Abstract
Liver cirrhosis, alcoholic liver diseases, non-alcoholic fatty liver and steatohepatitis are the major risk factors for liver damage leading to hepatocellular carcinoma. Oxidative stress and insulin resistance are the main pathogenetic mechanisms leading the hepatic cell injury and damage in these patients. The present review is the first attempt which focuses on the biological activities of Bergenia ciliata to explore its benefits and possible applications in the treatment of liver ailments. Bergenia ciliata is an evergreen herb belonging to the family saxifragaceae and is regarded as a miracle herb due to its wide medicinal applications. The data published in India and other nations are methodically reviewed and summarized in this article. It covers the facts collected from scientific journals, theses and online bibliographical databases: PubMed, Scopus, Google Scholar and Web of Science from year 1995–2020. The phytochemical studies on B. ciliata have shown the presence of many phytochemicals belonging to phenols, flavonoids, fatty acid, glycosides, terpenoids, etc. Due to the presence of a multitude of these bioactives, the whole plant of B. ciliata has numerous medicinal applications such as diuretic, antipyretic, α-glucosidase, antiviral, antibacterial, anti-inflammatory and insecticidal activity. Therefore in the present study, we invite the attention of scientists and researchers to carry out further clinical and toxicological studies on this valuable plant in order to discover and develop novel hepatoprotective medicine with fewer side effects on human beings.
Similar content being viewed by others
Background
Liver diseases continue to be a major health concern over the last few years due to chronic alcohol abuse and modern lifestyle, and cause of morbidity and mortality worldwide (Iqbal et al., 2019). Every year, 3 million deaths occur due to alcohol consumption all over the world (WHO, 2019). At the same time, NAFLD is emerging even larger health problem and is considered to be the most common liver disease. A significant number of individuals are developing non-alcoholic steatohepatitis (NASH) which may progress toward hepatic fibrosis, cirrhosis and ultimately hepatocellular carcinoma (Ahmad & Ahmad, 2012; Page & Harrison, 2009). Approximately one-third of the population in developed countries have NAFLD responsible for liver transplantation (Angulo, 2006; Mikolasevic et al., 2018). Hepatitis B and C virus infections, like ALD and NAFLD, cause chronic liver disease (Raimondo et al., 2005). Due to lack of any effective treatment and increase in the number of cases of cirrhosis and in need of liver transplantation, chronic liver diseases are important health and economic concern. Therefore, there is a need of effective and affordable treatment modalities to reduce the morbidity and mortality associated with CLDs.
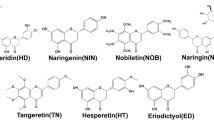
Herbal remedies are highly valued all over the world as a rich source of pharmaceutical agents for the prevention of infections and diseases (Kayani et al., 2014; Latief & Ahmad, 2018; Zain-ul-Abidin et al., 2018). In India, there are enormous varieties of medicinal plants; thus, our country has often been referred as ‘Medicinal Garden of the world’. These plants have played vital roles in various ancient traditional systems of medication and even today, provide an inexpensive source of drugs for majority of world’s population (Sen & Chakraborty, 2017). Bergenia ciliata (family Saxifragaceae), a highly valuable plant has been used as a medicine for the treatment of different kinds of human diseases since long. It is commonly called ‘Zakhmehayat’ or ‘Pakhanabhed’ and is an evergreen perennial herb, widely distributed in Central and East Asia (Phull et al., 2016; Tiwari et al., 2020). This plant has thick rootstock, and outer surface is dark brown and rough whereas the inner skin is pinkish and smooth. It is covered with dark sheaths of withered leaves. Flowers are arranged in terminal corymbs and may be pink, white or purple. In Himalayan region, people traditionally use B. ciliata for the treatment of various ailments (Chowdhary et al., 2009). Bergenia ciliata is considered as a miracle herb due to its use in treatment of numerous diseases such as gastrointestinal problems, pulmonary infections, heart diseases, ophthalmic, hemorrhoids, kidney and gall bladder stones. (Hussain et al., 2019; Rajkumar et al., 2011). In addition, it is accredited with antifungal, diuretic, antitussive, anticancer, analgesic, antiviral, antibacterial, anti-inflammatory and antimalarial properties (Rajkumar et al., 2011; Ruby et al., 2012; Timalsena & Lamichhane, 2019; Zafar et al., 2019). In India, an Ayurvedic polyherbal formulation ‘Cystone’ contains Bergenia in combination with other plants and is used against urolithiasis (Vidyashankar et al., 2010). These virtues of the plant are attributed directly to its phytochemicals composition and account for its utilization in traditional medicine (Fig. 1).
Phytochemical studies on this plant have revealed the presence of gallic acid (3,4,5 trihydroxybenzoic acid), bergenin (C-glycoside of 4-O-methyl Gallic acid), catechin, gallicin, paashaanolactone, arbutin, β-sitosterol, afzelechin, etc. (Dharmender et al., 2010; Kanth et al., 2019). Tannic acid, mucilage, glucose, albumen, metarbin, mineral salts and wax are also reported to be present (Kanth et al., 2019). Extensive examination of medicinal plants for bioactive compounds and biological activities is the foremost and critical step in development of effective novel medications. In view of this, the present review is the first attempt to gather utmost fragmented literature showing the protective effects of various bioactive compounds of B. ciliata against liver diseases. It will improve the efficacy of this miracle herb against liver infirmities, as well as the active medicinal compounds responsible for them. Furthermore, this article would unfurl logical holes in existing knowledge and make it easier for researchers all over the world to approach studies relating to the discovery of novel compounds and medicines from B. ciliata.
Methodology
This review article has been designed by compiling and consulting published papers about the protective efficacy and scientific validation of Bergenia ciliata as an anti-hepatotoxic agent. Published papers were retrieved from scientific journals, theses and online bibliographical databases: PubMed, Scopus, Google Scholar and Web of Science. In total, almost 100 research articles on B. ciliata plant and its phytochemicals published in English language were reviewed for this article. Inside the databases, we used the keywords including: liver diseases, hepatoprotective activity, Bergenia ciliata, pharmacology, phytochemicals, bergenin, gallic acid, arbutin, tannic acid, β-sitosterol, limonene and β-caryophyllene. All the obtained data from previous published literature is summarized in three figures and two table.
Phytochemical constituents
Phytochemical studies include identification and isolation of the chemical compounds, determination of their biological effectiveness through in vitro and in vivo studies in experimental models and through epidemiological and clinical trials in humans. The phytochemical constituents of Bergenia species are summarized in Table 1.
Therapeutic activities of phytochemicals of Bergenia ciliata against liver diseases
Gallic acid
Gallic acid (GA) is an important phytochemical of B. ciliata and is also found in tea leaves, sumac, oak bark, gallnuts, witch hazel and other kinds of plants (Nabavi et al., 2012). Studies have shown that GA possesses a lot of biological activities such as antiviral antibiotic, anti-inflammatory, antimutagenic and anticancer (Badhani et al., 2015; Kahkeshani et al., 2019). These effects are due to the fact that GA is a potent antioxidant, involved in neutralizing and absorbing free radicals produced by the cells (Badhani et al., 2015).
It is reported that gallic acid has protective activity against hepatotoxicity due to its hydroxyl groups (Anand et al., 1997). Several previous studies have revealed the efficacy of GA on hepatic injury caused by different etiologies, such as cyclophosphamide, paracetamol, diethylnitrosamine, carbon tetrachloride, lindane and methotrexate. (Latief et al., 2016; Oyagbemi et al., 2016; Padma et al., 2011; Safaei et al., 2018; Wang et al., 2014). GA attenuated on hepatic injury and hepatic fibrosis induced by these chemicals in rodent models, which might be due to inhibition of inflammation, oxidative stress and hepatic stellate cell (HSC) activity. The ameliorative effect of GA on hepatic glycoprotein components and lipid peroxidation in the streptozotocin-induced diabetic rats has also been found (Punithavathi et al., 2011). Gallic acid treatment was found to reverse the disturbed metabolism to its normal condition in a mice model with non-alcoholic fatty liver disease (Chao et al., 2014). Results indicated that the potential targets of GA were lipid metabolism and ketogenesis, amino acids metabolism, choline metabolism, glycolysis and gut-microbiota metabolism. GA improved lipid metabolism and glucose tolerance in obese mice, thereby showing evidence of anti-hyperglycemic activity (Bak et al., 2013). This was due to improved triglyceride concentrations and induced PPAR-γ and Akt activations, thus improving the glucose metabolism. Gallic acid was found active on chronic ethanol-induced liver injury in rats by decreasing the serum alanine aminotransferase, aspartate aminotransferase and lactate dehydrogenase activities and elevating paraoxonase and arylesterase activity (Kartkaya et al., 2013). GA suppressed ethanol-induced necroptosis in hepatocytes by reducing the expression of distinct necroptotic signals receptor-interacting protein 1 (RIP1) and RIP3, as well as the release of high mobility group box protein 1 (Zhou et al., 2019). It also increased the expression of NrF2, which served as a molecular basis for suppressing ethanol-induced hepatocyte necroptosis. Thus, NrF2, a classical antioxidant protein, is a newly identified crucial suppressor for necroptosis. It has been reported that GA attenuated hepatitis C virus infection in hepatoma cells through its antioxidant and antiviral production (Govea-Salas et al., 2016; Hsu et al., 2015). It was also reported that GA decreased DEN-induced HCC by diminishing expression of proliferative marker PCNA and regulating signal transducer and activator of transcription 3 (STAT 3) signaling pathway (Aglan et al., 2017; Jagan et al., 2008). This was due to its high bioactivity, which included antioxidant, anti-inflammatory, apoptotic and antitumor properties. GA was able to inhibit liver metastasis of mastocytoma cells P-815 (Ohno et al., 2001).
Bergenin
Bergenin (C14H16O9) is a natural secondary metabolite isolated from the herb Bergenia ciliata, and it is reported that rhizome of B. ciliata contains 0.75% bergenin (Ahmad et al., 2018a, 2018b, 2018c). It is an isocoumarin compound extracted from the leaves, roots and bark of many families and genera of plants (Patel et al., 2012). It exhibits anti-inflammatory, antiarrhythmic, antitussive, antifungal, anticancer, antitumor, antiviral, immune enhancement, wound repair, anticoagulant, analgesic, antidiabetic, neuroprotective, antimalarial and antioxidant properties (Aggarwal et al.,; 2016; Ahmed & Urooj, 2012; Bajracharya, 2015; Bessong et al., 2005; Patel et al., 2012). It is reported that there are no side effects of bergenin even in very high dosages (Chauhan et al., 2012).
It was found that liver injury altered the pharmacokinetic behavior of bergenin and enhanced its absorption after given orally (Rong-Hua et al., 2016). These findings provided valuable information for the study of clinical pharmacokinetics of bergenin under hepatic injury condition and guidance for the potential use of bergenin as a hepatoprotective agent. It is reported that bergenin exerted hepatic protection in hepatic ischemia reperfusion (IR) injury model (Xiang et al., 2020). The protective action of bergenin was due to its ability to eliminate reactive oxygen species (ROS), influence the release of inflammatory factors, apoptosis and autophagy-related genes via the PPAR pathway. In a recent study, it was found that bergenin acted as a promising drug candidate for abrogating hepatic fibrosis induced by carbon tetrachloride and bile duct ligation (Xia et al., 2020). Bergenin retarded autophagy and hindered the energy supply required for HSC activation, thereby reducing collagen deposition and hepatocyte damage. Bergenin and metformin helped with hepatic hyperglycemia, insulin sensitivity and glucose uptake (Ambika & Saravanan, 2016). These phytochemicals increased the activity of glycolytic enzymes and significantly decreased the gluconeogenic enzymes in diabetic mice. Under diabetic conditions, this facilitated the release of hepatic glucose into circulation. Bergenin and metformin regulated the activities of these enzymes through metabolic activation or inhibition of glycolysis and gluconeogenesis, respectively. Bergenin improved insulin signalling in the liver of HFD-fed mice by increasing the tyrosine phosphorylation of IR-β and IRS-1, improving PI3K/Akt activation and glucose transporter protein 2 (GLUT 2) translocation. Thus, this phytochemical may be used to treat obesity-related type 2 diabetes mellitus as it enhanced insulin-dependent glucose transport in hepatic tissues by activating and translocating GLUT 2 in a PI3K/phosphorylated protein kinase B (AKT) dependent pathway. Bergenin was also effective against alcohol and tert-butyl hydroperoxide (TBHP)-induced liver injury in hepatoma cells (Sriset et al., 2020). It exhibited hepatoprotective activity via restoration of oxidant-antioxidant system and thus a potential candidate for hepatoprotective treatment.
β-Sitosterol
β-Sitosterol (BSS) is a plant derived natural dietary phytosterol similar to cholesterol. It is present in B. ciliata roots and leaves and in many oils from plants and vegetables (Manjunatha, 2010). β-Sitosterol has a wide spectrum of therapeutic effects against various chronic ailments (Yuan et al., 2019). According to reports, this phytosterol shows various types of health benefits against oxidative stress, obesity, anxiety, diabetes, cancer, sedative and prostatauxe effects (Baskar et al., 2012; Berges et al., 1995; Gumede et al., 2020; Jenkins et al., 2003; López-Rubalcava et al., 2006; Normén et al., 2001).
Treatment with BSS showed dose-dependent hepatoprotective effect against CCl4-induced chronic liver diseases (Devaraj et al., 2020). Its treatment inhibited ROS by causing diminution of intracellular enzymatic antioxidants such as superoxide dismutase and catalase in the rat liver. It also significantly reduced the expression of HSCs activation markers (hydroxyproline, collagen, α-SMA, desmin, vimentin, and MMP 9), thus exhibiting antifibrotic action. BSS has radio-protective effect via regulating the gene expression of PPAR-γ which in turn cause rise in PON-1 and ARE enzymes activities (Moustafa & Thabet, 2017). This action of BSS was due to its antioxidant potential, cholesterol reduction and PPAR-γ agonist properties. Another study indicated that BSS and its derivatives restrained LPS/ GalN-induced liver injury by inhibiting the oxidation and inflammation in mice (Yin et al., 2018). Their treatment regulated antioxidant status through the Nrf2 activation, heme oxygenase-1 (HO-1) promotion and controlling anti-inflammatory pathway through the toll like receptor 4 (TLR4) inhibition. It is reported that β-sitosterol in combination with stigmasterol acted against high-fat Western diet (HFWD)-induced NAFLD (Feng et al., 2018). Lipidomic analyses conducted in liver samples collected after thirty three weeks of the treatment have revealed the potency of these phytochemicals against NAFLD. Thus, these phytosterols serve as future candidates for human NAFLD by reducing plasma cholesterol levels (Table 2).
Other phytochemicals
Other phytochemicals found in B. ciliata are arbutin, tannic acid, fatty acids, terpenes, etc. Arbutin, a glycosylated form of hydroquinone is found in rhizome of B. ciliata and other green plants, is often used in various skin diseases (Khanal et al., 2011; Kunwar et al., 2013). It is also effective in repulsion of kidney stones as it possesses antibacterial properties, and heal cystitis and urinary tract infections (Funayama et al., 1995). It was found that arbutin mitigated tert-butyl hydroperoxide-induced toxicity in Hep-G2 cell line (Seyfizadeh et al., 2012). Reports showed that arbutin may protect the liver against cyclosporine and CCl4-induced oxidative damage in rats (Khadir et al., 2015; Mirshahvalad et al., 2016). This hepatoprotective effect was correlated with the antioxidant, lipoperoxidative and free radical scavenger effects of arbutin. Another finding demonstrated that arbutin is a strong radio-protector for reducing the radiation damage in megavoltage therapeutic x-irradiated mice (Nadi et al., 2019). Thus, arbutin may be used as an antioxidant to protect against oxidative damage induced by toxic chemicals and radiations on liver. Tannic acid (TA) is another polyphenol present in B. ciliata and in several fruits and vegetables (Ahmad et al., 2018a, 2018b, 2018c; Fraga-Corral et al., 2020). This compound possesses strong antimicrobial, antioxidant, antiviral, antibacterial and astringent properties, reduces serum cholesterol and triglycerides, and suppresses lipogenesis (Chung et al., 1998; Kaczmarek, 2020). TA exerted significant liver-protective effects against CCl4- and acetaminophen-induced liver damage and fibrosis in mice (Chu et al., 2016; Zhang et al., 2017). The potential mechanism relied on the inhibition of collagen accumulation, antioxidation, anti-inflammation and antiapoptosis.
Limonene is a monoterpene found in the numerous medicinal plants including rhizome of B. ciliata and citrus fruits (Adhikary et al., 2011; Kumar et al., 2010; Peng et al., 2009). It is a colorless liquid and exists in two optical isomers, d- or l-limonene as well as a racemic mixture (Vieira et al., 2018). d-Limonene is reported to have a variety of pharmaceutical applications such as anticancer, antioxidant and anti-inflammatory (Khan et al., 2013; Roberto et al., 2009). It has been reported that d-Limonene is effective against CCl4-induced hepatic fibrosis in Wistar rats via reducing oxidative stress and inflammation (Ahmad et al., 2018). It boosted the antioxidant status, regulated collagen accumulation and inhibited inflammation through ameliorating NF-κB. Another study demonstrated that d-Limonene reduced the oxidative stress in streptozotocin-induced diabetic rats by decreasing lipid peroxidation and restoring the activities of antioxidant enzymes (Murali et al., 2012). d-Limonene supplementation also ameliorated the NAFLD in rats and thus could serve as a promising complementary therapy against metabolic syndrome associated with NAFLD (Santiago et al., 2012). It is found that limonene inhibited experimental hepatocarcinogenesis in rat model via increased apoptosis and decreased cell proliferation (Kaji et al., 2001). Another terpene found in B. ciliata rhizome is β-caryophyllene, a bicyclic sesquiterpene, also a major component of essential oils of food plants such as cinnamon, cloves, black pepper and rosemary (Calleja et al., 2013; Jayaprakasha et al., 2003; Varga et al., 2018). This terpenoid is found to reduce CCl4-mediated hepatic fibrosis and hepatic cell activation by declining the gene expressions of Collagen-1α1, TGF-β1 and TIMP1 (Calleja et al., 2013). It is reported that β-caryophyllene ameliorated alcoholic and non-alcoholic steatohepatitis in experimental mice by regulating the activities of various inflammatory markers and antioxidant enzymes (Arizuka et al., 2017; Varga et al., 2018) (Fig. 2).
Conclusions
The present review gathers the detailed information about the hepatoprotective potential of Bergenia ciliata for the first time. Almost all parts of the plant are used for curing different ailments; the most frequent part used is rhizome followed by root, leaf, flower and latex. The major phytochemical compounds reported in this species are of wide range phenols, flavonoids, fatty acid, glycosides, terpenoids, etc. These phytochemicals exhibit various biological activities including antibacterial, antioxidants, antifungal, antihemolytic and cytotoxic and had been traditionally used among the various communities particularly across the Himalayan region for urinary, gastrointestinal, skin, respiratory, gynecological, inflammatory, kidney disorders and infectious diseases. The techniques of HPLC, NMR, and FTIR can be used to characterize, isolate, and quantify these phytochemicals (Ahmad et al., 2018a, 2018b, 2018c; Majeed et al., 2021). Bergenin, the most abundant phytochemical, may be isolated and studied further in preclinical and clinical studies, allowing researchers to gain a better understanding of its nature and function in order to develop novel treatments for liver illnesses in near future. The antioxidant and hepatoprotective properties of the crude extract and subfractions can also be investigated. Based on the experimental evidences in the current review, Bergenia ciliata is considered is one of the most important anti-hepatotoxic agent which is attributed to its phytochemical constituents. But there is a dire need for further experimental investigations for its use as an antifibrotic and hepatoprotective agents as deficiency in clinical trials has been observed. Therefore, for the future discovery of it as liver medicine, it is necessary to conduct additional clinical studies on this plant. These clinical trials should be conducted to test the efficiency of this plant for its clinical uses along with its safety profit. The outcome of research in these areas will give convincing support for clinical use of B. ciliata in modern medicine in near future. Moreover, the plant has also lesser side effects on living organisms as compared to modern medicines (Fig. 3).
Availability of data and materials
Not applicable.
Abbreviations
- CLDs:
-
Chronic liver diseases
- GA:
-
Gallic acid
- BSS:
-
β-Sitosterol
- LPS:
-
Lipopolysaccharide
- GalN:
-
d-Galactosamine
- PI3K:
-
Phosphatidylinositol 3-kinase
- IR:
-
Insulin receptor
References
Adhikary, P., Roshan, K. C., Kayastha, D., Thapa, D., Shrestha, R., Shrestha, T. M., & Gyawali, R. (2011). Phytochemical screening and anti-microbial properties of medicinal plants of Dhunkharka community, Kavrepalanchowk, Nepal. International Journal of Pharmaceutical and Biological Archives, 2(6), 1663–1667.
Aggarwal, D., Gautam, D., Sharma, M., & Singla, S. K. (2016). Bergenin attenuates renal injury by reversing mitochondrial dysfunction in ethylene glycol induced hyperoxaluric rat model. European Journal of Pharmacology, 791, 611–621.
Aglan, H. A., Ahmed, H. H., El-Toumy, S. A., & Mahmoud, N. S. (2017). Gallic acid against hepatocellular carcinoma: An integrated scheme of the potential mechanisms of action from in vivo study. Tumor Biology, 39(6), 1010428317699127.
Ahmad, A., & Ahmad, R. (2012). Understanding the mechanism of hepatic fibrosis and potential therapeutic approaches. Saudi Journal of Gastroenterology, 18(3), 155–167.
Ahmad, M., Butt, M. A., Zhang, G., Sultana, S., Tariq, A., & Zafar, M. (2018). Bergenia ciliata: A comprehensive review of its traditional uses, phytochemistry, pharmacology and safety. Biomedicine and Pharmacotherapy, 97, 708–721.
Ahmad, M., Malik, K., Tariq, A., Zhang, G., Yaseen, G., Rashid, N., Sultana, S., Zafar, M., Ullah, K., & Khan, M. P. Z. (2018). Botany, ethnomedicines, phytochemistry and pharmacology of Himalayan paeony (Paeonia emodi Royle.). Journal of Ethnopharmacology, 220, 197–219.
Ahmad, S. B., Rehman, M. U., Fatima, B., Ahmad, B., Hussain, I., Ahmad, S. P., Farooq, A., Muzamil, S., Razzaq, R., Rashid, S. M., & Ahmad Bhat, S. (2018). Antifibrotic effects of d-limonene (5 (1-methyl-4-[1-methylethenyl]) cyclohexane) in CCl4 induced liver toxicity in Wistar rats. Environmental Toxicology, 33(3), 361–369.
Ahmed, F., & Urooj, A. (2012). Cardioprotective activity of standardized extract of Ficus racemosa stem bark against doxorubicin-induced toxicity. Pharmaceutical Biology, 50(4), 468–473.
Ambika, S., & Saravanan, R. (2016). Effect of bergenin on hepatic glucose metabolism and insulin signaling in C57BL/6J mice with high fat-diet induced type 2 diabetes. Journal of Applied Biomedicine, 14(3), 221–227.
Anand, K. K., Singh, B., Saxena, A. K., Chandan, B. K., Gupta, V. N., & Bhardwaj, V. (1997). 3, 4, 5-Trihydroxy benzoic acid (gallic acid), the hepatoprotective principle in the fruits ofterminalia belerica-bioassay guided activity. Pharmacological Research, 36(4), 315–321.
Angulo, P. (2006). Nonalcoholic fatty liver disease and liver transplantation. Liver Transplantation, 12(4), 523–534.
Arizuka, N., Murakami, T., & Suzuki, K. (2017). The effect of β-caryophyllene on nonalcoholic steatohepatitis. Journal of Toxicologic Pathology, 30(4), 263–273.
Badhani, B., Sharma, N., & Kakkar, R. (2015). Gallic acid: A versatile antioxidant with promising therapeutic and industrial applications. RSC Advances, 5(35), 27540–27557.
Bajracharya, G. B. (2015). Diversity, pharmacology and synthesis of bergenin and its derivatives: Potential materials for therapeutic usages. Fitoterapia, 101, 133–152.
Bak, E. J., Kim, J., Jang, S., Woo, G. H., Yoon, H. G., Yoo, Y. J., & Cha, J. H. (2013). Gallic acid improves glucose tolerance and triglyceride concentration in diet-induced obesity mice. Scandinavian Journal of Clinical and Laboratory Investigation, 73(8), 607–614.
Baskar, A. A., Al Numair, K. S., Gabriel Paulraj, M., Alsaif, M. A., Muamar, M. A., & Ignacimuthu, S. (2012). β-Sitosterol prevents lipid peroxidation and improves antioxidant status and histoarchitecture in rats with 1, 2-dimethylhydrazine-induced colon cancer. Journal of Medicinal Food, 15(4), 335–343.
Berges, R. R., Windeler, J., Trampisch, H. J., Senge, T. H., β-Sitosterol Study Group. (1995). Randomised, placebo-controlled, double-blind clinical trial of β-sitosterol in patients with benign prostatic hyperplasia. The Lancet, 345(8964), 1529–1532.
Bessong, P. O., Obi, C. L., Andréola, M. L., Rojas, L. B., Pouységu, L., Igumbor, E., Meyer, J. M., Quideau, S., & Litvak, S. (2005). Evaluation of selected South African medicinal plants for inhibitory properties against human immunodeficiency virus type 1 reverse transcriptase and integrase. Journal of Ethnopharmacology, 99(1), 83–91.
Calleja, M. A., Vieites, J. M., Montero-Meterdez, T., Torres, M. I., Faus, M. J., Gil, A., & Suárez, A. (2013). The antioxidant effect of β-caryophyllene protects rat liver from carbon tetrachloride-induced fibrosis by inhibiting hepatic stellate cell activation. British Journal of Nutrition, 109(3), 394–401.
Chao, J., Huo, T. I., Cheng, H. Y., Tsai, J. C., Liao, J. W., Lee, M. S., Qin, X. M., Hsieh, M. T., Pao, L. H., & Peng, W. H. (2014). Gallic acid ameliorated impaired glucose and lipid homeostasis in high fat diet-induced NAFLD mice. PLoS ONE, 9(6), e96969.
Chauhan, R., Ruby, K., & Dwivedi, J. (2012). Bergenia ciliata mine of medicinal properties: A review. International Journal of Pharmaceutical Sciences Review and Research, 15(2), 20–23.
Chowdhary, S., Verma, D., & Kumar, H. (2009). Biodiversity and traditional knowledge of Bergenia spp. in Kumaun Himalaya. New York Science Journal, 2(6), 105–108.
Chu, X., Wang, H., Jiang, Y. M., Zhang, Y. Y., Bao, Y. F., Zhang, X., Zhang, J. P., Guo, H., Yang, F., Luan, Y. C., & Dong, Y. S. (2016). Ameliorative effects of tannic acid on carbon tetrachloride-induced liver fibrosis in vivo and in vitro. Journal of Pharmacological Sciences, 130(1), 15–23.
Chung, K. T., Wong, T. Y., Wei, C. I., Huang, Y. W., & Lin, Y. (1998). Tannins and human health: A review. Critical Reviews in Food Science and Nutrition, 38(6), 421–464.
Devaraj, E., Roy, A., Veeraragavan, G. R., Magesh, A., Sleeba, A. V., Arivarasu, L., & Parasuraman, B. M. (2020). β-Sitosterol attenuates carbon tetrachloride–induced oxidative stress and chronic liver injury in rats. Naunyn-Schmiedeberg’s Archives of Pharmacology, 393, 1067–1075.
Dharmender, R., Madhavi, T., Reena, A., & Sheetal, A. (2010). Simultaneous quantification of Bergenin, (+)-Catechin, Gallicin and Gallic acid; and quantification of β-Sitosterol using HPTLC from Bergenia ciliata (Haw.) Sternb. Forma ligulata Yeo (Pasanbheda). Pharmaceutica Analytica Acta, 1, 104.
Feng, S., Dai, Z., Liu, A. B., Huang, J., Narsipur, N., Guo, G., Feng, S., Dai, Z., Liu, A. B., Huang, J., Narsipur, N., Guo, G., Kong, B., Reuhl, K., Lu, W., Luo, Z., & Yang, C. S. (2018). Intake of stigmasterol and β-sitosterol alters lipid metabolism and alleviates NAFLD in mice fed a high-fat western-style diet. Biochimica Et Biophysica Acta (BBA)-Molecular and Cell Biology of Lipids, 1863(10), 1274–1284.
Fraga-Corral, M., García-Oliveira, P., Pereira, A. G., Lourenço-Lopes, C., Jimenez-Lopez, C., Prieto, M. A., & Simal-Gandara, J. (2020). Technological application of tannin-based extracts. Molecules, 25(3), 614.
Funayama, M., Arakawa, H., Yamamoto, R., Nishino, T., Shin, T., & Murao, S. (1995). Effects of α-and β-arbutin on activity of tyrosinases from mushroom and mouse melanoma. Bioscience, Biotechnology, and Biochemistry, 59(1), 143–144.
Govea-Salas, M., Rivas-Estilla, A. M., Rodríguez-Herrera, R., Lozano-Sepúlveda, S. A., Aguilar-Gonzalez, C. N., Zugasti-Cruz, A., Salas-Villalobos, T. B., & Morlett-Chávez, J. A. (2016). Gallic acid decreases hepatitis C virus expression through its antioxidant capacity. Experimental and Therapeutic Medicine, 11(2), 619–624.
Gumede, N. M., Lembede, B. W., Brooksbank, R. L., Erlwanger, K. H., & Chivandi, E. (2020). β-Sitosterol shows potential to protect against the development of high-fructose diet-induced metabolic dysfunction in female rats. Journal of Medicinal Food, 23(4), 367–374.
Harb, A. A., Bustanji, Y. K., & Abdalla, S. S. (2018). Hypocholesterolemic effect of β-caryophyllene in rats fed cholesterol and fat enriched diet. Journal of Clinical Biochemistry and Nutrition, 62(3), 230–237.
Hsu, C. L., & Yen, G. C. (2007). Effect of gallic acid on high fat diet-induced dyslipidaemia, hepatosteatosis and oxidative stress in rats. British Journal of Nutrition, 98(4), 727–735.
Hsu, W. C., Chang, S. P., Lin, L. C., Li, C. L., Richardson, C. D., Lin, C. C., & Lin, L. T. (2015). Limonium sinense and gallic acid suppress hepatitis C virus infection by blocking early viral entry. Antiviral Research, 118, 139–147.
Hussain, A., Kanth, M., Shrivastva, P. K., Sharma, M., Tripath, J., & Khan, M. A. (2019). Phytochemical analysis of the rhizomes of Bergenia ciliata (How) Sternb. Journal of Drug Delivery and Therapeutics, 9(3), 412–416.
Iqbal, U., Perumpail, B. J., Akhtar, D., Kim, D., & Ahmed, A. (2019). The epidemiology, risk profiling and diagnostic challenges of nonalcoholic fatty liver disease. Medicines, 6(1), 41.
Jagan, S., Ramakrishnan, G., Anandakumar, P., Kamaraj, S., & Devaki, T. (2008). Antiproliferative potential of gallic acid against diethylnitrosamine-induced rat hepatocellular carcinoma. Molecular and Cellular Biochemistry, 319(1), 51–59.
Jayaprakasha, G. K., Jagan Mohan Rao, L., & Sakariah, K. K. (2003). Volatile constituents from Cinnamomum zeylanicum fruit stalks and their antioxidant activities. Journal of Agricultural and Food Chemistry, 51(15), 4344–4348.
Jenkins, D. J., Kendall, C. W., Marchie, A., Jenkins, A. L., Augustin, L. S., Ludwig, D. S., Barnard, N. D., & Anderson, J. W. (2003). Type 2 diabetes and the vegetarian diet. The American Journal of Clinical Nutrition, 78(3), 610S-616S.
Kaczmarek, B. (2020). Tannic acid with antiviral and antibacterial activity as a promising component of biomaterials—A minireview. Materials, 13(14), 3224.
Kahkeshani, N., Farzaei, F., Fotouhi, M., Alavi, S. S., Bahramsoltani, R., Naseri, R., Momtaz, S., Abbasabadi, Z., Rahimi, R., Farzaei, M. H., & Bishayee, A. (2019). Pharmacological effects of gallic acid in health and diseases: A mechanistic review. Iranian Journal of Basic Medical Sciences, 22(3), 225–237.
Kaji, I., Tatsuta, M., Iishi, H., Baba, M., Inoue, A., & Kasugai, H. (2001). Inhibition by d-limonene of experimental hepatocarcinogenesis in Sprague-Dawley rats does not involve p21ras plasma membrane association. International Journal of Cancer, 93(3), 441–444. https://doi.org/10.1002/ijc.1353
Kanth, M., Hussain, A., Shrivastva, P. K., Sharma, M., Tripath, J., & Khan, M. A. (2019). Extraction, qualitative and quantitative determination of secondary metabolites of Bergenia ciliata (How) sternb rhizome. Journal of Drug Delivery and Therapeutics, 9(3), 407–411.
Karimi-Khouzani, O., Heidarian, E., & Amini, S. A. (2017). Anti-inflammatory and ameliorative effects of gallic acid on fluoxetine-induced oxidative stress and liver damage in rats. Pharmacological Reports, 69(4), 830–835.
Kartkaya, K., Oğlakçı, A., Şentürk, H., Bayramoğlu, G., Canbek, M., & Kanbak, G. (2013). Investigation of the possible protective role of gallic acid on paraoxanase and arylesterase activities in livers of rats with acute alcohol intoxication. Cell Biochemistry and Function, 31(3), 208–213.
Kayani, S., Ahmad, M., Zafar, M., Sultana, S., Khan, M. P. Z., Ashraf, M. A., Hussain, J., & Yaseen, G. (2014). Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies-Abbottabad, Northern Pakistan. Journal of Ethnopharmacology, 156, 47–60.
Khadir, F., Pouramir, M., Joorsaraee, S. G., Feizi, F., Sorkhi, H., & Yousefi, F. (2015). The effect of arbutin on lipid peroxidation and antioxidant capacity in the serum of cyclosporine-treated rats. Caspian Journal of Internal Medicine, 6(4), 196–200.
Khan, A. Q., Khan, R., Qamar, W., Lateef, A., Rehman, M. U., Tahir, M., Ali, F., Hamiza, O. O., Hasan, S. K., & Sultana, S. (2013). Geraniol attenuates 12-O-tetradecanoylphorbol-13-acetate (TPA)-induced oxidative stress and inflammation in mouse skin: Possible role of p38 MAP Kinase and NF-κB. Experimental and Molecular Pathology, 94(3), 419–429.
Khanal, T., Kim, H. G., Hwang, Y. P., Kong, M. J., Kang, M. J., Yeo, H. K., Kim, D. H., Jeong, T. C., & Jeong, H. G. (2011). Role of metabolism by the human intestinal microflora in arbutin-induced cytotoxicity in HepG2 cell cultures. Biochemical and Biophysical Research Communications, 413(2), 318–324.
Koul, B., Kumar, A., Yadav, D., & Jin, J. O. (2020). Bergenia genus: Traditional uses, phytochemistry and pharmacology. Molecules, 25(23), 5555.
Kumar, P. M., Sasmal, D., & Mazumder, P. M. (2010). The antihyperglycemic effect of aerial parts of Salvia splendens (scarlet sage) in streptozotocin-induced diabetic-rats. Pharmacognosy Research, 2(3), 190–194.
Kunwar, R. M., Mahat, L., Acharya, R. P., & Bussmann, R. W. (2013). Medicinal plants, traditional medicine, markets and management in far-west Nepal. Journal of Ethnobiology and Ethnomedicine, 9(1), 1–10.
Latief, U., & Ahmad, R. (2018). Herbal remedies for liver fibrosis: A review on the mode of action of fifty herbs. Journal of Traditional and Complementary Medicine, 8(3), 352–360.
Latief, U., Husain, H., Mukherjee, D., & Ahmad, R. (2016). Hepatoprotective efficacy of gallic acid during Nitrosodiethylamine-induced liver inflammation in Wistar rats. Journal of Basic and Applied Zoology, 76, 31–41.
López-Rubalcava, C., Piña-Medina, B., Estrada-Reyes, R., Heinze, G., & Martínez-Vázquez, M. (2006). Anxiolytic-like actions of the hexane extract from leaves of Annona cherimolia in two anxiety paradigms: Possible involvement of the GABA/benzodiazepine receptor complex. Life Sciences, 78(7), 730–737.
Majeed, S., Zafar, M., Ahmad, M., Ozdemir, F. A., Kilic, O., Hamza, M., Sultana, S., Yaseen, G., & Raza, J. (2021). Ethnobotany, medicinal utilization and systematics of opuntia species from deserts of Pakistan. In M. F. Ramadan, T. E. M. Ayoub, & S. Rohn (Eds.), Opuntia spp.: Chemistry, bioactivity and industrial applications (pp. 49–80). Springer.
Manjunatha, S. N. (2010). Pharmacognostic finger print profile of a controversial drug Pashana Bedha (Doctoral dissertation).
Mikolasevic, I., Filipec-Kanizaj, T., Mijic, M., Jakopcic, I., Milic, S., Hrstic, I., Sobocan, N., Stimac, D., & Burra, P. (2018). Nonalcoholic fatty liver disease and liver transplantation—Where do we stand? World Journal of Gastroenterology, 24(14), 1491–1506.
Mirshahvalad, S., Feizi, F., Barkhordar, A., Bahadoram, M., Houshmand, G., & Pouramir, M. (2016). Hepatoprotective effects of arbutin against liver damage induced by carbon tetrachloride in rats. Jundishapur Journal of Natural Pharmaceutical Products, 11(3), e33392.
Moustafa, E. M., & Thabet, N. M. (2017). Beta-sitosterol upregulated paraoxonase-1 via peroxisome proliferator-activated receptor-γ in irradiated rats. Canadian Journal of Physiology and Pharmacology, 95(6), 661–666.
Murali, R., Karthikeyan, A., & Saravanan, R. (2012). Protective effects of d-limonene on lipid peroxidation and antioxidant enzymes in streptozotocin-induced diabetic rats. Basic and Clinical Pharmacology and Toxicology, 112(3), 175–181.
Nabavi, S. F., Habtemariam, S., Jafari, M., Sureda, A., & Nabavi, S. M. (2012). Protective role of gallic acid on sodium fluoride induced oxidative stress in rat brain. Bulletin of Environmental Contamination and Toxicology, 89(1), 73–77.
Nadi, S., Elahi, M., Moradi, S., & Banaei, A. (2019). Radioprotective effect of arbutin in megavoltage therapeutic X-irradiated mice using liver enzymes assessment. Journal of Biomedical Physics and Engineering, 9(5), 533–540.
Normén, A. L., Brants, H. A., Voorrips, L. E., Andersson, H. A., van den Brandt, P. A., & Goldbohm, R. A. (2001). Plant sterol intakes and colorectal cancer risk in the Netherlands Cohort Study on Diet and Cancer. The American Journal of Clinical Nutrition, 74(1), 141–148.
Ohno, T., Inoue, M., & Ogihara, Y. (2001). Cytotoxic activity of gallic acid against liver metastasis of mastocytoma cells P-815. Anticancer Research, 21(6A), 3875–3880.
Oyagbemi, A. A., Omobowale, O. T., Asenuga, E. R., Akinleye, A. S., Ogunsanwo, R. O., & Saba, A. B. (2016). Cyclophosphamide-induced hepatotoxicity in wistar rats: The modulatory role of gallic acid as a hepatoprotective and chemopreventive phytochemical. International Journal of Preventive Medicine, 7, 51.
Padma, V. V., Sowmya, P., Felix, T. A., Baskaran, R., & Poornima, P. (2011). Protective effect of gallic acid against lindane induced toxicity in experimental rats. Food and Chemical Toxicology, 49(4), 991–998.
Page, J. M., & Harrison, S. A. (2009). Nash and HCC. Clinics in Liver Disease, 13(4), 631–647.
Patel, D. K., Patel, K., Kumar, R., Gadewar, M., & Tahilyani, V. (2012). Pharmacological and analytical aspects of bergenin: A concise report. Asian Pacific Journal of Tropical Disease, 2(2), 163–167.
Peng, C. H., Ker, Y. B., Weng, C. F., Peng, C. C., Huang, C. N., Lin, L. Y., & Peng, R. Y. (2009). Insulin secretagogue bioactivity of finger citron fruit (Citrus medica L. var. Sarcodactylis Hort, Rutaceae). Journal of Agricultural and Food Chemistry, 57(19), 8812–8819.
Phull, A. R., Abbas, Q., Ali, A., Raza, H., Zia, M., & Haq, I. U. (2016). Antioxidant, cytotoxic and antimicrobial activities of green synthesized silver nanoparticles from crude extract of Bergenia ciliata. Future Journal of Pharmaceutical Sciences, 2(1), 31–36.
Punithavathi, V. R., Stanely Mainzen Prince, P., Kumar, M. R., & Selvakumari, C. J. (2011). Protective effects of gallic acid on hepatic lipid peroxide metabolism, glycoprotein components and lipids in streptozotocin-induced type II diabetic Wistar rats. Journal of Biochemical and Molecular Toxicology, 25(2), 68–76.
Raimondo, G., Cacciamo, G., & Saitta, C. (2005). Hepatitis B virus and hepatitis C virus co-infection: Additive players in chronic liver disease?: Concise review. Annals of Hepatology, 4(2), 100–106.
Rajkumar, V., Guha, G., & Kumar, R. A. (2011). Anti-neoplastic activities of Bergenia ciliata rhizome. Journal of Pharmacy Research, 4(2), 443–445.
Roberto, D., Micucci, P., Sebastian, T., Graciela, F., & Anesini, C. (2009). Antioxidant activity of limonene on normal murine lymphocytes: Relation to H2O2 modulation and cell proliferation. Basic and Clinical Pharmacology and Toxicology, 106(1), 38–44.
Rong-Hua, P. A. N., Hong-Mei, H. E., Yue, D. A. I., & Yu-Feng, X. I. A. (2016). Comparative pharmacokinetics of bergenin, a main active constituent of Saxifraga stolonifera Curt., in normal and hepatic injury rats after oral administration. Chinese Journal of Natural Medicines, 14(10), 776–782.
Ruby, K. M., Chauhan, R., Sharma, S., & Dwivedi, J. (2012). Polypharmacological activities of Bergenia species. International Journal of Pharmaceutical Sciences Review and Research, 13(1), 100–110.
Safaei, F., Mehrzadi, S., Khadem Haghighian, H., Hosseinzadeh, A., Nesari, A., Dolatshahi, M., Esmaeilizadeh, M., & Goudarzi, M. (2018). Protective effects of gallic acid against methotrexate-induced toxicity in rats. Acta Chirurgica Belgica, 118(3), 152–160.
Santiago, J. V. A., Jayachitra, J., Shenbagam, M., & Nalini, N. (2012). Dietary d-Limonene alleviates insulin resistance and oxidative stress–induced liver injury in high-fat diet and L-NAME-treated rats. European Journal of Nutrition, 51(1), 57–68.
Sen, S., & Chakraborty, R. (2017). Revival, modernization and integration of Indian traditional herbal medicine in clinical practice: Importance, challenges and future. Journal of Traditional and Complementary Medicine, 7(2), 234–244.
Seyfizadeh, N., Mahjoub, S., Zabihi, E., Moghadamnia, A., Pouramir, M., Mir, H., Khosravifarsani, M., & Elahimanesh, F. (2012). Cytoprotective effects of arbutin against tert-butyl hydroperoxid induced toxicity in Hep-G2 cell line. World Applied Sciences Journal, 19(2), 163–167.
Sousa, J. N., Paraíso, A. F., Andrade, J. M. O., Lelis, D. F., Santos, E. M., Lima, J. P., Monteiro-Junior, R. S., D’Angelo, M. F. S. V., de Paula, A. M. B., Guimarães, A. L. S., & Santos, S. H. S. (2020). Oral gallic acid improve liver steatosis and metabolism modulating hepatic lipogenic markers in obese mice. Experimental Gerontology, 134, 110881.
Sriset, Y., Chatuphonprasert, W., & Jarukamjorn, K. (2020). Hepatoprotective activity of bergenin against xenobiotics-induced oxidative stress in human hepatoma (HepG2) cells. Chiang Mai University Journal of Natural Sciences, 20(1), e2021011.
Tanaka, Y., Obinata, H., Konishi, A., Yamagiwa, N., & Tsuneoka, M. (2020). Production of ROS by gallic acid activates KDM2A to reduce rRNA transcription. Cells, 9(10), 2266.
Timalsena, S., & Lamichhane, P. P. (2019). Astible rivularis: Bioactive compounds and pharmacological functions. Chinese Journal of Integrative Medicine, 25(10), 795–799.
Tiwari, V., Meena, B., Nair, N. K., & Rana, T. S. (2020). Molecular analyses of genetic variability in the populations of Bergenia ciliata in Indian Himalayan Region (IHR). Physiology and Molecular Biology of Plants, 26(5), 975–984.
Varga, Z. V., Matyas, C., Erdelyi, K., Cinar, R., Nieri, D., Chicca, A., Nemeth, B. T., Paloczi, J., Lajtos, T., Corey, L., & Pacher, P. (2018). β-Caryophyllene protects against alcoholic steatohepatitis by attenuating inflammation and metabolic dysregulation in mice. British Journal of Pharmacology, 175(2), 320–334.
Vidyashankar, S., Maheshkumar, P., & Patki, P. S. (2010). Cystone–An ayurvedic polyherbal formulation inhibits adherence of uropathogenic E. coli and modulates H2O2-induced toxicity in NRK-52E cells. Journal of Experimental Pharmacology, 2, 19–27.
Vieira, A. J., Beserra, F. P., Souza, M. C., Totti, B. M., & Rozza, A. L. (2018). Limonene: Aroma of innovation in health and disease. Chemo-Biological Interactions, 283, 97–106.
Wang, J., Tang, L., White, J., & Fang, J. (2014). Inhibitory effect of gallic acid on CCl4-mediated liver fibrosis in mice. Cell Biochemistry and Biophysics, 69(1), 21–26.
World Health Organization. (2019). Global status report on alcohol and health 2018. World Health Organization.
Xia, Y., Li, J., Chen, K., Feng, J., & Guo, C. (2020). Bergenin Attenuates Hepatic Fibrosis by Regulating Autophagy Mediated by the PPAR-γ/TGF-β Pathway. PPAR Research, 2020, 1–13.
Xiang, S., Chen, K., Xu, L., Wang, T., & Guo, C. (2020). Bergenin exerts hepatoprotective effects by inhibiting the release of inflammatory factors, apoptosis and autophagy via the PPAR-γ pathway. Drug Design, Development and Therapy, 14, 129–143.
Yin, Y., Liu, X., Liu, J., Cai, E., Zhu, H., Li, H., Zhang, L., Li, P., & Zhao, Y. (2018). Beta-sitosterol and its derivatives repress lipopolysaccharide/d-galactosamine-induced acute hepatic injury by inhibiting the oxidation and inflammation in mice. Bioorganic and Medicinal Chemistry Letters, 28(9), 1525–1533.
Yuan, C., Zhang, X., Long, X., Jin, J., & Jin, R. (2019). Effect of β-sitosterol self-microemulsion and β-sitosterol ester with linoleic acid on lipid-lowering in hyperlipidemic mice. Lipids in Health Disease, 18(1), 1–11.
Zafar, R., Ullah, H., Zahoor, M., & Sadiq, A. (2019). Isolation of bioactive compounds from Bergenia ciliata (haw.) Sternb rhizome and their antioxidant and anticholinesterase activities. BMC Complementary and Alternative Medicine, 19(1), 1–13.
Zain-ul-Abidin, S., Khan, R., Ahmad, M., Bhatti, M. Z., Zafar, M., Saeed, A., & Khan, N. (2018). Ethnobotanical survey of highly effective medicinal plants and phytotherapies to treat diabetes mellitus II in South-West Pakistan. Indian Journal of Traditional Knowledge, 17, 682–690.
Zhang, J., Song, Q., Han, X., Zhang, Y., Zhang, Y., Zhang, X., Chu, X., Zhang, F., & Chu, L. (2017). Multi-targeted protection of acetaminophen-induced hepatotoxicity in mice by tannic acid. International Immunopharmacology, 47, 95–105.
Zhou, Y., Jin, H., Wu, Y., Chen, L., Bao, X., & Lu, C. (2019). Gallic acid protects against ethanol-induced hepatocyte necroptosis via an NRF2-dependent mechanism. Toxicology in Vitro, 57, 226–232.
Acknowledgements
The authors are thankful to University Grant Commission (UGC) to provide the grant in aid under RUSA grant to Guru Nanak Dev University, Amritsar to established Centre for Basic and Translational Research in Health Science. All the authors have equal contribution in this work. The authors acknowledge Dr. Riaz Ahmad, Aligarh Muslim University for his valuable suggestions.
Funding
The review article does not receive funding in any form.
Author information
Authors and Affiliations
Contributions
UL and SKJ conceived and designed the article. UL and GKT carried out the literature survey. UL prepared the manuscript. HS, TSP and SKJ refined the manuscript for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by ethical review board of the university.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Latief, U., Tung, G.K., Singh, H. et al. Bergenia ciliata as a future candidate for liver diseases: a concise review. JoBAZ 83, 17 (2022). https://doi.org/10.1186/s41936-022-00282-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41936-022-00282-x