Abstract
Background
Treatment as prevention evolved into the universal HIV test-and-treat (UTT) strategy, which entails testing to the general population and treatment to every people living with HIV. We investigated universal testing (UT) performance and its determinants in urban Ethiopia and explore magnitude of late diagnosis and its impact on disease stages.
Method
We used data from the Ethiopia Population Based HIV Impact assessment (EPHIA), conducted in 2017/2018 which was a cross-sectional and household-based study. For current analysis, we considered self-report first diagnosis to estimate universal testing irrespective of their serostatus and also consider HIV LAg avidity vs viral load vs plasma antiretroviral drug level algorithm to categorize the late diagnosis. We finally evaluate disease stages using CD4 count and viral load. A 2-level multilevel mixed-effect logistic regression model was employed. The effects of individual-level predictors were quantified by the estimates from the fixed-effect part of the model with p-value < 0.05.
Result
Data were collected from 18,926 adults among those 29.4% of people living in Urban Ethiopia were never tested for HIV. Never tested females was 26.4% (95% CI = 25.3; 27.5). Never tested among divorced and widowed were 19.4% (95% CI: 17.3; 21.8) and 28.3% (95% CI: 24.6; 32.2), respectively. Never tested among elderly and youth were high (28.3% among 45–54 years old) to (41.2% among 55–64 years old) to 47.8% among 15–24 years old. Overall, late HIV diagnosis among adults in urban Ethiopia was 25.9% (95% CI: 21.7, 30.2). Late diagnosis varies by region ranged from 38.1% in the Gambella to 5.8% in Benishangul Gumuz. Advanced immune suppression (CD4 count < 350 cells/µl) among newly diagnosed long-term infection were significantly higher compared to those who were recently infected which accounted 47.8% (95%CI = 33.2–52.1) and 30.9% (95%CI = 21.3–32.2), respectively. Moreover, Viral load suppression were significantly lower among those who were late diagnosed 26.1% (95%CI = 13.6–33.8) compared to those of newly infected 89.6% (95%CI = 76.2; 93.4).
Conclusion
With the aim of UT for high risk and priority population, the low rate of HIV testing among widowed, elderly, young adolescent and women in urban Ethiopia calls for enhanced HIV testing. Moreover, the low HIV testing and high late diagnosis among the high-burden regions calls for region-specific intervention. Advanced disease stages as a result of the high proportion of late diagnosis may impact on fueling community transmission and hinder treatment outcome among PLHIV.
Similar content being viewed by others
Background
Human immunodeficiency virus (HIV) remains one of the leading causes of morbidity and mortality in sub-Saharan Africa. Although global commitment to control the HIV/AIDS pandemic has increased significantly in recent years, the virus continues to spread with alarming and increasing speed [1]. Globally, HIV Testing Service (HTS) and antiretroviral therapy (ART) have been scaled up substantially. In 2005 it was estimated that in Africa only 10% of people with HIV were aware of their HIV status and that, globally, only 12% of people who wanted to test for HIV were able to do so. Nearly 15 years later it is now estimated that 85% of all people with HIV in eastern and southern Africa, and nearly 80% of people with HIV worldwide, know their status. With the offer of immediate ART initiation and improved treatment options, access to and uptake of treatment has increased. Now, most people with HIV who know their status are accessing treatment and care [2].
In Ethiopia, the burden of HIV is high as in elsewhere in sub-Saharan Africa (SSA), accounting for about 720,000 people living with HIV (PLHIV) and 27,104 newly diagnosed cases by 2020. Overall prevalence of HIV in Ethiopia was therefore, 0.96% while the prevalence in urban was 3% by 2020 [3].
Targeted HIV testing among the key and priority population and early HIV diagnosis is one of the effective ways to prevent the spread of the epidemic [4]. This helps to lower the viral load (VL) and improve CD4 count, resulting in a dramatic reduction of the risk of morbidity and mortality among PLHIV, and in decreasing HIV transmission by greater than 90% [5, 6]. The World Health Organization (WHO) recommend “universal test and treat” (UTT) approach to end AIDS by 2030. UTT is approach which recommends all population at risk to be screened for HIV infection and those diagnosed HIV positive receive immediate treatment regardless of CD4 count [7]. In Ethiopia at risk and priority populations to be covered under UTT strategy were women, people living in hotspot areas (Gambella and Addis Ababa), female sex workers, widowed and separated, elderly and families of PLHIV [8]. Understanding status of universal testing among at risk population and assessing determinants of late diagnosis and its impact on disease stage is of a priority for the program to focus areas of intervention.
Late diagnosis is associated with: increased HIV-related morbidity and mortality, shorter survival, poor response to treatment, increased healthcare costs and increased rates of HIV transmission. If a person is diagnosed and treated for HIV early in the course of infection before severe impairment of the immune system has occurred, life-expectancy may approach that of the general population [9,10,11,12,13].
In Ethiopia, evidences on the universal testing in urban Ethiopia among the different subpopulation and magnitude and determinants of late diagnosis and its impact on the different disease stage are limited. Hence, we evaluated status of universal testing and late diagnosis among at risk and priority population in urban Ethiopia and assess the impact of late diagnosis on disease stages.
Methods
Study design and setting
This analysis involved the Ethiopian Population Based HIV Impact Assessment (EPHIA) data, which was collected through urban-representative, cross-sectional and household-based survey conducted in urban Ethiopia from October 2017 to April 2018.
The domain of analysis for the universal testing was all adult people (age > 15 years old) in urban Ethiopia (which was further disaggregated to evaluate testing among the different key and priority population in Ethiopia) while for the late diagnosis, we considered only adult PLHIV. For the categories of the different disease stages we considered CD4 count < 350 cells/µl or Viral load ≥ 1000 copies/ml as defined by the world Health organization [14, 15].
Hence, for the universal testing we included all adults stayed overnight in the household (de facto). Moreover, for the late diagnosis and classification of disease stages, we considered only adult people living with HIV (tested positive). HIV-negative population was excluded from analysis of late diagnosis and disease stages.
Study population and sampling procedures
EPHIA used a two-stage cluster sampling design with stratification into small and large urban areas. In the first stage 393 enumeration area (EAs)/clusters were selected using a probability proportional to size method based on EAs created by CSA for the 2007 Ethiopia Population and Housing Census, which included 17,339 EAs containing around three million households. The 393 EAs were further stratified by nine regional states and two city administrations: Tigray, Afar, Amhara, Oromia, Somali, Benishangul Gumuz, SNNPR, Gambella, Harari, Addis Ababa, and Dire Dawa. In second stage sampling, 30 households were randomly selected from each EA using an equal probability method, resulting in a total number of 11,810 households where 19,136 adults reside in.
Data collection
Survey Staff Fieldwork started at the beginning of October 2017 and was completed in April 2018. Fieldwork was conducted by 31 locally hired field teams composed of a team leader, six nurse interviewers and two drivers, who were locally hired. Field teams included both male and female staff members who spoke the languages used in the areas to which they were deployed. A total of about 328 field staff (six field coordinators, 31 team leaders, 211 nurse interviewers [93 testers and 118 interviewers], six community-mobilization coordinators, and 74 drivers) participated in data collection. The field teams were supervised by 31 team leaders, six field coordinators and managed by central staff, who guided and oversaw data collection activities, performed quality checks, and provided technical support. In addition, the laboratory staff was organized at different levels (central laboratory staff, regional field supervisors, onsite laboratory supervisors, satellite lab technicians, and satellite lab logisticians). Laboratory staff were trained in specimen management, including sample processing, labeling, and quality assurance (QA). Central laboratory staff were trained in VL measurement, early infant diagnosis, HIV confirmatory testing, and testing for recent HIV infection using the limiting antigen (LAg) avidity enzyme immunoassay (EIA). National and international monitors periodically conducted direct observation of data collection activities in the field and in the laboratories to provide technical support and ensure quality.
Laboratory-based biomarker testing to identify late diagnosis
HIV-1 VL (HIV RNA copies per mL) of confirmed HIV-positive participants was measured from plasma using the Roche (COBAS® AmpliPrep/COBAS® TaqMan® HIV-1 Test, Roche Diagnostics, Indianapolis, Indiana, United States) and from DBS using Abbott m2000 System (Abbott Molecular Inc., Chicago, Illinois, United States). Both instruments consist of two separate instruments, the sample preparation (Ampli prepap and m2000sp, which carries out automated extraction, purification, and preparation of HIV-1 RNA), and the Cobas Taqman-96 and m2000rt (which amplifies, detects, and measures the HIV-1 RNA load). In Cobas Taqman-96, 1 mL of plasma protocol was used, while the open-mode protocol for the Abbott Real Time HIV-1 assay was used to measure VL from DBS samples from adults with insufficient volume of plasma.
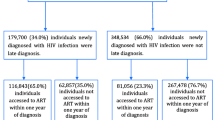
To distinguish recent from long-term HIV infections, in order to estimate incidence, the study used two different laboratory-based testing algorithms. Each algorithm employed a combination of assays: 1) HIV-1 LAg-Avidity EIA (Sedia Biosciences Corporation, Portland, Oregon, United States) and VL and 2) HIV-1 LAg Avidity EIA, VL, and ARV detection (Fig. 1).
Specimens with median normalized optical density (OD), ≤ 1.5 using LAg avidity testing was classified as potential recent infections, and their VL results were assessed. Specimens with VL < 1000 copies/mL were classified as long-term infections, while those with VL ≥ 1,000 copies/mL were classified as recent infections. In the ARV-adjusted algorithm, specimens with VL ≥ 1000 copies/ml and with detectable ARVs were classified as long-term infections. Specimens with VL ≥ 1000 copies/mL and without detectable ARVs were classified as recent infections.
Qualitative screening, for detectable concentrations of ARVs, was conducted on DBS specimens from all HIV-positive adults by means of high-resolution liquid chromatography coupled with tandem mass spectrometry. The method used for ARV detection was a modified version of the methodology described by Koal et al. This qualitative assay was highly specific, as it separates the parent compound from the fragments, and highly sensitive, with a limit of detection of 0.02 μg/mL for each drug and a signal-to-noise ratio of at least 5:1 for all drugs. As detection of all ARVs in use at the time of the study was cost-prohibitive, three ARVs, efavirenz, lopinavir, and nevirapine, selected as markers for the most commonly prescribed first and second line regimens. Samples from participants who had suppressed viral loads and/or reported being on ART, but had no evidence of the first three compounds, were tested for nevirapine. These ARVs were also selected based on their relatively long half-lives, allowing for a longer period of detection following intake. ARV detection was performed by the Division of Clinical Pharmacology of the Department of Medicine at the University of Cape Town in South Africa.
Statistical analysis
For this analysis, demographic, behavioral and environmental factors were considered as independent variable. HIV testing, late diagnosis and disease stages were also considered as dependent variables.
A descriptive analysis was done to assess demographic and individual characteristics of the study population. Bivariate analysis with cross-tabulation and 95% confidence interval (CI) were employed to examine the association between the outcome variable (HIV testing and late diagnosis) and the selected predictor variables.
A multilevel logistic regression model was fitted to assess for regional variation in the two dependent variables and identify their association with the independent variables considered in the study. A 2-level multilevel mixed-effect logistic regression model was employed. All the independent variables categorized as individual-level variables were considered level-1 variables and the region as level-2 variables. In the multilevel regression model, the effect of level-2 variable (regional) was quantified by intra-class correlation (ICC), the proportion of total variation in the response variable accounted for by the between-regional variation. The effects of individual-level predictors were quantified by the estimates from the fixed-effect part of the model with a p-value less than 0.05 or 95% CI.
The significance in improvement of multilevel model over the usual standard logistic model was checked by the Chi-square test. A significance Chi-square test result indicated that the multilevel model better fitted over the standard logistic model. Data analysis was done using Stata Statistical Software v16.0 (TX: Stata Corp LLC).
Results
Demographic characteristics of the study participants
Overall, data were collected from 18,926 adults. The higher proportion of population 4708 (33.5%) were from Oromoia region while 3280 (18.8%) and 2795 (16.1%) were from Amhara and SNNPR regions. With regard to the marital status, 8896 (46.5%), 7529 (35.9%) and 1829 (8.6%) were married, never married and divorced, respectively. While study participants disaggregated educational status, 7098 (35%), 5783 (28.8%) and 4682 (24.3%) attended primary, secondary and more than secondary education, respectively. Majority 18,176 (90.1%) were in the age from 15 to 49 years old while 1994 (9.9%) were in the age range from 50 to 64 years old (Table 1).
HIV testing by different characteristics in urban Ethiopia
A total of 18,926 adults aged 15 to 64 years were included in the analysis to assess self-reported awareness of HIV testing in urban Ethiopia. Overall, 29.4% of them reported that they never got tested for HIV. The proportion never tested for HIV ranged from 18.8% in the Harari region to 20.3% in Afar to 32.6% in Oromia to 69.1% in the Somali region. Proportion never tested in small urban areas was 32.1%, and 26.8% among adults in large urban areas (Table 1).
As shown in Table 2, the proportion of never tested among adult males was significantly higher, 32.4% (95%: 31.0, 33.9) than females, 6.4% (95%: 25.3, 27.5). Nearly half of those who were never married, 49.5% (95% CI: 47.7, 51.3) were never tested. The proportion never tested was more than double among the married 17.3% (95% CI: 16.1, 18.6) and the divorced or separated 19.4% (95% CI: 17.3, 21.8), and was almost twice among widowed, 28.3% (95% CI: 24.6, 32.2).
In terms of wealth quintile, 39.3% of the adults who were in the lowest quintile had never tested for HIV, significantly more than those who were in the second, third, fourth, and highest quintiles (30.0%, 26.3%, 26.6%, and 27.2%) respectively, with non-overlapping 95% CIs. Similarly, the proportion of never tested for HIV among adults who were not employed (during the last 12 months) preceding the study was 37.0%, significantly more than almost twice among employed (during last 12 months) (21.0%) with the non-overlapping 95% CIs. Among the behavioral characteristics, the proportion of never tested for HIV was significantly higher in adults who did not report drinking alcohol, 33.2% (95% CI: 31.9, 34.5) compared with adult who used alcohol, 24.2% (95% CI: 22.7, 25.7).
Late HIV diagnosis
Among adults aged 15 to 64 years tested for HIV, 614 (3.0%) adults tested positive. A total of 611 PLHIV were included in the analysis to assess late HIV diagnosis. Overall, late HIV diagnosis among adults in urban Ethiopia was 25.9% (95% CI: 21.7, 30.2). Despite the diagnosis, 3.4% of PLHIV were also not linked to HAART. The proportion of adults who tested for HIV late ranged from 38.1% in Gambela to 34.7% in Addis Ababa to 5.8% in Benishangul Gumuz to none in the Somali region (Table 3).
As shown in Table 4, the proportion of late diagnosis of HIV among adult males was significantly higher, 36.8% (95%: 28.0, 46.6), than females, 20.8% (95%: 17.3, 24.9). The proportion of never married, married or living together PLHIV was slightly higher among those with late diagnosis, 30.3% and 29.2%, respectively, compared to the divorced, separated and widowed, 21.5% and 20.6%, respectively.
Over one-third (35.4%) of the adult PLHIV attended secondary education and above were diagnosed late, followed by those with primary education (28.4%), secondary education (25.5%), and those who never attended school (16.4%). The highest proportion of late HIV diagnosis was observed among the adult PLHIV was in younger age group, 15–24 years (43.5%), followed by those 25–34 years (26.6%), and those 45–54 years (25.2%). Late HIV diagnosis was the lowest among the 55–64 year age group (19.5%) (Table 4).
PLHIV among adults with the lowest, fourth, and the highest quintiles had a higher proportion of late HIV diagnosis, 31.7%, 30, 5%, and 29.0%, respectively, while lower proportion was seen in second (17.8%) followed by the middle quintile (21.4%). The proportion of late diagnosis among PLHIV who used alcohol was 36.1%, almost twice compared with adults not reported using alcohol (19.7%).
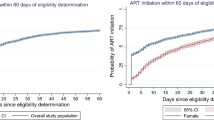
Magnitude of never tested, burden of HIV and newly diagnosed long-term infections among people in urban Ethiopia, disaggregated by region
As shown in Fig. 2 below, prevalence of HIV among the regional administrations in Ethiopia was heterogonous, ranging from 5.7% in Gambella to 0.8% in Somali. Never tested among people in urban Ethiopia also ranged from 69.1% in Somali to 20.3% in Afar regions. Newly diagnosed long-term infection was the highest in Gambella 38.1 to 0.0% in Somali region.
Determinants for never tested for HIV
The results multilevel mixed-effect logistic regression model on diagnosis show that the model fitted well for the data over the standard logistic regression to assess determinants for never tested for HIV (X2 = 547.62, p < 0.01). The result of ICC of the two-level multilevel model revealed that about 9.6% of the variation in the likelihood of never tested for HIV was explained by the variation among the regions in urban Ethiopia (95% CI: 0.043, 0.199) (Table 4).
Adults aged 15–24 years (AOR: 2.49; 95% CI: 2.24, 2.77), 35–44 years (AOR: 1.54; 95% CI: 1.35, 1.75), 45–54 years (AOR: 3.14; 95% CI: 2.72, 3.64), and those 55–64 years (AOR: 5.26; 95% CI: 4.48, 6.17) were more likely to have never tested for HIV, respectively, as compared to those 25–34 years of age. The odds of being never tested for HIV among adults living in small urban areas were 1.24 times higher than those living in large urban areas (AOR: 1.24; 95% CI: 1.14, 1. 36). Being male was significantly and positively associated with never tested status compared with the female counterparts (AOR: 1.39; 95% CI: 1.29, 1.50) (Table 4).
Adults who were married or living together, divorced or separated, and widowed had 82.0% (AOR: 0.18; 95% CI: 0.16, 0.20), 81.0% (AOR: 0.19; 95% CI: 0.17, 0.23), and 80.0% (AOR: 0.20; 95% CI: 0.16, 0.25), respectively, lower odds of being never tested for HIV compared to their never married counterparts. In terms of education level of respondents who never attended school (AOR: 3.77; 95% CI: 3.27, 4.34), primary (AOR: 2.34; 95% CI: 2.10, 1.79), and secondary education (AOR: 1.62; 95% CI: 1.45, 1.79) were more likely to never tested for HIV, respectively as compared to those who had above secondary education (Table 4).
Adults who were in second, middle, fourth, and highest wealth quintiles had 27.0% (AOR: 0.73; 95% CI: 0.65, 0.82), 33.3% (AOR: 0.67; 95% CI: 0.59, 0.75), 32.0% (AOR: 0.68; 95% CI: 0.60, 0.77), and 18.0% (AOR: 0.82; 95% CI: 0.72, 0.93), respectively, lower odds of being never tested compared to their counterparts in the lowest quintiles. The odds of being never tested for HIV among adults aged 15 to 64 who had not drink alcohol (AOR 1.37; 95% CI; 1.26, 1.48) was 1.37 times higher compared to those who used alcohol.
Determinants for late HIV diagnosis
The results on the diagnosis of multilevel mixed-effect logistic regression model showed that the model fitted well for the data over the standard logistic regression to assess determinants for late diagnosis for HIV (X2 = 6.6, p < 0.01). The result of ICC of the two-level multilevel model revealed that about 6% of the variation in the likelihood of never tested for HIV was explained by the variation among the regions in urban Ethiopia (95% CI: 0.012, 0.257) (Table 5).
Among PLHIV aged 15 to 64 years, being male was 1.69 times more likely to present late for HIV diagnosis as compared to those female counterparts within the regions (AOR: 1.69; 95% CI: 1.09, 2.63). PLHIV in the age group of 25–34 years, 35–44 years, 45–54 years, and those 55–64 years had 59% (AOR: 0.41; 95% CI: 0.22, 0.79), 68.0% (AOR: 0.32; 95% CI: 0.17, 0.60), 66.0% (AOR: 0.34; 95% CI: 0.17, 0.70), and 76.0% (AOR: 0.24; 95% CI: 0.09, 0.66), respectively, lower odds of being lately diagnosed for HIV compared to those 15–24 years of age with in the regions (Table 5).
The odds of late diagnosis for HIV among PLHIV aged 15 to 64 who ever had used alcohol (AOR 2.07; 95% CI; 1.38, 3.09) was 2.07 times higher compared to those who had drink with in the regions.
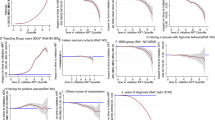
Disease stages among newly diagnosed
Proportion of advanced immune suppression (CD4 count < 350 cells/µl) among newly diagnosed long-term PLHIV were significantly higher compared to those who were newly infected which accounted 47.8% and 30.9% (P = 0.001), respectively. Moreover, the median CD4 count among those who were newly diagnosed long-term PLHIV were lower 352 cells/mm3 compared to those who newly diagnosed new infections 457 cells/ mm3. Viral load suppression were significantly lower among those who were newly diagnosed long-term PLHIV (26.1%) compared to those newly diagnosed new infections (89.6%) (P = 0.001) (Fig. 3).
Discussion
As the gateway to a continuum of HIV/AIDS services, timely HIV testing plays a central role in the fight against the HIV epidemic [16]. A recent study demonstrated the efficacy of early testing in immediately keeping patients on ART for the prevention of HIV transmission; and studies based on mathematical models suggest that UTT, consisting of treating every HIV-infected person as soon as diagnosis is made, can curb the epidemic. For all these reasons there is international consensus to expand HIV testing in resource limited countries like Ethiopia, as part of which generating evidence in this field will be crucial.
In this analysis, 29.4% of adults in urban Ethiopia were never tested for HIV. It was relatively higher compared to a study conducted in Malawi that revealed 25% of population reported having never been tested for HIV [17]. However, other similar studies reported higher HIV testing in Cóˆte d’Ivoire (50%) [16] and Mozambique (51%) [18]. This might be explained by program implementations among the different countries in a consistent time point.
Furthermore, our finding revealed that HIV testing differed across the administrative regions in Ethiopia. The proportion of adults who reported being never tested for HIV ranged from 18.8% in the Harari region to 20.3% in Afar to 32.6% in Oromia and to 69.1% in Somalia, which might be explained by the heterogeneity of HIV and program implementation among the different regional administrations in Ethiopia. This could also be explained by variations in the burden of HIV among the different regional administrations in the country which ranged from 0.1 to 5.6% [19]. This may highlight the importance of expanding testing among the high-burden regions including Gambella and Addis Ababa which are categorized under the hot spot areas and be included in Universal Testing in the country. The result of ICC of the two-level multilevel model revealed that about 6% of the variation in the likelihood of never tested for HIV was explained by the variation among the regions in urban Ethiopia. This calls for region-specific program interventions to enhanced HIV testing among high-burden priority regions.
Our study showed that the proportion of never tested among adult males was significantly higher than females. This is consistent with evidence from Zimbabwe, which showed a significant difference between male and female testing [20]. In contrast, a study conducted in Uganda reported a lower proportion of males (16%) than females was never tested [21]. Other studies have shown that women are more likely to report having ever been tested than men [16, 22, 23]. In our study, among adults aged 15 to 64 years being male was significantly associated with never tested for HIV compared with the female counterparts in the regions. This might be explained by the high rate of testing uptake for female as a result of PMTCT during antenatal follow-up [24]. Despite the high proportion of testing among women in urban Ethiopia, more than a quarter of women in reproductive age living in urban Ethiopia never tested. Women are among the priority population in Ethiopia and are parts of UT. Hence, this highlights the low testing of women in reproductive age in urban Ethiopia.
In the current study, the proportion of adults never tested was highest at age 15–24 years (47.8%) followed by 55–64 years (41.2%). Adults aged between 15–24, 35–44, 45–54 and 55–64 years were 2.49, 1.54, 3.14, and 5.26 times more likely to have never tested for HIV compared to 25–34 years, respectively. HIV incidence in the age 15–24 years is the highest among all age group (0.12) and HIV prevalence among the elderly accounts for 4.4%, compared to the prevalence in the general population of 0.96%. This might be explained by age-related behavioral factors for HIV testing [25, 26]. In this study, the low rate of testing among widowed could be worrisome for the program since the prevalence of HIV among the widowed is significantly higher 14.0% compared to 0.96% in the general and 3.0% in urban Ethiopia [27]. Widowed were also a priority population in the country.
Overall, 25.9% (95% CI: 21.7, 30.2) of the adults were diagnosed late for HIV in urban Ethiopia. This was high compared to the finding of a study conducted in United Kingdom (UK), which showed that 15.4% were diagnosed late [28], while our study is consistent with a report from Spain, which showed 30.4% were late presenters [12]. This might be explained by the different behavioral and environmental factors contributing to the different time to diagnosis [29].
Proportion of adults who tested late for HIV ranged from 38.1% in the Gambella region to 34.7% in Addis Ababa to 5.8% in Benishangul Gumuz and to 0.0% in Somalia, given the heterogeneity of HIV epidemic prevalence by region in Ethiopia, which ranged from 5.6% in Gambella followed by 3.3% in Addis Ababa and is less than 1% in Somali [30] and that the highest proportion of people with late diagnosis is in the high-burden regions, the program may consider focusing on devising strategies to increase testing in the high-burden regions.
In our study, the proportion of late diagnosis for HIV among adult males was significantly higher (36.8%; 95%: 28.0, 46.6) than females (20.8%; 95%: 17.3, 24.9). This result was not in line with a study in Mozambique which reported late diagnosis among males Vs females of 43.7% and 55.3% [31], respectively. However, our finding concurs with the findings of a study from South Africa which revealed that 57% of males and 43% of females were diagnosed late [32], showing that the proportion late diagnosis is higher among males.
The highest proportion of late diagnosis for HIV among adults living with HIV was in younger age 15–24 years (43.5%), followed by 25–34 years (26.6%) and in 45–54 years (25.2%), the lowest was in 55–64 years (19.5%). This may indicate the need for a more rigorous programmatic intervention among the adolescent and early diagnosis. Among PLHIV aged 15 to 64 years, males were 1.69 times more likely to present late for HIV diagnosis as compared to their female counterparts in the regions. Likewise, PLHIV in the age group of 25–34 years, 35–44 years, 45–54 years and those 55–64 years had 59.0%, 68.0%, 66.0% and 76.0%, respectively, and had lower odds of being diagnosed late for HIV compared to those 15–24 years of age. The different studies highlighted variations among the different age group, a study conducted in Durban revealed the high rate of late diagnosis at early adult stage and elderly which was consistent with this study [32]. Other study conducted in Uganda revealed late diagnosis among elderly [21]. This difference might be explained by the variations in behavioral factors among people in this age group [18].
In this study, the proportion of advanced immune suppression (CD4 count < 350 cells/µl) among newly diagnosed long-term infection PLHIV were significantly higher compared to those who were new infections which accounted 47.8% (95%CI = 33.2–52.1) and 30.9% (95%CI = 21.3–42.2), respectively. This was consistent with other studies which has been previously conducted [22, 33, 34]. This could impact on poor treatment outcome and could lead to opportunistic infections [10, 35]. A study conducted in south Africa also indicated there is 3.46 times risk of mortality among patients who were initiated for HAART with baseline CD4 count < 350 cells/mm3 [36].
Viral load suppression were significantly lower among those who were late diagnosed 26.1% (95%CI = 13.6–33.8) compared to those who were recently infected 89.6% (95%CI = 76.2, 93.4) which was also similar to other studies conducted in South Africa and Zimbabwe [35,36,37]. This may highlight the importance of early diagnosis for better therapeutic outcome of PLHIV during clinical management and also for the program prevention and control strategy [32, 38, 39]. The significantly low level of viral load suppression among newly diagnosed long-term infections could fuel the risk of community transmission (42).
Strength and limitation of the study
One of the strengths of this study is, it provides evidence for a global priority public health issue in the context of Ethiopia using a large number of study participants (n = 18,926) across the different regions of urban Ethiopia using a cross-sectional household-based data collection. It also differentiates recent HIV infections from long-term HIV infections using different laboratory biomarkers and test algorithms.
However, this study did not consider all priority and at risk groups of HIV and further study may be required to specific group of population including female sex workers and drug users. Moreover, there has to be a continuous interpretation of this finding for the current use since data were collected by 2017–2018. Moreover, it has to be noted, the study is limited to urban setting in Ethiopia.
Conclusion
With the aim of universal testing for high risk and priority population, the low HIV testing among widowed, elderly, young adolescent and women in urban Ethiopia calls for enhanced testing strategy among the high risk and priority population. Moreover, the low testing and high late diagnosis in Gambella and Addis Ababa regions which are high-burden priority regions may call for region-specific intervention. The high proportion of new diagnosis with long-term infection which led to advanced disease stages may impact on fueling community transmission and hinder treatment outcome among PLHIV.
Availability of data and materials
Data of this analysis are publicly available at https://phia.icap.columbia.edu/countries/ethiopia/.
Abbreviations
- AOR:
-
Adjusted odds ratio
- ARV:
-
Antiretroviral
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- CSA:
-
Central Statistics Agency
- DBS:
-
Dried blood spot
- EPHI:
-
Ethiopian Public Health Institute
- HIV:
-
Human immunodeficiency virus
- HTS:
-
HIV testing service
- ICC:
-
Intra-cluster correlation
- OD:
-
Optical density
- PLHIV:
-
People living with HIV
- PMTCT:
-
Prevention of mother to child HIV transmission
- SERO:
-
Scientific and Ethical Review Office
- UT:
-
Universal testing
- UTT:
-
Universal test and treat
- VL:
-
Viral load
- VLS:
-
Viral load suppression
References
Bertozzi S, Padian NS, Wegbreit J, Lisa M, Feldman B, Gayle H, et al. HIV / AIDS prevention and treatment. Dis Control Prior Dev Ctries. 2005;2:331–69.
WHO. Consolidated guidelines on HIV testing services. N C Med J. 2019;53(1):55. https://www.who.int/publications/i/item/978-92-4-155058-1
Ministry of Health, The Ethiopian Public Health Institute; HIV related estimates and projections in Ethiopia, 2020-2021. https://ephi.gov.et/wpcontent/uploads/2014/09/HIV_estimation_and_projection_for_Ethiopiawith-uncertainity_2019-PR.pdf. Accessed March 2021.
USAID (Health Policy Initiative), Equity and Access To Art in Ethiopia, June, 2010. https://pdf.usaid.gov/pdf_docs/Pnadx843.pdf.
UNAIDS (Joint United Nations Programme on HIV/AIDS). 90-90-90 An ambitious treatment target to help end the AIDS epidemic. 2014. https://www.Unaids.Org/Sites/Default/Files/Media_Asset/90-90-90_En_0.Pdf.
Organization WH, others. Global update on HIV treatment 2013: results, impact and opportunities. 2013;(June). http://apps.who.int/iris/handle/10665/85326.
Etoori D, Kerschberger B, Staderini N, Ndlangamandla M, Nhlabatsi B, Jobanputra K, et al. Challenges and successes in the implementation of option B+ to prevent mother-to-child transmission of HIV in southern Swaziland. BMC Public Health. 2018;18(1):1–9.
FHAPCO. HIV/AIDS National Strategic Plan for Ethiopia, 2021–2025. 2546.
Ribeiro LCS, Freitas MIdF, Tupinambás U, Lana FCF. Late diagnosis of human immunodeficiency virus infection and associated factors. Rev Lat Am Enfermagem. 2020;28:1–12.
Waters L, Sabin CA. Late HIV presentation: epidemiology, clinical implications and management. Expert Rev Anti Infect Ther. 2011;9(10):877–89.
Camoni L, Raimondo M, Regine V, Salfa MC, Suligoi B. Late presenters among persons with a new HIV diagnosis in Italy, 2010–2011. BMC Public Health. 2013;13(1):1–6.
Díez R-N. Late diagnosis of HIV infection. An Sist Sanit Navar. 2014;37(3):313–5.
van der Kop ML, Thabane L, Awiti PO, Muhula S, Kyomuhangi LB, Lester RT, et al. Advanced HIV disease at presentation to care in Nairobi, Kenya: late diagnosis or delayed linkage to care?-a cross-sectional study. BMC Infect Dis. 2016;16(1):1–9. https://doi.org/10.1186/s12879-016-1500-8.
WHO. On the use of antiretroviral drugs for treating and preventing HIV infection. in 2014.
WHO. Guidelines for surveillance of drug resistance in tuberculosis. 2018; 5th edition (ISBN 978 92 4 154913 4):2011.
Jean K, Anglaret X, Moh R, Lert F, Dray-Spira R. Barriers to HIV testing in Côte d’ivoire: the role of individual characteristics and testing modalities. PLoS ONE. 2012;7(7):12–8.
Kigozi IM, Dobkin LM, Martin JN, et al. Late-stage disease at presentation to an HIV clinic in eastern Tanzania: a retrospective cross-sectional study. NIH Public Access. 2010;52(2):1–21. https://doi.org/10.4314/mmj.v27i4.2.
Maheu-Giroux M, Marsh K, Doyle CM, Godin A, Lanièce Delaunay C, Johnson LF, et al. National HIV testing and diagnosis coverage in sub-Saharan Africa: a new modeling tool for estimating the “first 90” from program and survey data. AIDS. 2019;2019(33):S255–69.
The DHS Program. Ethiopia Demographic and Health Survey. 2016. 187–189 p. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf.
Gazimbi MM, Magadi MA. A multilevel analysis of the determinants of HIV Testing in Zimbabwe: evidence from the demographic and health surveys. HIV/AIDS Res Treat Open J. 2017;4(1):14–31.
Nangendo J, Katahoire AR, Armstrong-Hough M, Kabami J, Obeng-Amoako GO, Muwema M, et al. Prevalence, associated factors and perspectives of HIV testing among men in Uganda. PLoS ONE. 2020;15(8 August):1–20. https://doi.org/10.1371/journal.pone.0237402.
Hall HI, Halverson J, Wilson DP, Suligoi B, et al. Late diagnosis and entry to care after diagnosis of HIV infection: a country comparison. PLoS One. 2013. https://doi.org/10.1371/journal.pone.0077763.
Sabin CA, Smith CJ, Gumley H, Murphy G, Lampe FC, Phillips AN, et al. Late presenters in the era of highly active antiretroviral therapy: uptake of and responses to antiretroviral therapy. AIDS. 2004;18(16):2145–51.
Torpey K, Kabaso M, Kasonde P, Dirks R, Bweupe M, Thompson C. Increasing the uptake of prevention of mother-to-child transmission of HIV services in a resource-limited setting. BMC Health Serv Res. 2010;10:29. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed9&NEWS=N&AN=20109210.
Chen X, Qin C, Chen R, Huang Y, Xu Y, Tang Q, et al. Epidemiological profile and molecular genetic characterization of HIV-1 among female sex workers and elderly male clients in Guangxi, China. Emerg Microbes Infect. 2021;10(1):384–95.
Mahy M, Autenrieth CS, Stanecki K, Wynd S. Increasing trends in HIV prevalence among people aged 50 years and older: evidence from estimates and survey data. AIDS. 2014;28(September):S453–9.
Ethiopian Public Health Institute, Ethiopia Population-based HIV Impact Assessment EPHIA 2017-2018. https://www.ephi.gov.et/images/EPHIA_Final%20Report.pdf. Accessed May 2022.
Maheu-Giroux M, Tanser F, Boily MC, Pillay D, Joseph SA, Bärnighausen T. Determinants of time from HIV infection to linkage-to-care in rural KwaZulu-Natal, South Africa. AIDS. 2017;31(7):1017–24.
Delpierre C, Dray-Spira R, Cuzin L, Marchou B, Massip P, Lang T, et al. Correlates of late HIV diagnosis: implications for testing policy. Int J STD AIDS. 2007;18(5):312–7.
Central Statistics Agency. Ethiopia Demographic and Health Survey 2016. 2016. http://www.unicef.org/ethiopia/ET_2011_EDHS.pdf. Accessed 26 Feb 2016.
Lahuerta M, Lima J, Nuwagaba-Biribonwoha H, Okamura M, Alvim MF, Fernandes R, et al. Factors associated with late antiretroviral therapy initiation among adults in Mozambique. PLoS ONE. 2012;7(5):1–10.
Drain PK, Losina E, Parker G, Giddy J, Ross D, Katz JN, et al. Risk factors for late-stage HIV disease presentation at initial HIV diagnosis in Durban, South Africa. PLoS One. 2013. https://doi.org/10.1371/journal.pone.0055305.
Shao L, Zhang X, Gao Y, Xu Y, Zhang S, Yu S. Hierarchy low CD4+/CD8+ T-cell counts and IFN- γ responses in HIV-1+ individuals correlate with active TB and/or M. TB co-infection PLoS One. 2016. https://doi.org/10.1371/journal.pone.0150941.
Kebede MM, Zegeye DT, Berihun M. Predictors of CD4 count changes after initiation of antiretroviral treatment in University of Gondar Hospital. Gondar Ethiop. 2014;1:1–7.
Ginwalla R, Chama E, Thomas R, Mwiya M, Kankasa C. Prevalence of clinical, immunological and virological failure among children on Haart at the University Teaching Hospital, Lusaka, Zambia. Med J Zambia. 2012;39(3):1–5.
Sebunya R, Musiime V, Kitaka SB, Ndeezi G. Incidence and risk factors for first line anti retroviral treatment failure among Ugandan children attending an urban HIV clinic. AIDS Res Ther. 2013;10(1):1.
Humphreys E, Lb H, Rutherford G, et al. Antiretroviral regimens for patients with HIV who fail first-line antiretroviral therapy (review). Cochrane Library. 2009. https://doi.org/10.1002/14651858.CD006517.pub2.
Gesesew HA, Ward P, Woldemichael K, Mwanri L. Late presentation for HIV care in Southwest Ethiopia in 2003–2015: prevalence, trend, outcomes and risk factors. BMC Infect Dis. 2018;18(1):1–11.
Horsley Downie J, Pegler M, Widdrington J, Price DA, Premchand N, Chadwick DR. Late HIV diagnosis and missed opportunities for testing: piloting a standardised, multi-source review process. Int J STD AIDS. 2020;31(3):208–13.
Acknowledgements
The authors are grateful to Chinese Center for Disease Prevention and Control, Zhejiang University, school of Medicine and the Ethiopian Public Health Institute. The authors would like to express their special thanks to all data collectors and the study participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas: took part in drafting, revising, or critically reviewing the article; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The ethical approval was obtained from the Ethiopian Public health Institute Scientific and Ethical review office (SERO) with approval number; EPHI-IRB-187-2020. As the study was conducted using secondary data, study participants were not subject to any harm. During data extraction, no personal identification methods were used on data collection formats. Considering there will be no harm for the study participants and since the data were collected confidentially and given the study will benefit the HIV program in the country, informed consent was waived by the scientific and Ethical review office of the Ethiopian Public Health Institute. The study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Authors and responsible authorities were informed and agreed for this publication.
Competing interests
There was no competing interest, between the authors, declared for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Operational definition
- Adults
-
For the purposes of this study, adults are defined as the population aged 15-64 years.
- Antiretroviral (ARV)
-
A type of medication used in the treatment of HIV.
- Antiretroviral therapy (ART)
-
Treatment with antiretroviral (ARV) drugs that inhibit the ability of HIV to multiply in the body, leading to improved health and survival among HIV-positive persons.
- Enumeration area (EA)
-
A limited geographic area defined by the national statistical authority and the primary sampling unit for the Population-Based HIV Impact Assessment (PHIA) surveys.
- HIV viral load (VL)
-
The concentration of HIV virus particles in the blood, expressed as copies per milliliter (copies/mL).
- HIV viral load suppression (VLS)
-
An HIV VL of less than 1000 copies per mL
- Risk group for universal testing
-
By gender (female); by age (Elderly (>50 years old) and young, by marital status (Widowed or separated), by geography (high risk and burden regions; Gambella and Addis Ababa).
- Late diagnosis and new infection
-
PLHIV who were classified by LAg avidity assay
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Getaneh, Y., Ayalew, J., He, Q. et al. Universal HIV testing and the impact of late diagnosis on disease stage among adults in urban Ethiopia. Trop Med Health 51, 4 (2023). https://doi.org/10.1186/s41182-023-00494-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-023-00494-z