.
Management: surgical management that needs general anaesthesia was done in 22 patients whereas conservative management was provided to 13 patients. The plates were removed in 3 cases in which poor response to suction irrigation was encountered. We observed that the use of irrigation with CSF leak would not delay the healing or prolong the leak.
Re-hospitalization stay: ranged from 10 days to 3 months.
Fate: out of 35 cases, only one patient died from the complications of infection.
Discussion
The number of spinal operations had greatly increased due to many factors. Increased awareness about the spine biomechanics and development of many devices that facilitate and increase the accuracy and safety of new techniques are among these factors [11]. Consequently, the post-operative complications including post spinal surgery infections have increased. Post spinal surgery infections result from reaction and integration of patient, hospital and surgery team factors. Great efforts should be directed to prevent the morbidity and mortality sequelae of infections [12]. The great importance of post spinal infection is the economic burdens related to re-admission of the patients or revision surgeries [13, 14].
The mean age in this study is 52.7 years which is comparable with the age of patients with post spinal infections in literature which is above 48 years, and this may be due to decreased immunity with age [15, 16].
Pre-operative risk factors played a very significant role in the occurrence, type and management of post spinal infections. Diabetes and obesity were the most common risk factors detected in our study, and this observation is matching with other authors. Some authors reported increased incidence of post-operative infection with previous history of epidural corticosteroid injection, rheumatoid, renal failure, old age and alcohol addiction [5, 17, 18].
Increased incidence of infection with foreign body implantation was observed, and this infection is more resistant to treatment. This observation was explained in a study proofed that these organisms are firmly adherent to the surface of the foreign body forming the biofilm leading to colonization of organisms leading to antimicrobial resistance [19].
In many studies, post-operative infection usually occur in the first 4 weeks after surgery but late superficial or deep infections may occur even after 1 year from surgery [20,21,22].
Intra- or post-operative complications may be the precipitating factors and largely affect the development of post-operative infections especially if being major or devastating complications. In our study, we faced one major intra-operative complication in the form of right common iliac artery injury in a case operated upon for recurrent lumbar disc prolapse causing massive bleeding in the surgical site and forming a large retro-peritoneal haematoma. We immediately turned the patient to his left side, and a right retro-peritoneal approach was done. Direct compression was applied on the site of the tear, evacuation of the haematoma and blood transfusion. Within 30 min, the vascular surgeon reached the operating room and successful repair of the arterial tear was done. The patient was saved but suffered from right lower limb mono-paresis immediate postoperative. Two weeks post-operatively, the patient suffered from discitis and retroperitoneal abscess. The patient was operated upon through the retro-peritoneal approach to evacuate the abscess and do curettage of disc space and insertion of irrigation suction system. The infection healed after 5 weeks, and the paresis improved within 2 months.
Two patients suffered from post-operative esophageal perforation as a complication of tracheostomy. The first one was managed conservatively at the start by insertion of nasogastric tube and total parenteral nutrition and antibiotics for 3 weeks which failed to control the infection. Under general anaesthesia, removal of plate and screws, insertion of suction-irrigation system and feeding gastrostomy were done. Despite of all these, the patient deteriorated till death occurred after 3 months from perforation. The second one was managed surgically from the start by direct esophageal repair by cardiothorathic team, insertion of irrigation-suction system and total parenteral nutrition for 25 days. Complete healing of infection was encountered in this patient without the need to remove the plate and screws.
In our study, we managed patients with post-operative superficial infections by re-hospitalization, radiological and laboratory investigations especially blood picture, C-reactive protein and culture and sensitivity from the wound. Maximum dose combination parenteral antibiotics according to results of culture and sensitivity were given for at least 2 weeks. Local application of Betadine and Rifamycin powder was done in all patients. Patients with deep infections were managed surgically by opening the surgical site, evacuation of the abscess, curettage of the disc space if no cage was present, removal of implants (only in 3 cases), extensive wash with betadine and saline, application of antibiotic powder and insertion of irrigation-suction system. Five hundred cubic centimeter normal saline with 1 g vancomycin and 80 mg gentamycin was infused through the irrigation system every 6 h and kept inside for 1 h then drained. These cycles of irrigation followed by suctions were repeated for at least 2 weeks. From the start, maximum dose combination-sensitive parenteral antibiotics were given for at least 1 month followed by intra-muscular and oral antibiotics for another 2 months. We faced one case with fungal discitis that need parenteral antifungal and antibiotics for 11 weeks followed by oral treatment for 3 months. We found that Staphylococcus aureus was the most common organism causing post-operative infection (Table 4).
Prophylactic measures directed for prevention of post spinal surgery infection were proved to decrease the incidence of infection by many authors. Our usual plan for prophylaxis is to follow these measures. These include sterile operating rooms, pre-operative microbial screening of patients and decolonization of any septic focus, glycemic control, smoking stoppage, antiseptic showers, pre-operative antibiotics, Betadine and saline irrigation at the surgical site and Vancomycin topical application [23,24,25]. Some authors used the peri-operative (intra-operative and post-operative) local antibiotics irrigation for 1–7 days and proved the decrease in the rate of post-operative infections [26,27,28].
Conclusion
Post spinal surgery infection is a devastating complication that needs multi-modalities for prevention and control. Neutralization of the pre-operative risk factors can dramatically reduce the post-operative infections. Once diagnosed, the patients with infection must be hospitalized and extensive management should be applied. Irrigation-suction application is a very effective and safe measure in treating infections, so the need to remove the implanted grafts is limited.
References
Smith JS, Shaffrey CI, Sansur CA, Berven SH, Fu KMG, Broadstone PA. Rates of infection after spine surgery based on 108,419 procedures. Spine. 2011;36:556–63.
Weinstein MA, McCabe JP, Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. Clin Spine Surg. 2000;13(5):422–6.
Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90:62–9.
Lim MR, Lee JY, Vaccaro AR. Surgical infections in the traumatized spine. Clin Orthop Relat Res. 2006;444:114–9.
Yang S, Werner BC, Cancienne JM, Hassanzadeh H, Shimer AL, Shen FH, et al. Preoperative epidural injections are associated with increased risk of infection after single-level lumbar decompression. Spine J. 2016;16:191–6.
Olsen MA, Mayfield J, Lauryssen C. Risk factors for surgical site infection in spinal surgery. J Neurosurg. 2003;98:149–55.
Chevalier J, Gremillard L. Ceramics for medical applications: a picture for the next 20 years. J Eur Ceram Soc. 2009;29:1245–55.
Thanni LO, Aigoro NO. Surgical site infection complicating internal fixation of fractures: incidence and risk factors. J Natl Med Assoc. 2004;96:1070–2.
Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783–805.
Mok JM, Guillaume TJ, Talu U, et al. Clinical outcome of deep wound infection after instrumented posterior spinal fusion: a matched cohort analysis. Spine (Phila Pa 1976). 2009;34:578–83.
Bekelis K, Desai A, Bakhoum SF, et al. A predictive model of complications after spine surgery: The National Surgical Quality Improvement Program (NSQIP) 2005–2010. Spine J. 2014;14:1247–55.
Shousha M, Cirovic D, Boehm H. Infection rate after minimally invasive noninstrumented spinal surgery based on 4350 procedures. Spine (Phila Pa 1976). 2015;40:201–5.
Kim BD, Smith TR, Lim S, et al. Predictors of unplanned readmission in patients undergoing lumbar decompression: multi-institutional analysis of 7016 patients. J Neurosurg Spine. 2014;20:606–16.
Schairer WW, Carrer A, Deviren V, et al. Hospital readmission after spine fusion for adult spinal deformity. Spine (Phila Pa 1976). 2013;38:1681–9.
Greene LR. Guide to the elimination of orthopedic surgery surgical site infections: an executive summary of the Association for Professionals in Infection Control and Epidemiology elimination guide. Am J Infect Control. 2012;40:384–6.
Cremet L, Corvec S, Bemer P, Bret L, Lebrun C, Lesimple B. Orthopaedic-implant infections by Escherichia coli: molecular and phenotypic analysis of the causative strains. J Inf Secur. 2012;64:169–75.
Chen TY, Anderson DJ, Chopra T, Choi Y, Schmader KE, Kaye KS. Poor functional status is an independent predictor of surgical site infections due to methicillin-resistant Staphylococcus aureus in older adults. J Am Geriatr Soc. 2010;58:527–32.
Henriksen NA, Meyhoff CS, Wetterslev J, Wille-Jorgensen P, Rasmussen LS, Jorgensen LN. Clinical relevance of surgical site infection as defined by the criteria of the Centers for Disease Control and Prevention. J Hosp Infect. 2010;75:173–7.
Senthilkumar S, Anitha C, Vignesh S, Shanmugapriya R, Cherian KM. Detection of biofilm formation and mecA gene from clinical isolates of Staphylococcus sp. Adv Biomed Pharma. 2014;1:21–6.
Jin SW, Kim SH, Choi JI, Ha SK, Lim DJ. Late infection from anterior cervical discectomy and fusion after twenty years. Korean J Spine. 2014;11:22–4. https://doi.org/10.14245/kjs.2014.11.1.22.
Basu S, Sreeramalingam R. Adjacent level spondylodiscitis after anterior cervical decompression and fusion. Indian J Orthop. 2012;46:360–3. https://doi.org/10.4103/0019-5413.96367.
Korovessis P, Repantis T, Vitsas V, Vardakastanis K. Cervical spondylodiscitis associated with oesophageal perforation: a rare complication after anterior cervical fusion. Eur J Orthop Surg Traumatol. 2013;23(suppl 2):S159–63. https://doi.org/10.1007/s00590-012-1092-y.
Tomov M, Mitsunaga L, Durbin-Johnson B, et al. Reducing surgical site infection in spinal surgery with betadine irrigation and intra-wound vancomycin powder. Spine (Phila Pa 1976). 2015. https://doi.org/10.1097/BRS.0000000000000789.
Kang DG, Holekamp TF, Wagner SC, Lehman RA. Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: a systematic literature review. Spine J. 2015. https://doi.org/10.1016/j.spinee.2015.01.030.
Caroom C, Tullar JM, Benton EG, et al. Intrawound vancomycin powder reduces surgical site infections in posterior cervical fusion. Spine (Phila Pa 1976). 2013;38:1183–7. https://doi.org/10.1097/BRS.0b013e31828fcfb5.
Godil SS, Parker SL, O’Neill KR, et al. Comparative effectiveness and cost-benefit analysis of local application of vancomycin powder in posterior spinal fusion for spine trauma: clinical article. J Neurosurg Spine. 2013;19:331–5.
Sweet FA, Roh M, Sliva C. Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions: efficacy, drug levels, and patient outcomes. Spine (Phila Pa 1976). 2011;36:2084–8.
Zebala LP, Chuntarapas T, Kelly MP, et al. Intrawound vancomycin powder eradicates surgical wound contamination: an in vivo rabbit study. J Bone Joint Surg (Am). 2014;96-A:46–51.
Acknowledgements
Not applicable.
Funding
The author received no specific funding for this work.
Availability of data and materials
Not applicable to this article as no data sets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Contributions
Not applicable. I am responsible for study design, manuscript writing, etc. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Ethical Committee of the Alexandria Faculty of Medicine with approval reference number of (0303820) dated 18/1/2018. Informed consent to participate in the study was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Eshra, M.A. Experience in the management of post-operative spinal infection. Egypt J Neurol Psychiatry Neurosurg 55, 9 (2019). https://doi.org/10.1186/s41983-019-0053-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-019-0053-3