Abstract
Fibroblast growth factor 23 (FGF23) is a bone-derived hormone regulating phosphate and vitamin D metabolism. FGF23 works by binding to Klotho-FGF receptor (FGFR) complex. FGF23 reduces serum phosphate level by suppressing the expression of type 2a and 2c sodium-phosphate cotransporters in the renal proximal tubules. In addition, FGF23 suppresses intestinal phosphate absorption by reducing 1,25-dihydroxyvitamin D (1,25(OH)2D) level. FGF23 also inhibits the production and secretion of parathyroid hormone. FGF23 starts to increase in the early phase of chronic kidney disease (CKD) and is considered to prevent the development of hyperphosphatemia. With the progression of CKD, the expression of Klotho decreases causing impaired actions of FGF23. It has been reported that FGF23 level is correlated with various adverse events including cardiovascular diseases especially in patients with CKD. It was also shown that FGF23 induces left ventricular hypertrophy by directly acting on cardiomyocytes in a Klotho-independent way. However, there still remain several unanswered questions concerning FGF23-Klotho axis. We hope that further studies elucidate unsolved problems and will be useful for more appropriate management of patients with CKD.
Similar content being viewed by others
Background
Kidney is essential for maintaining mineral metabolism. Thus, deranged mineral metabolism and abnormal serum concentrations of minerals including calcium (Ca) and phosphate can be observed in patients with chronic kidney disease (CKD). CKD-mineral and bone disorder (CKD-MBD) was defined as a systemic disease including abnormal mineral and bone metabolism, ectopic calcification [1]. CKD-MBD is at least one of conditions that affect morbidity and mortality of patients with CKD [2]. Therefore, it has been a big challenge to understand the pathophysiology of CKD-MBD and to develop effective drugs for this disorder. Serum Ca level is mainly regulated by two calciotropic hormones, parathyroid hormone (PTH) and 1,25-dihydroxyvitamin D (1,25(OH)2D). While these hormones can also affect serum phosphate level, the investigations of hypophosphatemic diseases revealed that there are other humoral factors regulating phosphate metabolism than these calciotropic hormones [3]. Fibroblast growth factor 23 (FGF23) was identified as a humoral phosphaturic factor responsible for autosomal dominant hypophosphatemic rickets (ADHR) and tumor-induced osteomalacia (TIO) [4, 5]. Since then, it was shown that excessive actions of FGF23 cause several kinds of hypophosphatemic diseases [6]. In addition, deficient actions of FGF23 result in a hyperphosphatemic disease [7], and FGF23 is now considered to be a hormone regulating phosphate metabolism [8, 9]. FGF23 is produced mainly by the bone [10, 11] and binds to Klotho-FGF receptor (FGFR) complex [12, 13]. Serum FGF23 level is high in patients of CKD, suggesting that FGF23 has some role in the development of CKD-MBD [14]. Here, we briefly summarize the significance of FGF23 in patients with CKD and discuss some controversies concerning FGF23 especially in patients with end-stage renal disease (ESRD).
The structure and function of FGF23
FGF23 is produced by the bone, especially by osteocytes [10, 11]. FGF23 protein is produced as a peptide with 251 amino acids. After the cleavage of a signal peptide with 24 amino acids, FGF23 protein with 227 amino acids is secreted [4, 5]. A part of FGF23 protein is proteolytically cleaved between Arg179 and Ser180 into inactive N-terminal and C-terminal fragments before or during the process of secretion [5] (Fig. 1). FGF23 has a FGF homology region as other members of FGF family in the N-terminal portion of this processing site [15]. Therefore, only full-length FGF23 with 227 amino acids is considered to have a hormonal activity. It is suggested that FGF23 activity is regulated not only by its production but also by post-translational modification of FGF23 protein. It was previously shown that O-glycosylation of Thr178 in FGF23 protein by polypeptide N-acetylgalactosaminyltransferase 3 (GalNac-T3), a gene product of polypeptide N-acetylgalactosaminyltransferase 3 (GALNT3), inhibits this cleavage and works to increase full-length FGF23 [16] (Fig. 1). On the other hand, phosphorylation of Ser180 in FGF23 protein by family with sequence similarity 20, member C (FAM20C) inhibits O-glycosylation by GALNT3 and enhances the processing of FGF23 protein [17] (Fig. 1).
The structure and post-translational modification of FGF23 protein. FGF23 protein is produced as a peptide with 251 amino acids. FGF23 with 227 amino acids is secreted after the cleavage of a signal peptide with 24 amino acids. A part of FGF23 protein is cleaved between Arg179 and Ser180 into inactive N-terminal and C-terminal fragments before or during the process of secretion. O-glycosylation of Thr178 by GalNac-T3, a gene product of GALNT3, inhibits this cleavage and increases full-length FGF23. Phosphorylation of Ser180 inhibits O-glycosylation by GALNT3 and enhances the processing of FGF23 protein. GalNac-T3: polypeptide N-acetylgalactosaminyltransferase 3; GALNT3: polypeptide N-acetylgalactosaminyltransferase 3
FGF23 reduces serum phosphate level by suppressing the expression of type 2a and 2c sodium-phosphate cotransporters in the renal proximal tubules [8] (Fig. 2). In addition, FGF23 reduces 1,25(OH)2D level not only by suppressing CYP27B1 expression which produces 25-hydroxyvitamin D-1α-hydroxylase but also by enhancing that of CYP24A1 encoding 25-hydroxyvitamin D-24-hydroxylase [8] (Fig. 2). Because 1,25(OH)2D is a hormone that enhances intestinal phosphate absorption, FGF23 reduces serum phosphate by inhibiting both intestinal phosphate absorption via reducing 1,25(OH)2D level and proximal tubular phosphate reabsorption. FGF23 was also shown to suppress both production and secretion of PTH in rodents [18]. Furthermore, it was recently reported that FGF23 regulates renal calcium and sodium handling by modifying the expression of the calcium channel, transient receptor potential vanilloid-5 (TRPV5), and sodium-chloride cotransporter (NCC) in renal distal tubules [19, 20] while FGF23 did not change urinary calcium and sodium excretion in a previous study [5]. These results indicated that FGF23 produced by the bone works as a systemic humoral factor and suggested that there is a specific receptor for FGF23 at least in the kidney and parathyroid glands.
The activities of FGF23 in the kidney. FGF23 reduces serum phosphate level by suppressing the expression of type 2a and 2c sodium-phosphate cotransporters in the renal proximal tubules. In addition, FGF23 decreases intestinal phosphate absorption by reducing 1,25(OH)2D level via not only suppressing CYP27B1 which produces 25-hydroxyvitamin D-1α-hydroxylase but also enhancing CYP24A1 expression encoding 25-hydroxyvitamin D-24-hydroxylase
FGF family members have been shown to bind to FGFRs [15]. While the affinity of FGF23 for FGFRs is quite low, FGF23 was shown to bind to Klotho-FGFR complex [12, 13]. Klotho was identified as a gene whose expression was severely reduced in genetically engineered mice called Klotho [21]. Both FGF23 knockout and Klotho mice were shown to have hyperphosphatemia with increased renal proximal tubular phosphate reabsorption and high 1,25(OH)2D level [9, 12, 13, 22], indicating that FGF23-Klotho pathway is essential for maintaining phosphate and vitamin D metabolism. However, there still remain several unsolved questions concerning the mechanisms of actions of FGF23. First, Klotho is mainly expressed in the renal distal tubules, parathyroid glands, and choroid plexus [21]. The initial signal after the administration of FGF23 was detected in the distal tubules [23]. On the other hand, the actions of FGF23 are observed in the proximal tubules. It is possible that there is an unknown communication pathway between the renal distal tubules and proximal tubules. In addition, while it was reported that Klotho is also expressed in the renal proximal tubules [24], the direct evidence that proximal tubular Klotho mediates in vivo actions of FGF23 is lacking. Second, it is not clear how FGF23 can regulate the expression of several genes including CYP24A1 and CYP27B1 and those encoding sodium-phosphate cotransporters after binding to Klotho-FGFR complex. A recent study indicated that FGF23 uses different signal transduction pathways for phosphate handling and vitamin D metabolism [25]. However, it is still unclear what molecules finally mediate FGF23 actions and regulate gene expression in the target cells.
FGF23 and abnormal mineral metabolism in patients with CKD
CKD and CKD-MBD are becoming big social problems all over the world. CKD-MBD is manifested by abnormalities in bone and mineral metabolism or extra skeletal calcification [1]. It was revealed that serum FGF23 level starts to increase early in the progression of CKD before the increase of serum phosphate or PTH level [26]. This increase of FGF23 was shown to be associated with enhanced urinary phosphate excretion [27]. In addition, the administration of neutralizing anti-FGF23 antibodies increased serum phosphate in an animal model of early CKD [28]. Therefore, the increase of FGF23 in patients with early CKD seems to work to prevent the development of hyperphosphatemia at least in part by enhancing urinary phosphate excretion [28]. On the other hand, the increase of FGF23 was also associated with the decrease of 1,25(OH)2D in patients with CKD [27]. Furthermore, the inhibition of FGF23 activity in the animal model of CKD increased serum 1,25(OH)2D [28]. While the reduction of 1,25(OH)2D by increased FGF23 is likely to reduce intestinal phosphate absorption and contribute to maintaining serum phosphate level, it may induce or aggravate secondary hyperparathyroidism. However, the role of FGF23 in the development of secondary hyperparathyroidism is complex because FGF23 was shown to directly inhibit production and secretion of PTH [18]. With the progression of CKD, the expression of Klotho in kidneys and parathyroid glands were shown to decrease that likely leads to impaired actions of FGF23 [29, 30]. Together with reduced nephron mass, frank hyperphosphatemia develops in patients with advanced CKD.
While FGF23 begins to elevate in patients with early CKD, it is not evident what triggers this increase of FGF23. Serum phosphate and PTH are normal when FGF23 starts to increase although phosphate and PTH were shown to affect FGF23 level [31, 32]. While 1,25(OH)2D was shown to increase FGF23 level [33], 1,25(OH)2D is not high in patients with early CKD. It is proposed that the reduced Klotho in patients with CKD has some role in the increase of FGF23 [34]. Still, it is not clear how reduced Klotho expression in kidneys or parathyroid glands affect FGF23 production in osteocytes without changing phosphate or PTH levels. It was also reported that the impairment of renal function affects the processing of FGF23 protein [35]. The ratio of C-terminal fragment of FGF23 to total FGF23 protein was lower in patients with CKD compared to that of healthy control. However, the mechanism of this reduced processing of FGF23 protein is not clear, either.
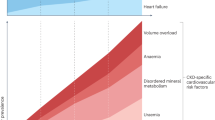
FGF23 and cardiovascular diseases in patients with CKD
It has been well known that hyperphosphatemia is a risk factor for ectopic calcification, cardiovascular diseases, and high mortality [36]. Wolf et al. reported that serum FGF23 level at the time of starting hemodialysis positively correlated with mortality in a subsequent year [37]. The most important finding of this report was that the relationship between FGF23 level and mortality remained to be significant even after adjusting by serum phosphate level or other confounding factors. Since then, many epidemiological studies investigated the relationship between FGF23 and various adverse events especially in patients with CKD. High serum FGF23 level was shown to be associated with left ventricular hypertrophy (LVH), heart failure, atherosclerosis, stroke, and various cardiovascular events [38]. However, these associations are not evident in all the reported studies. Some reports did not find such associations [38]. In addition, other reports indicated the association between FGF23 and adverse events in a general population whose FGF23 level is not so high [38].
The association between FGF23 level and various adverse events does not necessarily indicate the direct cause-effect relationship. However, Faul et al. reported that FGF23 directly acted on cardiomyocytes and induced LVH independent of Klotho [39, 40]. Therefore, it was postulated that FGF23 causes cardiovascular diseases by directly acting on the heart. However, there remain several questions concerning the relationship between FGF23 level and various adverse events. First, FGF23 was shown to activate FGFR4 independent of Klotho [40]. Because the affinity of FGF23 for FGF receptors is low [12], it is not clear how FGF23 can activate FGFR4 in cardiomyocytes without Klotho. Second, if FGF23 affects cardiomyocytes directly and induces LVH, LVH could be prevented by blocking FGF23 actions. However, the blockade of FGF23 effects by anti-FGF23 antibody did not reduce the expression of hypertrophic marker genes in an animal model of CKD [41]. Third, FGF23 level was also reported to be associated with various parameters other than cardiovascular diseases such as fractures, progression of CKD, insulin resistance, high C-reactive protein, and abnormal lipid profile [38, 42]. However, it is not known whether FGF23 affects these parameters by directly acting on several tissues like the bone, kidney, fat, and muscle. Fourth, it is not clear either whether the association between FGF23 and cardiovascular events in general population is explained by direct effects of FGF23 on the heart. Recent studies suggest that inflammation or oxidative stress can increase FGF23 level [43–46]. Thus, it is necessary to clarify the regulatory mechanisms and the determinants of FGF23 levels to further elucidate the role of FGF23 especially in patients with CKD.
Conclusions
The identification of FGF23 and the subsequent investigations established that FGF23-Klotho axis plays essential roles in the regulation of phosphate and vitamin D metabolism. However, there still remain many important questions concerning this pathway. Especially, the detailed regulatory mechanisms of FGF23 production and activities need to be clarified. Therefore, it has not yet been established whether the suppression of FGF23 activities is beneficial for patients with CKD. We hope that further studies elucidate unsolved problems concerning FGF23-Klotho axis and will be useful for more appropriate management of patients with CKD.
Abbreviations
- 1,25(OH)2D:
-
1,25-dihydroxyvitamin D
- ADHR:
-
autosomal dominant hypophosphatemic rickets
- CKD:
-
chronic kidney disease
- CKD-MBD:
-
chronic kidney disease-mineral and bone disorder
- ESRD:
-
end-stage renal disease
- FAM20C:
-
family with sequence similarity 20, member C
- FGF23:
-
fibroblast growth factor 23
- FGFR:
-
fibroblast growth factor receptor
- GalNac-T3:
-
polypeptide N-acetylgalactosaminyltransferase 3
- GALNT3 :
-
polypeptide N-acetylgalactosaminyltransferase 3
- LVH:
-
left ventricular hypertrophy
- NCC:
-
sodium-chloride cotransporter
- PTH:
-
parathyroid hormone
- TIO:
-
tumor-induced osteomalacia
- TRPV5:
-
transient receptor potential vanilloid-5
References
Moe S, Drueke T, Cunningham J, Goodman W, Martin K, Olgaard K, et al. Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2006;69:1945–53.
Moe SM, Drueke T. Improving global outcomes in mineral and bone disorders. Clin J Am Soc Nephrol. 2008;3:S127–30.
Meyer Jr RA, Tenenhouse HS, Meyer MH, Klugerman AH. The renal phosphate transport defect in normal mice parabiosed to X-linked hypophosphatemic mice persists after parathyroidectomy. J Bone Miner Res. 1989;4:523–32.
ADHR Consortium. Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat Genet. 2000;26:345–8.
Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, et al. Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Natl Acad Sci U S A. 2001;98:6500–5.
Hori M, Shimizu Y, Fukumoto S. Minireview: fibroblast growth factor 23 in phosphate homeostasis and bone metabolism. Endocrinology. 2011;152:4–10.
Fukumoto S, Yamashita T. FGF23 is a hormone-regulating phosphate metabolism—unique biological characteristics of FGF23. Bone. 2007;40:1190–5.
Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, et al. FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res. 2004;19:429–35.
Shimada T, Kakitani M, Yamazaki Y, Hasegawa H, Takeuchi Y, Fujita T, et al. Targeted ablation of Fgf23 demonstrates an essential physiological role of FGF23 in phosphate and vitamin D metabolism. J Clin Invest. 2004;113:561–8.
Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, et al. Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet. 2006;38:1310–5.
Liu S, Zhou J, Tang W, Jiang X, Rowe DW, Quarles LD. Pathogenic role of Fgf23 in Hyp mice. Am J Physiol Endocrinol Metab. 2006;291:E38–49.
Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblatt KP, et al. Regulation of fibroblast growth factor-23 signaling by klotho. J Biol Chem. 2006;281:6120–3.
Urakawa I, Yamazaki Y, Shimada T, Iijima K, Hasegawa H, Okawa K, et al. Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature. 2006;444:770–4.
Weber TJ, Liu S, Indridason OS, Quarles LD. Serum FGF23 levels in normal and disordered phosphorus homeostasis. J Bone Miner Res. 2003;18:1227–34.
Itoh N, Ornitz DM. Evolution of the Fgf and Fgfr gene families. Trends Genet. 2004;20:563–9.
Frishberg Y, Ito N, Rinat C, Yamazaki Y, Feinstein S, Urakawa I, et al. Hyperostosis-hyperphosphatemia syndrome: a congenital disorder of O-glycosylation associated with augmented processing of fibroblast growth factor 23. J Bone Miner Res. 2007;22:235–42.
Tagliabracci VS, Engel JL, Wiley SE, Xiao J, Gonzalez DJ, Nidumanda Appaiah H, et al. Dynamic regulation of FGF23 by Fam20C phosphorylation, GalNAc-T3 glycosylation, and furin proteolysis. Proc Natl Acad Sci U S A. 2014;111:5520–5.
Ben-Dov IZ, Galitzer H, Lavi-Moshayoff V, Goetz R, Kuro-o M, Mohammadi M, et al. The parathyroid is a target organ for FGF23 in rats. J Clin Invest. 2007;117:4003–8.
Andrukhova O, Smorodchenko A, Egerbacher M, Streicher C, Zeitz U, Goetz R, et al. FGF23 promotes renal calcium reabsorption through the TRPV5 channel. Embo J. 2014;33:229–46.
Andrukhova O, Slavic S, Smorodchenko A, Zeitz U, Shalhoub V, Lanske B, et al. FGF23 regulates renal sodium handling and blood pressure. EMBO Mol Med. 2014;6:744–59.
Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390:45–51.
Sitara D, Razzaque MS, Hesse M, Yoganathan S, Taguchi T, Erben RG, et al. Homozygous ablation of fibroblast growth factor-23 results in hyperphosphatemia and impaired skeletogenesis, and reverses hypophosphatemia in Phex-deficient mice. Matrix Biol. 2004;23:421–32.
Farrow EG, Davis SI, Summers LJ, White KE. Initial FGF23-mediated signaling occurs in the distal convoluted tubule. J Am Soc Nephrol. 2009;20:955–60.
Andrukhova O, Zeitz U, Goetz R, Mohammadi M, Lanske B, Erben RG. FGF23 acts directly on renal proximal tubules to induce phosphaturia through activation of the ERK1/2-SGK1 signaling pathway. Bone. 2012;51:621–8.
Portale AA, Zhang MY, David V, Martin A, Jiao Y, Gu W, et al. Characterization of FGF23-dependent egr-1 cistrome in the mouse renal proximal tubule. PLoS One. 2015;10:e0142924.
Isakova T, Wahl P, Vargas GS, Gutierrez OM, Scialla J, Xie H, et al. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 2011;79:1370–8.
Gutierrez O, Isakova T, Rhee E, Shah A, Holmes J, Collerone G, et al. Fibroblast growth factor-23 mitigates hyperphosphatemia but accentuates calcitriol deficiency in chronic kidney disease. J Am Soc Nephrol. 2005;16:2205–15.
Hasegawa H, Nagano N, Urakawa I, Yamazaki Y, Iijima K, Fujita T, et al. Direct evidence for a causative role of FGF23 in the abnormal renal phosphate handling and vitamin D metabolism in rats with early-stage chronic kidney disease. Kidney Int. 2010;78:975–80.
Koh N, Fujimori T, Nishiguchi S, Tamori A, Shiomi S, Nakatani T, et al. Severely reduced production of klotho in human chronic renal failure kidney. Biochem Biophys Res Commun. 2001;280:1015–20.
Komaba H, Goto S, Fujii H, Hamada Y, Kobayashi A, Shibuya K, et al. Depressed expression of Klotho and FGF receptor 1 in hyperplastic parathyroid glands from uremic patients. Kidney Int. 2010;77:232–8.
Ferrari SL, Bonjour JP, Rizzoli R. Fibroblast growth factor-23 relationship to dietary phosphate and renal phosphate handling in healthy young men. J Clin Endocrinol Metab. 2005;90:1519–24.
Rhee Y, Bivi N, Farrow E, Lezcano V, Plotkin LI, White KE, et al. Parathyroid hormone receptor signaling in osteocytes increases the expression of fibroblast growth factor-23 in vitro and in vivo. Bone. 2011;49:636–43.
Saito H, Maeda A, Ohtomo S, Hirata M, Kusano K, Kato S, et al. Circulating FGF-23 is regulated by 1alpha,25-dihydroxyvitamin D3 and phosphorus in vivo. J Biol Chem. 2005;280:2543–9.
Olauson H, Vervloet MG, Cozzolino M, Massy ZA, Urena Torres P, Larsson TE. New insights into the FGF23-Klotho axis. Semin Nephrol. 2014;34:586–97.
Smith ER, Cai MM, McMahon LP, Holt SG. Biological variability of plasma intact and C-terminal FGF23 measurements. J Clin Endocrinol Metab. 2012;97:3357–65.
Stevens KK, Patel RK, Mark PB, Delles C, Jardine AG. Phosphate as a cardiovascular risk factor: effects on vascular and endothelial function. Lancet. 2015;385:S10.
Gutierrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med. 2008;359:584–92.
Fukumoto S, Shimizu Y. Fibroblast growth factor 23 as a phosphotropic hormone and beyond. J Bone Miner Metab. 2011;29:507–14.
Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, et al. FGF23 induces left ventricular hypertrophy. J Clin Invest. 2011;121:4393–408.
Grabner A, Amaral AP, Schramm K, Singh S, Sloan A, Yanucil C, et al. Activation of cardiac fibroblast growth factor receptor 4 causes left ventricular hypertrophy. Cell Metab. 2015;22:1020–32.
Shalhoub V, Shatzen EM, Ward SC, Davis J, Stevens J, Bi V, et al. FGF23 neutralization improves chronic kidney disease-associated hyperparathyroidism yet increases mortality. J Clin Invest. 2012;122:2543–53.
Domingo P, Lamarca MK, Gallego-Escuredo JM, Torres F, Domingo JC, Villarroya J, et al. Circulating fibroblast growth factor 23 (FGF23) levels are associated with metabolic disturbances and fat distribution but not cardiovascular risk in HIV-infected patients. J Antimicrob Chemother. 2015;70:1825–32.
Hanks LJ, Casazza K, Judd SE, Jenny NS, Gutierrez OM. Associations of fibroblast growth factor-23 with markers of inflammation, insulin resistance and obesity in adults. PLoS One. 2015;10:e0122885.
Holecki M, Chudek J, Owczarek A, Olszanecka-Glinianowicz M, Bozentowicz-Wikarek M, Dulawa J, et al. Inflammation but not obesity or insulin resistance is associated with increased plasma fibroblast growth factor 23 concentration in the elderly. Clin Endocrinol (Oxf). 2015;82:900–9.
Hori M, Kinoshita Y, Taguchi M, and Fukumoto S. Phosphate enhances Fgf23 expression through reactive oxygen species in UMR-106 cells. J Bone Miner Metab. in press.
Ito N, Wijenayaka AR, Prideaux M, Kogawa M, Ormsby RT, Evdokiou A, et al. Regulation of FGF23 expression in IDG-SW3 osteocytes and human bone by pro-inflammatory stimuli. Mol Cell Endocrinol. 2015;399:208–18.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Our department is supported by Chugai Pharmaceutical Co. Ltd.
Authors’ contributions
YT made the original form of this review article and SF supervised this work. Both authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Takashi, Y., Fukumoto, S. FGF23-Klotho axis in CKD. Ren Replace Ther 2, 20 (2016). https://doi.org/10.1186/s41100-016-0032-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-016-0032-4