Abstract
Background
This study evaluated the existence of anti-drug antibodies (ADAs) before and 52 weeks after switching from intravenous infliximab (IFX) to intravenous CT-P13 in patients with rheumatoid arthritis (RA).
Methods
We performed a prospective observational study. Twenty-eight patients (7 males and 21 females) received intravenous CT-P13 after intravenous IFX, and the clinical data were collected from medical records. Rheumatoid factor (RF) and anti-CCP antibody were examined at baseline. At baseline and 52 weeks after the start of CT-P13 treatment, the Disease Activity Score based on the 28-joint count and the levels of C-reactive protein, matrix metalloproteinase-3, and ADA, as well as the erythrocyte sedimentation rate were evaluated. ADAs were measured using an enzyme-linked immunosorbent assay kit.
Results
Seven (25%) and 6 (21.4%) cases were positive for ADAs at baseline and 52 weeks after, respectively. One case became newly positive for ADAs at week 52. Two of the ADA-positive cases became ADA-negative 52 weeks after. The ADA-positive group showed significantly higher RF values at baseline than the ADA-negative group (p = 0.03). No difference was observed between the ADA-positive group and the ADA-negative group regarding other clinical parameters.
Conclusions
The positive rate of ADAs did not increase after switching from intravenous IFX to intravenous CT-P13. Among the patients with ADAs, a high level of RF was observed at baseline.
Similar content being viewed by others
Introduction
CT-P13 is a biosimilar (BS) of infliximab (IFX) approved for rheumatoid arthritis (RA). Previous clinical trials revealed that switching from IFX to a BS had no detrimental effect on disease activity compared to the IFX-continued groups [1,2,3,4]. Because the price of biosimilar is generally less than that of originator, switching from IFX to CT-P13 are strongly encouraged for economic reasons [5, 6].
The emergence of anti-drug antibodies (ADAs) with neutralizing activities has been a concern when using CT-P13 as well as IFX originator drug [1,2,3, 6, 7]. The prevalence of ADAs in patients receiving IFX therapy has been reported to range from 15 to 54% [3, 6, 8, 9]. Patients with ADAs for IFX had a significantly lower drug concentration than those without ADA, and the serum drug concentration was negatively correlated with the C-reactive protein (CRP) level and erythrocyte sedimentation rate (ESR) [10]. In addition, ADA-positive patients also showed more infusion-related reactions [7, 8]. Therefore, it is clinically important to determine whether or not CT-P13 will increase the positive rate for ADAs after switching.
In this study, we investigated the existence of ADAs before and 52 weeks after switching from IFX to CT-P13. In addition, we compared the baseline characteristics of the ADA-positive and ADA-negative groups.
Materials and methods
Patients
This was a prospective observational study. Twenty-nine patients who met the American College of Rheumatology 1987 criteria [11] and treated with intravenous IFX and switched to intravenous CT-P13 at a single center were assessed for their eligibility. All patients had been treated with CT-P13 for 52 weeks except for one patient who had methotrexate-associated pneumonitis. Thus, 28 RA patients were enrolled in this study. The patients’ data were collected from medical records. There was no change in the dose and interval of prior infliximab and CT-P13 in all patients. The study was conducted in accordance with the ethical principles derived from the Declaration of Helsinki and in compliance with the Good Clinical Practice guideline. Inoue Hospital Institutional Review Board approved this study (approval number: 2016-001), and written informed consent for participation was obtained from all patients.
Before and 52 weeks after the start of CT-P13 treatment, the Disease Activity Score based on the 28-joint count (DAS28) and the levels of CRP, matrix metalloproteinase (MMP)-3, and ADA, as well as the ESR were evaluated. Rheumatoid factor (RF) and anti-CCP antibody (ACPA) were investigated at baseline. An enzyme-linked immunosorbent assay kit (Shikari Q-ATI, Matriks Biotek, Turkey) was used for the measurement of the ADA level for both infliximab and CT-P13, and the ADA cut-off value for positivity was set at 10 ng/ml, according to a previous study [12, 13].
Statistical analyses
The Mann–Whitney U test was used for the comparison of continuous data, and the chi-squared test was used for categorical variables. The paired t-test was used to compare characteristics at baseline and 52 weeks after switching. The SPSS Statistics software program, version 25 (IBM Corp., Armonk, NY, USA), was used for the statistical analyses.
Results
Baseline characteristics and RA treatment
The baseline characteristics are shown in Table 1. All patients used methotrexate (MTX) and the median dose was 6 (4–8) mg/week. The median duration of prior IFX treatment was 109 (93.5–131.5) months, the median dose of IFX was 6.5 (4.5–8.9) mg/ kg, and the median interval of each IFX administration was 8 (8–9) weeks. The median DAS28 at baseline was 2.9 (2.3–3.2).
Characteristics after 52-week use of CT-P13
The characteristics of patients after 52-week use of CT-P13 are shown in Table 1. The dosages of MTX and corticosteroid were not significantly changed. The median DAS28 at Week 52 was 2.7 (1.9–3.1). There were no serious complications over the 52-week period. The dose and interval of CT-P13 were the same as those of prior IFX treatment.
Differences in ADA levels at baseline and week 52
At baseline, the ADA-positive rate was 25% (7/28 patients), and 52 weeks after treatment with CT-P13, it was 21.4% (6/28 patients). Two of 7 patients who had ADAs at baseline became negative for ADA, and 1 of 21 patients who had been negative for ADAs at baseline became positive after 52-week use of CT-P13 (Fig. 1A). Switching from IFX to CT-P13 did not significantly increase the positive rate for ADA after 52 weeks. The distribution of ADA titers at baseline and 52 weeks were shown in Fig. 1B. One case with a particularly high titer of ADA was a male patient with a 12-year history of RA who had an ACPA exceeding 400 U/ml; however, his disease activity was suppressed to the point of remission during the observation period.
ADA-positive patients
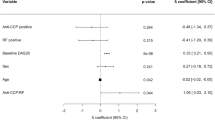
Patients were divided into two groups by the existence of ADA at Week 52. The age, sex, RA disease duration, treatment duration of IFX, DAS28, and levels of CRP, ESR, MMP-3, RF, and ACPA at baseline were compared between these two groups. In the ADA-positive group, the value of RF was significantly higher than that in the ADA-negative group (p = 0.03) (Table2).
Discussion
In this study, we investigated the incidence of ADAs among RA patients who switched from innovator IFX to biosimilar CT-P13. There was no significant increase in the ADA-positive rate after switching from IFX to CT-P13, and a high titer of RF at baseline was observed in the ADA-positive group (p = 0.03).
Previous studies demonstrated that the change from IFX to CT-P13 did not significantly increase ADA incidence [2, 3, 14]. A worldwide randomized, multi-center study demonstrated that the ADA-positive rate after 54-week use of IFX was 48.3% at baseline and 44.8% after 48-week use of CT-P13 [2]. In the Japanese extension study of the clinical trial of CT-P13 (phase I/ II), 33 patients received CT-P13 after 54-week use of IFX. The ADA-positive rate was 48.5% (16/33 patients) at baseline and 21.7% (5/23 patients) after 48 weeks of CT-P13 [3]. Sixteen of 17 patients continued to be negative for ADAs during these 48 weeks, and 5 of 16 patients who were positive for ADAs became negative after 48 weeks in their study. A recent study with a longer observation period also revealed that the ADA-positive rate was 35.6% at baseline and 41.7% after CT-P13 use during the study [14]. In our study, the ADA-positive rates at the time of switching from IFX to CT-P13 and 52 weeks later were 25% and 21.4%, respectively. The dose of IFX and CT-P13 was relatively higher in our study compared to the dose in the previous studies [2, 3], this might influence serum levels of ADA and also the ADA formation.
The DANBIO study, which was based on the Danish nationwide registry, reported that ADA positivity was associated with reduced clinical efficacy and infusion reaction [8]. A low drug concentration [8, 15], long disease duration and smoking [16] have been identified as factors related to ADA positivity in IFX. In addition, a Swedish randomized trial showed that female gender and RF positivity were associated with a low serum IFX concertation and the appearance of ADAs [17]. There was also reported that CT-P13 administered by subcutaneous injection led to the higher serum concentration after 24 weeks and lower ADA positive rate than the CT-P13 by intravenous administration [18].
In our study, the RF values were significantly higher in the ADA-positive group than in the ADA-negative group. RF is an IgM type autoantibody against denatured IgG, and the latest EULAR recommendation has identified it as a poor prognostic factor [19]. A previous randomized double-blind study in Japan revealed that high titers of RF and ACPA were correlated with a low serum IFX level and high TNF level [15]. A high level of RF might thus be associated with a low serum IFX level, leading to the appearance of ADAs. A multi-national, cross-sectional study revealed that IFX-treated patients with ADAs had significantly lower drug concentrations than those without ADAs [10]. The ADA generation was explained by the high TNF level, the higher inflammation or the propensity for antibody production in patients with high RF level.
Several limitations associated with the present study warrant mention. First, the sample size was small, and the observational period was short. Second, the subjects for this study had a long disease duration. Finally, we did not check the drug concentration, although previous reports have shown that ADA positivity was associated with low serum drug concentrations. A further investigation will be needed to clarify the reason for the appearance of ADAs and the treatment effect of CT-P13.
Conclusion
The ADA-positive rate did not increase after switching from innovator IFX to biosimilar CT-P13. Among the patients with ADA, a high level of RF was observed at baseline.
Availability of data and materials
The datasets from this study are available from the corresponding author upon request.
Abbreviations
- ACPA:
-
Anti-CCP antibody
- ADAs:
-
Anti-drug antibodies
- BS:
-
Biosimilar
- CRP:
-
C-reactive protein
- DAS28:
-
Disease Activity Score based on the 28-joint count
- ESR:
-
Erythrocyte sedimentation rate
- IFX:
-
Infliximab
- MMP:
-
Matrix metalloproteinase
- RA:
-
Rheumatoid arthritis
- RF:
-
Rheumatoid factor
References
Jørgensen KK, Olsen IC, Goll GL, Lorentzen M, Bolstad N, Haavardsholm EA, et al. Switching from originator infliximab to biosimilar CT-P13 compared with maintained treatment with originator infliximab (NOR-SWITCH): a 52-week, randomised, double-blind, non-inferiority trial. Lancet. 2017;389(10086):2304–16.
Yoo DH, Prodanovic N, Jaworski J, Miranda P, Ramiterre E, Lanzon A, et al. Efficacy and safety of CT-P13 (biosimilar infliximab) in patients with rheumatoid arthritis: comparison between switching from reference infliximab to CT-P13 and continuing CT-P13 in the PLANETRA extension study. Ann Rheum Dis. 2017;76:355–63.
Tanaka Y, Yamanaka H, Takeuchi T, Inoue M, Saito K, Saeki Y, et al. Safety and efficacy of CT-P13 in Japanese patients with rheumatoid arthritis in an extension phase or after switching from infliximab. Mod Rheumatol. 2017;27:237–45.
Glintborg B, Sørensen IJ, Loft AG, Lindegaard H, Linauskas A, Hendricks O, et al. A nationwide non-medical switch from originator infliximab to biosimilar CT-P13 in 802 patients with inflammatory arthritis: 1-year clinical outcomes from the DANBIO registry. Ann Rheum Dis. 2017;76:1426–31.
Brodszky V, Baji P, Balogh O, Péntek M, Brodszky V. Budget impact analysis of biosimilar infliximab (CT-P13) for the treatment of rheumatoid arthritis in six Central and Eastern European countries. Eur J Health Econ. 2014;15(Suppl 1):S65-71.
Valido A, Silva-Dinis J, Saavedra MJ, Iria I, Gonçalves J, Lopes JP, et al. Efficacy, immunogenicity and cost analysis of a systematic switch from originator infliximab to biosimilar CT-P13 of all patients with inflammatory arthritis from a single center. Acta Reumatol Port. 2019;44:303–11.
Lee SJ, Baek K, Lee S, Lee YJ, Park JE, Lee SG. Post-marketing pooled safety analysis for CT-P13 Treatment of patients with immune-mediated inflammatory diseases in observational cohort studies. BioDrugs. 2020;34:513–28.
Krintel SB, Grunert VP, Hetland ML, Johansen JS, Rothfuss M, Palermo G, et al. The frequency of anti-infliximab antibodies in patients with rheumatoid arthritis treated in routine care and the associations with adverse drug reactions and treatment failure. Rheumatology (Oxford). 2013;52:1245–53.
Wolbink GJ, Vis M, Lems W, Voskuyl AE, de Groot E, Nurmohamed MT, Stapel S, et al. Development of antiinfliximab antibodies and relationship to clinical response in patients with rheumatoid arthritis. Arthritis Rheum. 2006;54:711–5.
Moots RJ, Xavier RM, Mok CC, Rahman MU, Tsai WC, Al-Maini MH, et al. The impact of anti-drug antibodies on drug concentrations and clinical outcomes in rheumatoid arthritis patients treated with adalimumab, etanercept, or infliximab: Results from a multinational, real-world clinical practice, non-interventional study. PLoS ONE. 2017;12: e0175207.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24.
Bálint A, Rutka M, Végh Z, Kürti Z, Gecse KB, Banai J, et al. Frequency and characteristics of infusion reactions during biosimilar infliximab treatment in inflammatory bowel diseases: results from Central European nationwide cohort. Expert Opin Drug Saf. 2017;16:885–90.
Patil A, Upadhyaya S, Dawar R, Dadhaniya N, Sood I, Gupta SJ, et al. Anti-drug antibodies and low serum trough infliximab levels correlate with disease activity measures in spondyloarthritis patients on an as-needed infliximab treatment. Int J Rheum Dis. 2019;22:1638–43.
Cheon JH, Nah S, Kang HW, Lim YJ, Lee SH, Lee SJ, Kim SH, Jung NH, Park JE, Lee YJ, Jeon DB, Lee YM, Kim JM, Park SH. Infliximab biosimilar CT-P13 observational studies for rheumatoid arthritis, inflammatory bowel diseases, and ankylosing spondylitis: pooled analysis of long-term safety and effectiveness. Adv Ther. 2021;38(8):4366–87.
Takeuchi T, Miyasaka N, Inui T, Yano T, Yoshinari T, Abe T, Koike T. High titers of both rheumatoid factor and anti-CCP antibodies at baseline in patients with rheumatoid arthritis are associated with increased circulating baseline TNF level, low drug levels, and reduced clinical responses: a post hoc analysis of the RISING study. Arthritis Res Ther. 2017;19:194.
Quistrebert J, Hässler S, Bachelet D, Mbogning C, Musters A, Tak PP, et al. Incidence and risk factors for adalimumab and infliximab anti-drug antibodies in rheumatoid arthritis: a European retrospective multicohort analysis. Semin Arthritis Rheum. 2019;48:967–75.
Hambardzumyan K, Hermanrud C, Marits P, Vivar N, Ernestam S, Wallman JK, et al. Association of female sex and positive rheumatoid factor with low serum infliximab and anti-drug antibodies, related to treatment failure in early rheumatoid arthritis: results from the SWEFOT trial population. Scand J Rheumatol. 2019;48:362–6.
Westhovens R, Wiland P, Zawadzki M, Ivanova D, Kasay AB, El-Khouri EC, Balázs É, Shevchuk S, Eliseeva L, Stanislavchuk M, Yatsyshyn R, Hrycaj P, Jaworski J, Zhdan V, Trefler J, Shesternya P, Lee SJ, Kim SH, Suh JH, Lee SG, Han NR, Yoo DH. Efficacy, pharmacokinetics and safety of subcutaneous versus intravenous CT-P13 in rheumatoid arthritis: a randomized phase I/III trial. Rheumatology (Oxford). 2021;60(5):2277–87.
Smolen JS, Landewé RBM, Bijlsma JWJ, Burmester GR, Dougados M, Kerschbaumer A, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79:685–99.
Acknowledgements
None.
Funding
The authors declare that they do not receive any source of funding.
Author information
Authors and Affiliations
Contributions
HS and KO made substantial contributions to the design of the study, acquisition, analysis, interpretation of data, and writing of the manuscript. YY and KO participated in the design of the study, acquiring data, helped to draft the manuscript, and contributed to revising the manuscript critically. MI, HI, HM, KT, TS and TK participated in acquiring data and critically contributing to revising the manuscript. HC critically contributed to revising the manuscript enhancing its intellectual content and participated in approving the final content of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the ethical principles derived from the Declaration of Helsinki and in compliance with the Good Clinical Practice guideline. Inoue Hospital Institutional Review Board approved this study (approval number: 2016-001), and written informed consent for participation was obtained from all patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sakane, H., Okamura, K., Inoue, M. et al. Anti-drug antibodies and rheumatoid factor level in patients with rheumatoid arthritis using the infliximab biosimilar CT-P13. BMC Rheumatol 6, 74 (2022). https://doi.org/10.1186/s41927-022-00304-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41927-022-00304-9