Abstract
Purpose
The aim of this study was to create a model of patient-centered outcomes with respect to self-management tasks and skills of patients with a tracheostomy in their home setting.
Methods
A scoping review using four search engines was undertaken (Medline, CINAHL, PsycINFO, Cochrane Library) to identify studies relevant to this issue and published since 2000. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statements for Scoping Reviews (PRISMA-ScR), the Joanna Briggs Institute (JBI) approach of conducting and reporting a scoping review, and the Participants, Concept, Context (PCC) scheme were employed. The following elements of the framework synthesis study data were screened, and presented based on the self-management model of Lorig and Holman.
Results
34 publications from 17 countries met the criteria for study inclusion: 24 quantitative, 8 qualitative and 2 mixed methods designs. Regarding the dimensions of self-management, 28 articles reported on “managing the therapeutic regimen”, 27 articles discussed “managing role and behavior changes”, and 16 articles explored “managing emotions”. A model of self-management of patients with tracheostomy was developed, which placed the patient in the center, since it is this individual who is completing the tasks and carrying out his or her skill sets.
Conclusion
This scoping review represents the first comprehensive overview and modeling of the complex self-management tasks and skills required of patients with tracheostomy in their home setting. The theoretical model can serve as a cornerstone for empirical intervention studies to better support this patient-centered outcome for this population in the future.
Similar content being viewed by others
Background
Although about 250,000 tracheostomies are performed annually worldwide in resource rich countries [1], living with a tracheostomy is far from normal. Those affected have to adjust to a wide range of changes to manage their day-to-day life [2,3,4]. The term tracheotomy refers to an incision in the trachea; tracheostomy represents a temporary or permanent opening in the neck [5, 6]. However, the terms for the procedure are often used interchangeably [5]. A tracheostoma describes an opening into the trachea. Through the stoma a tracheostomy tube is usually inserted [5]. Nowadays, a tracheotomy is performed as an elective as well as an emergency surgical procedure. Indications have expanded over time [7], the most prominent being to provide mechanical ventilation, to protect the airway, and to bypass an upper airway obstruction [5, 6]. In particular, the total laryngectomy should be mentioned in this context, the major treatment modality for stage III-IV laryngeal cancer [8], which requires the surgical removal of the larynx and leads to a permanent artificial airway which is separate from mouth, nose, and esophagus.
Because of the varying indications the impacted patient population ranges from the critically ill patient with intensive care requirements to the independent patient who has received a tracheostomy as part of the medical therapy [9]. Consequently, care of patients with tracheostomy takes place in different healthcare settings, both in the hospital and in outpatient settings [5]. Due to a decline in hospital length of stay, there is an increasing percentage of patients with tracheostomy living in the community [10]. In Germany it is assumed that around 15,000–30,000 patients are affected [11]. In the hospital as well as in the outpatient environment consistent care of patients with tracheostomy is emphasized [5]. However, patients report many negative experiences [7], which may impact their quality of life [7, 12,13,14,15,16].
A publication by Richard and Shea (2011) delineated self-care and associated concepts, according to them self-care, self-management, self-monitoring, and symptom management represent overlapping concepts that build on each other [17]. However, a consensus on the definition of the concept does not exist [18]. Self-management is an overarching concept that includes all “[…] activities necessary to achieve, maintain, or promote optimal health […]” [17, p 261]. It represents the ability of the individual to manage the consequences of health conditions [17]. Following Richard and Shea [17], and Matarese and associates [19], self-management of patients with tracheostomy is conceptualized as the individual’s ability to perform activities related to the care of a tracheostomy and to cope with the life impact of the presence of a tracheostomy. According to Lorig and Holman [20], self-management comprises three dimensions: managing the therapeutic regimen; managing role and behavior changes; and managing emotions. This encompasses self-management tasks and the development of core self-management skills including problem-solving, decision-making, resource utilization, forming a partnership with the healthcare provider, and taking action [20]. Self-management provides opportunities for patients to positively impact their health and health-related habits [21]. Patients are supported in gaining skills and applying them to their routines on a daily basis [22]. Self-management programs have been developed for specific patient populations and have been evaluated as successful in terms of health outcomes and costs [21, 23].
Patients with a tracheostomy are required to manage a comprehensive therapeutic regimen including cannula cleaning, stoma care and dressing changes [24] in order to avoid complications, which can be life-threatening [9]. Daily tracheostomy care, which includes the use of a variety of assistive devices, is very time-consuming [12, 25] and associated with fears, uncertainties [26], and restrictions in numerous activities of daily living [27]. Furthermore, several studies report reduced general health in these patients [28,29,30]. The presence of a tracheostomy leads to physical changes, especially with regard to communication, breathing and nutrition [3, 7, 31]. Moreover, those individuals have to adapt to a changed body image [3, 31]. In a study with patients after laryngectomy, half of the respondents felt embarrassed [32]. They feel stigmatized and isolated [7]. They withdraw from social interactions [32, 33] which influences their social relationships [33]. Psychological effects [34] and a decline in mental health [30] also are described. Patients reported higher levels of depression and anxiety compared to the normative population [28]. Considering the complex impact the tracheostomy has on a patients’ life, those affected have to learn tasks [34] and skills [35] to care for and live with their tracheostomy. A focus on patient-centered outcomes becomes increasingly important, and successful self-management of the tracheostomy in their home setting is needed.
To the best of our knowledge, there is no review of patient-centered outcome research with respect to self-management for patients with tracheostomy. An overview of self-management tasks and skills for patients with tracheostomy could help to guide the development of population specific interventions, their implementation and evaluation, with the aim of improving patient quality of life. Thus, the aim of this paper was to review the literature in order to gain an understanding of patient self-management when living with a tracheostomy at home.
Methods
For this purpose, a scoping review was conducted [36,37,38]. Evidence gaps were identified. This review was conducted and reported in concordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statements for Scoping Reviews (PRISMA-ScR) [39] and the Joanna Briggs Institute (JBI) approach to conducting and reporting scoping reviews [40].
Literature search
After a limited search in Medline and CINAHL to identify keywords and index terms the final search in the databases Medline, CINAHL, PsycINFO, and Cochrane Library was conducted with support by a librarian. Due to a paradigm shift from paternalistic towards patient-centered care the concept of self-mnagement emerged and has been accompanied by an increasing number of publications in this field [41]. Consequently, articles with a publication year of 2000 or later were included in the search for this review. A free text and keyword search was performed using the PCC scheme with search terms related to the participants (P) “patients with tracheostomy”, the concept (C) “self-management” (including related concepts due to their inconsistent use), and context (C) “home setting”. Available Medical Subject Headings (MeSH) terms were added. Search terms were logically combined. Please see supplementary file 1 as an online resource. The process followed the flowchart for study selection adapted from the PRISMA statement [42].
Inclusion and exclusion criteria
Inclusion and exclusion criteria were defined using the PCC scheme (Participants, Concept, Context) [36]. All records that fulfilled the following criteria and were available in English or German language were included:
Participants (P)
Studies of adults (> 18 years of age) either with a temporary or permanent tracheostomy who were fully or partially self-sufficient in tracheostomy care were included. Research on ventilated patients was excluded due to their additional and possibly other needs in managing their self-management.
Concept (C)
This review considered studies that described aspects of self-management in the context of tracheostomy care from the point of view of those affected. Following Richard and Shea [17], and Matarese et al. [19] self-management involved the ability of an individual to perform actions related to the care of a tracheostomy as needed and to deal with the changes in lifestyle and the effects associated with the tracheostomy. For further operationalization self-management tasks and skills included in self-management processes [43] were considered following the model of Lorig and Holman [20].
Context (C)
Studies taking place in the home setting were considered. Research studies that examined the acute inpatient, rehabilitative or nursing home setting as well as publications that focused on tracheostomy care in the context of end-of-life (understood as expected life expectancy of a few months [44]) were excluded. Studies that took place in less developed countries, as well as low and middle income countries (DAC list) [45], were also purposefully excluded because external factors such as available resources, environmental factors, and the health care system may have influenced self-management [21, 46].
This scoping review included qualitative, quantitative, mixed methods studies and systematic reviews. Case studies, text and opinion papers, and letters (editorials, commentaries) were not considered.
Data abstraction and analysis
Data from the included articles were abstracted applying elements of framework synthesis, a strategy for collecting data in scoping reviews [40]. It aims to reduce complexity [47] by searching, screening, and presenting study data using a pre-identified concept [40, 47]. Coding categories were established based on pre-identified themes and expanded with themes that emerged from the data [48]. Based on the self-management model by Lorig and Holman [20] the following dimensions were selected to code data in this review: managing the therapeutic regimen; managing role and behavior changes; and managing emotions [20]. After assigning content to the appropriate dimension, sub-dimensions were created if useful. Each process step was performed by one person, after each separate step the work group met to discuss, critically appraise and reach consensus with regards to findings from this step before the person performing this study moved forward to the next step within this process. Study characteristics were displayed in tabular format.
Results
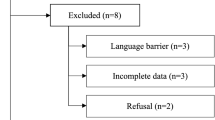
The search in Medline, CINAHL, PsycINFO, Cochrane Library resulted in 3,488 records. After removing duplicates, 2,685 articles remained. After title and abstract screening, 94 full texts were assessed for eligibility. Finally, 34 studies met the criteria for inclusion. The selection process is illustrated in Fig. 1 based on the PRISMA statement as recommended by Moher et al. [42].
Flow chart of the search process according to PRISMA 2009 [41]
Study characteristics
Overall, 34 publications with a focus on patient-centered outcomes from 17 countries, published in the period of the literature search, were included. Study designs captured were quantitative (n = 24; 71%), qualitative (n = 8; 23%), and mixed methods (n = 2, 6%). The objectives of the studies varied. In 47% of quantitative studies (n = 16; 47%) quality of life was the major focus, whereas in 18% of qualitative studies experiences (n = 6; 18%), in one qualitative study adjustment (n = 1; 3%), in one qualitative study needs (n = 1; 3%), and in one qualitative study body image (n = 1; 3%) were the focus of the research. Time from tracheostomy surgery to data collection varied considerably. In 71% of all included studies tracheostomy surgery was on average more than six months prior to data collection (n = 24; 71%). Three studies (9%) utilized longitudinal designs with data collection at six months [49], one year [29], and three years [50] after tracheostomy surgery. 91% of all included publications studied patients after laryngectomy (n = 31; 91%), patients with a permanent artificial airway created after surgical removal of the larynx and which is separate from mouth, nose and esophagus. For more details on the study characteristics see Table 1.
Self-management of patients with tracheostomy
The studies described multiple changes in lifestyle when living with a tracheostomy in the home setting. Regarding the dimensions of self-management, 28 articles (82%) discussed management of the therapeutic regimen, 27 articles (79%) examined managing role and behavior changes, while 16 articles (47%) described managing emotions. An overview of the captured self-management dimensions in the included studies are given in Table 2. Table 3 displays the dimensions and sub-dimensions of self-management of patients with tracheostomy.
Patients with tracheostomy are challenged by a complex therapeutic regimen. In concordance with the generic self-management model provided by Lorig and Holman [20], three self-management dimensions were identified for patients with tracheostomy by this review. Based on these findings, a model of self-management of patients with tracheostomy was developed (Fig. 2).
The patient with a tracheostomy was placed in the center of this pictogram because it is this individual who must perform the tasks and apply his or her skill sets needed for self-management. The circles surrounding the individual represent the self-management dimensions of patients with tracheostomy following Lorig and Holman [20]. Each dimension can be divided into sub-dimensions based on the results of this scoping review. The dimensions overlap based on to the studies included. Detailed information can be seen in Table 4.
Dimension 1: managing the therapeutic regimen
Six publications (18%) reported on self-management in the context of tracheostomy care, which means managing an altered airway [3] and includes stoma care [56], dealing with complications [49] and using medical aids [51]. The latter includes products that are necessary for living with a tracheostomy: tracheostomy tube [62], humidification aids [62], suction devices [62], communication aids [62], and voice prostheses [56] for laryngectomy patients as well as aids that (should) make life easier (such as aids to shower and swim, jewelry to cover the tracheostomy [62]). Moreover, patients have to manage an altered body care concerning dealing with water [25] and showering [3, 51]. Twenty- seven studies (79%) described aspects of managing the tracheostomy- related physical/ functional changes. In this context, alterations in speech / voice, respiratory function, swallowing, senses, oral health, pain, defecation, appearance, power(lessness) and fatigue, including associated tasks, were identified.
Dimension 2: managing role and behavior changes
This portion of the model included studies that described changed roles and everyday behavior which have to be managed by patients. Seventeen studies (50%) reported changed roles. In this context changes in self-identity, social and professional life were reported. Twenty- four studies (71%) described changed everyday behavior. These changes related to social participation, sports activities / leisure activities, communication and eating.
Dimension 3: managing emotions
Sixteen studies (47%) reported on emotions after tracheostomy, patients had to manage in their home setting. The management of negative emotions were described in sixteen studies (47%). According to Izard [70, 71] changes in emotions were related to the concepts of distress, fear, anger, shame, and guilt, stigma was related to these concepts. Three studies reported on positive emotions and included life-saving feeling and optimism.
Discussion
In this comprehensive scoping review, thirty-four articles on patient-centered outcomes with respect to self-management in patients with a tracheostomy in their home setting were synthesized. Patients with a tracheostomy face complex changes in their self-management to adjust to their “daily life with the tracheostomy”. They are required to manage a multitude of changes in the context of “managing their therapeutic regimen”, “managing role and behavior changes”, and “managing their emotions”. The self-management model provided by Lorig and Holman [20] was adapted for patients with a tracheostomy; however, evidence on these three major dimensions differs widely. The majority of publications emphasized the dimension “management of the therapeutic regimen”, and “managing role and behavior changes”, however patient perceptions and skills required to care for the tracheostomy were reported to a lesser extent. In addition, the dimension “managing emotions” was investigated to a lesser extent in the articles studied. Aspects within the three dimensions overlap, e.g. considerations in the physical/ bodily component lead to role changes and/ or emotional implications.
Patients with a tracheostomy in the home setting have received considerable attention by the scientific community during the last decade. Most of the included articles studied patients with a permanent tracheostomy after laryngectomy, which leads to lifelong changes in self-management. These patients are facing a chronic oncological condition. Thus, the promotion of self-management is emphasized with a view to autonomy, adaptation and prevention of complications [72]. Jansen and colleagues [54] assume that self-management interventions for patients after laryngectomy can prevent the development of more serious complications, which may result in more intensive and costly interventions. Patients with head and neck cancer were the main population included in that study. They may suffer from various symptoms and side effects, which influence their physical and emotional wellbeing and quality of life [73, 74]. Symptom experiences and subsequent self-management may relate to the tracheostomy or to the underlying diagnoses, co-morbidities, or side effects of the treatment plan.
For the first self-management dimension, managing the therapeutic regimen, two sub-dimensions were identified: tracheostomy care and tracheostomy- related physical/ functional changes. Tracheostomy care was reported to a lesser extent (n = 6), although correct performance of that skill is essential for patient safety. Moreover, most of the included publications studied patients with respect to their self-management skills in the long-term and reported on participants who had the tracheostomy surgery on average more than six months prior to data collection (n = 24; 71%). Given the theoretical framework of self-management outlined by Lorig and Holman [20], patients’ self-management skills are time dependent. In the context of tracheostomy care, Wulff and associates [16] pointed out that how and when effects are measured is important. Previous studies have found that skills deteriorate right after laryngeal or hypopharyngeal cancer treatment and with subsequent tracheostomy surgery, and stabilize after approximately one year. In addition, the patient perspective with respect to prioritizing their self-management tasks and skills might shift over time [5, 75, 76] and requires further investigation. More precisely, Leemans and colleagues [77] concluded in a study with 1,705 laryngectomized patients that pulmonary changes in particular caused limitations in daily activities and social living.
The second self-management dimension, managing role and behavior changes, included the sub-dimensions of changed roles and changed everyday behavior. Overall, 47% of the studies (n = 17) reported on changed roles. Changes in self-identity, social and professional life were described; however, the implications of these changes on self-management in daily life were reported to a lesser extent. More studies (71%, n = 24) described changed everyday behavior. Dooks and colleagues [3] emphasized that day to day challenges were found by the patients to be more important when compared with the physical management after hospital discharge. Changes regarding social participation, sports activities / leisure activities, communication and eating indicated how profound these influences are on everyday behavior. Responses to these challenges may vary significantly by the individual. Considerable emphasis also has been given to changes in communication. In a study by Danker and associates [32], 54% of patients with tracheostomy talked less than before treatment, 57% stated that much was remaining unsaid, 51% exclusively talked about important things, 42% spoke as little as possible, and 40% refused to speak. Other important changes regarding eating and body care have been investigated to a lesser extent and need further exploration.
The third self-management dimension, managing emotions, can be characterized as adapting and coping with emotional changes having a tracheostomy. Overall, 47% of the included studies (n = 16) reported on a variety of emotions with an overwhelming proportion being negative emotions. Future research is needed with a focus on managing emotions throughout the healthcare experience following a tracheostomy. Continued psychosocial assessment, beginning in the pre-operative period and continuing to the long-term follow-up when patients have returned to the community setting [78] are needed in order to provide appropriate emotional and psychosocial support [8, 72, 76, 78, 79].
The majority of studies focused exclusively on patients after laryngectomy as a permanent condition, whereas a minority of four articles studied patients with a temporary tracheostomy. Although Everitt [78] argued in her expert statement that tracheostomy care does not differ for a temporary tracheostomy or a permanent tracheostomy, Querós and colleagues [31] suggested that the duration of the tracheostomy and the type of surgery are relevant influencing factors on self-management. Future research of self-management of patients with tracheostomy must take this aspect into account.
Strengths and limitations
This study carries several strengths and limitations. First and foremost, a strength of this study is that it was based on the theoretical framework, the definition and the operationalization of the concept of self-management [41]. Because self-management is often used in the context of chronic conditions [17], the applicability of generally accepted self-management definitions and concepts was critically examined in advance. Such definitions must be refined to situation- and/ or disease specific settings [41], and then put into the context of the patient population under investigation. In addition, the data analysis presented provided further description and specification of the dimensions and sub-dimensions of the concept of self-management of patients with a tracheostomy.
This review included studies with adults (> 18 years of age) with either a temporary or permanent tracheostomy, who were fully or partially self-sufficient in tracheostomy care and lived at home. Studies, which did not clearly describe these characteristics were excluded from this analysis, which may have resulted in important data being overlooked. For the literature search, four major databases were used. However, potentially relevant sources might have been missed in databases not considered for this study. Also, articles in languages/ idioms not available to the reviewer might limit our findings. Furthermore, the process of study selection, abstraction and analysis was performed by one person, critically appraised, and consented by the work group and might have led to a potential risk of bias. In addition, it can be assumed that internal and external factors at the individual or micro level may influence self-management processes [80], which also was not the focus of this review. Finally, the aim of this study was an overview of existing literature on self-management of patients with tracheostomy. Since a scoping review does not require a quality assessment [36], included studies had their own strengths and limitations.
Conclusions
This scoping review represents the first comprehensive overview of patient-centered outcomes with respect to the complex self-management tasks and skills required of patients with a tracheostomy living at home. Three self-management dimensions - “managing the therapeutic regimen”, “managing roles and behavior change”, and “managing emotions” - were identified and systematically integrated into a theoretical model. This model can serve as a cornerstone for empirical intervention studies to better support this patient population in the future. A multi-professional approach is recommended to best meet the needs of these patients in their home setting.
Data availability
All data analysed and synthesized during this study are included in this published article.
References
Brenner MJ, Pandian V, Milliren CE, Graham DA, Zaga C, Morris LL, Bedwell JR, Das P, Zhu H, Lee Y, Allen J, Peltz A, Chin K, Schiff BA, Randall DM, Swords C, French D, Ward E, Sweeney JM, Warrillow SJ, Arora A, Narula A, McGrath BA, Cameron TS, Roberson DW (2020) Global Tracheostomy Collaborative: data-driven improvements in patient safety through multidisciplinary teamwork, standardisation, education, and patient partnership. Br J Anaesth 125(1):e104–e118. https://doi.org/10.1016/j.bja.2020.04.054
Bickford J, Coveney J, Baker J, Hersh D (2013) Living with the altered self: a qualitative study of life after total laryngectomy. Int J Speech Lang Pathol 15(3):324–333. https://doi.org/10.3109/17549507.2013.785591
Dooks P, McQuestion M, Goldstein D, Molassiotis A (2012) Experiences of patients with laryngectomies as they reintegrate into their community. Support Care Cancer 20(3):489–498. https://doi.org/10.1007/s00520-011-1101-4
Nalbadian M, Nikolaou A, Nikolaidis V, Petridis D, Themelis C, Daniilidis I (2001) Factors influencing quality of life in laryngectomized patients. Eur Arch Otorhinolaryngol 258(7):336–340. https://doi.org/10.1007/s004050100376
Mitchell RB, Hussey HM, Setzen G, Jacobs IN, Nussenbaum B, Dawson C, Brown CA 3rd, Brandt C, Deakins K, Hartnick C, Merati A (2013) Clinical consensus statement: tracheostomy care. Otolaryngol Head Neck Surg 148(1):6–20. https://doi.org/10.1177/0194599812460376
Cheung NH, Napolitano LM (2014) Tracheostomy: epidemiology, indications, timing, technique, and outcomes. Respir Care 59(6):895–915. https://doi.org/10.4187/respcare.02971
Nakarada-Kordic I, Patterson N, Wrapson J, Reay SD A systematic review of patient and caregiver experiences with a Tracheostomy. Patient 11(2):175–191. https://doi.org/10.1007/s40271-017-0277-1
Yang H, Zeng F, Pang T, Zhang H, Lu J (2021) A qualitative study of the experience of returning to family life and the coping styles of patients after total laryngectomy. Ann Palliat Med 10(11):11482–11491. https://doi.org/10.21037/apm-21-2687
Spataro E, Durakovic N, Kallogjeri D, Nussenbaum B (2017) Complications and 30-day hospital readmission rates of patients undergoing tracheostomy: a prospective analysis. Laryngoscope 127(12):2746–2753. https://doi.org/10.1002/lary.26668
Mehta AB, Syeda SN, Bajpayee L, Cooke CR, Walkey AJ, Wiener RS (2015) Trends in Tracheostomy for mechanically ventilated patients in the United States, 1993–2012. Am J Respir Crit Care Med 192(4):446–454. https://doi.org/10.1164/rccm.201502-0239OC
Osterloh F (2016) Tracheotomierte Patienten: Intensivpatienten beim Hausarzt. Dtsch Ärztebl 113(33–34):A1482–1484
Pereira da Silva A, Feliciano T, Vaz Freitas S, Esteves S, Almeida e Sousa C (2015) Quality of life in patients submitted to total laryngectomy. J Voice 29(3):382–388. https://doi.org/10.1016/j.jvoice.2014.09.002
Gilony D, Gilboa D, Blumstein T, Murad H, Talmi YP, Kronenberg J, Wolf M (2005) Effects of tracheostomy on well-being and body-image perceptions. Otolaryngol Head Neck Surg 133(3):366–371. https://doi.org/10.1016/j.otohns.2005.04.025
Hu Z-Y, Feng X-Q, Fu MR, Yu R, Zhao H-L (2020) Symptom patterns, physical function and quality of life among head and neck cancer patients prior to and after surgical treatment: a prospective study. Eur J Oncol Nurs 46:101770. https://doi.org/10.1016/j.ejon.2020.101770
Li Y, Li X, Mao C, Lv G, Xie Z, Jiang H, Li P (2020) Symptom clusters in head and neck cancer patients with endotracheal tube: which symptom clusters are independently associated with health-related quality of life? Eur J Oncol Nurs 48:101819. https://doi.org/10.1016/j.ejon.2020.101819
Wulff NB, Dalton SO, Wessel I, Arenaz Búa B, Löfhede H, Hammerlid E, Kjae TK, Godballe C, Kjaergaard T, Homøe P (2021) Health-Related Quality of Life, Dysphagia, Voice Problems, Depression, and Anxiety After Total Laryngectomy. Laryngoscope 2022;132(5):980–988. https://doi.org/10.1002/lary.29857
Richard AA, Shea K (2011) Delineation of Self-Care and Associated Concepts: Self-Care Concept Delineation. J Nurs Scholarsh 43(3):255–264. https://doi.org/10.1111/j.1547-5069.2011.01404.x
Van de Zutter VD, Satink F, Costa T, Janquart U, Senn S, Vriendt D PD (2019) Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ Open. https://doi.org/10.1136/bmjopen-2018-027775
Matarese M, Lommi M, De Marinis MG, Riegel B (2018) A systematic review and integration of Concept analyses of self-care and related concepts: self-care and related concepts. J Nurs Scholarsh 50(3):296–305. https://doi.org/10.1111/jnu.12385
Lorig KR, Holman H (2003) Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 26:1–7. https://doi.org/10.1207/S15324796ABM2601_01
Grady PA, Gough LL (2014) Self-Management: a Comprehensive Approach to Management of Chronic Conditions. Am J Public Health 104(8):e25–31. https://doi.org/10.2105/AJPH.2014.302041
Lorig K (1996) Chronic Disease Self-Management: a model for Tertiary Prevention. Am Behav Sci 39(6):676–683. https://doi.org/10.1177/0002764296039006005
Bodenheimer T, Lorig K, Holman H, Grumbach K (2002) Patient self-management of Chronic Disease in Primary Care. JAMA 288(19):2469–2475. https://doi.org/10.1001/jama.288.19.2469
Karaca T, Altinbas Y, Aslan S (2019) Tracheostomy care education and its effect on knowledge and burden of caregivers of elderly patients: a quasi-experimental study. Scand J Caring Sci 33(4):878–884. https://doi.org/10.1111/scs.12684
Mertl J, Žáčková E, Řepová B (2018) Quality of life of patients after total laryngectomy: the struggle against stigmatization and social exclusion using speech synthesis. Disabil Rehabil Assist Technol 13(4):342–352. https://doi.org/10.1080/17483107.2017.1319428
Jerusel R (2017) Das Erleben von Menschen mit Tracheostoma im häuslichen setting. Pflegewissenschaft 19(9–10):468–474
Wrapson J, Patterson N, Nakarada-Kordic I, Reay S (2017) A life-changing event: patients’ personal experiences of living with a long-term tracheostomy. Des Health 1(2):256–271. https://doi.org/10.1080/24735132.2017.1386432
Perry A, Casey E, Cotton S (2015) Quality of life after total laryngectomy: functioning, psychological well-being and self-efficacy. Int J Lang Commun Disord 50(4):467–475. https://doi.org/10.1111/1460-6984.12148
Singer S, Danker H, Guntinas-Lichius O, Oeken J, Pabst F, Schock J, Vogel H-J, Meister EF, Wulke C, Dietz A (2014) Quality of life before and after total laryngectomy: results of a multicenter prospective cohort study. Head Neck 36(3):359–368. https://doi.org/10.1002/hed.23305
Hashmi NK, Ransom ER, Nardone HC, Redding N, Mirza N (2010) Quality of life and self-image in patients undergoing tracheostomy. Laryngoscope 120(Suppl 4):S196. https://doi.org/10.1002/lary.21663
Queirós S, Santos C, Brito A, Pinto I (2017) Conditioning factors for the development of the self-care competence in the person with a tracheostomy. Rev Enferm Referência 4(14):57–67. https://doi.org/10.12707/RIV17010
Danker H, Wollbruck D, Singer S, Fuchs M, Brahler E, Meyer A (2010) Social withdrawal after laryngectomy. Eur Arch Otorhinolaryngol 267(4):593–600. https://doi.org/10.1007/s00405-009-1087-4
Babin E, Beynier D, Le Gall D, Hitier M (2009) Psychosocial quality of life in patients after total laryngectomy. Rev Laryngol Otol Rhinol (Bord) 130(1):29–34
Al Humaid M, Wiechula R (2017) The experience of adult patients who have tracheostomy tubes in situ: a systematic review. Saudi Crit Care J 1(1):24–42. https://doi.org/10.4103/sccj.sccj_2_17
Bickford J, Coveney J, Baker J, Hersh D (2019) Validating the changes to self-identity after total laryngectomy. Cancer Nurs 42(4):314–322. https://doi.org/10.1097/NCC.0000000000000610
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, Khalil H (2021) Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement 19(1):3–10. https://doi.org/10.1097/XEB.0000000000000277
Pollock D, Davies EL, Peters MD, Tricco AC, Alexander L, McInerney P, Godfrey CM, Khalil H, Munn Z (2021) Undertaking a scoping review: a practical guide for nursing and midwifery students, clinicians, researchers, and academics. J Adv Nurs 77(4):2102–2113. https://doi.org/10.1111/jan.14743
Khalil H, Peters MD, Tricco AC, Pollock D, Alexander L, McInerney P, Godfrey CM, Munn Z (2021) Conducting high quality scoping reviews-challenges and solutions. J Clin Epidemiol 130:156–160. https://doi.org/10.1016/j.jclinepi.2020.10.009
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE (2018) PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 169(7):467–473. https://doi.org/10.7326/M18-0850
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H (2020) Chap. 11: Scoping reviews. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis, JBI. https://synthesismanual.jbi.global. Accessed 4 Jan 2023
Jaarsma T, Strömberg A, Dunbar SB, Fitzsimons D, Lee C, Middleton S, Vellone E, Freedland KE, Riegel B (2020) Self-care research: how to grow the evidence base? Int J Nurs Stud 105:103555. https://doi.org/10.1016/j.ijnurstu.2020.103555
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Schulman-Green D, Jaser S, Martin F, Alonzo A, Grey M, McCorkle R, Redeker NS, Reynolds N, Whittemore R (2012) Processes of self-management in chronic illness. J Nurs Scholarsh 44(2):136–144. https://doi.org/10.1111/j.1547-5069.2012.01444.x
Hui D, Nooruddin Z, Didwaniya N, Dev R, De La Cruz M, Kim SH, Kwon JH, Hutchins R, Liem C, Bruera E (2014) Concepts and definitions for actively dying. “End of Life ” “Terminally Ill ” “Terminal Care ” and “Transition of Care”: A Systematic Review J Pain Symptom Manage 47(1):77–89. https://doi.org/10.1016/j.jpainsymman.2013.02.021
OECD (2021) DAC List of ODA Recipient for reporting on aid in 2021. https://www.oecd.org/dac/financing-sustainable-development/development-finance-standards/DAC-List-of-ODA-Recipients-for-reporting-2021-flows.pdf. Accessed 11 Oct 2021
Schulman-Green D, Jaser SS, Park C, Whittemore R (2016) A metasynthesis of factors affecting self-management of chronic illness. Adv Nurs 72(7):1469–1489. https://doi.org/10.1111/jan.12902
Brunton G, Oliver S, Thomas J (2020) Innovations in framework synthesis as a systematic review method. Res Synth Methods 11(3):316–330. https://doi.org/10.1002/jrsm.1399
Dixon-Woods M (2011) Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 9:39. https://doi.org/10.1186/1741-7015-9-39
Armstrong E, Isman K, Dooley P, Brine D, Riley N, Dentice R, King S, Khanbhai F (2001) An investigation into the quality of life of individuals after laryngectomy. Head Neck 23(1):16–24
Singer S, Keszte J, Dietz A, Kluge A, Plontke S, Heim M, Vogel HJ, Matthäus C, Oeken J, Breitenstein K, Koscielny S, Pabst F, Schock J, Eichhorn T, Meister E, Mehnert A, Meyer A (2013) [Vocational rehabilitation after total laryngectomy]. Berufliche Rehabilitation nach Laryngektomie Laryngorhinootologie 92(11):737–745. https://doi.org/10.1055/s-0033-1343454
van Sluis KE, Kornman AF, van der Molen L, van den Brekel MWM, Yaron G (2020) Women’s perspective on life after total laryngectomy: a qualitative study. Int J Lang Commun Disord 55(2):188–199. https://doi.org/10.1111/1460-6984.12511
Teruya N, Sunagawa Y, Toyosato T, Yokota T (2019) Association between Daily Life Difficulties and Acceptance of disability in Cancer Survivors after total laryngectomy: a cross-sectional survey. Asia-Pac J Oncol Nurs 6(2):170–176. https://doi.org/10.4103/apjon.apjon_50_18
Bickford JM, Coveney J, Baker J, Hersh D (2018) Self-expression and identity after total laryngectomy: implications for support. Psychooncology 27(11):2638–2644. https://doi.org/10.1002/pon.4818
Jansen F, Eerenstein SEJ, Lissenberg-Witte BI, van Uden-Kraan CF, Leemans CR, Leeuw IMV (2018) Unmet supportive care needs in patients treated with total laryngectomy and its associated factors. Head Neck 40(12):2633–2641. https://doi.org/10.1002/hed.25358
Morris LL, Lupei M, Afifi MS (2017) FEATURE. Body image perception after Tracheostomy. ORL Head Neck Nurs 35(4):13–18
Cnossen IC, van Uden-Kraan CF, Eerenstein SE, Rinkel RN, Aalders IJ, van den Berg K, de Goede CJ, van Stijgeren AJ, Cruijff-Bijl Y, de Bree R, Leemans CR, -de Verdonck IM (2015) A participatory design approach to develop a web-based self-care program supporting early rehabilitation among patients after total laryngectomy. Folia Phoniatr Logop 67(4):193–201. https://doi.org/10.1159/000441251
Offerman MPJ, Pruyn JFA, de Boer MF, Busschbach JJV, Baatenburg de Jong RJ (2015) Psychosocial consequences for partners of patients after total laryngectomy and for the relationship between patients and partners. Oral Oncol 51(4):389–398. https://doi.org/10.1016/j.oraloncology.2014.12.008
Roick J, Keszte J, Danker H, Meister EF, Vogel HJ, Jenzewski EM, Horn IS, Singer S (2014) [Social integration and its relevance for quality of life after laryngectomy]. Soziale Integration und deren Bedeutung für die Lebensqualität nach Laryngektomie. Laryngorhinootologie 93(5):321–326. https://doi.org/10.1055/s-0033-1358715
Tsikoudas A, Barnes ML, White P (2011) The impact of tracheostomy on the nose. Eur Arch Otorhinolaryngol 268(7):1005–1008. https://doi.org/10.1007/s00405-011-1522-1
Noonan BJ, Hegarty J (2010) The impact of total laryngectomy: the patient’s perspective. Oncol Nurs Forum 37(3):293–301. https://doi.org/10.1188/10.ONF.293-301
Minovi A, Nowak C, Marek A, Hansen S, Dazert S, Brors D (2009) [Quality of life in long-term survivors after laryngectomy]. Lebensqualität bei Langzeitüberlebenden nach Laryngektomie. Laryngorhinootologie 88(1):18–22. https://doi.org/10.1055/s-2008-1077312
Singer S, Meyer A, Kienast U, Rust V, Taschner R, Wulke C, Schwarz R (2007) [Use of adaptive devices by laryngectomees]. Nutzung ausgewählter Hilfsmittel durch Laryngektomierte. Rehabilitation (Stuttg) 46(6):356–362. https://doi.org/10.1055/s-2007-985169
Singer S, Danker H, Bloching M, Kluge A, Schwenke J, Oeken J, Fuchs M, Schwarz R (2007) [Perceived stigmatisation following laryngectomy]. Stigmatisierungsgefühle nach Kehlkopfentfernung. Psychother Psychosom Med Psychol 57(8):328–333. https://doi.org/10.1055/s-2006-952016
Woodard TD, Oplatek A, Petruzzelli GJ (2007) Life after total laryngectomy: a measure of long-term survival, function, and quality of life. Arch Otolaryngol Head Neck Surg 133(6):526–532. https://doi.org/10.1001/archotol.133.6.526
Vilaseca I, Chen AY, Backscheider AG (2006) Long-term quality of life after total laryngectomy. Head Neck 28(4):313–320. https://doi.org/10.1002/hed.20268
Schuster M, Hoppe U, Kummer P, Eysholdt U, Rosanowski F (2003) [Coping strategies in laryngectomy patients]. Krankheitsbewältigungsstrategien Laryngektomierter Patienten HNO 51(4):337–343. https://doi.org/10.1007/s00106-003-0810-5
Birkhaug EJ, Aarstad HJ, Aarstad AKH, Olofsson J (2002) Relation between mood, social support and the quality of life in patients with laryngectomies. Eur Arch Otorhinolaryngol 259(4):197–204. https://doi.org/10.1007/s00405-001-0444-8
Lennie TA, Christman SK, Jadack RA (2001) Educational needs and altered eating habits following a total laryngectomy. Oncol Nurs Forum 28(4):667–674
Relic A, Mazemda P, Arens C, Koller M, Glanz H (2001) Investigating quality of life and coping resources after laryngectomy. Eur Arch Otorhinolaryngol 258(10):514–517. https://doi.org/10.1007/s004050100380
Izard CE (2009) Emotion theory and research: highlights, unanswered questions, and emerging issues. Annu Rev Psychol 60:1–25. https://doi.org/10.1146/annurev.psych.60.110707.163539
Izard CE (1999) Die Emotionen des Menschen - Eine Einführung in die Grundlagen der Emotionspsychologie, 4th edn. Psychologie Verlags Union, Weinheim
Queirós SMM, Pinto IES, Brito MAC, Santos CSV (2021) Nursing interventions for the promotion of tracheostomy self-care: a scoping review. J Clin Nurs 30(21–22):3055–3071. https://doi.org/10.1111/jocn.15823
Zebralla V, Wichmann G, Pirlich M, Hammermüller C, Berger T, Zimmermann K, Neumuth T, Mehnert-Theuerkauf A, Dietz A, Hinz A, Wiegand S (2021) Dysphagia, voice problems, and pain in head and neck cancer patients. Eur Arch Otorhinolaryngol 278(10):3985–3994. https://doi.org/10.1007/s00405-020-06584-6
Tashimo Y, Ihara Y, Yuasa K, Shinji S, Saito Y, Katsuta H, Shimane T, Takahashi K (2019) Acute Stage Longitudinal Change of Quality of Life from pre- to 3 months after Surgical Treatment in Head and Neck Cancer Patients. Asian Pac J Cancer Prev 20(10):3129–3136. https://doi.org/10.31557/APJCP.2019.20.10.3129
Lewarski JS (2005) Long-term care of the patient with a Tracheostomy. Respir Care 50(4):534–537
Paul F (2010) Tracheostomy care and management in general wards and community settings: literature review. Nurs Crit Care 15(2):76–85. https://doi.org/10.1111/j.1478-5153.2010.00386.x
Leemans M, van Sluis KE, van Son RJJH, van den Brekel MWM (2020) Interaction of functional and participation issues on quality of life after total laryngectomy. Laryngoscope Investig Otolaryngol 5(3):453–460. https://doi.org/10.1002/lio2.381
Everitt E (2016) Care of patients with permanent tracheostomy. Nurs Times 112(21–23):20–22
Bowers B, Scase C (2007) Tracheostomy: facilitating successful discharge from hospital to home. Br J Nurs 16(8):476–479. https://doi.org/10.12968/bjon.2007.16.8.23418
Miller WR, Lasiter S, Bartlett Ellis R, Buelow JM (2015) Chronic disease self-management: a hybrid concept analysis. Nurs Outlook 63(2):154–161. https://doi.org/10.1016/j.outlook.2014.07.005
Acknowledgements
We would like to express our gratitude to our graphic design department for their graphical support of the model.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors declare that this study has been performed without external funds or grants.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
SW and CK contributed to the review conception and design. Material preparation, data collection and analysis were performed by SW. The first draft of the manuscript was written by SW. CK and JP commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests in this section.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weidlich, S., Pfeiffer, J. & Kugler, C. Self-management of patients with tracheostomy in the home setting: a scoping review. J Patient Rep Outcomes 7, 101 (2023). https://doi.org/10.1186/s41687-023-00643-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-023-00643-2