Abstract
Background
A tracheostomy is a surgically created opening through the anterior neck tissues and the trachea, into which a tube is inserted. Despite its influence on basic human needs such as respiration, communication and nutrition, little is known about the impact of tracheostomy on patients and their caregivers or what could be done to enable better care and quality of life (QoL) for these individuals.
Objective
The aim of this review was to better understand the current knowledge related to the experience and QoL of adults living with a tracheostomy and their caregivers so as to be able to improve these experiences.
Method
A systematic review of the English-language, peer-reviewed literature was conducted in PubMed, Scopus, PsychINFO, Google Scholar, and CINAHL databases. Articles were eligible if they included adult patient or lay caregiver-reported experiences of tracheostomy.
Results
Overall, 1080 articles were identified and 17 eligible for inclusion. Fourteen articles reported on experiences of tracheostomy patients, while three focused on those of their caregivers. Studies were conducted in the home setting (n = 5), on a hospital ward (n = 4), in an intensive care unit (n = 3), in an outpatient clinic (n = 3), in a rehab facility (n = 1), and online (n = 1). Patients and their caregivers reported a range of mostly negative experiences related to the care, support, and management of a tracheostomy, speech and communication, wellbeing and QoL, disfigurement and body image, and stigma and social withdrawal.
Conclusion
Few studies have published data on the patient and caregiver experiences with tracheostomy, especially in the community setting. There is a need to better understand these experiences in order to be able to formulate strategies and provide resources to improve the quality of care and overall QoL of patients with a tracheostomy and their caregivers in-hospital and in the community.
Similar content being viewed by others
People who have first-hand experiences of a tracheostomy and their caregivers report feeling scared, overwhelmed, unsupported, self-conscious, powerless, judged, and isolated. |
More research is needed to gain a deeper understanding of the first-hand experiences of individuals with long-term tracheostomies living in the community so as to develop new tools and strategies to enable a better quality of life for them and their families. |
Practical steps could be taken to improve the experiences of persons with a tracheostomy and their caregivers, namely, providing more information and counselling prior to and immediately after receiving a tracheostomy; formulating a patient-specific communication plan early on; providing help through social support groups to overcome social isolation and withdrawal and to reduce stigma; and revisiting the design of tracheostomy-related products to improve comfort, aesthetics, and usability. |
1 Introduction
A tracheostomy is a surgically created opening through the anterior neck tissues and the trachea, into which a tube is inserted. Tracheotomy is one of the oldest surgical procedures, the indications for which have changed and expanded over the 20th century. Traditionally used almost exclusively to bypass upper airway obstruction, it is now a common procedure performed as both a temporary and permanent measure for a variety of additional reasons, such as clearing bronchial secretions and providing mechanical ventilation [2]. Advances such as percutaneous dilatational tracheostomy, a minimally invasive, alternative to surgical tracheostomy, which can be performed bedside, have added to the increased use of tracheostomy [1]. Concrete numbers are hard to find, but it is suggested that around 7000 tracheostomies are performed in Australia and New Zealand annually [3]. In the USA, this figure exceeds 113,000 a year for patients 18 years and older [4].
Individuals with tracheostomies are presented with a variety of functional, physical, and psychosocial challenges spanning from the point of insertion [5] through hospital discharge [6] to caring for the tracheostomy at home [7]. Due to its influence on basic human needs such as respiration, communication, and nutrition, the presence of a long-term tracheostomy will likely impact upon the psychosocial wellbeing and quality of life (QoL) of the individual concerned. Adverse psychosocial impacts may arise due to the inherent disfigurement accompanying a tracheostomy. It is widely understood that acquired disfigurement presents unique psychological and social challenges and may profoundly impact upon an individual’s life [8,9,10]. The aim of this paper was to examine the current literature with the hope of gaining an understanding of the experiences of these individuals and their families and of identifying opportunities for improvement in their care and QoL.
2 Method
Keyword searches were conducted on the following electronic databases: PubMed, Scopus, PsychINFO, Google Scholar, and CINAHL. Search strings combined the following terms as well as relevant variations of each term: ‘tracheostomy’, ‘tracheotomy’, ‘experience’, ‘living’, ‘psychosocial’, and ‘quality of life’. No limits were placed on publication dates. References of the identified papers were examined for additional relevant studies.
Titles and abstracts were screened first to determine eligibility. The criteria for inclusion in the review were:
-
English-language only.
-
Patients aged 18 years and older.
-
The paper has been published in a peer reviewed journal or conference proceedings.
-
Experiences from patient/family perspective only.
Exclusion criteria were:
-
Paediatric patients and caregivers.
-
Laryngectomy.
-
Mechanical ventilation—where the article did not distinguish between the intubated and tracheostomised patients.
-
Tracheostomy for end-of-life care.
For all studies that could not be definitively excluded, the full-text versions of the articles were reviewed.
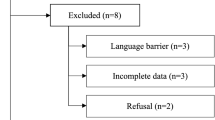
The review was conducted by two independent reviewers in March 2016 and again in April 2017 to ensure no highly relevant literature was missed for the purposes of this review. Each reviewer read and assessed titles and abstracts for eligibility independently. The full manuscripts of potentially eligible studies were then retrieved and assessed by both reviewers against the inclusion and exclusion criteria. At this stage, the reviewers resolved any disagreements in the application of inclusion or exclusion criteria by consensus and/or consultation with one other reviewer. After the first review, the decision was made to narrow the search criteria in the subsequent review to exclude the studies that included the following words: ‘pediatric’, ‘parent’, ‘child’, ‘children’, and ‘infant’. Studies involving paediatric patients largely focused on neonates with multiple care needs in an intensive care setting, where issues related to tracheostomy alone could not easily be singled out, as well as the fact that the patient’s perspective could not be captured. This narrowed the final number of articles suitable for inclusion from 27 to 17. Full details of the search and screening results are provided in Fig. 1.
Articles were reviewed and analysed through thematic analysis [11]. This involved extracting patterns or themes pertinent to the patient or caregiver experiences with tracheostomy (such as impacts on day-to-day living, physical function, and psychosocial issues). The primary researcher used an inductive approach to repeatedly reading the selected articles to identify repeated patterns of meaning. Key initial codes were identified for each topic (for example, management-related issues, such as discomfort associated with suction, tube change and cleaning), and these key codes were checked by another member of the research team. Once initial codes had been identified within each topic, these were sorted into potential themes and sub-themes, and these were reviewed and refined by both researchers in terms of their scope and content.
3 Results
Overall, 1080 articles were identified and 17 were eligible for inclusion. These are summarised in Table 1. Fourteen articles reported on experiences of tracheostomy patients, while three focused on those of their caregivers. We decided to include one study that reported on experiences of patients and caregivers, most of which cared for a child with a tracheostomy. The sample of participants in this study was large (n = 220) compared to other reviewed studies (where sample size varied from n = 1 to n = 70) and included adult patients with a tracheostomy, whose valuable experiences would have been overlooked if the study was excluded from the review.
Studies were conducted in the home setting (n = 5), on a hospital ward (n = 4), in an intensive care unit (ICU) (n = 3), in an outpatient clinic (n = 3), in a rehab facility (n = 1), and online (n = 1). Apart from three studies conducted in the 1980s and focusing on a small number of individuals with sleep apnoea, the majority of studies were conducted in the last 10 years.
Five main themes emerged from the research: (1) care, support, and management of a tracheostomy; (2) speech and communication; (3) wellbeing and QoL; (4) disfigurement and body image; and (5) stigma and social withdrawal.
3.1 Care, Support, and Management
Care of tracheostomy patients is traditionally undertaken in specialised areas such as the ICU or on the ear, nose, and throat (ENT) hospital wards where the procedure was carried out [11].
Studies regarding the care of tracheostomy patients in the ICU and in the general ward are largely focused on physical care and wellbeing, and issues arising at the point of patient discharge [12].
In all but one reviewed study, basic tube care was reported as an issue. Participants described finding aspects of tracheostomy tube care as initially frightening, since problems and complications with it could be life-threatening [13]. For some, this was exacerbated by the lack of understanding of the benefits of the procedure and poor preoperative counselling [14], especially in those cases where there was no time to prepare the patient or their family to come to terms with having a tracheostomy because of the patient’s critical condition [15]. Patients often reported being fearful of and experiencing discomfort during cleaning, suctioning, and tube change [16, 17]. Some individuals reported having physical discomfort when moving their head and neck, which they attributed to the tube pressing on their trachea [18].
Most common problems with tracheostomy as identified by users were mucus plugging, coughing, difficulty talking, and throat irritation (often in dry and cold weather when the tube was in direct contact with clothing), difficulty swallowing, and accidental decannulation, often due to excessive coughing [5, 18,19,20]. Despite the fear and discomfort associated with suction [16], in one study, a patient described the relief after tube cleaning as being due to ‘something disgusting being taken away’, rather than the phlegm being cleared from her chest to make it easier to breathe [5]. Coughing and dry heaving from water accidentally getting in during showering, and fear and anxiety around not being able to breathe were cited as distressing in the same study.
Fear of tube suction and change was, however, alleviated if the patient was adequately prepared by the staff for the upcoming procedure [17]. Establishing trust in, and receiving reassurance from, the nursing staff prior to tube change helped prepare and relax the patient and their family for what they described as an unpleasant, but not a painful procedure [15, 17]. In those studies where participants said health care staff made them feel safe and cared for, they attributed this not only to competence and skill with procedures, but also to the manner and sensitivity with which the staff performed the procedures [5, 21]. In the study by Flinterud and Andershed [21], participants said health professionals in the ICU often instinctively knew their needs, even though they were unable to communicate them verbally. However, this was not always the case outside the ICU.
The experience of being discharged from hospital is a daunting process for tracheostomised individuals and their carers [6]. The effectiveness of hospital and community medical staff is imperative for a successful discharge and to prevent readmission and critical incidents [6]. Discharge planning is recommended up to 2 weeks before discharge, and preparation of the community nurse, as well as patient and carer education are extremely important [6, 15]. However, Garner et al. [12] found that 47% of otolaryngologists did not use a standardised tracheostomy discharge protocol. McCormick et al. [22] surveyed tracheostomised patients and their families and found that only 48% felt ‘very prepared’ at discharge, 11% reported they did not receive emergency training prior to discharge, and fragmented care or limited teamwork was reported by 32% of participants. Sherlock et al. [16] also reported the participants in their study felt they received insufficient information about their tracheostomy and its complications that was not adapted to their individual needs. Participants in this study suggested different ways in which information could be provided both during admission and discharge to meet differing needs, including demonstrations, models, leaflets, and dedicated time to discuss issues.
Caring for a tracheostomy at home is burdensome on both the patient and the caregiver, commonly a spouse [15, 19, 23]. Support and education for both the individual living with the tracheostomy and their caregiver is paramount [24]. Participants in the reviewed studies generally reported the lack of and the strong need for guidance, training, periodic support or reassurance from health professionals [18, 20, 23, 25]. Family members often educated themselves about tracheostomy care through their own research and experimentation, and sometimes ended up supervising and educating the very health care providers meant to oversee the patient’s care (e.g. having to intervene when home health care providers failed to recognise a dislodged tube or properly treat mucus plugging) [22]. In the same study, family caregivers expressed frustration and dissatisfaction with transition to home due to ‘fragmented’ care and lack of standardised knowledge among home health care professionals. Family members also saw themselves as managers of their loved one’s care, being involved with arranging home care and supplies and coordinating health care visits [22].
Citing lack of follow-up care from health professionals, people living with a tracheostomy resorted to finding solutions for their tracheostomy problems through trial and error, a process that, in one case reported in 1980s, took a year [20]. These solutions involved a great deal of customisation by the user, such as cutting off and curving a small brush used to clean coffee percolators to clean the inside of the tracheostomy tube, using a toothbrush to clean the outside of the tube, or replacing the hospital ties that secure the tube around the neck with a small elastic cord tied to hooks from hook–eye sets.
In a study conducted in the 1980s, people living with a tracheostomy also expressed fear and frustration about the lack of opportunities for discussing their concerns with people who could understand their situation [18]. In a study by McCormick et al. [22], nearly half of respondents indicated a desire to have met with a patient with a tracheostomy prior to surgery or discharge, but were not offered that opportunity.
3.2 Speech and Communication
Immediately after tracheostomy, the presence of a tracheostomy tube does not permit the passage of air up through the larynx and over the vocal cords so the individual cannot speak (produce sound) [26]. The diameter, length, and type of tracheostomy tube as well as factors such as the amount of ventilator dependence for patients on mechanical ventilation via a tracheostomy all affect the ability of a patient to regain speech; therefore, methods to help restore speech vary considerably [27, 28]. Some methods include a speaking valve, tracheostomy button, and cuff deflation, but all methods have pros and cons, and the process is extremely patient specific [28].
The existing research suggests regaining speech is of the utmost importance to recovering patients [5, 13]. The initial inability to communicate via speech causes anxiety, fear, frustration, and powerlessness [5, 21]. Lack of privacy due to having to rely on a third party in communication made participants in one reviewed study feel controlled and lacking integrity [13]. Donnelly and Wiechula [17] reported that patients found the experience of loss of speech more distressing than the discomfort of the actual tracheotomy procedure and other ICU procedures.
In a study by Flinterud and Andershed [21], patients recounted their distress at waking up in an unfamiliar situation, unable to speak. The distress was in some cases exacerbated by the person at first not realising they could not speak and becoming increasingly agitated as they tried to talk louder and louder with no success. Other participants described the excruciating pain they had, but were unable to communicate to health care professionals, and the feeling of loss of control because of their inability to speak. Although communication became easier over time, some participants reported that the period during which they were unable to speak felt as though time had stood still and they were fearful of never being able to speak again [21]. Regaining oral communication was a central issue and a matter of urgency for individuals receiving home mechanical ventilation (HMV) via tracheostomy [13]. Periods of voicelessness were often experienced as loss, and getting one’s voice back was described as exhilarating, bringing relief, and a sense of pleasure [13, 17]. Participants in Laakso et al.’s [13] study saw being able to speak again as a way of regaining control, regaining their ability to express their opinions and emotions, power and independence. Freeman-Sanderson et al. [29] recently found that the return of voice in mechanically ventilated tracheostomy patients in the ICU was associated with significant improvement in areas of self-esteem such as cheerfulness and ability to be understood by others. Participants who had had living experiences of a tracheostomy in a study by Foster [5] also saw verbal communication as fundamental for social interaction. Writing and other non-verbal forms of communication were often found to be frustrating as they required coordination, physical strength, mental effort, and a willingness that many voiceless individuals did not have at the time [5, 21].
Ineffective communication has been suggested to be a barrier to ideal patient treatment due to patients’ inability to voice their needs and wishes [30, 31]. Research points to the inconsistency in staff education around communication and regaining speech [32], and the limited knowledge regarding the continued issues with mastering speech after discharge [13, 25]. Participants in Laakso et al.’s [13] study who were mechanically ventilated through a tracheostomy reported feeling frustrated and frightened due to not getting enough support from health professionals in improving their communication, both during and after HMV. They described how they had to come up with their own strategies to adapt to the changes in their speech and solve communication problems through learning by doing.
Both patients and their carers reported having to deal with various communication limitations, including the patient having a weak, monotonous, unintelligible or different-sounding voice compared to that before the tracheostomy, the patient having slow and interrupted speech, and the frustration around not being able to understand the person’s speech and the person not being able to be understood [13, 17, 25].
In the studies by Flinterud and Andershed [21] and Laakso et al. [13], participants described how they at first had to repeatedly use different strategies (such as mouthing words, using sounds, such as lip or tongue clicking or whistling) to communicate the same thing to family members and health professionals, which they found incredibly frustrating, defeating, and exhausting. They emphasised the importance of having close family members who were familiar with their gestures and body language involved in their initial efforts to communicate. Family members also reported developing communication strategies to better understand the tracheostomised individual they cared for [15, 21, 25]. Examples of these included asking closed questions when communicating, being physically close to the person and maintaining eye contact with them, lip reading, repeating the person’s utterances back to them, and ensuring the surroundings were quiet. Family carers often saw themselves as communication facilitators and enablers, interpreters, and advocates for the person living with a tracheostomy [25].
Communication did improve over time as individuals got stronger and developed new strategies for communicating with their family members and health professionals, as well as with the use of various communication aids (such as speaking valves, digital devices, and mirrors in the car to ensure eye contact, or alarms to ensure the individual could call for attention) [21, 25]. Laakso et al.’s [13] participants emphasised the importance of actually speaking in order to better their speech and attune the people they communicated with to it, as they often felt speaking was the only way they could make themselves heard and seen.
3.3 Wellbeing and Quality of Life
Sherlock et al. [16] note that ‘tracheostomy is potentially much more physically and psychologically traumatic for patients than clinicians may be aware of’ (p. 507). Studies point to individuals struggling with regaining confidence and returning to life as they knew it before tracheostomy [13, 15]. Participants reported that the physical and psychological effects were more disturbing than they expected, especially if the procedure was done non-electively, and despite initially accepting a tracheostomy as being necessary and even welcomed for survival [14, 16]. In one study, participants recounted how having a tracheostomy worsened existing problems, such as depression, and brought about new ones, the most frequently mentioned being disability for work [13]. None of the participants in this study returned to work post-tracheostomy, citing their employers’ reluctance to rehire them due to concerns around compensation litigation.
Participants in a study by Ashley [18] described their emotional turmoil at not being able to engage in physical activities they enjoyed prior to getting a tracheostomy. Shortness of breath often prevented them from running, heavy lifting, and winter sports, while fear of drowning made them fearful of water sports. Anxiousness around how to deal with the tracheostomy tube if she became breathless made one person reluctant to leave the house even for short trips, despite her husband always accompanying her [15]. Travelling restrictions were also an issue reported by those tracheostomised individuals who had to transport equipment if they needed oxygen [18].
A few researchers reported on how individuals often developed strategies to cope with a tracheostomy that improved their mood and self-esteem and helped them reintegrate into society. In the study by Flinterud and Andershed [21], individuals who were tracheostomised while in the ICU recounted how they used humour to get them through and tried to stay calm and informed about when their tube would be removed. Participants in the study by Laakso et al. [13] who received HMV reported going back to work or school after they regained their voice, despite still experiencing some physical and communication restrictions. Making equipment for managing the tracheostomy portable and having a family member take over strenuous household tasks and assist with tube issues enabled one family to regain the confidence to return to the lifestyle they had prior to tracheostomy [15].
Restrictions in daily activities were not only reported by individuals with tracheostomies, but also by their primary carers and family members. At a rehabilitation facility, researchers exploring the experiences of lay principal caregivers of inpatients and outpatients who had undergone tracheostomies found that female caregivers and those caring for patients who had their tracheostomies less than 14 months ago experienced the greatest strain [23]. Carers surveyed in this study reported having restricted outdoor leisure activities; 75% of them said they never went to the cinema or went walking or cycling. Despite leading a very restricted personal life and experiencing fear, anxiety, and insecurities related to the responsibilities of caring for someone with a tracheostomy, family members often saw their situation as helping their personal growth and making them become more skilled communicators [25]. Nearly all the interviewees in this study reported caring for their loved one made them feel good; they thought the person with a tracheostomy experienced more psychosocial distress than they did, including feeling like they were a burden on their family.
There is an abundance of health-related quality of life (HRQoL) measures used to assess head and neck cancer patients [33]; similar measures have been used to assess long-term mechanically ventilated patients [34] and patients with amyotrophic lateral sclerosis (ALS) [35]. These measures could be adapted to specifically assess individuals with long-term tracheostomy, yet few studies have been undertaken, particularly in the home setting, using empirical measures of either QoL or HRQoL.
Tracheostomy is a treatment procedure performed to alleviate some form of inadequate respiration. Naturally, researchers focus their attention on the physical elements of QoL crucial for survival such as respiration, speech, swallowing, and sleep quality, often in the hope of seeing improvement after the insertion of a tracheostomy tube [14]. Also, tracheostomy is often performed in the ICU, directing research to patient QoL in acute settings [5, 29]. The QoL and psychological wellbeing in general of these individuals appears to take a back seat because of the necessity of the procedure for survival.
In a limited number of studies, empirical measures of QoL involving all three aspects of the concept have been used to assess individuals with long-term tracheostomy. Tracheostomy has been found to have a ‘profoundly negative impact’ on QoL [7] (p. 444). Gul and Karadag [7] investigated QoL in 70 tracheostomised individuals using the Short Form 36 QoL scale [36] that assesses physical function, role limitation due to physical and emotional problems, social functioning, general mental health, vitality, bodily pain and general health perception. As expected, the results indicated the negative influence of tracheostomy on respiration, nutrition, and communication, as well as body image and mental wellbeing. More than half of the patients included in the study stated that after tracheostomy, their sense of smell decreased or completely disappeared, and this influenced them as adversely as the loss of speech function did. Gul and Karadag also found that 66% of participants reported an adverse effect on economic status and 55% reported an adverse effect on social relation. Using the Short Form 12 Health Survey (SF12) [37], Hashmi et al. [14] investigated QoL and self-image in individuals living with a tracheostomy for 6 months or more, compared to participants about to undergo elective tracheotomy. Both mental and physical health scores were lower for those living with the tracheostomy. They also compared pre- and post-tracheostomy scores of the elective tracheostomy group and found that although physical health improved slightly after tracheotomy, mental health declined. In a prospective study by Freeman-Sanderson et al. [29] of experiences of patients who were mechanically ventilated in the ICU, participants reported an improvement in self-esteem after getting their voice back. However, no notable improvement in general health status, confidence, sense of outgoingness, anger, sense of being trapped, optimism, or frustration was reported after the return of their voice. In what the authors termed ‘the first report on tracheostomy related quality of life in noncancer patients’, Gilony et al. [38] (p. 366) investigated wellbeing and body image in 24 individuals living with tracheostomy, 19 decannulated (post-tracheostomy) individuals, and 20 healthy individuals undergoing an unrelated elective surgery. Results showed a significant reduction in life satisfaction among those living with a tracheostomy, which improved only slightly on decannulation. The authors speculated this to be related to personality changes caused by a long-term tracheostomy. Post-tracheostomy, after a long period of obvious neck disfigurement and altered communication, individuals had negative body image perception, became introverted, and had lost their confidence and the ability to seek social support.
Only two studies focused on the factors that could improve the QoL in people with tracheostomy. In the above study by Gul and Karadag [7], those individuals who cared for their own tracheostomy and who used oesophageal speech reported higher QoL. Mohammadi et al. [39] assessed the effectiveness of a self-care training by video method and found that routine training for patient care to watch at home improved QoL (including physical, mental, and social aspects) for 80 tracheostomised patients, compared to those patients receiving only routine care training.
3.4 Disfigurement and Body Image
Disfigurement, especially injuries to the head and neck more so than other body regions, presents a serious psychological and social challenge, impacting body image, sexuality and relationships, QoL, and psychological health [9, 40,41,42]. Tracheostomy involves a prominent disfigurement in the anterior neck that is often permanent, and even if the stoma opening is no longer needed, a scar will most likely prevail. A tracheostomy collar, opening, stoma or scar may seem minor in comparison to severe facial disfigurement. However, research as well as clinical and patient accounts indicate that the level of severity and type of disfigurement do not predict adjustment level [40, 41]. Mild disfigurement can cause as much or more anxiety than highly visible conditions [43]. Milder disfigurement may bring about more variability in reactions from others, resulting in feelings of loss of control over one’s situation and increased anxiety [44]. Furthermore, the closer a disfigurement is to the central triangle of the eyes and mouth, the more noticeable it is to others, and, as Bradbury [45] suggests, ‘a small deficit in a tooth is more noticeable than a similar degree of deficit in the ear’ (p. 194). It is thought that individuals with acquired facial disfigurement have more problems adjusting than individuals with congenital facial deformity [41, 46, 47]. Tracheostomy is an acquired disfigurement, and individuals do not have the possible advantage of adjusting to the disfigurement since birth. Furthermore, in many cases, tracheotomy is performed in emergency settings because of trauma [48], and the individual is completely unprepared for the disfigurement, which may add to the negative impact [49].
Based on studies of colostomy patients, Bronheim et al. [42] concluded that ‘it would reasonably be expected that otolaryngology patients with a tracheostomy stoma might feel injured, penetrated, and preoccupied with the consequences of an artificial orifice in their body’ (p. 226). Yet, there is a paucity of research on the effects of tracheostomy as a form of disfigurement. The limited research that does exist highlights the negative impacts on body image and wellbeing of the affected person. Gilony et al. [38] found significantly lower levels of body image satisfaction in patients at a laryngotracheal clinic with tracheostomies compared to those without. Those patients who scored lower on body image perception also had lower extroversion and higher neuroticism scores—a finding the researchers interpreted as being related to the patients’ personality being affected by ‘a long period of obvious neck disfigurement and altered communication’ (p. 370).
In their survey of 70 patients who have lived with a tracheostomy for at least 3 months, Gul and Karadag [7] found that individuals often experienced shame due to altered physical appearance. Those who stated that their physical appearance had not been affected by the fact that they had a tracheostomy also reported a higher QoL. In the study by Laakso et al. [13], individuals receiving HMV reported experiencing a change in appearance due to a tracheostomy or a nose mask that may have impacted on how they viewed themselves. In other studies, participants who had a lived experience of a tracheostomy saw the tube as bulky, ‘ugly’ and ‘unattractive’, and a ‘visible disfigurement’ that attracted stares from the public and caused a negative self-image [16, 18]. Family carers of people with a tracheostomy also commented on the tube causing embarrassment and psychological distress to those people [23]. In some cases, having to live with a permanent tracheostomy had more impact on family members than on the affected person [15]. Spouses often had difficulty accepting the tracheostomy, and in one case reported in the 1980s, it even led to the couple separating [19].
3.5 Stigma and Social Withdrawal
Inevitable when issues of disfigurement and difference arise are issues of stigma and social exclusion, isolation, and avoidance. Gilbert [50] argues that, due to the fact that social attractiveness has become a very salient feature in our society, we will, where possible, attempt to form alliances with attractive people and avoid alliances with those perceived as unattractive. Stigma occurs when society acts on these innate feelings, leading to a person being labelled as tainted, handicapped, or less desirable [51].
Research on stigma and how the presence of a tracheostomy affects individuals’ social activity is scarce. However, several studies reveal that individuals with tracheostomies often fear others’ reactions and the stigmatisation that their tracheostomies may engender, which tends to lead to social withdrawal. Ashley [18] interviewed seven sleep apnoea patients with tracheostomies who said they felt uncomfortable in public with their tube being visible. This resulted in them trying to conceal the tube, and if this was not possible, they coped by physically withdrawing from social situations. Withdrawal was particularly difficult for more socially active patients. Altered communication and obvious neck disfigurement, as well as persistent coughing, often made people with a tracheostomy feel like they were the focus of attention in their community, were misperceived as being of low intelligence by others and made to feel self-conscious; they felt ashamed, worthless, powerless, mistreated, ignored, and alienated, and consequently, grew increasingly quieter and withdrawn from social situations [5, 13, 38]. Patients who had a tracheostomy for HMV felt that when they had difficulties communicating, people were nervous and afraid of them, had prejudices, or avoided them [13]. Persistent coughing also caused tiredness that left individuals with little energy to socialise with others [5]. Feelings of isolation due to inability to travel and missing out on activities with friends and family were reported by sleep apnoea patients with tracheostomies [18]. Participants in this study reported they found it more comforting to talk informally to other people in a similar situation than to their own family. In a study by Rossi Ferrario et al. [23], out of 63 family caregivers of people with tracheostomies, 84% said that their patients felt ashamed of their condition and avoided social contact as a result. Most caregivers reported having restricted social relationships themselves, hardly ever seeing their friends or going to social meeting places.
4 Discussion
The aim of this review was to explore the literature available on patient and caregiver experiences of tracheostomy, and thereby gain an understanding of the broad challenges faced by individuals who undergo this procedure and their families in order to ensure they enjoy better care and QoL. Despite a limited number of studies reporting either qualitative or quantitative data on the topic, this literature review demonstrates that the treatment and management of tracheostomy have a significant impact on the wellbeing of the patient and their family.
The literature found was commonly centred on tracheostomised patients in an acute (ICU) setting, with fewer studies focusing on the experiences of long-term tracheostomy users and their families. Based on the recounts in the hospital setting, it appears that patients and their families would benefit from being given more information and counselling prior to and immediately after the tracheostomy. Being given the opportunity to establish trust and receive continuous reassurance and support from clinical staff would help alleviate the shock, fear, and anxiety in the emergency cases where tracheostomy is performed without the patient’s prior consent.
Research highlights the disconnect between hospital and home care and the varying competence of health care professionals in the two settings. After a somewhat rough transition at discharge, there appears to be limited knowledge as to how adults with tracheostomies perceive their medical care and professional support after their return into the community. A multidisciplinary team is essential for tracheostomy patients, who may be going through a range of emotions and concerns in their health care journey. Multidisciplinary teams, as championed by the Global Tracheostomy Collaborative (http://www.globaltrach.org)—a nonprofit international quality improvement initiative that includes benchmarking data collection that fosters multidisciplinary team care as a key driver—is a helpful organising principle that is increasingly being adopted internationally and can do much to alleviate the potentially profound distress of these patients. Early involvement of multidisciplinary care teams can improve clinical outcomes and patient satisfaction, mainly by reducing time needed to restore speech [52]. Clear and substantial evidence highlights a desperate need for effective ways for recently tracheostomised voiceless patients to communicate. Alternative methods of communicating do exist in ICU environments, such as lip-reading, writing, hand signals, and picture boards [53, 54], as well as high-tech aids such as apps, tablets, and other electronic devices [55]. These methods can be useful for enabling patients to express basic needs, although they do not fully encompass the reciprocal nature of human communication [30, 56]. Furthermore, it has been suggested that these aids are rarely utilised [57]. A patient-specific communication plan should be at the patient’s bedside [53], and technological methods of communication should be further explored. Staff in the ICU should be comfortable and confident in dealing with patients who are unable to speak; however, literature suggests that nurses, despite their knowledge and experience, continue to find it difficult to communicate with critically ill and voiceless patients [58, 59]. This view was largely shared by the patients in the reviewed studies.
Research is extremely limited regarding the QoL of individuals living with long-term tracheostomy. The scant research that is available speaks of the negative impacts that ensue [7, 14]. This review included studies in which participants underwent tracheostomies for a variety of reasons. This encompasses individuals on HMV and individuals with neuromuscular diseases that affect respiration, such as ALS. This poses a possible limitation and highlights a hurdle in tracheostomy research. It is acknowledged that subjects with different types of respiratory disorders may have varying perceptions of QoL [1]. Furthermore, the severity of the disease responsible for the tracheostomy will likely contribute to QoL [1].
Distress, anxiety, self-esteem, ability to adjust, and coping skills in patients with disfigurement due to diseases such as head and neck cancer [60, 61], ptosis [62], and other disfiguring conditions [63] have been acknowledged and researched extensively. Body image assessment tools have developed [64] and intervention programmes have been suggested [65, 66]. The negative impacts of disfigurement were largely ignored in those with tracheostomies, which are often more visible and certainly of equal functional importance. The ways in which people experience issues of disfigurement and dysfunction vary greatly and depend on many factors, such as their cultural background [67] and their gender [60]. Research in numerous areas of psychopathology highlights the importance of identifying those at higher risk of developing problems and requiring additional support [68]. It is known that psychological symptoms after facial trauma occur more in women than men as facial appearance and disfigurement concerns are more prevalent in women [10]. In studies of individuals with head and neck cancer, women have been found to experience poorer appearance-related adjustment to disfigurement than men [60, 69] and have been found to be more susceptible to emotional distress [61]. In view of these findings, the gender differences related to how people experience the adverse effects of tracheostomy need further investigation.
The importance of addressing the psychosocial effects of disfigurement is clear from research on patients with other bodily and facial disfigurements. Despite their interest to acquire the appropriate skills, it has been noted that medical staff feel ill-equipped to deal with the needs of patients with disfigurement and that the psychosocial needs of outpatients with disfigurement are not being met [40]. Suggestions have been made that hospital staff working with patients with disfigurement should have an understanding of their unique needs and there should be access to an identified staff member with counselling skills and a recognised route to a psychologist [40, 45]. Until more research is conducted, we may only infer the effects of disfigurement on those living with tracheostomies and conclude that they should be included in this group of individuals in need of specific psychological care.
The importance of social acceptance and support within the community has been highlighted in the reviewed studies. Social support has been associated with better adjustment levels in individuals with a range of disfiguring conditions [8, 70]. Social isolation and withdrawal may also be reduced with the help of social support groups. Social media sites such as those on Facebook have been found to be a promising source of support for teenagers with tracheostomies [71]. An investigation into the presence and application of support groups both on- and offline may inform further initiatives to reduce the stigmas that people with differences due to tracheotomy surgery are faced with.
Patient-focused qualitative research may provide insight into patient needs and preferences and serve to assist in the evaluation of new treatments. Research specific to tracheostomy is needed so we can go further than hypothesise the subsequent impacts of the procedure, which are undoubtedly suggested as being broadly adverse by the limited existing research. To fully understand these adverse impacts, more research is needed with emphasis on individuals with long-term tracheostomies living in the community. Further research may highlight characteristics that put individuals at increased risk of these adverse impacts and inform initiatives and interventions to address them. This research could also inform projects in a broad scope of disciplines such as communication and product design and impel collaborations from professionals both academic and clinical.
5 Conclusion
Little data exist on the first-hand experiences of tracheostomy. There is a need to deepen our understanding of these experiences to develop tools and strategies to better support patients and their families both practically and emotionally while in the hospital and upon return to the community.
References
Bello G, Di Muzio F, Antonelli M. Quality of life and complications after percutaneous tracheostomy. In: Servillo G, Pelosi P, editors. Percutaneous tracheostomy in critically ill patients. Switzerland: Springer; 2016. p. 131–47.
Feber T. Tracheostomy care for community nurses: basic principles. Br J Community Nurs. 2006;11(5):186–93.
Garrubba M, Turner T, Grieveson C. Multidisciplinary care for tracheostomy patients: a systematic review. Crit Care. 2009;13(6):R177.
Shah RK, Lander L, Berry JG, Nussenbaum B, Merati A, Roberson DW. Tracheotomy outcomes and complications: a national perspective. Laryngoscope. 2012;122(1):25–9.
Foster A. More than nothing: the lived experience of tracheostomy while acutely ill. Intensive Crit Care Nurs. 2010;26(1):33–43.
Bowers B, Scase C. Tracheostomy: facilitating discharge from hospital to home. Br J Nurs. 2007;16(8):476–9.
Gul ND, Karadag A. An evaluation of the quality of life in patients with tracheostomy. Pak J Med Sci Q. 2010;26:444–9.
Rumsey N, Clarke A, White P, Wyn-Williams M, Garlick W. Altered body image: appearance-related concerns of people with visible disfigurement. J Adv Nurs. 2004;48(5):443–53.
Rumsey N, Harcourt D. Body image and disfigurement: issues and interventions. Body Image. 2004;1(1):83–97.
Thomas CS, Goldberg DP. Appearance, body image and distress in facial dysmorphophobia. Acta Psychiatr Scand. 1995;92:231–6.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psych. 2006;3(2):77–101.
Garner JM, Shoemaker-Moyle M, Franzese CB. Adult outpatient tracheostomy care: practices and perspectives. Otolaryngol Head Neck Surg. 2007;136(2):301–6.
Laakso K, Markstrom A, Idvall M, Havstam C, Hartelius L. Communication experience of individuals treated with home mechanical ventilation. Int J Lang Commun Disord. 2011;46(6):686–99.
Hashmi NK, Ransom E, Nardone H, Redding N, Mirza N. Quality of life and self-image in patients undergoing tracheostomy. Laryngoscope. 2010;120(4):S196.
Barnett M. Adapting to living with a tracheostomy. J Community Nurs. 2006;20(1):4–8.
Sherlock ZV, Wilson JA, Exley C. Tracheostomy in the acute setting: patient experience and information needs. J Crit Care. 2009;24(4):501–7.
Donnelly F, Wiechula R. The lived experience of a tracheostomy tube change: a phenomenological study. J Clin Nurs. 2006;15(9):1115–22.
Ashley MJ. Concerns of sleep apnea patients with tracheostomies. West J Nurs Res. 1989;11(5):600–8.
Conway WA, Victor LD, Magilligan DJ Jr, Fujita S, Zorick FJ, Roth T. Adverse effects of tracheostomy for sleep apnea. JAMA. 1981;246(4):347–50.
Dye JP. Living with a tracheostomy for sleep apnea. N Engl J Med. 1983;308(19):1167–8.
Flinterud SI, Andershed B. Transitions in the communication experiences of tracheostomised patients in intensive care: a qualitative descriptive study. J Clin Nurs. 2015;24(15–16):2295–304.
McCormick ME, Ward E, Roberson DW, Shah RK, Stachler RJ, Brenner MJ. Life after tracheostomy: patient and family perspectives on teaching, transitions, and multidisciplinary teams. Otolaryngol Head Neck Surg. 2015;153(6):914–20.
Rossi Ferrario S, Zotti AM, Zaccaria S, Ferdinando D. Caregiver strain associated with tracheostomy in chronic respiratory failure. Clin Investig Crit Care. 2001;119:1498–502.
Paul F. Tracheostomy care and management in general wards and community settings: literature review. Nurs Critic Care. 2010;15(2):76–85.
Laakso K, Markstrom A, Havstam C, Idvall M, Hartelius L. Communicating with individuals receiving home mechanical ventilation: the experiences of key communication partners. Disabil Rehabil. 2014;36(11):875–83.
Shikani AH, Dietrich-Burns K. Comparison of speech parameters and olfaction using different tracheotomy speaking valves. Int Forum Allergy Rhinol. 2012;2(4):348–53.
Hess DR. Facilitating speech in the patient with a tracheostomy. Respir Care. 2005;50(4):519–25.
Morris LL, Bedon AM, McIntosh E, Whitmer A. Restoring speech to tracheostomy patients. Crit Care Nurse. 2015;35(6):13–28.
Freeman-Sanderson AL, Togher L, Elkins MR, Phipps PR. Quality of life improves with return of voice in tracheostomy patients in intensive care: An observational study. J Crit Care. 2016;33:186–91.
Guttormson JL, Bremer KL, Jones RM. “Not being able to talk was horrid”: a descriptive, correlational study of communication during mechanical ventilation. Intens Crit Care Nurs. 2015;31(3):179–86.
Rattray J, Crocker C, Jones M, Connaghan J. Patients’ perceptions of and emotional outcome after intensive care: results from a multicentre study. Nurs Crit care. 2010;15(2):86–93.
Ward E, Agius E, Solley M, Cornwell P, Jones C. Preparation, clinical support, and confidence of speech-language pathologists managing clients with a tracheostomy in Australia. Am J Speech Lang Pathol. 2008;17(3):265–76.
Ojo B, Genden EM, Teng MS, Milbury K, Misiukiewicz KJ, Badr H. A systematic review of head and neck cancer quality of life assessment instruments. Oral Oncol. 2012;48(10):923–37.
Euteneuer S, Windisch W, Suchi S, Kohler D, Jones PW, Schonhofer B. Health-related quality of life in patients with chronic respiratory failure after long-term mechanical ventilation. Respir Med. 2006;100(3):477–86.
Kaub-Wittemer D, Steinbüchel NV, Wasner M, Laier-Groeneveld G, Borasio GD. Quality of life and psychosocial issues in ventilated patients with amyotrophic lateral sclerosis and their caregivers. J Pain Symptom Manage. 2003;26(4):890–6.
Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976). 2000;25(24):3130–9.
Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Gilony D, Gilboa D, Blumstein T, Murad H, Talmi YP, Kronenberg J, et al. Effects of tracheostomy on well-being and body-image perceptions. Otolaryngol Head Neck Surg. 2005;133(3):366–71.
Mohammadi N, Farahani M, Vatandost S. Effect of videotape for home instruction on the quality of life of tracheostomy patients: a randomized clinical trial. J Med Life. 2015;8(4):287–94.
Rumsey N, Clarke A, White P. Exploring the psychosocial concerns of outpatients with disfiguring conditions. J Wound Care. 2003;12(7):247–52.
Thompson A, Kent G. Adjusting to disfigurement: processes involved in dealing with being visibly different. Clin Psychol Rev. 2001;21(5):663–82.
Bronheim H, Strain JJ, Biller HF. Psychiatric aspects of head and neck surgery part II: body image and psychiatric intervention. Clin Hosp Psychiat. 1991;13:225–32.
Macgregor FC. Facial disfigurement: problems and management of social interaction and implications for mental health. Aesthetic Plast Surg. 1990;14(1):249–57.
Lansdown R. Visibly different: coping with disfigurement. Oxford; Boston: Butterworth-Heinemann; 1997.
Bradbury E. Meeting the psychological needs of patients with facial disfigurement. Br J Oral Maxillofac Surg. 2012;50(3):193–6.
Robinson E, Rumsey N, Partridge J. An evaluation of the impact of social interaction skills training for facially disfigured people. Br J Plast Surg. 1996;49(5):281–9.
Sarwer DB, Wadden TA, Pertschuk MJ, Whitaker LA. The psychology of cosmetic surgery: a review and reconceptualization. Clin Psychol Rev. 1998;18(1):1–22.
Shirawi N, Arabi Y. Bench-to-bedside review: early tracheostomy in critically ill trauma patients. Crit Care. 2006;10(1):201.
Newell R. Psychological difficulties amongst plastic surgery ex-patients following surgery to the face: a survey. Br J Plast Surg. 2000;53:386–92.
Gilbert P. The evolution of social attractiveness and its role in shame, humiliation, guilt and therapy. Br J Med Psychol. 1997;70(2):113–47.
Goffman E. Stigma notes on the management of spoiled identity. New York: J. Aronson; 1974.
Freeman-Sanderson A, Togher L, Phipps P, Elkins M. A clinical audit of the management of patients with a tracheostomy in an Australian tertiary hospital intensive care unit: focus on speech-language pathology. Int J Speech Lang Pathol. 2011;13(6):518–25.
Grossbach I, Stranberg S, Chlan L. Promoting effective communication for patients receiving mechanical ventilation. Crit Care Nurse. 2011;31(3):46–60.
Patak L, Gawlinski A, Fung NI, Doering L, Berg J. Patients’ reports of health care practitioner interventions that are related to communication during mechanical ventilation. Heart Lung. 2004;33(5):308–20.
Finke EH, Light J, Kitko L. A systematic review of the effectiveness of nurse communication with patients with complex communication needs with a focus on the use of augmentative and alternative communication. J Clin Nurs. 2008;17(16):2102–15.
Batty S. Communication, swallowing and feeding in the intensive care unit patient. Nurs Crit Care. 2009;14(4):175–9.
Happ MB, Garrett KL, Tate JA, DiVirgilio D, Houze MP, Demirci JR, et al. Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart Lung. 2014;43(2):89–98.
Leathart AJ. Communication and socialisation (1): an exploratory study and explanation for nurse-patient communication in an ITU. Intensive Crit Care Nurs. 1994;10(2):93–104.
Rodriguez CS, Spring HJ, Rowe M. Nurses’ experiences of communicating with hospitalized, suddenly speechless patients. Qual Health Res. 2015;25(2):168–78.
Clarke SA, Newell R, Thompson A, Harcourt D, Lindenmeyer A. Appearance concerns and psychosocial adjustment following head and neck cancer: a cross-sectional study and nine-month follow-up. Psychol Health Med. 2014;19(5):505–18.
Singer S, Krauss O, Keszte J, Siegl G, Papsdorf K, Severi E, et al. Predictors of emotional distress in patients with head and neck cancer. Head Neck. 2012;34(2):180–7.
Richards HS, Jenkinson E, Rumsey N, White P, Garrott H, Herbert H, et al. The psychological well-being and appearance concerns of patients presenting with ptosis. Eye. 2014;28(3):296–302.
Pope SJ, Solomons WR, Done DJ, Cohn N, Possamai AM. Body image, mood and quality of life in young burn survivors. Burns. 2007;33(6):747–55.
Fingeret MC, Teo I, Goettsch K. Body image: a critical psychosocial issue for patients with head and neck cancer. Curr Oncol Rep. 2015;17(1):422.
Callahan C. Facial disfigurement and sense of self in head and neck cancer. Soc Work Health Care. 2005;40(2):73–87.
Rumsey N, Bull R, Gahagen D. A preliminary study of the potential of social skills for improving the quality of social interaction for the facially disfigured. Soc Behav. 1986;1:143–5.
McLellan KM, McCann CM, Worrall LE, Harwood MLN. “For Māori, language is precious. And without it we are a bit lost”: Māori experiences of aphasia. Aphasiology. 2013;28(4):453–70.
Dennis CL, Janssen PA, Singer J. Identifying women at-risk for postpartum depression in the immediate postpartum period. Acta Psychiatr Scand. 2004;110(5):338–46.
Katz MR, Irish JC, Devins GM, Rodin GM, Gullane PJ. Psychosocial adjustment in head and neck cancer: the impact of disfigurement, gender and social support. Head Neck. 2003;25(2):103–12.
Kleve L, Rumsey N, Wyn-Williams M, White P. The effectiveness of cognitive-behavioural interventions provided at Outlook: a disfigurement support unit. J Eval Clin Pract. 2002;8(4):387–95.
Madan G, Stadler ME, Uhrich K, Reilly C, Drake AF. Adolescents with tracheostomies–communications in cyberspace. Int J Pediatr Otorhinolaryngol. 2011;75(5):678–80.
Author information
Authors and Affiliations
Contributions
INK was involved in conception and planning, acquisition of data, analysis and interpretation of data, and drafting and revision of the manuscript. NP participated in the conception and planning, analysis and interpretation of data, and drafting of the manuscript. JW was involved in the conception and planning, interpretation of data, and revision of the manuscript. SR was involved in conception and planning and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
The study was funded by an Auckland University of Technology Strategic Research Investment Fund award 2016.
Conflict of interest
INK has no conflict of interest to declare. NP has no conflict of interest to declare. JW has no conflict of interest to declare. SR has no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Nakarada-Kordic, I., Patterson, N., Wrapson, J. et al. A Systematic Review of Patient and Caregiver Experiences with a Tracheostomy. Patient 11, 175–191 (2018). https://doi.org/10.1007/s40271-017-0277-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-017-0277-1