Abstract
Background
Preventive chemotherapy with a single dose of praziquantel given to an all-at-risk population through mass drug administration is the cornerstone intervention to control and eliminate schistosomiasis as a public health problem. This intervention mainly targets school age children, and pre-school age children (pre-SAC) are excluded from receiving preventive chemotherapy, partly due to scarcity of data on praziquantel treatment outcomes.
Methods
We conducted active efficacy and safety surveillance of praziquantel treatment among 240 Schistosoma mansoni-infected pre-SAC who received a single dose of praziquantel (40 mg/kg) in southern Ethiopia. The study outcomes were egg reduction rates (ERR) and cure rates (CRs) four weeks after treatment using the Kato–Katz technique and treatment-associated adverse events (AEs) that occurred within 8 days post-treatment.
Results
The overall ERR was 93.3% (WHO reference threshold ≥ 90%), while the CR was 85.2% (95% CI = 80.0–89.5%). Baseline S. mansoni infection intensity was significantly associated with CRs, 100% among light infected than moderate (83.4%) or heavy (29.4%) infected children. An increase of 100 in baseline S. mansoni egg count per gram of stool resulted in a 26% (95% CI: 17%, 34%) reduction in the odds of cure. The incidence of experiencing at least one type of AE was 23.1% (95% CI: 18.0%, 29.0%). Stomachache, diarrhea, and nausea were the most common AEs. AEs were mild-to-moderate grade and transient. Pre-treatment moderate (ARR = 3.2, 95% CI: 1.69, 6.14) or heavy infection intensity (ARR = 6.5, 95% CI: 3.62, 11.52) was a significant predictor of AEs (p < 0.001). Sex, age, or soil-transmitted helminth coinfections were not significant predictors of CR or AEs.
Conclusions
Single-dose praziquantel is tolerable and effective against S. mansoni infection among pre-SAC, and associated AEs are mostly mild-to-moderate and transient. However, the reduced CR in heavily infected and AEs in one-fourth of S. mansoni-infected pre-SAC underscores the need for safety and efficacy monitoring, especially in moderate-to-high infection settings. Integrating pre-SACs in the national deworming programs is recommended to accelerate the elimination of schistosomiasis as a public health problem.
Similar content being viewed by others
Background
Schistosomiasis is a common Neglected Tropical Disease (NTD) and a public health problem in the tropical and subtropical regions of Africa, Asia, the Caribbean, and South America, mainly affecting poor and rural communities [1]. Sub-Saharan Africa (SSA) is the most significantly affected continent, bearing more than 90% of the global burden of schistosomiasis, with an estimated annual death rate of 280,000 and 800 million people at risk of infection [2,3,4]. In SSA, intestinal schistosomiasis is mainly caused by Schistosoma mansoni infection, and children living in poor communities without access to safe drinking water and adequate sanitation are the most affected population. The disease can cause growth retardation, fatigue, weakness, memory impairment, anemia, poor cognition, and academic performance in infected children [4, 5]. In Ethiopia, schistosomiasis is a major public health problem causing marginalization and stigmatization, as well as a social and economic burden [6]. Schistosomiasis is highly prevalent in Ethiopia, affecting mostly preschool-aged children (pre-SAC) and school-aged children (SAC) children [7,8,9]. The revised NTD master plan aims to halt transmission of S. mansoni infection and eliminate the disease as a public health problem by 2025 [6].
For over 40 years, praziquantel (PZQ) has been the only approved drug by the World Health Organization (WHO) to treat schistosomiasis [10]. Except for the ongoing clinical trials, no approved vaccine for preventing schistosomiasis is on the market to date [11]. The WHO guideline recommends large-scale periodic administration of single-dose PZQ and albendazole combination to all at-risk populations in endemic areas through mass drug administration (MDA) as a preventive chemotherapy to control and halt transmission of S. mansoni and soli-transmitted helminths (STH) infections, respectively [10, 12]. In 2021, 75.3 million people received treatment for schistosomiasis in endemic areas worldwide, of which 94% of all therapy delivered globally was in the African region [13].
The MDA programs mainly target SAC and pre-SAC are excluded from deworming programs due to limited PZQ safety and efficacy information in this age group and the lack of suitable pediatric formulation [14]. Recognizing the unmet medical needs of schistosome-infected pre-SAC, a public–private partnership called Pediatric Praziquantel Consortium was formed to develop an oral dispersible tablet formulation of PZQ to treat pre-SAC infected with schistosomiasis. This Consortium supports the WHO strategic plan for schistosomiasis control and elimination in children [15]. Over a decade of annual school-based deworming with single-dose PZQ, MDA with scaled-up coverage resulted in a significant decrease in the number of disability-adjusted life years lost due to schistosomiasis [16]. However, the reduction has been less in pre-SAC mainly because they are not targeted for MDA [16]. Hence, the inclusion of pre-SAC in mass PZQ administration remains a priority to reduce the possible source of re-infection to at-risk populations covered with MDA and the occurrence of chronic schistosomiasis among pre-SAC. The safety and effectiveness of single-dose PZQ and associated factors are well-documented in SAC, but data are scarce from pre-SAC [17,18,19,20]. Few studies that assessed single-dose PZQ in pre-SAC reported its safety and tolerability but with varying egg reduction rate (ERR) and cure rate (CR) [21,22,23,24,25]. The most frequently reported adverse events (AEs) include abdominal pain, vomiting, nausea, dizziness, and diarrhea. The type and frequency of treatment-related AEs vary among populations due to genetic differences, nutritional status, age, intensity of infection, and other factors [17,18,19,20].
Preventive chemotherapy with single-dose PZQ is crucial to control and eliminate schistosomiasis as a public health problem and to fulfill the WHO strategy—Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Tropical Diseases 2021–2030 [26]. Achieving this goal relies, among others, on drug effectiveness and scaling up the program to involve all at-risk groups since untreated infected individuals can serve as parasite reservoirs for continued transmission in the community. The recent WHO guideline recommends the inclusion of pre-SAC in mass PZQ administration starting from the age of 2 years based on the efficacy and safety evidence reported from SAC and adult studies [1]. In the absence of other treatment alternatives, a single dose of PZQ of 40 mg/kg, which is recommended by the WHO for S. mansoni infections in SAC, is suggested for pre-SAC with proper efficacy and safety monitoring [22, 27]. Establishing the safety and efficacy of PZQ in pre-SAC children is urgently needed to inform the national NTD program and policymakers before nationwide scaling up of the intervention in this vulnerable age group. Therefore, the present study investigated the efficacy and safety of PZQ among S. mansoni-infected pre-SAC in southern Ethiopia.
Methods
Study area, setting, and design
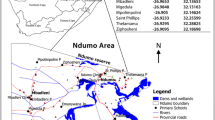
A facility-based efficacy and safety surveillance study was conducted among pre-SAC (children aged 4–7 years) who were identified positive for S. mansoni infection during the baseline screening using Kato–Katz for S. mansoni infection in Hawella Tulla district, Sidama Region, southern Ethiopia. The study was conducted during August to December 2021 at Bushulo Health Center with comprehensive pediatric healthcare services, including laboratory facility enrolling cases linked from three catchment villages/kebeles (lowest administrative units in Ethiopia). The villages were Tullo, Finchawa, and Chefe Kotijebesa. According to the results of NTD mapping done in Ethiopia [28], these villages were categorized as high schistosomiasis prevalent areas.
The sample size based on anticipated ERR was estimated using G* power sample size calculation software. The assumptions used from a previous study [29] conducted among SAC were arithmetic mean (AM) ± standard deviation (SD) of egg count before and after treatment being 365.06 ± 437.8 and 78.6 ± 65.6 respectively, power of 0.9, alpha (α) of 0.05, effect size of 0.2, and within-subject correlation of 0.5. The smaller effect size of 0.2 was considered to get a larger sample size, and the total sample size was 265. However, during the baseline screening for S. mansoni infection, 241 children tested positive for S. mansoni and constituted the final sample.
Study population
The study population were pre-SAC diagnosed with S. mansoni infection. The eligibility criteria for enrollment were being S. mansoni-infected aged 4–7 years, living in the study area permanently, and whose parents or primary caregivers gave written consent. Pre-SAC with known chronic medical conditions confirmed by the study physician on the day of the treatment were excluded from the study. Children who received PZQ treatment within the past 4 weeks and those who participated in any other drug trial during the data collection period were excluded to avoid the impact of other medications on the study. Except for one child who received PZQ before enrollment, all S. mansoni-infected pre-SAC from the three villages were enrolled for PZQ efficacy and safety evaluation.
Diagnosis, treatment, and follow-up
The study employed a community-based recruitment strategy that involved screening of pre-SAC at households in the catchment area of the health center. A total of 1683 pre-SAC (4 to 7 years old) residing at three study villages in the Hawella Tulla district of southern Ethiopia were screened for S. mansoni infection using the Kato–Katz technique. S. mansoni-infected pre-SAC were linked to the health facility to get treatment. Children diagnosed with S. mansoni infection (n = 241) were recruited and enrolled in this safety and efficacy surveillance study. After recording baseline sociodemographic data including age, sex, and medical history including pre-existing clinical symptoms, and comorbidities, concomitant medications, participants received a single dose of PZQ (40 mg/kg) as recommended by WHO [30]. Praziquantel 600 mg tablets (Batch M00761, Merck KGaA, Darmstadt, Germany) were obtained from the Ethiopian NTD control program. After meal intake, the treating physician gave each child the appropriate dosage calculated based on the child’s body weight. The tablet was crushed with a mortar and pestle, and the powder was mixed and suspended in 10 ml of syrup-flavored water to mask the bitter taste. Crushing of the tablets avoids the risk of choking, which is a potential adverse event in pre-SAC and helpful to make suspension with syrup-flavored water [31]. The appropriate 40 mg/kg PZQ treatment was given to each participant through direct observed therapy by a trained nurse who prepared the medication. Study participants were followed for 8 days to monitor any treatment-associated adverse events, and efficacy was monitored at 4 weeks post-treatment as described previously [17, 20, 30, 32].
Stool exam using Kato–Katz technique
A single fresh stool sample was collected both at the baseline (pre-treatment) for diagnosis 4 weeks after drug administration (28 days) for monitoring drug efficacy in terms of ERR and CR following the WHO guideline for assessing the efficacy of anthelminthic drugs against schistosomiasis [30]. The stool samples were assessed through duplicate Kato–Katz thick smears (standard template of 41.7 mg) and S. mansoni eggs per gram of stool (EPG) was calculated by multiplying the mean egg count by a constant factor of 24 [33]. S. mansoni infection intensities were classified according to light infection (EPG < 100), moderate infection (EPG 100–399), and heavy infection intensities (EPG ≥ 400) following the WHO guideline, as per the recommendation of the WHO [30].
Assessment of treatment-associated adverse events
Study participants were closely monitored for any treatment-associated AEs, including gastrointestinal, neurological, and dermatological symptoms within 4, 24, and 192 h of drug administration. The intensities of the reported AEs were graded as mild, moderate, and severe. Severity grading of treatment-associated AEs was done using the following Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0 [34]:
-
Grade 1 (mile): asymptomatic or mild symptoms that require clinical or diagnostic observations only, with no indication of intervention.
-
Grade 2 (moderate): moderate AEs limiting age-appropriate Instrumental Activities of Daily Living (ADL); minimal, local, or non-invasive interventions indicated.
-
Grade 3 (severe): severe or medically significant AEs not immediately life-threatening but that are disabling and/or limiting self-care ADL. Hospitalization or prolongation of hospitalization indicated.
-
Grade 4 (serious)—comprises life-threatening consequences with an indication of urgent intervention.
-
Grade 5—death related to AE.
Before the commencement of the study, referral arrangements to a health facility with specialized pediatric care were in place for study participants with definite or suspected serious AEs (any event > grade 2) for further evaluation.
Study outcomes
The primary study outcome was efficacy (ERR and CR) based on the thick smear Kato–Katz method at 4 weeks post-treatment. The ERR was calculated as 100 times [1 − (Arithmetic mean egg counts at follow-up/Arithmetic mean egg counts at baseline)] per the recommendation of the WHO [30]. The CR was determined as the proportion of infected (egg-positive) children before treatment who became egg-free (egg-negative) at 4 weeks post-treatment. The secondary outcome was treatment-associated AEs experienced or reported within 8 days of drug administration. The major exposure variable was PZQ treatment administered in a single dose of 40 mg/kg. Other covariates for efficacy and safety included age, sex, and co-infection with the three common STHs: hookworm, Ascaris lumbricoides, and Trichuris trichuria.
Statistical analysis
All data were recorded on standard record forms, entered the RedCap database, and exported to an Excel file for cleaning. The data analysis was done using Stata version 14 (StataCorp LLC, College Station, Texas, US). Descriptive analyses were done by calculating frequencies and percentages for categorical variables, mean with standard deviations and medians with interquartile ranges for continuous variables. Associations between cure rates and predictor variables were analyzed using binary logistic regression. Predictors of the cure rate for S. mansoni infection were analyzed using univariate followed by multivariate logistic regression.
All predictor variables in the univariate analyses were entered into the multivariate model. Adjusted odds ratios (AORs) with a 95% confidence interval (CIs) were reported based on the multivariable logistic regression model. Safety data were analyzed using descriptive statistics and presented in tables and graphs. The log-binomial regression was used to analyze the associations between having any AEs or not with predictor variables. Variables with a p value ≤ 0.25 on the crude analysis were included in the multivariable log-binomial regression model. Adjusted risk ratios (ARRs) with 95% confidence intervals (CIs) were reported based on the multivariable log-binomial model. A p value ≤ 0.05 was considered statistically significant.
Results
Sociodemographic and baseline characteristics
A total of 1683 pre-SAC were screened for S. mansoni infection, and 241 (14.3%) had detectable S. mansoni infection. Infected children (n = 240) were enrolled in this safety and efficacy surveillance study and one child who had received PZQ treatment before enrollment was excluded from the study. Study participants received a single dose of 40 mg/kg PZQ. They were actively followed for 1 week to document any treatment-associated adverse event (safety) and for 28 days to assess the CR and ERR (efficacy). Complete data for efficacy and safety were available from 236 and 234 respectively. Two children withdrew from the study based on the informed decision of their parents. Two pre-SACs from efficacy evaluation and four pre-SACs from safety assessments were lost to follow-up. Figure 1 shows the study flow chart. Table 1 presents the sociodemographic characteristics of the study participants.
Egg reduction rate and cure rate
The pre-treatment egg count among the pre-SAC ranged from 12 to 2560 EPG (median = 72 EPG; IQR = 24–228 EPG). The overall ERR (93.3%) was above the WHO reference threshold for efficacy regardless of sex, age category, status of STH co-infection or pre-treatment S. mansoni infection intensity (Table 2).
Of the 236 pre-SAC, 201 children became egg-free at 4 weeks post-treatment. The overall cure rate was 85.2% (95% CI = 80.0%, 89.5%). There was no significant difference in cure rate between females and males, age categories, or STH co-infection status. However, the cure rate was significantly different based on pre-treatment infection intensity, 100% among children with light infection intensity compared to those with moderate (83.3%) or heavy infections (29.4%).
Pre- and post-treatment S. mansoni infection intensity
All participants with light infection intensity showed 100% parasitological cure, while pre-treatment moderate infection intensity progressed to heavy infection intensity after treatment in one participant (1.5%). No persistent heavy infection intensity following PZQ treatment among pre-SAC was observed (Table 3).
Predictors of parasitological cure rate
Predictors of cure rate were analyzed using univariate followed by multivariate logistic regression. Sociodemographic characteristics, including age, sex, STH co-infection, and baseline egg count in hundred, were analyzed in the univariate and multivariable regression model. An increase of 100 in baseline egg count resulted in a 26% (95% CI: 17%, 34%) reduction in the odds of cure. None of the other variables had a significant association with the odds of cure (Table 4).
Incidence and type of treatment‐associated adverse events
Two hundred thirty-four participants completed the 8-day post-treatment safety follow-up period, and 54 reported experiencing 169 treatment-associated AEs. The overall incidence of experiencing at least one type of treatment-associated AEs was 23.1% (95% CI: 18.0–29.0%). Among the participants who experienced AEs, 33 (61.1%) experienced three or more types of AEs, 15 (27.8%) experienced two types of AEs, and the remaining 6 (11.1%) experienced one type of AE. Of the 169 AEs that occurred after treatment, 110 (65.1%) of the AEs occurred within 4 h of receiving treatment, and 59 (34.9%) occurred during day 2 to 8 follow-up period (Table 5).
Stomachache (16.0%), diarrhea (11.2%), nausea (10.7%), drowsiness and fever (10.1%), vomiting (9.5%), headache (7.7%), dizziness (8.9%), and loss of appetite (8.3%) were the most common AEs following PZQ treatment among S. mansoni-infected pre-SAC. The least reported AEs were confusion (3.0%), cough and itching (1.8%), and other symptoms (1.2%) (Fig. 2).
Severity grading of adverse events
Out of the total 169 treatment-associated AEs, 88.8% (n = 150) were mild, 10.7% (n = 18) were moderate, and only 0.6% (n = 1) were severe. Most of the AEs were transient and resolved within 2 days of post-treatment. No life-threatening AE that required hospitalization (Grade 4) was reported (Table 6).
Predictors of treatment-associated adverse events
In multivariable log-binomial regression, residing in Tullo village (ARR = 8.8, 95% CI: 1.28, 60.93) and pre-treatment moderate infection intensity (ARR = 3.2, 95% CI: 1.69, 6.14) and heavy infection intensity (ARR = 6.5, 95% CI: 3.6, 11.52) were significant predictors of PZQ treatment AEs (Table 7). The distribution of pre-treatment heavy S. mansoni infection intensity varied greatly between villages, being higher in Tullo village (18%) followed by Chefe Kotijebesa (10%), and Finchawa village (7%).
Discussion
In this study, we assessed the safety, tolerability, and effectiveness of single-dose PZQ for the treatment of S. mansoni infection among pre-SAC in southern Ethiopia. The type, incidence, and severity grading of treatment-associated AEs that occurred within a week after receiving treatment were assessed. Reported post-treatment AEs were cross-checked and verified with any existing symptoms or clinical conditions before receiving treatment, and efficacy was measured in terms of CRs and ERR following the WHO guideline for assessing the efficacy of anthelminthic drugs against schistosomiasis [30].
Our study had several notable findings. First, the overall PZQ treatment showed satisfactory ERR (93.3%) and CR (85.2%) against S. mansoni infection among pre-SAC; Second, pre-treatment infection intensity was a significant predictor of CR. While all children with light and 83.3% with moderate infection intensity were cured, only one-third of those with heavy infection intensity were cured. A higher baseline egg count was associated with reduced odds of cure. Third, overall, PZQ treatment was tolerated, and about one-fifth of pre-SAC (23.1%) experienced at least one type of treatment-associated mild-to-moderate grade AEs during the first 2 days of receiving treatment. Stomachache, diarrhea, and nausea were the most common AEs. The reported AEs were transient, resolving within a week. Fourth, pre-treatment moderate-to-heavy infection intensity was significantly associated with an increased risk of experiencing treatment-associated AEs. No significant effect of sex, age, or STH co-infection status on the safety and efficacy of PZQ was observed.
Monitoring efficacy after multiple rounds of MDA is recommended since repeated drug exposure may result in parasite tolerability and resistance [35]. Our finding indicates that single-dose PZQ significantly reduced S. mansoni infection among pre-SAC, and the overall ERR of 93.3% was above the 90% threshold for optimal PZQ efficacy set by the WHO [30]. Previous studies of single-dose PZQ (40 mg/kg) given to pre-SAC reported varying CR and ERR [23]. A randomized controlled trial conducted in southern Côte d’Ivoire to compare a single dose of 20 mg/kg, 40 mg/kg, and 60 mg/kg PZQ reported the best cure (72%) with 40 mg/kg among pre-SAC [36]. A higher CR and ERR in pre-SAC from Sudan (geometric mean egg reduction rates ranging from 96.4% to 99.4%) [37] and from Eastern Ethiopia (96.4% CR, 99.4% ERR) were reported [25]. On the other hand, a considerably low CR (50.6%) and a geometric mean ERR of 66.7% at 6 weeks post-treatment from Niger were reported [38]. Nevertheless, the observed CR and ERR in pre-SAC in our study are in line with a recent report conducted among S. mansoni-infected SAC from the same study area (89.1% CR, 93.7% ERR) [20] and a systematic review of other studies from Ethiopia (pooled CR = 89.2% (95% CI: 85.4–93.1), mean ERR = 90.2%) [39].
The difference in the PZQ treatment outcome between populations could be due to variability in infection intensity prevalence in different geo-locations, and the follow-up time in the study setting might contribute to the difference in ERR among pre-SAC infected with S. mansoni. Furthermore, recent studies highlight the importance of genetic variation for PZQ disposition [19, 40], but the impact of genetic variations on PZQ treatment outcomes needs further investigation. Despite the relatively lower CR of pre-SAC with moderate-to-heavy intensity infection groups than the light-intensity infection, the moderate-to-heavy intensity showed satisfactory ERR. This finding indicates that PZQ could reduce morbidities associated with moderate-to-heavy intensity infections among pre-SAC in hyper-endemic communities. This might be related to the paralyzing effect of PZQ on the parasite fecundity, which, in turn, results in low egg count post-treatment, as reported in a previous study [41].
In the present study, even though PZQ showed a high CR against S. mansoni infection, about 14.8% of the study participants were not cured of the infection 4 weeks after treatment. The CR among moderately to heavily infected pre-SAC was significantly lower (29.3%) than those who had light (100%) or moderate (83.3%) infection intensity. An increase of 100 in baseline egg count decreased the odds of cure by 26%. Several studies reported significantly reduced CR among moderate-to-heavy infected children than light infections [18, 20, 32]. This could be attributed to the poor efficacy of PZQ against the immature/juvenile stage of the parasites [11, 18]. Repeated infections leading to suppression of the immune response resulting in the survival of the adult worms to favor the spread of infection might also be responsible for the ineffectiveness of PZQ in curing all study participants. This highlights the need to integrate other intervention measures besides MDA, as WHO recommended, to enhance the achievement of the elimination target [1]. Although the observed ERR and CR in the present study indicate that PZQ is effective against S. mansoni infection to reduce morbidity among pre-SAC in endemic communities, the search for new anti-schistosome drugs or other alternative treatment strategies, such as drug combinations targeting the different developmental stages of the parasites, is imperative to eliminate the diseases [18, 42].
The present study showed that a single dose of PZQ (40 mg/kg) is tolerable among S. mansoni-infected pre-SAC. The overall cumulative incidence of experiencing at least one type of AE among pre-SAC was 23.1% within 8 days of PZQ administration. A recent study among S. mansoni-infected SAC (17.0%) from the same study area in Ethiopia and another study in Rwanda (20.6%) revealed a slightly lower incidence of AE compared to our study in pre-SAC [17, 20]. Our study finding aligns with previous reports of a higher incidence rate of AEs in pre-SAC than SAC [43]. The most common AEs observed after receiving PZQ were gastrointestinal disorders. Our finding aligns with previous reports in pre-SAC from elsewhere [38]. The difference in reported AE incidence may be due to variations in intensity of infections and parasite transmission. Genetic differences in the study population, physiological, nutritional, follow-up period, and other environmental factors may also cause variability in treatment outcomes [21, 43]. The difference in AE incidence in various population segments indicates the need for safety monitoring since results from SAC and adult studies may not apply to pre-SAC.
Fifty-four pre-SAC reported a total number of 169 AEs during the follow-up period. Of the total treatment-associated AEs, 65.1% occurred within 4 h of drug intake, and the rest occurred between days 2 to 8 post-drug administration. The most common AEs reported in this study were stomachache, nausea, diarrhea, drowsiness, fever, and vomiting. This observation is similar to previous studies conducted among children aged 2 to 15 in Angola [43] and SAC in Ethiopia [29]. Cough and rash were the least reported AEs in the present study. Almost all the observed AEs were mild and self-limiting, which agrees with reports from studies among SAC in Rwanda [17], Ethiopia [20], and another previous study [44].
The present study showed residing in Tullo village with a higher moderate-to-heavy S. mansoni infection intensity was a significant predictor of AEs. The highest incidence of AEs (30.6%) was observed at Tullo village, followed by 9.3% at Finchawa village and 3.2% at Chefe Kotijebesa village. Residing in Tullo village increased the risk of experiencing at least one AE by 20% compared to living in Chefe Kotijebesa village. The increased risk of AEs in Tullo village children could be due to the high number of cases with heavy-intensity infection in this village. The village is closer to the infested water body bordering Lake Hawassa than the other study villages. Pre-SAC with heavy baseline infection intensity had a 6.5 times increased risk of experiencing an AE, and those with moderate infection intensity experienced a 3.2 times increased risk compared to those with light infection intensity. A similar finding was reported by a study conducted in the same area among SAC [45]. Thus, safety monitoring of PZQ administration to pre-SAC living in hyper-endemic villages and high pre-treatment infection intensity remains crucial.
Following the WHO guideline to assess anthelminthic drug efficacy [30], we used the Kato–Katz technique to determine CR and ERR and compare them with the threshold set in the guideline to conclude PZQ effectiveness. The Kato–Katz technique can accurately detect schistosome eggs in stool in high-intensity infection settings to diagnose the disease and conduct infection-intensity assessment, and program evaluation. However, in low-intensity infection settings, the Kato–Katz technique is less sensitive and may result in an overestimation of the efficacy. Hence, using this technique in our study can be considered a limitation. Nevertheless, our surveillance study was conducted in a moderate-to-high-intensity infection area [8], and the CR and ERR observed in our study may accurately estimate PZQ efficacy. On the other hand, point-of-care urine circulating cathodic antigen (POC-CCA), the other alternative diagnostic method, is not yet approved by WHO to assess anthelmintic drug efficacy, and it requires further evaluation, including post-treatment CCA clearance time in different age groups and epidemiological settings [46, 47]. Findings from this study provide valuable evidence on the safety and efficacy of single-dose PZQ treatment among S. mansoni-infected pre-SAC for the national NTD program in Ethiopia and the SSA region that follows the WHO guidelines and NTD control strategies.
Conclusions
Single-dose PZQ (40 mg/kg) administered to S. mansoni-infected pre-SAC is effective in curing light-to-moderate infection intensities and reducing morbidity in heavy infections. The treatment is tolerable, and associated AEs are mostly mild-to-moderate and transient resolving within a week. Pre-treatment moderate-to-heavy intensity infection significantly predicts failure to cure and experience treatment-associated adverse events. The lack of cure in 35 (14.8%) and adverse events in one-fifth (23.1%) of S. mansoni-infected pre-SAC highlights the need for consistent and close monitoring of the efficacy and safety of the drug, especially in high-transmission and high infection-intensity endemic area. We advocate the inclusion of pre-SAC in the national deworming program and other disease control intervention measures to accelerate the achievement of eliminating schistosomiasis as a public health problem by 2030. Schistosomiasis control program could be extended to pre-SAC using crushed PZQ tablets before the availability of a pediatric formulation.
Availability of data and materials
All data presented in this study are contained within the manuscript.
Abbreviations
- CR:
-
Cure rate
- ERR:
-
Egg reduction rate
- MDA:
-
Mass drug administration
- PZQ:
-
Praziquantel
- Pre-SAC:
-
Pre-school age children
- STH:
-
Soil-transmitted helminths
- SSA:
-
Sub-Saharan Africa
References
World Health Organization. Guideline on control and elimination of human schistosomiasis. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO. 2022.
van der Werf MJ, de Vlas SJ, Brooker S, Looman CW, Nagelkerke NJ, Habbema JD, Engels D. Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Trop. 2003;86(2–3):125–39. https://doi.org/10.1016/s0001-706x(03)00029-9.
Aula OP, McManus DP, Jones MK, Gordon CA. Schistosomiasis with a focus on Africa. Trop Med Infect Dis. 2021. https://doi.org/10.3390/tropicalmed6030109.
Adenowo AF, Oyinloye BE, Ogunyinka BI, Kappo AP. Impact of human schistosomiasis in sub-Saharan Africa. Braz J Infect Dis. 2015;19(2):196–205. https://doi.org/10.1016/j.bjid.2014.11.004.
Stecher CW, Sacko M, Madsen H, Wilson S, Wejse C, Keita AD, Landoure A, Traore MS, Kallestrup P, Petersen E, Vennervald B. Anemia and growth retardation associated with Schistosoma haematobium infection in Mali: a possible subtle impact of a neglected tropical disease. Trans R Soc Trop Med Hyg. 2017;111(4):144–53. https://doi.org/10.1093/trstmh/trx037.
Federal Democratic Republic of Ethiopia Ministry of Health. The Third National Neglected Tropical Diseases Strategic Plan 2021–2025. Addis Ababa, Ethiopia: 2021. Available online: https://espen.afro.who.int/system/files/content/resources/Third%20NTD%20national%20Strategic%20Plan%202021-2025.pdf. Accessed 15 Nov 2023.
Bisetegn H, Eshetu T, Erkihun Y. Prevalence of Schistosoma mansoni infection among children in Ethiopia: a systematic review and meta-analysis. Trop Dis Travel Med Vaccines. 2021;7(1):30. https://doi.org/10.1186/s40794-021-00156-0.
Tadele T, Astatkie A, Abay SM, Tadesse BT, Makonnen E, Aklillu E. Prevalence and determinants of Schistosoma mansoni infection among pre-school age children in Southern Ethiopia. Pathogens. 2023;12(7):858. https://doi.org/10.3390/pathogens12070858.
Gebreyesus TD, Tadele T, Mekete K, Barry A, Gashaw H, Degefe W, Tadesse BT, Gerba H, Gurumurthy P, Makonnen E, Aklillu E. Prevalence, intensity, and correlates of schistosomiasis and soil-transmitted helminth infections after five rounds of preventive chemotherapy among school children in southern Ethiopia. Pathogens. 2020;9(11):920. https://doi.org/10.3390/pathogens9110920.
Preventive chemotherapy in human helminthiasis. Coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers. Available online: https://www.who.int/publications/i/item/9241547103. Accessed 15 Nov 2023.
Molehin AJ. Schistosomiasis vaccine development: update on human clinical trials. J Biomed Sci. 2020;27(1):28. https://doi.org/10.1186/s12929-020-0621-y.
WHO. World Health Organization World Health Assembly. Schistosomiasis and Soil-Transmitted Helminth Infections. World Health Assembly 54.19 Available online: https://apps.who.int/iris/bitstream/handle/10665/78794/ea54r19.pdf .Accessed 10 Nov 2023.
World Health Organization. Schistosomiasis and soil-transmitted helminthiases: progress report, 2021. Weekly Epidemiological Record, 2022, 48, 97, 621–632. Latest information on epidemiology, distribution and progress made against schistosomiasis. Available online: https://www.who.int/publications/i/item/who-wer9748-621-632. Accessed 10 Nov 2023.
Report of a meeting to review the results of studies on the treatment of Schistosomiasis in preschool-age chidren, WHO report. Geneva: World Health Organization, 2010. Available online: https://www.who.int/publications/i/item/9789241501880. Accessed 10 Nov 2023.
Reinhard-Rupp J, Klohe K. Developing a comprehensive response for treatment of children under 6 years of age with schistosomiasis: research and development of a pediatric formulation of praziquantel. Infect Dis Poverty. 2017;6(1):122. https://doi.org/10.1186/s40249-017-0336-9.
Montresor A, Mwinzi P, Mupfasoni D, Garba A. Reduction in DALYs lost due to soil-transmitted helminthiases and schistosomiasis from 2000 to 2019 is parallel to the increase in coverage of the global control programmes. PLoS Negl Trop Dis. 2022;16(7): e0010575. https://doi.org/10.1371/journal.pntd.0010575.
Kabatende J, Barry A, Mugisha M, Ntirenganya L, Bergman U, Bienvenu E, Aklillu E. Safety of praziquantel and albendazole coadministration for the control and elimination of schistosomiasis and soil-transmitted helminths among children in Rwanda: an active surveillance study. Drug Saf. 2022;45(8):909–22. https://doi.org/10.1007/s40264-022-01201-3.
Mnkugwe RH, Minzi O, Kinung’hi S, Kamuhabwa A, Aklillu E. Efficacy and safety of praziquantel and dihydroartemisinin piperaquine combination for treatment and control of intestinal schistosomiasis: a randomized, non-inferiority clinical trial. PLoS Negl Trop Dis. 2020;14(9): e0008619. https://doi.org/10.1371/journal.pntd.0008619.
Mnkugwe RH, Minzi O, Kinung’hi S, Kamuhabwa A, Aklillu E. Effect of pharmacogenetics variations on praziquantel plasma concentrations and schistosomiasis treatment outcomes among infected school-aged children in Tanzania. Front Pharmacol. 2021;12: 712084. https://doi.org/10.3389/fphar.2021.712084.
Gebreyesus TD, Makonnen E, Tadele T, Mekete K, Gashaw H, Gerba H, Aklillu E. Efficacy and safety of praziquantel preventive chemotherapy in Schistosoma mansoni infected school children in Southern Ethiopia: a prospective cohort study. Front Pharmacol. 2023;14: 968106. https://doi.org/10.3389/fphar.2023.968106.
Sousa-Figueiredo JC, Betson M, Atuhaire A, Arinaitwe M, Navaratnam AM, Kabatereine NB, Bickle Q, Stothard JR. Performance and safety of praziquantel for treatment of intestinal schistosomiasis in infants and preschool children. PLoS Negl Trop Dis. 2012;6(10): e1864. https://doi.org/10.1371/journal.pntd.0001864.
Olliaro PL, Coulibaly JT, Garba A, Halleux C, Keiser J, King CH, Mutapi F, N’Goran EK, Raso G, Scherrer AU, Sousa-Figueiredo JC, Stete K, Utzinger J, Vaillant MT. Efficacy and safety of single-dose 40 mg/kg oral praziquantel in the treatment of schistosomiasis in preschool-age versus school-age children: an individual participant data meta-analysis. PLoS Negl Trop Dis. 2020;14(6): e0008277. https://doi.org/10.1371/journal.pntd.0008277.
Kabuyaya M, Chimbari MJ, Mukaratirwa S. Efficacy of praziquantel treatment regimens in pre-school and school aged children infected with schistosomiasis in sub-Saharan Africa: a systematic review. Infect Dis Poverty. 2018;7(1):73. https://doi.org/10.1186/s40249-018-0448-x.
Kimani BW, Mbugua AK, Kihara JH, Ng’ang’a M, Njomo DW. Safety, efficacy and acceptability of praziquantel in the treatment of Schistosoma haematobium in pre-school children of Kwale County, Kenya. PLoS Negl Trop Dis. 2018;12(10): e0006852. https://doi.org/10.1371/journal.pntd.0006852.
Kemal M, Tadesse G, Esmael A, Abay SM, Kebede T. Schistosoma mansoni infection among preschool age children attending Erer Health Center, Ethiopia and the response rate to praziquantel. BMC Res Notes. 2019;12(1):211. https://doi.org/10.1186/s13104-019-4246-8.
WHO. Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021–2030. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. 2020.
Montresor A, Garba A. Treatment of preschool children for schistosomiasis. Lancet Glob Health. 2017;5(7):e640–1. https://doi.org/10.1016/S2214-109X(17)30202-4.
Federal Democratic Republic of Ethiopia Ministry of Health. Second Edition of National Neglected Tropical Diseases Master Plan, Addis Ababa. Available online: [https://www.afro.who.int/publications/second-edition-national-neglected-tropical-diseases-master-plan-ethiopia-2016. Accessed 10 Nov 2023.
Erko B, Degarege A, Tadesse K, Mathiwos A, Legesse M. Efficacy and side effects of praziquantel in the treatment of Schistosomiasis mansoni in schoolchildren in Shesha Kekele Elementary School, Wondo Genet, Southern Ethiopia. Asian Pac J Trop Biomed. 2012;2(3):235–9. https://doi.org/10.1016/S2221-1691(12)60049-5.
World Health Organization, Geneva (2013). Assessing the efficacy of anthelminthic drugs against schistosomiasis and soil-transmitted helminthiases. Available online: https://apps.who.int/iris/handle/10665/79019. Accessed 15 Nov 2023.
Kernell JW, DePaola RV, Maglione AM, Ahern LN, Penney NG, Addiss DG. Risk of adverse swallowing events and choking during deworming for preschool-aged children. PLoS Negl Trop Dis. 2018;12(6): e0006578. https://doi.org/10.1371/journal.pntd.0006578.
Mnkugwe RH, Minzi OS, Kinung’hi SM, Kamuhabwa AA, Aklillu E. Efficacy and safety of praziquantel for treatment of Schistosoma mansoni infection among school children in Tanzania. Pathogens. 2019. https://doi.org/10.3390/pathogens9010028.
World Health Organization. (1991). Basic laboratory methods in medical parasitology. World Health Organization. Available online: https://apps.who.int/iris/handle/10665/40793. Accessed 10 Nov 2023.
Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. Available online: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_8.5x11.pdf. Accessed 10 Nov 2023.
Crellen T, Walker M, Lamberton PH, Kabatereine NB, Tukahebwa EM, Cotton JA, Webster JP. Reduced efficacy of praziquantel against Schistosoma mansoni is associated with multiple rounds of mass drug administration. Clin Infect Dis. 2016;63(9):1151–9. https://doi.org/10.1093/cid/ciw506.
Coulibaly JT, Panic G, Silue KD, Kovac J, Hattendorf J, Keiser J. Efficacy and safety of praziquantel in preschool-aged and school-aged children infected with Schistosoma mansoni: a randomised controlled, parallel-group, dose-ranging, phase 2 trial. Lancet Glob Health. 2017;5(7):e688–98. https://doi.org/10.1016/S2214-109X(17)30187-0.
Amin MA, Swar M, Kardaman M, Elhussein D, Nouman G, Mahmoud A, Appiah A, Babiker A, Homeida M. Treatment of pre-school children under 6 years of age for schistosomiasis: safety, efficacy and acceptability of praziquantel. Sudan J Med Sci. 2012;7(2):67–76.
Garba A, Lamine MS, Djibo A, Tahirou A, Aouami MA, Alfari A, Phillips AE, Fenwick A, Utzinger J. Safety and efficacy of praziquantel syrup (Epiquantel(R)) against Schistosoma haematobium and Schistosoma mansoni in preschool-aged children in Niger. Acta Trop. 2013;128(2):318–25. https://doi.org/10.1016/j.actatropica.2012.12.003.
Hailegebriel T, Nibret E, Munshea A. Efficacy of praziquantel for the treatment of human schistosomiasis in Ethiopia: a systematic review and meta-analysis. J Trop Med. 2021;2021:2625255. https://doi.org/10.1155/2021/2625255.
Barry A, Kabatende J, Telele NF, Mnkugwe RH, Mugisha M, Ntirenganya L, Bienvenu E, Aklillu E. Effect of pharmacogenetic variations on praziquantel plasma concentration and safety outcomes among school children in Rwanda. Sci Rep. 2023;13(1):1446. https://doi.org/10.1038/s41598-023-28641-w.
Lamberton PHL, Faust CL, Webster JP. Praziquantel decreases fecundity in Schistosoma mansoni adult worms that survive treatment: evidence from a laboratory life-history trade-offs selection study. Infect Dis Poverty. 2017;6(1):110. https://doi.org/10.1186/s40249-017-0324-0.
Cioli D, Pica-Mattoccia L, Basso A, Guidi A. Schistosomiasis control: praziquantel forever? Mol Biochem Parasitol. 2014;195(1):23–9. https://doi.org/10.1016/j.molbiopara.2014.06.002.
Lemos M, Pedro JM, Fancony C, Moura S, Brito M, Nery SV, Sousa CP, Barros H. Schistosomiasis and soil-transmitted helminthiasis preventive chemotherapy: adverse events in children from 2 to 15 years in Bengo province, Angola. PLoS ONE. 2020;15(3): e0229247. https://doi.org/10.1371/journal.pone.0229247.
Zwang J, Olliaro P. Efficacy and safety of praziquantel 40 mg/kg in preschool-aged and school-aged children: a meta-analysis. Parasit Vectors. 2017;10(1):47. https://doi.org/10.1186/s13071-016-1958-7.
Gebreyesus TD, Makonnen E, Tadele T, Gashaw H, Degefe W, Gerba H, Tadesse BT, Gurumurthy P, Aklillu E. Safety surveillance of mass praziquantel and albendazole co-administration in school children from southern Ethiopia: an active cohort event monitoring. J Clin Med. 2022. https://doi.org/10.3390/jcm11216300.
Mazigo HD, Fuss A, Mueller A. High egg reduction rate but poor clearance of circulating cathodic antigen three weeks after Praziquantel treatment among school children on Ijinga Island, north-western Tanzania. Acta Trop. 2021;218: 105871. https://doi.org/10.1016/j.actatropica.2021.105871.
Straily A, Kavere EA, Wanja D, Wiegand RE, Montgomery SP, Mwaki A, Eleveld A, Secor WE, Odiere MR. Evaluation of the point-of-care circulating cathodic antigen assay for monitoring mass drug administration in a Schistosoma mansoni control program in Western Kenya. Am J Trop Med Hyg. 2021;106(1):303–11. https://doi.org/10.4269/ajtmh.21-0599.
Acknowledgements
We thank the Neglected Tropical Diseases Control Program team of the Ministry of Health Ethiopia and the Ethiopian Public Health Institute Neglected Tropical Diseases Control Program team, officials from the Hawella Tulla District Health Office and kebele administrators for their support during the conduct of the study. We extend our gratitude to Bushulo Health Center and Hawassa University Comprehensive Specialized Hospital staff for the favorable working environment and their participation in the planning, awareness creation, and supervision during the data collection. We are grateful to the health extension workers from the three study villages for their facilitation during the data collection. We thank the study participants and their parents/primary caregivers from the three villages for their participation.
Funding
Open access funding provided by Karolinska Institute. This study was conducted as part of the Pharmacovigilance infrastructure and post-marketing surveillance system capacity building for regional medicine regulatory harmonization in East Africa (PROFORMA) project funded by the European & Developing Countries Clinical Trials Partnership (EDCTP) 2 program supported by the European Union (Grant number CSA2016S-1618) and the Swedish International Development Cooperation Agency (SIDA), and PrazOpt project funded by the EDCTP 2 program supported by the European Union (Grant number TMA2018CDF-2345).
Author information
Authors and Affiliations
Contributions
TT, EM, EA, and SMA conceived and designed the study. TT, AA, BTT, EM, EA, and SMA conducted the study and analyzed the data. AA, EM, EA, and SMA supervised the study EA; EM, and SMA acquired funding. TT wrote the first draft, and all authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted as per the Declaration of Helsinki and approved by the Institutional Review Board of the College of Medicine and Health Sciences of Hawassa University (Ref. No: IRB/200/13) and the national research ethics review committee (Ref no MoSHE//RD/401/0974/20). Written informed consent was obtained from parents/primary caregivers of each study participant after clarifying the purpose, method, possible risks/benefits, rights, confidentiality, nature of the study, and the scope of their involvement in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tadele, T., Astatkie, A., Tadesse, B.T. et al. Efficacy and safety of praziquantel treatment against Schistosoma mansoni infection among pre-school age children in southern Ethiopia. Trop Med Health 51, 72 (2023). https://doi.org/10.1186/s41182-023-00562-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-023-00562-4