Abstract
Background
The growing burden of diabetes mellitus (DM) and hypertension (HTN) on the background of endemic Human Immuno-deficiency Virus (HIV) and tuberculosis (TB) is a concern in low- and middle-income countries. We aimed to describe annual trends in admissions, mortality rates and premature mortality (years of potential life lost—YPLLs) due to HIV, tuberculosis (TB), diabetes mellitus (DM) and hypertension (HTN) in Uganda.
Methods
We conducted a retrospective cohort study, retrieving electronic records of adults admitted to Mulago and Kiruddu national referral hospitals medical wards between 1st January 2011 and 31st December 2019. We used STATA BE 17.0 and GraphPad Prism 8.0.2 to compute total admissions, inpatient crude mortality rates, and YPLLs; and demonstrate trends using Mann–Kendall test.
Results
Of 108,357 admissions, 55,620 (51.3%) were female, 15,300 (14.1%) were recorded in 2012, and 22,997 (21.2%) were aged 21–30 years. HIV, TB, DM and HTN accounted for 26,021 (24.0%); 9537 (8.8%); 13,708 (12.7) and 13,252 (12.2%) of all admissions, respectively. Overall inpatient mortality was 16.7% (18,099/108,357), 53.5% (9674/18,099) were male, 21.5% (3898) were aged 31–40 years and 2597 (14.4%) were registered in 2013. HIV, TB, DM and HTN accounted for 35.6% (6444), 14.6% (2646), 9.1% (1648) and 11.8% (2142) of all deaths, respectively. Total admissions (Kendall’s tau-B = − 0.833, p < 0.001) and deaths declined (Kendall’s tau-B = − 0.611, p = 0.029). A total of 355,514 (mean = 20.8 years, SD 30.0) YPLLs were recorded, of which 54.6% (191,869) were in males; 36.2% (128,755) were among those aged 21–30 years and were recorded in 2012 (54,717; 15.4%). HIV, TB, DM and HTN accounted for 46.5% (165,352); 19.5% (69,347); 4.8% (16,991) and 4.5% (16,167) of YPLLs, respectively. Proportionate contribution of HIV to deaths and YPLLs declined, remained stagnant for TB; and increased for both DM and HTN.
Conclusion
TB and HIV account for higher though declining, while DM and HTN account for lower albeit rising morbidity and premature mortality among adult medical patients in Uganda. TB prevention and treatment; and DM/HTN service integration in HIV care should be optimized and scaled up.
Similar content being viewed by others
Introduction
Human immunodeficiency virus (HIV) and tuberculosis (TB) still account for substantial adult morbidity and mortality in low- and middle-income countries (LMICs), Uganda inclusive [1]. In 2020, there were over 7000 TB-related deaths and 90,000 new TB cases in Uganda [2]. Moreover, there were 38,000 new HIV infections and 21,000 HIV-related deaths in Uganda in 2020 [3]. There is, however, growing concern over the rapidly rising burden of premature mortality attributable to non-communicable diseases (NCDs) such as diabetes mellitus (DM) and hypertension, in Uganda and sub-Saharan Africa [4]. The rise in DM is expected to retard progress towards elimination of TB since it increases the risk of active TB disease threefold, and increases risk of sub-optimal TB treatment outcomes [5]. In addition, the scale-up of universal ART has resulted in more people living with HIV (PLHIV) surviving into older age, and hypertension, a key risk factor for cardiovascular mortality has been identified as a leading cause of non-AIDS-related mortality among PLHIV [6]. The dual burden of NCDs and infectious diseases is expected to strain health systems in LMICs and Uganda in particular [7,8,9].
Due to the rapid scale-up of universal antiretroviral therapy in Uganda, over the last nearly two decades, HIV incidence, morbidity and mortality have declined [10, 11]. However, from a recent study of adult patients admitted at a national referral hospital, at least 25% of admissions were HIV positive and HIV-positive individuals contributed almost half of all deaths [12]. Moreover, the same study showed a rise in inpatient mortality over a period of 4 years [12]. This was on the background of increasing proportions of patients admitted with hypertension and diabetes mellitus [12]. It however remains unclear whether these observations can be attributed to the growing burden of NCD-associated morbidity among ageing PLHIV or a growing burden of HIV among young people with NCDs. To inform re-prioritization of resources for age-appropriate NCD or HIV disease prevention, assessment of trends in premature mortality attributable to each disease condition is important. The Years of Potential Life Lost (YPLL) metric, introduced by the United States Centers for Disease Control and Prevention (CDC) in 1982, overcomes the effect of ageing-related disease deaths that often skew relative mortality measures, by weighting each death as the difference between an expected age of survival and observed age at death [13,14,15,16,17]. This allows for distinction between true increase in disease-specific mortality and increase in mortality attributable to ageing.
In this study, we determined disease (HIV, TB, DM and hypertension) and sex-specific trends in proportionate admissions, mortality, and premature mortality (YPLL) on adult medical inpatient wards at Mulago and Kiruddu national referral hospitals in Uganda over a 9-year-period (2011–2019).
Methods
Study design
This was a retrospective cohort study. We obtained patient data from the Rainer Arnolds Senior House Officers Training support (RASHOTs) database for patients admitted to adult medical inpatient wards at Mulago and Kiruddu national referral hospitals (NRH) from 2011 to 2019 [12].
Study setting
We retrieved records of patients admitted to the adult medical wards at Mulago NRH (2011–2014) and Kiruddu NRH from 2014 to 2020. In 2014, the Government of Uganda (GoU) undertook a major renovation of Mulago NRH that necessitated migration of medical inpatient services to Kiruddu Hospital, which had been newly upgraded from a divisional hospital [18, 19]. Mulago NRH is located in Kawempe Division; whereas Kiruddu NRH is located in Makindye division of the capital city. The RASHOTs database was the central repository for adult medical inpatient data for the study period.
Data collection
We retrieved data on patient sex, age at admission, and diagnoses at discharge or death; and downloaded as spreadsheets, which we cleaned and conducted preliminary analyses using Microsoft Excel. Diagnoses were made by specialist physicians on inpatient wards using clinical algorithms involving patient clinical history, physical examination, laboratory tests and radiological imaging, where applicable and available. We carried out additional analyses and generated graphs using GraphPad Prism 8. Individuals with incomplete data (age, sex, or diagnoses) were excluded from the data analysis. For each patient who died, we computed YPLL by subtracting the age at death from the sex-specific life expectancy at birth in Uganda as determined by the 2014 Population Census, i.e. female—64.5 years and male—62.8 years [20]. Where the difference was less than zero (patient died at an age older than the sex-specific life-expectancy), the YPLL was reported as zero.
Data analysis
We determined percentage contribution to total inpatient admissions, mortality and YPLLs for each sex, age group and major disease conditions: HIV, TB, DM, and Hypertension. We summarized patient characteristics as frequencies and demonstrated trends using line graphs; and, computed total and mean YPLLs by year, sex, and disease condition. We calculated inpatient mortality rate as a percentage of deaths divided by number of admissions. We determined disease, age-group and sex-specific total annual YPLLs and used Mann–Kendall test to analyse for trends in number of admissions, deaths and total annual YPLLs. We applied the Mann–Kendall test to overall absolute numbers of admissions, deaths and total YPLLs; and then to proportions of the different sub-populations; using Stata BE 17.0. We compared median YPLLs between sexes and disease classes using Mann–Whitney U test. A p < 0.05 was considered statistically significant. We defined trend as the magnitude and direction of the Mann–Kendall tau-B coefficient between the outcome and time in years (2011–2019).
Results
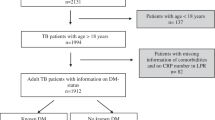
We retrieved 128,086 records, of which 18,837 were duplicates, and 892 were excluded because of incomplete data as shown in Fig. 1.
Trends in admissions
Of a total of 108,357 inpatient admissions, 51.3% (55,620) were female, 21.2% (22,997) were aged 21–30 years, 14.1% (15,300), 24.0% were HIV positive. The proportion of admissions that were 41–50, 51–60 and over 70 years of age increased across the period (Table 1).
Among females, HIV or TB admissions were highest in the 21–30 years age group (34.5%, 40.1%, respectively) while among males, it was in the 31–40 years age group (37.2% and 35.4%, respectively). DM admissions among females were highest in the 51–60 age group (24.2%), and in the 41–50 years age group among males (20.3%). HTN admissions among both females and males were highest in those above 70 years age group (24.5% and 21.6%, respectively).
Total admissions declined (TB = − 0.83; p < 0.01, Kendall’s score = − 30, SE = 9.59); the proportions of admissions in the age groups: 20 years and below; 21–30 years, 31–40 years declined (TB = − 0.61, p = 0.03, score = −22; TB = − 0.89, p < 0.01, Kendall’s score = − 22; TB = − 0.67, p = 0.02, Kendall’s score = − 24, SE = 9.59, respectively) while the proportions of admissions in the older age groups (51–60, 61–70 and over 70 years) increased. The proportions of patients admitted with HIV declined (TB = − 0.67; p = 0.02, Kendall’s score = − 24, SE = 9.59), remained stable for TB (TB = − 0.39, p = 0.18, Kendall’s score = − 14) and DM (TB = 0.39, p = 0.18, Kendall’s score = 14, SE = 9.59) while these increased for HTN (TB = 0.67, p = 0.02, Kendall’s score = 24 SE = 9.59) (Table 1, Fig. 2a) and these appeared similar between males and females (Fig. 2b, c).
Annual trends in total and proportionate admissions and deaths by disease. a Annual trends in total and proportionate admissions by disease. b Annual trends in female total and proportionate admissions by disease. c Annual trends in male total and proportionate admissions by disease. d Annual trends in total and proportionate deaths by disease. e Annual trends in female total and proportionate deaths by disease. f Annual trends in male total and proportionate deaths by disease
Comorbidity among admissions
Among HIV admissions, 25.9% (6738/26,021) of HIV-positive patients had tuberculosis, 2.6% (666) and 2.6% (665) had diabetes mellitus and hypertension, respectively. Among patients with tuberculosis, 70.7% (6738/9537) had HIV, 2.2% (214) and 1.0% (94) had diabetes mellitus and hypertension, respectively. Among patients with diabetes mellitus, 4.9% (666/13708), 1.6% (214), 27.6% (3790) had HIV, tuberculosis and hypertension, respectively. In patients with hypertension, 5% (665/13252), 0.7% (94), and 28.6% (3790) had HIV, TB and DM, respectively.
Trends in inpatient mortality rate
Overall inpatient mortality rate of 16.7% (18,099 deaths) was registered. Overall absolute number of deaths declined (TB = − 0.61, p = 0.03, Kendall’s score = − 22, SE of score = 9.59), but inpatient mortality rate remained stable (TB = 0.17, p = 0.60, Kendall’s score = 6, SE = 9.59) (Table 2, Fig. 2d–f). Females accounted for 46.5% of deaths, while 35.6% and 24.9% of deaths occurred among HIV-positive patients and ages 31–40 years, respectively. Of the 6444 deaths among HIV-positive patients, 32.1% (2070), 1.7% (108), 2.0% (129) had tuberculosis, diabetes mellitus, hypertension, respectively. Of the 2646 deaths among TB patients, 78.2% (2070), 1.4% (36), 0.6% (17) had HIV, DM or HTN, respectively. Of the 1648 deaths among DM patients, 6.6% (108), 2.2% (36), 33.6% (554) had HIV, TB or HTN, respectively. Of the 2142 deaths among HTN patients, 6.0% (129), 0.8% (17), 25.9% (554) had HIV, TB or HTN, respectively.
Among HIV-positive deaths, majority were in the 31–40 age group (2257/6444, 35.0%). The same age group accounted for the highest proportion of TB deaths (909/2646, 34.4%). Individuals above 70 years of age accounted for most of the deaths in hypertension (703/2142, 32.8%). The proportionate contribution to deaths reduced for the younger age groups and increased for the older age groups.
Trends in premature mortality
The deaths recorded in the period resulted in 355,514 YPLLs; majority of which occurred among males (54.0%), were attributable to HIV (46.5%) and among 21- to 30-year-olds (36.2%) (Table 3). Overall, TB accounted for 19.5% (69,347/355,514) of YPLLs while DM and HTN accounted for 4.8% (16,991) and 4.5% (16,167), respectively. Median YPLL was similar between sexes (20.8, p = 0.14) (Fig. 3a). Disease-specific median YPLLs were higher for HIV compared to TB, and higher for HTN compared to DM (Fig. 3b). Among HIV deaths, median YPLL was higher among females than males (27.8 vs 24.8, p < 0.01), similarly among TB deaths (29.8 vs 26.8, p < 0.001) and DM deaths (5.8 vs 3.8, p = 0.08). In HTN deaths, median YPLL was higher among males than among females (11.8 vs 14.8, p ≤ 0.01) (Fig. 4).
Boxplots comparing disease-specific median YPLLs by sex. a. Boxplot comparing median HIV YPLLs between females and males. b. Boxplot comparing median DM YPLLs between females and males. c. Boxplot comparing median TB YPLLs between females and males. d. Boxplot comparing median HTN YPLLs between females and males
Overall, total YPLLs declined over the decade (TB = − 0.778, p < 0.01) (Table 3, Fig. 5b–f).
Annual trends in mortality rates, overall and proportionate disease premature mortality by sex. a. Annual trends in overall mortality rates by disease. b. Annual trends in total and proportionate YPLLs by disease and sex. c. Annual trends in HIV YPLLs by sex. d. Annual trends in TB YPLLs by sex. e. Annual trends in DM YPLLs by sex. f. Annual trends in HTN YPLLs by sex
Proportionate contribution to YPLLs by females remained constant. Over the period, the contribution to YPLLs by HIV declined (TB = − 0.78, p < 0.01), remained stable for TB (TB = − 0.28, p = 0.35); and increased for both DM and HTN (TB = 0.56, p = 0.05; TB = 0.83, p < 0.01).
Discussion
We retrospectively reviewed adult inpatient hospital admission data at national referral hospitals for the period 2011–2019, and analysed for trends in admissions, deaths, mortality rates and premature mortality (measured as years of potential life lost—YPLL), focusing on the two commonest infectious (HIV and TB) and non-infectious (hypertension and diabetes mellitus) disease conditions. More than two-thirds of TB admissions were HIV co-infected, over a quarter of DM patients had hypertension. Females accounted for more than half of HIV-related admissions across the decade. We found declines in overall admissions, deaths, and premature mortality among patients admitted to medical wards at Mulago and Kiruddu NRHs. HIV and TB accounted for the largest proportion of admissions, deaths and YPLLs. Whereas females accounted for more admissions, deaths and YPLLs were higher among males, and yet HIV-related YPLLs were higher among females. Majority of HIV and TB-related admissions and deaths occurred in young adults (21–30 and 31–40 years), while majority of DM and HTN-related admissions and deaths occurred in older individuals. HIV co-morbidity was high among TB patients and TB-related deaths. HIV-, TB- and DM-related YPLLs were higher among females than among males, while hypertension-related YPLLs were higher among males. Proportions of DM and HTN among admissions, deaths and YPLLs increased significantly during the decade.
The decline in patient admissions and absolute number of deaths is probably due to the declining national burden of HIV, which accounted for a significant number of medical inpatient admissions and deaths in the 1990s and early 2000s [21, 22]. In 1994, Tembo et al. reported that HIV accounted for 55.6% of adult inpatient admissions at a large urban hospital in Uganda [21]. In addition, the total years of life lost among admitted medical patients, due to endemic diseases such as HIV and TB is declining over the years [23], in tandem with reported declines in HIV-associated morbidity and mortality over the last decade due to roll-out of universal antiretroviral therapy [11, 24,25,26]. Our study also found that HIV-related conditions still account for the highest proportion of premature mortality in this population. This is similar to what was found by Rumisha et al. in Tanzania where HIV was the leading cause of premature mortality [27], and is further supported findings from the Global Burden of Disease study where HIV is among the leading causes of mortality in Uganda [1, 28]. In an earlier autopsy study describing causes of death among hospitalized patients at Mulago NRH, 83% of the deaths among HIV + individuals were from infectious causes [29]. Equally, between 2002 and 2012, at an urban HIV clinic, TB and other infectious diseases accounted for majority of deaths. Over the period, the contribution of TB and other infectious diseases declined, whereas non-communicable disease conditions accounted for a growing number of deaths in this population [30]. In a similar study in Malawi, 71% of deaths among patients less than 55 years of age were due to infectious diseases [31], while another study in Southern Nigeria also showed infectious diseases as a leading cause of inpatient mortality [32].
The higher burden of premature mortality attributable to HIV among females than males corroborates the higher prevalence of HIV among females at younger age in Uganda, and is also supported by global and local reports that show a rising number of new HIV infections among adolescent girls and young women [33, 34]. The higher burden of HIV-associated YPLLs among females was also reported in a population-based cohort in South-Western Uganda [35]. Of note, however, associated mortality was higher in males than among females, probably suggesting delayed care seeking among middle-aged compared to young adult males. This is similar to findings by Rubaihayo et al. in outpatient HIV clinics [23]. Our findings support global and local efforts to invest in HIV prevention among adolescent girls and young women as this is resulting in significant preventable premature adult mortality, and promotion of healthcare seeking among middle-aged males to reduce overall HIV-related mortality.
In this study, more than two-thirds of TB patients were HIV positive and this highlights HIV as the most important risk factor for TB disease in our setting. However, we demonstrate significant declines in TB-associated morbidity, mortality and premature mortality across the decade, and this is similar to what was reported by Kiragga et al. [6]. The high TB-associated morbidity and mortality among HIV-positive patients underlines missed opportunities for TB diagnosis and prevention in the HIV program [36]. Early diagnosis and treatment of TB, coupled with universal access to TB preventive therapy and anti-retroviral therapy (ART) are effective tools that have not been adequately scaled up especially in vulnerable sub-populations [37,38,39]. Kalema et al. found that about half of PLHIV at an urban outpatient clinic were not initiated on TB preventive therapy [40]. This may explain the disproportionately high contribution of TB to mortality in HIV participants, observed in this study. Nevertheless, the decline in absolute numbers of TB admissions, deaths and YPLLs over the years attest to progress made in ending the TB epidemic in Uganda [41].
The rise in DM and HTN-associated morbidity, proportionate mortality and premature mortality both in the HIV-negative and HIV-positive participants underscores the growing burden of these NCDs in our setting [1]. The rise in DM/HTN co-morbidity among PLHIV has been attributed to natural ageing as PLHIV attain comparable life expectancies as HIV-negative individuals following universal ART roll-out; metabolic disorders associated with HIV, opportunistic infections and antiretroviral drugs [42, 43]. We report a higher prevalence of DM among PLHIV (2.7% vs < 1%) than was reported from a population-based study in South Central Uganda [44], and yet this is lower than was reported by Kansiime et al. (4.7%) suggesting population differences [42]. The rise in DM/HTN co-morbidity and premature mortality among PLHIV threatens to reverse some of the gains made in achieving zero HIV-related deaths towards ending HIV as an epidemic. This threatens progress towards eliminating HIV-related deaths, and is supported by findings from Kiragga et al. that showed increasing role of NCDs as causes of death among PLHIV on ART in an urban outpatient clinic [6]. Kwarisiima et al. therefore recommend HTN and DM care integration in HIV chronic care clinics to prevent morbidity and mortality from HTN, DM and HIV, tailored to context [45, 46].
Strengths of the study The study used a large dataset from hospital records. This is the first study to utilize hospital records to describe annual trends in premature mortality from HIV, TB, DM and hypertension among adult inpatients in Uganda.
Study limitations
This study used routinely collected health facility data that were incomplete in a number of patients, which could result in biased estimation of study outcomes.
We based our analysis on reported clinical and not postmortem diagnoses which may bias our estimates. However, since most of the final diagnoses for most patients are made by senior physicians, supported by imaging and laboratory tests, we are confident that the diagnoses are fairly accurate.
In computing the years of potential life lost, we assumed the same life expectancy age across the years, which may have overestimated the YPLL for years before 2014 when period life expectancy could have been lower. This is an inherent limitation of the YPLL method, but nevertheless allows for age-based weighting of deaths to further characterize disease burden.
We may have underestimated the respective disease burdens by not including data on co-morbidly affected individuals treated at specialized centres such as the Uganda Heart Institute and Uganda Cancer Institute. Data on these are not available through the RASHOTs database.
Conclusions and recommendations
HIV and TB contribute a higher burden of premature mortality among inpatients than non-infectious diseases like HTN and DM. This is higher among females. HIV and TB account for a disproportionate burden of premature mortality among inpatients, more-so among females. Overall, premature mortality among inpatients has declined over the 10-year period. We recommend further implementation science research to inform optimization and scale-up of primary and secondary prevention of tuberculosis among individuals with HIV, integration of HTN and DM prevention in HIV care; and renewed focus on HIV prevention among young females.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- COVID19:
-
Corona virus 2019 disease
- DM:
-
Diabetes mellitus
- GoU:
-
Government of Uganda
- HIV:
-
Human immunodeficiency virus
- LMICs:
-
Low- and middle-income countries
- MoH:
-
Ministry of Health
- NCDs:
-
Non-communicable diseases
- NRH:
-
National referral hospital
- OR:
-
Odds ratio
- PLHIV:
-
People living with HIV
- RASHOTs:
-
Rainer Arnolds Senior House Officers Training support
- RR:
-
Risk ratio
- TB:
-
Tuberculosis
- TB :
-
Kendall’s tau-B
- WHO:
-
World Health Organization
- YPLLs:
-
Years of potential life lost
References
IHME. Global Burden of Disease: Uganda Profile. 2010;2010(Gbd):4pp. Available from: http://www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_uganda.pdf.
Stop TB Partnership. Tuberculosis situation in 2020: Uganda. 2022.
UNAIDS. final-2021-hiv-aids-factsheet. Factsheet: Facts on HIV and AIDS in Uganda 2021 [Internet]. [cited 2022 Jul 29]; Available from: https://uac.go.ug/media/attachments/2021/09/13/final-2021-hiv-aids-factsheet.pdf.
Uganda | Institute for Health Metrics and Evaluation [Internet]. [cited 2022 Feb 25]. Available from: https://www.healthdata.org/uganda.
Harries AD, Kumar AMV, Satyanarayana S, Lin Y, Zachariah R, Lönnroth K, et al. Addressing diabetes mellitus as part of the strategy for ending TB. Trans R Soc Trop Med Hyg. 2015;110(3):173–9.
Kiragga AN, Mubiru F, Kambugu AD, Kamya MR, Castelnuovo B. A decade of antiretroviral therapy in Uganda: what are the emerging causes of death? BMC Infect Dis. 2019;19(1).
Katende D, Mutungi G, Baisley K, Biraro S, Ikoona E, Peck R, et al. Readiness of Ugandan health services for the management of outpatients with chronic diseases. Trop Med Int Health. 2015;20(10):1385–95.
Rogers HE, Akiteng AR, Mutungi G, Ettinger AS, Schwartz JI. Capacity of Ugandan public sector health facilities to prevent and control non-communicable diseases: an assessment based upon WHO-PEN standards. BMC Health Serv Res. 2018;18(1):1–13.
Settumba SN, Sweeney S, Seeley J, Biraro S, Mutungi G, Munderi P, et al. The health system burden of chronic disease care: an estimation of provider costs of selected chronic diseases in Uganda. Trop Med Int Health. 2015;20(6):781–90.
AIDS Control Program UM of H. The 2019 HIV epidemiological surveillance report for Uganda [Internet]. Kampa; 2019. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwj6tMjC28XwAhV3QhUIHRrSAmgQFjAOegQIGhAD&url=https%3A%2F%2Fwww.health.go.ug%2Fdownload-attachment%2F3brCB1ufww53zXB9VbqX0y4Yl-uEsyjlJqfdxUHqIu0%2C&usg=AOvVaw0OqGc5DpkTX.
Nabukalu D, Reniers G, Risher KA, Blom S, Slaymaker E, Kabudula C, et al. Population-level adult mortality following the expansion of antiretroviral therapy in Rakai, Uganda. Popul Stud. 2019;74(1):93–102. https://doi.org/10.1080/00324728.2019.1595099.
Kalyesubula R, Mutyaba I, Rabin T, Andia-Biraro I, Alupo P, Kimuli I, et al. Trends of admissions and case fatality rates among medical in-patients at a tertiary hospital in Uganda; a four-year retrospective study. PLoS ONE [Internet]. 2019;14(5):1–14. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0216060.
Yen EY, Singh RR. CS-32 SLE-YPLL (years of potential life lost) as a measure of relative burden of premature mortality. Lupus Sci Med. 2018;5(Suppl 2):A40–1.
Gardner JW, Sanborn JS. Years of potential life lost (YPLL)—what does it measure? Epidemiology [Internet]. 1990;1(4):322–9.
Gordis L. Epidemiology. 5th ed. Philadelphia: Elsevier Saunders; 2014. p. 68–73.
Years of Potential Life Lost (YPLL)—What Does it Measure? on JSTOR [Internet]. [cited 2021 Jul 10]. Available from: https://www.jstor.org/stable/25759821?casa_token=xfeiz57kBVwAAAAA:QaYKW0g3G2c3xVHrvfBDGHDvsX0wjbb_Yw2ccJmX-9ArwS429gYlp7NF8_crtTrMiPsvB9LbAbNDhX0CslQOjPu0Y_Ms9XV6FeXhkayJqbtxfmgJSyPH.
Song M, Hildesheim A, Shiels MS. Premature years of life lost due to cancer in the United States in 2017. Cancer Epidemiol Prev Biomarkers [Internet]. 2020;29(12):2591–8.
Ninsiima R, Nakabugo Z. Kiruddu hospital in race against time to fill Mulago hospital void. The Observer. 2016.
Kiruddu Referral Hospital. Who we are. 2022.
UBOS. Statistical Abstract, 2019. Uganda Bureau of Statistics Statistics. 2019;185.
Tembo G, Friesan H, Asiimwe-Okiror G, Moser R, Naamara W, Bakyaita N, et al. Bed occupancy due to HIV/AIDS in an urban hospital medical ward in Uganda. AIDS. 1994;8(8):1169–72.
Granich R, Gupta S, Hersh B, Williams B, Montaner J, Young B, et al. Trends in AIDS deaths, new infections and ART coverage in the top 30 countries with the highest AIDS mortality Burden; 1990–2013. PLoS ONE. 2015;10(7): e0131353.
Rubaihayo J, Tumwesigye NM, Konde-Lule J, Makumbi F, Nakku EJ, Wamani H, et al. Trends and predictors of mortality among HIV positive patients in the era of highly active antiretroviral therapy in Uganda. Infect Dis Rep [Internet]. 2015;7(3):66–73.
Kasamba I, Baisley K, Mayanja BN, Maher D, Grosskurth H. The impact of antiretroviral treatment on mortality trends of HIV-positive adults in rural Uganda: a longitudinal population-based study, 1999–2009. Trop Med Int Health. 2012;17(8):e66-73.
Slaymaker E, Todd J, Marston M, Calvert C, Michael D, Nakiyingi-Miiro J, et al. How have ART treatment programmes changed the patterns of excess mortality in people living with HIV? Estimates from four countries in East and Southern Africa. https://doi.org/10.3402/gha.v722789.
Otieno G, Whiteside YO, Achia T, Kwaro D, Zielinski-Gutierrez E, Ojoo S, et al. Decreased HIV-Associated mortality rates during scale-up of antiretroviral therapy, 2011–2016. AIDS. 2019;33(15):2423–30.
Rumisha SF, George J, Bwana VM, Mboera LEG. Years of potential life lost and productivity costs due to premature mortality from six priority diseases in Tanzania, 2006–2015. PLoS ONE. 2020;15(6): e0234300.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396(10258):1204–22.
Cox JA, Lukande RL, Nelson AM, Mayanja-Kizza H, Colebunders R, van Marck E, et al. An autopsy study describing causes of death and comparing clinico-pathological findings among hospitalized patients in Kampala, Uganda. PLoS ONE. 2012;7(3): e33685.
Cox JA, Kiggundu D, Elpert L, Meintjes G, Colebunders R, Alamo S. Temporal trends in death causes in adults attending an urban HIV clinic in Uganda: a retrospective chart review. BMJ Open [Internet]. 2016;6(1):e008718.
Allain TJ, Aston S, Mapurisa G, Ganiza TN, Banda NP, Sakala S, et al. Age related patterns of disease and mortality in hospitalised adults in Malawi. PLoS ONE. 2017;12(1):e0168368.
Okoroiwu HU, Uchendu KI, Essien RA. Causes of morbidity and mortality among patients admitted in a tertiary hospital in southern Nigeria: a 6 year evaluation. PLoS ONE. 2020;15(8):e0237313.
Birdthistle I, Tanton C, Tomita A, de Graaf K, Schaffnit SB, Tanser F, et al. Recent levels and trends in HIV incidence rates among adolescent girls and young women in ten high-prevalence African countries: a systematic review and meta-analysis. Lancet Glob Health. 2019;7(11):e1521–40.
UNAIDS. Ending the AIDS epidemic for adolescents, with adolescents. https://www.UnfpaOrg [Internet]. 2016;1–26. Available from: https://www.unaids.org/sites/default/files/media_asset/ending-AIDS-epidemic-adolescents_en.pdf%0A. http://www.unaids.org/en/resources/documents/2016/ending-AIDS-epidemic-adolescents.
Asiki G, Reniers G, Newton R, Baisley K, Nakiyingi-Miiro J, Slaymaker E, et al. Adult life expectancy trends in the era of antiretroviral treatment in rural Uganda (1991–2012). AIDS. 2015;30(3):487–93.
Kakame KT, Namuhani N, Kazibwe A, Bongomin F, Baluku JB, Baine SO. Missed opportunities in tuberculosis investigation and associated factors at public health facilities in Uganda. BMC Health Serv Res. 2021;21(1):359.
Pathmanathan I, Ahmedov S, Pevzner E, Anyalechi G, Modi S, Kirking H, et al. TB preventive therapy for people living with HIV: key considerations for scale-up in resource-limited settings [Internet]. Int J Tuberc Lung Dis. 2018;22:596–605.
Uppal A, Rahman S, Campbell JR, Oxlade O, Menzies D. Economic and modeling evidence for tuberculosis preventive therapy among people living with HIV: a systematic review and meta-analysis. PLoS Med. 2021;18(9):e1003712.
Lim RK, Semitala FC, Atuhumuza E, Sabiti L, Namakula-Katende J, Muyindike WR, et al. Patient choice improves self-efficacy and intention to complete tuberculosis preventive therapy in a routine HIV program setting in Uganda. PLoS ONE [Internet]. 2021;16(2):1–6. https://doi.org/10.1371/journal.pone.0246113.
Kalema N, Semeere A, Banturaki G, Kyamugabwa A, Ssozi S, Ggita J, et al. Gaps in TB preventive therapy for persons initiating antiretroviral therapy in Uganda: an explanatory sequential cascade analysis. Int J Tuberc Lung Dis [Internet]. 2021;25(5):388–94.
Zawedde‐Muyanja S, Manabe YC, Musaazi J, Mugabe FR, Ross JM, Hermans S. Anti‐retroviral therapy scale‐up and its impact on sex‐stratified tuberculosis notification trends in Uganda. J Int AIDS Soc. 2019;22(9).
Kansiime S, Mwesigire D, Mugerwa H. Prevalence of non-communicable diseases among HIV positive patients on antiretroviral therapy at joint clinical research centre, Lubowa, Uganda. PLoS ONE [Internet]. 2019;14(8):e0221022. https://doi.org/10.1371/journal.pone.0221022.
Lubega G, Mayanja B, Lutaakome J, Abaasa A, Thomson R, Lindan C. Prevalence and factors associated with hypertension among people living with HIV/AIDS on antiretroviral therapy in Uganda. Pan Afr Med J. 2021;38.
Enriquez R, Ssekubugu R, Ndyanabo A, Marrone G, Gigante B, Chang LW, et al. Prevalence of cardiovascular risk factors by HIV status in a population‐based cohort in South Central Uganda: a cross‐sectional survey. J Int AIDS Soc. 2022;25(4).
Kwarisiima D, Atukunda M, Owaraganise A, Chamie G, Clark T, Kabami J, et al. Hypertension control in integrated HIV and chronic disease clinics in Uganda in the SEARCH study. BMC Public Health. 2019;19(1):511.
Davis K, Perez-Guzman P, Hoyer A, Brinks R, Gregg E, Althoff KN, et al. Association between HIV infection and hypertension: a global systematic review and meta-analysis of cross-sectional studies. BMC Med. 2021;19(1):105.
Acknowledgements
The authors acknowledge support from the RASHOTs staff (Namakula Cissy, Nagganja Cate and Akullu Vicky) who played a pivotal role in retrieval and cleaning of the study dataset. We also acknowledge Ms. Nakagwa Mariam Lukwago of Tuberculosis and Comorbidities Research Consortium for providing logistical support during the study.
Funding
IAB was funded by the Government of Uganda through the Makerere University Research Investment Fund (MakRIF) Round One. (https://rif.mak.ac.ug/). RK is a Rainer-Arnolds fellow, and received funding to set up the RASHOTS database through the Uganda Foundation (https://ugandafoundation.com/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
AK contributed to conception, study design, data collection, analysis and interpretation; preparation of the draft and final manuscript. KRB contributed to study design, data analysis and interpretation, preparation of the draft and final manuscript. APK, SN, PS, FB, JBB, DK, GPA, MRK, HMK, PBK and MK contributed to supervision of data collection, data interpretation, preparation of draft and final manuscript. RK and IAB contributed to funding acquisition, study conceptualization, design; interpretation of study findings, preparation of the draft and final versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved under the machine learning project approved by the Makerere University School of Medicine Research and Ethics committee (Number: 2020/098) and the Uganda National Council for Science and Technology (Number: HS745ES). The study used secondary data and the need for informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that no competing interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kazibwe, A., Bisaso, K.R., Kyazze, A.P. et al. HIV, tuberculosis, diabetes mellitus and hypertension admissions and premature mortality among adults in Uganda from 2011 to 2019: is the tide turning?. Trop Med Health 50, 54 (2022). https://doi.org/10.1186/s41182-022-00447-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-022-00447-y