Abstract
Background
Little information is available on the validity of anthropometry or impedance-based equations for prediction of total body water (TBW) in African children. This study was designed to validate and develop equations to predict total body water in Cameroonian children.
Methods
TBW was measured by deuterium dilution in 102 children between 24 and 60 months of age and compared with the ones predicted by 5 anthropometric and 7 BIA equations. Multiple linear regression analysis was used to develop prediction equations for TBW from anthropometric parameters.
Results
Unacceptable discrepancies in the estimates of TBW at individual level were noted with all the equations tested. The following new anthropometry and BIA equations for the estimation of TBW were respectively developed: TBW = 6.488 + 0.434 × sex − 0.039 × age + 0.670 × weight − 0.081 × MUAC (cm) − 0.372 × BMI (adjusted R 2 = 0.71, RMSE = 3.6), and TBW = −6.206 + 0.0037 × height2/Z − 0.041 × age + 0.265 × weight + 0.1214 × height (adjusted R 2 = 0.68, RMSE = 1.4). The cross-validation procedures revealed that the predicted values of TBW compared with measured values are accurate at a group level.
Conclusion
The current published anthropometric and BIA equations are invalid for the estimation of TBW in Cameroonian preschool children. The newly developed anthropometry or BIA prediction equations are valid for use in Cameroonian children aged 24–60 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Nutrition transition, characterized by changes in food consumption habits and lifestyle, which is manifested by increase in consuming energy dense food and decrease of physical activities, has been reported in several developing countries [1]. This situation, known as the double burden malnutrition [2], is associated with increasing prevalence of obesity and non-communicable diseases in people of all age groups, while undernutrition remains a public health concern [3]. Epidemiological studies found high correlation between obesity in childhood and adult obesity [4, 5]. This implies the need to assess body composition in children.
Body composition which includes fat mass (FM) and fat-free mass (FFM) is a sensitive indicator of current health [6] and nutritional status [7] in children. The best way to assess body composition is by applying multicomponent models, in which measurements of at least two (three-component model) or more (four- or five-component models) constituents of the FFM are made [8, 9]. This approach usually requires measurement of total body water (TBW) (by isotope dilution), body density (usually by hydrodensitometry), and mineral content (by energy x-ray absorptiometry [DEXA]) [8, 9]. Although providing accurate information, this model is expensive, technically demanding, and difficult to perform on children.
The two-compartment model in which body weight is divided into FM and FFM is suitable for use in a wide range of settings. In this model, measurement of TBW can be used to predict fat-free mass (FFM), based on the principle that FFM contains a relatively constant proportion of water [10, 11]. TBW can be measured accurately and safely in children by using deuterium dilution technique. Unfortunately, this technique is relatively expensive, not widely available, and difficult to apply to many subjects. Therefore, cheap and simple methods are needed for routine clinical and epidemiological field studies, especially in developing countries. In this regard, anthropometry and bioelectric impedance analysis (BIA) have drawn attention as inexpensive, simple to use, and portable techniques. However, these are indirect methods based on prediction equations developed in a population in which the method was validated against a reference method, and are therefore population-specific [12].
Since the validity of anthropometry and BIA prediction equations in African children has not yet been demonstrated, the aims of the present study were to evaluate if some available prediction equations are applicable for Cameroonian children, and to develop new equations for predicting TBW as measured by deuterium dilution.
Methods
Subjects
One hundred two children, girls (n = 55) and boys (n = 47), between 24 and 60 months of age, were selected from an urban nursery school in Yaoundé, Cameroon. All measurements were performed by trained staff in the morning between 8 am and 1 am, at a room temperature of 23 ± 5 °C, after being assured that each subject abstained from food and drinks for at least 2 h, did not perform strenuous exercise, and emptying the bladder. The dose of deuterium was administered just after anthropometric and BIA measurements. Thus, the hydration status of a subject was likely to have remained the same throughout the measurement period.
Anthropometric measurements
Measurements were made using standard procedures [13]. Children were weighed without clothes to the nearest 0.01 kg using an electronic scale (Seca 882, Hamburg, Germany). Height was measured to the nearest millimeter using a portable gauge (Seca 225). Body mass index (BMI) (kilograms per meter squared) was calculated as weight (kilograms) per height (meters) square. Mid-upper arm, waist, and hip circumferences were measured to the nearest 0.1 cm using a non-elastic metric measuring tape (Seca 201).
Anthropometric indices (weight-for-height Z-score (WHZ), weight-for-age Z-score (WAZ), and height-for-age Z-score (HAZ)) were based on the WHO’s 2006 Child Growth Standards [14], calculated by using Anthro version 3.2.2 [15].
Bioelectrical impedance analysis
BIA was performed by a trained staff, using a multi-frequency impedance analyzer (Bodystat QuadScan 4000 with disposable long electrodes, Douglas, Isle of Man, UK) with a tetrapolar placement. Electrodes were placed on the right side of the subject on the hand, wrist, foot, and ankle according to the standard placement stated in the manufacturer’s guidelines. Measurements were performed with the subject in supine on a non-conductive surface with their arms and thighs apart, after being assured that the subject did not carry metal objects and that he was in the supine position for at least 15 min. The Bodystat QuadScan 4000 device was calibrated at the beginning of each day using the calibration unit provided by the manufacturer. The values used in the calculations were the mean of duplicate measurements. Only the impedance (Z) or resistance (R) data at 5, 50, and 100 were used in the calculations of this study. The impedance index was calculated as height2/Z (cm2/ohms) or height2/R, depending on the explanatory variable used in the equation tested. Height2/Z 5 is assumed to reflect the extracellular water (ECW) and height2/Z 100 the TBW; their ratio was used as a simple index of the ECW/TBW ratio [16].
Reference method: deuterium oxide dilution
A dose (0.5 g per kg of body weight) of deuterium oxide (99.8% purity; Cambridge Isotope Laboratories, Inc., Andover, MA, USA) was orally administrated to each child and saliva samples (2 mL) were collected before (natural deuterium abundance) and after administering the dose at 3 and 4 h respectively. Saliva collection was carried out after having been assured that the child did not eat or drink in the previous 30 min. Small pieces of cotton wool were used to collect saliva samples, after which saliva was released into sterile tubes by compressing the pieces in a syringe. Samples were stored on ice during transport on the days of fieldwork, brought to the laboratory, and stored at −20 °C until analysis.
The enrichment of deuterium in saliva samples was measured in the range of 2300–2900 cm−1 using a Fourier transformed infrared spectrophotometer (IRAffinity-1, Shimadzu, Kyoto, Japan) with a calcium fluoride cell with a thickness of 10−4 m, and a software (Isotope) developed by the Medical Research Council (Human Nutrition Research, Cambridge, UK).
Total body water calculations
From deuterium oxide dilution
TBW (kilograms) was calculated from deuterium enrichment, assuming that dilution space of deuterium (V D) or volume of distribution (V D) of a dose of deuterium oxide (2H2O) is 4.1% higher than TBW due to exchange of hydrogen with non-aqueous hydrogen in the body [17].
where
From anthropometry
The following five anthropometry-based prediction equations were used to estimate the TBW of Cameroonian children:
-
I
Friis-Hansen [18]:
TBW = k × weight0.790 × height0.425, where k is 0.195 for subjects aged 2 years to 7 years.
-
II
Morgenstern et al. [19]:
Boys from 3 months to 13 years: TBW = 0.0846 × (weight × height) 0.65
Girls from 3 months to 13 years: TBW = 0.08037 × (weight × height) 0.65
-
III
Mellits and Cheek [20]:
Boys ≤132.7 cm: TBW = −1.927 + 0.465 × weight + 0.045 × height
Boys ≥132.7 cm: TBW = −21.993 + 0.406 × weight + 0.209 × height
Girls ≤110.8 cm: TBW = 0.076 + 0.507 × weight + 0.013 × height
Girls ≥110.8 cm: TBW = −10.313 + 0.252 × weight + 0.154 × height
-
IV
Wickramasinghe et al. [21]:
TBW = 0.13 × height + 0.27 × weight + 1.82 × sex − 10.35; boy = 1 and girl = 0
-
V
Morgenstern et al. [22]:
Boys: TBW = 0.10 × (height × weight) 0.68 − 0.37 × weight
Girls: TBW = 0.14 (height × weight) 0.64 − 0.35 × weight
From BIA
Table 1 displays the seven impedance-based prediction equations used to estimate the TBW of Cameroonian children.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics 21. The Shapiro-Wilk test was used to test normality of data distribution. Results were expressed as mean ± standard deviation. Type I error risk was set at 0.05 for all analyses. Comparisons between dependent variables were determined using analysis of variance and Tukey’s B test was used for post-hoc comparisons of means when appropriate. Pearson’s correlations were used to study the relationship between the measured and predicted (obtained by BIA and anthropometric prediction equation) values. The difference between the measured and predicted values (bias) was tested against 0 (paired Student’s t test). Pure error was calculated using the following equation [13]:
where y is the measured value, y’ is the predicted value, and n is the number of subjects in the sample.
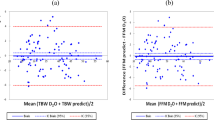
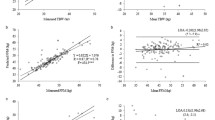
The test of Bland and Altman [23] was used to determine bias and limits of agreement between values predicted by equations and those measured by deuterium dilution. Limits of agreement were defined as upper and lower 95% confidence intervals and were determined by the mean differences ±1.96 × standard deviation [24].
In order to propose a new equation, the database was split in two subsamples and children were randomly allocated assigned to the equation development set (51 subjects) or the equation validation set (51 subjects). In the equation development set, multiple linear regression analysis was used to develop equations for predicting TBW as measured by deuterium, from anthropometric parameters such as sex, age, weight, height, and BMI or from BIA parameters. The resulted prediction equations were cross-validated by its application to the equation validation set and by using the Bland and Altman procedure to assess the agreement between the predicted and measured values.
Results
Table 2 displays the descriptive characteristics of the study population. Forty-six percent of the children included in the study were males and 54% were females. The mean age was 50.4 months, the mean weight was 16.7 kg, and the mean height was 107 cm. The children’s mean Z-scores (WHZ, HAZ, and WAZ) were within the normal range, suggesting that they had a good growth and nutritional status. However, 3.9% of the children were classified as wasted (WHZ < −2), 2.0% as stunted (HAZ < −2), 2.0% as underweight (WAZ < −2), and 3.9% as overweight (WAZ > 2). The analysis of variance showed that TBW of subjects was significantly affected (P < 0.05) by the methods used for its determination (Table 3). Most prediction equations (I, II, III, IV, V, D, F, G, and H) showed significant difference with the isotope dilution while some others such as A, B, C, and E showed non-significant differences according to Turkey’s B test, but this test does not indicate agreement between methods.
Comparisons between values of TBW measured by isotope dilution and predicted by each of the anthropometric and BIA equations are presented in Table 4. Significant correlations (P < 0.001) were noted between all predicted values of TBW and values measured by isotope dilution. However, correlation measures the strength of a relation between two variables not the agreement between them. Paired comparisons with the equations A, C, and E showed non-significant biases, while significant (P < 0.05) biases were noted with the other prediction equations. Equations IV, D, F, and G respectively underestimated TBW by 0.6, 1.1, 0.5, and 0.7 kg, while equations I, II, III, V, B, and H overestimated TBW by 3.7, 1.2, 0.9, 1.1, 0.6, and 0.9 kg. The Bland-Altman approach [23, 24] was used to better assess the agreement of each prediction equation with the deuterium dilution technique. In all cases, large 95% limits of agreement with large confidence interval (CI) were noted, demonstrating a lack of agreement between the anthropometry- and BIA-based prediction equations tested and the isotope dilution, with unacceptable discrepancies at individual level. This is illustrated in Fig. 1 with prediction equations that gave non-significant biases according to paired Student’s t test and where residuals of some children exceeded the 95% confidence limits of TBW. Despite the fact that there is no absolute criterion value for pure error that marks successful validation, most prediction equations gave pure error values that were within the limit recommended by Houtkouper et al. [25], except the equations I and A.
The relationship between the bias and sex, and some anthropometric parameters (age, height, weight, BMI, and MUAC), impedance index, and hydration (ECW/TBW ratio) characteristics of children were tested to determine any systematic error related to these characteristics (Table 5). Significant negative and positive correlation of the bias with sex were found for anthropometry-based equations IV and V, respectively indicating gradual underestimation and overestimation of TBW by these equations when the child is a boy or a girl. No significant correlation was found between bias and age suggesting no effect of TBW by increasing age. Significant negative and positive correlations of the bias with height were respectively found for equations I and A, respectively indicating gradual underestimation and overestimation of TBW by these equations in children with increase in height. Weight and bias were positively correlated for equation A only, indicating gradual overestimation of TBW by this equation with increase of weight. BMI and bias were negatively correlated for three equations (I, III, and E) indicating gradual underestimation of TBW by these equations with increase of fatness. Mid-upper arm circumference (MUAC) and bias were negatively and positively correlated respectively for equations of I and A, indicating gradual underestimation and overestimation of TBW by these equations respectively with increase of MUAC.
Impedance index and bias were positively correlated for equation A, indicating a gradual overestimation of TBW by this equation with increase impedance index in children. Furthermore, this index and bias were negatively correlated for four BIA equations (B, C, D, and G) indicating a gradual underestimation of TBW by these equations with increase impedance index in children. No significant correlation was found between bias and ECW/TBW ratio suggesting no effect of TBW by extracellular fluid.
Prediction equations for TBW were developed in the equation development set with sex, age, weight, height, BMI, and MUAC as possible predictor variables for anthropometry-based equation (Table 6) and sex, age, weight, height, and height2/Z as possible variable for BIA-based equation (Table 7). The following equations which presented the highest adjusted R 2, the lowest root mean square error (RMSE) value, and the lowest P value were selected:
The new equations were applied in the equation validation set. Good agreement was obtained with the isotope dilution with a pure error value within the ideal limit recommended by Houtkooper et al. [25] (Table 8). The Bland-Altman plots illustrated a good level of concordance between the TBW predicted by the new equations and TBW measured by isotope dilution (Fig. 2).
Discussion
A lack of agreement was noted in the present study between the isotope dilution and all the anthropometry- and BIA-based equations tested, with unacceptable discrepancies at individual level for clinical purposes, as residuals of some children exceeded the 95% confidence limits of TBW. This result agree with previous studies showing that anthropometry and BIA prediction equations used for TBW and body composition have the tendency to be population-specific and that inappropriate used of published prediction equations can lead to systematic errors and inaccurate estimations [26, 27]. In this regard, Tzamaloukas et al. [28] showed that each anthropometric measurement included in anthropometric equations for the prediction of body composition estimate a unique body composition which is for the average subject of the population in whom the equations were developed, while Haroun et al. [29] showed for the BIA model that variation of the relative body geometry between ethnic groups confound the relative distribution between weight and impedance among limb and trunk. However, apart from biological variations, errors in the measurements could also contribute to the bias between measured and predicted TBW by BIA. Despite the standardized approach used for BIA measurement, an improper control of some factors including hydration status, body position, skin temperature, electrode placement, previous exercise, and dietary intake may affect BIA measurement and prediction of TBW in children [30, 31].
To the best of our knowledge, there is no prediction equation for Cameroonian or African children that was developed or cross-validated to estimate body composition or TBW. In this study, one anthropometry and one BIA prediction equations for the estimation of TBW in Cameroonian children aged 24–60 months were developed. An adjusted R 2 of 0.71 and RMSE of 3.6 were obtained for the anthropometry-based prediction equation while adjusted R 2 of 0.68 and RMSE of 1.4 were obtained for the BIA-based prediction equation. This result agreed with previous studies displaying the method criterion (R 2 = 0.65–0.99, RMSE = 0.41–3.81) for TBW equations [32, 33]. Moreover, our prediction equations showed ideal prediction accuracy according to Houtkooper et al.’s [25] classification system for prediction errors.
In this study, the BIA equation included the impedance index, body weight, height, and age. This result was consistent with previous studies showing that the prediction of TBW from impedance index could be improved by the inclusion of anthropometric data such as body weight, age, and sex, which could correct differences across groups [34, 35]. The equation based on anthropometric measurements included body weight, BMI, MUAC, age, and sex. The precision of this model was comparable to that of the impedance equation. The cross-validation procedures revealed that the predicted values of TBW compared with measured values are accurate at a group level. The precision assessed with the pure error and the limits of agreement assessed by Bland-Altman approach facilitates generalization from the sample to the population. Both BIA and anthropometric new prediction equations had precise estimates of TBW, and therefore could be used to assess TBW in Cameroonian preschool children.
Although the use of deuterium oxide dilution technique for cross-validation analysis constitute a strength in the present study, the relatively small sample size used could be a limitation as participants were not fully representative of the Cameroonian preschool children population. Therefore, findings should be construe with caution when attempting to generalize prediction equations.
Conclusions
In conclusion, the available published anthropometric and BIA equations provide unacceptable discrepancies in the estimates of TBW at individual for Cameroonian preschool children. The present study presented two new gender-dependent equations to estimate TBW in Cameroonian children aged 24–60 months.
Abbreviations
- BIA:
-
Bioelectrical impedance analysis
- BMI:
-
Body mass index
- DEXA:
-
Energy x-ray absorptiometry
- ECW:
-
Extracellular water
- FFM:
-
Fat-free mass
- FM:
-
Fat mass
- HAZ:
-
Height-for-age Z-score
- MUAC:
-
Mid-upper arm circumference
- RMSE:
-
Root mean square error
- TBW:
-
Total body water
- WAZ:
-
Weight-for-age Z-score
- WHO:
-
World Health Organization
- WHZ:
-
Weight-for-height Z-score
References
Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;131:871S–3S.
Kennedy G, Nantel G, Hetty P. Assessment of the double burden of malnutrition in six case study countries. FAO Food Nutr Pap. 2006;84:1–20.
Amuna P, Zotor FB. Epidemiological and nutrition transition in developing countries: impact on human health and development. Proc Nutr Soc. 2008;67:82–90.
Power C, Lake JK, Cole TJ. Measurement and longterm health risks of child and adolescent fatness. Int J Obes. 1997;21:507–26.
Kotani K, Nishida M, Yamashita S, Funahashi T, Fujioka S, Tokunaga K, Ishikawa K, Tarui S, Matsuzawa Y. Two decades of annual medical examinations in Japanese obese children: do obese children grow into obese adults? Int J Obes. 1997;21:912–21.
Hill GL, Jonathan E, Lecture R. Body composition research: implications for the practice of clinical nutrition. JPEN J Parenter Enteral Nutr. 1992;16:197–218.
Shephard RJ. Physical activity and reduction of health risks: how far are the benefits independent of fat loss? J Sports Med Phys Fitness. 1994;34:91–8.
Elia M. Body composition analysis: an evaluation of two component models, multicomponent models, and bedside techniques. Clin Nutr. 1992;11:114.
Lohman TG. Advances in body composition assessment. Current issues in exercise. Monograph No. 3. Champaign, Illinois: Human Kinetics Publ; 1993.
Fomon SJ, Haschke F, Ziegler EE, Nelson SE. Body composition of reference children from birth to age 10 years. Am J Clin Nutr. 1982;35:1169.
Lohman TG. Applicability of body composition techniques and constants for children. In: Pandolf KB, editor. Exercise and sports science reviews. New York: Macmillan; 1986. p. 325.
Deurenberg P. The assessment of body composition: uses and misuses. Annual report. Lausanne, Switzerland: Nestle Foundation; 1992. p. 35–72.
Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics; 1988.
World Health Organization. Child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: WHO; 2006.
World Health Organization. WHO Anthro for personal computers, version 3.2.2, 2011: software for assessing growth and development of the world’s children. http://www.who.int/childgrowth/software/en/
Deurenberg P, Tagliabue A, Schouten FJM. Multi-frequency impedance for the prediction of extracellular water and total body water. Br J Nutr. 1995;73:349–58.
Racette SB, Schoeller DA, Luke AH, Shay K, Hnilicka J, Kushner RF. Relative dilution spaces of 2H- and 18O-labeled water in humans. Am J Physiol Endocrinol Metab. 1995;267:E585–90.
Friis-Hansen BJ. Changes in body water during growth. Acta Paediatr. 1957;46 Suppl 110:1–68.
Morgenstern BZ, Mahoney DW, Warady BA. Estimating total body water in children on the basis of height and weight: a reevaluation of the formulas of Mellits and Cheek. J Am Soc Nephrol. 2002;13:1884–8.
Mellits ED, Cheek DB. The assessment of body water and fatness from infancy to adulthood. Monogr Soc Res Child Dev. 1970;35:12–26.
Wickramasinghe VP, Laabadusuriya SP, Cleghorn GJ, Davies PS. Development of height-weight based equation for assessment of body composition in Sri Lankan children. Indian J Pediatr. 2010;77:155–60.
Morgenstern ZB, Wühl E, Nair SK, Warady AB, Schaefer F. Anthropometric prediction of total body water in children who are on pediatric peritoneal dialysis. J Am Soc Nephrol. 2006;17:285–93.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346:1085–7.
Houtkooper LB, Lohman TG, Going SB, Howell WH. Why bioelectrical impedance analysis should be used for estimating adiposity. Am J Clin Nutr. 1996;64:436S–48S.
Wagner DR, Heyward VH. Measures of body composition in blacks and whites: a comparative review. Am J Clin Nutr. 2000;71:1392–402.
Medoua NG, Essa’a a VJ, Tankou CT, Ndzana AAC, Dimodi HT, Ntsama PM. Validity of anthropometry- and impedance-based equations for the prediction of total body water as measured by deuterium dilution in Cameroonian haemodialysis patients. Clin Nutr ESPEN. 2015;10:e167–73.
Tzamaloukas HA, Murata HG, Vanderjagt JD, Glew HR. Estimates of body water, fat-free mass, and body fat in patients on peritoneal dialysis by anthropometric formulas. Kidney Int. 2003;63:1605–17.
Haroun D, Taylor SJ, Viner RM, Hayward RS, Darch TS, Eaton S, et al. Validation of bioelectrical impedance analysis in adolescents across different ethnic groups. Obesity (Silver Spring). 2010;18:1252–9.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23(6):1430–53.
Brantlov S, Ward LC, Jødal L, Rittig S, Lange A. Critical factors and their impact on bioelectrical impedance analysis in children: a review. J Med Eng Technol. 2017;41(1):22–35.
Nielsen BM, Dencker M, Ward L, Linden C, Thorsson O, Karlsson MK, et al. Prediction of fat-free body mass from bioelectrical impedance among 9-to 11-year-old Swedish children. Diabetes Obes Metab. 2007;9:521–39.
Wickramasinghe VP, Lamabadusuriya SP, Cleghorn GJ, Davies PS. Assessment of body composition in Sri Lankan children: validation of a bioelectrical impedance prediction equation. Eur J Clin Nutr. 2008;62:1170–7.
Kushner RF, Schoeller DA. Estimation of total body water by bioelectrical impedance analysis. Am J Clin Nutr. 1986;44:417–24.
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI. Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr. 1985;41:810–7.
Kushner RF, Schoeller DA, Fjeld CR, Danford L. Is the impedance index (ht2/R) significant in predicting total body water? Am J Clin Nutr. 1992;56:835–9.
Davies PSW, Preece MA, Hicks CJ, Halhiday D. The prediction of total body water using bioelectrical impedance in children and adolescents. Ann Hum Biol. 1988;l5:237–40.
Fjeld CR, Freundt-Thurn J, Schoeller DA. Total body water measured by 180 dilution and bioelectrical impedance in well and malnourished children. Pediatr Res. 1990;27:98–102.
Gregory JW, Greene SA, Scrimgeour CM, Rennie MJ. Body water measurement in growth disorders: a comparison of bioelectrical impedance and skinfold techniques with isotope dilution. Arch Dis Child. 1991;66:220–2.
Davies PSW, Gregory JW. Body water measurements in growth disorders. Arch Dis Child. 1991;66:1467.
Danford LC, Schoeller DA, Kushner RF. Comparison of two bioelectrical impedance analysis models for total water measurement in children. Ann Hum Biol. 1992;19:603–7.
Acknowledgements
This work was part of Technical Cooperation project CMR/6/010 supported by the International Atomic Energy Agency. We are grateful to the children and caregivers who generously gave their time and commitment to fulfil the need for taking part in this study. We acknowledge the contributions from Baleba Mbanga, Gondam Kamini, Thomas Ndanga, and Philomene Emale who participated in the field activities.
Funding
Not applicable.
Availability of data and materials
Important data for this study are contained in the manuscript. Subjects’ individual data are not shared in this work for ethical reasons. Authors did not include data sharing clearance during ethical approval.
Author information
Authors and Affiliations
Contributions
GN M initiated the study, drafted the research protocol, coordinated and led the research implementation in the field, analyzed the data, and drafted the manuscript. VJE, HTD, and PMN helped with subjects’ enrolment, sample collection and analysis as well as preparation of the manuscript. All authors edited the manuscript and approved its final contents.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by the ethics committee of the Institute of Medical Research and Medicinal Plants Studies (IMPM). Informed written consent was obtained from each caregiver of children participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors confirm that they have no competing interest in any company or organization sponsoring the research currently and at the time the research was done.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Essa’a, V.J., Dimodi, H.T., Ntsama, P.M. et al. Validation of anthropometric and bioelectrical impedance analysis (BIA) equations to predict total body water in a group of Cameroonian preschool children using deuterium dilution method. Nutrire 42, 20 (2017). https://doi.org/10.1186/s41110-017-0045-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41110-017-0045-y