Abstract
Heart failure (HF) remains a significant global health burden, and hypertension is known to be the primary contributor to its development. Although aggressive hypertension treatment can prevent heart changes in at-risk patients, determining the optimal blood pressure (BP) targets in cases diagnosed with HF is challenging owing to insufficient evidence. Notably, hypertension is more strongly associated with HF with preserved ejection fraction than with HF with reduced ejection fraction. Patients with acute hypertensive HF exhibit sudden symptoms of acute HF, especially those manifested with severely high BP; however, no specific vasodilator therapy has proven beneficial for this type of acute HF. Since the majority of medications used to treat HF contribute to lowering BP, and BP remains one of the most important hemodynamic markers, targeted BP management is very concerned in treatment strategies. However, no concrete guidelines exist, prompting a trend towards optimizing therapies to within tolerable ranges, rather than setting explicit BP goals. This review discusses the connection between BP and HF, explores its pathophysiology through clinical studies, and addresses its clinical significance and treatment targets.
Similar content being viewed by others
Background
Heart failure (HF) remains a major public health burden, with a rapidly increasing global prevalence. In the United States, more than 5 million people aged ≥20 years are affected by HF [1], and this number is expected to increase by 46%, resulting in an estimated 8 million Americans with HF in 2030 [2]. Hypertension is one of the most frequent comorbidities [3], playing a pivotal role in the development of HF [4]. In the Framingham Heart Study, hypertension progressed to HF in 91% of patients > 20 years of age, with a doubling and tripling of the risk of HF in male and female hypertensive patients, respectively [5, 6]. Chronic hypertension causes functional and structural changes in the heart, culminating in HF and further increasing the rate of mortality and morbidity [7]. Intensive treatment of hypertension can prevent and reverse myocardial changes in patients at risk of HF; however, defining optimal blood pressure (BP) targets for patients who have already developed HF is challenging owing to a lack of evidence.
Currently, HF is classified depending on the left ventricular ejection fraction (LVEF), with LVEF ≤40% defined as HF with reduced ejection fraction (HFrEF) and LVEF ≥50% as HF with preserved ejection fraction (HFpEF) [8]. In addition, if the LVEF is between 41 and 49%, the definition of HF with mildly reduced ejection fraction (HFmrEF) is commonly used in a dynamic trajectory to denote improvement from or deterioration to HFrEF [9]. HFmrEF occupies a spectrum between HFrEF and HFpEF, exhibiting the characteristics of both. However, this classification system is often ambiguous [10]. In the present review, rather than focusing on this detailed classification of LVEF, we focus on the classical phenotypes of HFrEF and HFpEF (implicitly including the concept of HFmrEF) and their association with BP from a more comprehensive perspective.
Development of hypertensive heart disease and HF
Traditionally, the development and progression of HF in hypertensive patients has been classified into four stages: (1) isolated left ventricular (LV) diastolic dysfunction without LV hypertrophy; (2) LV diastolic dysfunction with concentric LV hypertrophy; (3) clinical HFpEF accompanied by pulmonary edema; and (4) dilated cardiac chambers with HFrEF [6]. These stages suggest that diastolic dysfunction is an early phenomenon, and hypertension-induced LV hypertrophy leads to remodeling of the left atrium and ventricle, ultimately resulting in advanced diastolic and systolic dysfunction.
As reviewed in the article by Messerli et al. [6], hypertensive heart disease plays a pivotal role in the pathophysiology of HF through a sequential and intricate process. Initially, the LV responds to elevated BP by adapting to the hemodynamic wall stress, which results in pressure overload. This adaptation involves the thickening of the LV wall and an increase in LV mass, resulting in concentric LV hypertrophy. During this phase, the initial manifestation of cardiac dysfunction is LV diastolic dysfunction. With a persistent pressure overload, diastolic dysfunction progresses, ultimately leading to the onset of HFpEF. In the advanced stages of hypertensive heart disease, typically due to prolonged exposure to pressure overload with or without concurrent myocardial ischemia, the condition evolves into a dilated LV dimension. The final stage is characterized by reduced LVEF and development of HFrEF.
However, HFrEF and HFpEF should be considered from a slightly different perspective than that presented by Messerli et al. [6]. If HFrEF and HFpEF are considered part of a unified disease spectrum, they may be expected to respond similarly to HF treatment. However, numerous medications that have demonstrated clear improvements in HFrEF have not shown comparable beneficial effects on HFpEF [11]. Angiotensin receptor blockers (ARBs) [12], angiotensin-converting enzyme inhibitors (ACEis) [13], β-blockers [14, 15], and mineralocorticoid receptor antagonists (MRAs) [16], all of which are also used as antihypertensive drugs, have failed to show clinically significant prognostic improvements in HFpEF, unlike in HFrEF. These differences were also evident in epidemiological studies. For example, a Japanese chronic HF registry-based study showed that most patients with HFpEF and nearly half of those with HFrEF remained in their respective categories throughout a 3-year follow-up period [10]. A study consisting of 3480 consecutive Japanese patients with HF showed that HFpEF transitioned to HFrEF in only 4% of them after 3 years, whereas HFrEF at registration transitioned to HFpEF and HFmrEF in 26 and 21% of patients, respectively, at 3 years, suggesting reverse remodeling after treatment [10]. These findings further support the idea that HFpEF and HFrEF are distinct syndromes with fundamental pathophysiological differences and etiologies. Similarly, in another long-term longitudinal study of ambulatory HFpEF patients, LVEF remained ≥50% in most patients with HFpEF for 11 years, and only 1.6% of patients evolved to LVEF < 50% [17]. Therefore, approaching HFrEF and HFpEF differently when examining their associations with hypertension is imperative.
Association between hypertension and HF
Hypertension is widely recognized as one of the most important risk factors of HFpEF [18]. Increased LV filling pressure and chronic myocardial remodeling due to hypertension are considered the primary mechanisms leading to the development of HFpEF [19]. Elevated systolic BP (SBP) is notably observed in patients with HFpEF, with a 3% rise in the likelihood of prevalent HFpEF for every 1 mmHg increase in SBP > 120 mmHg in an acute HF setting [20].
In terms of HFrEF, the association manifests distinctively. According to the European Society of Cardiology Heart Failure Long-Term Registry, the largest pan-European cohort of patients with real-world chronic HF in the full spectrum of LVEF, HFrEF accounts for approximately 60% of all patients in the registry [21]. This registry data showed that mean SBP tends to be lower in HFrEF than in other categories, with 121.6 ± 20.8 mmHg in HFrEF, 126.5 ± 21.1 mmHg in HFmrEF, and 130.9 ± 21.4 mmHg in HFpEF. The use of antihypertensive therapy differed notably between the HFrEF and HFpEF groups, with 56% for HFrEF and 67% for HFpEF. Regarding the underlying etiology of HF, nearly half of HFrEF cases (49%) occur due to ischemic heart disease, approximately one-third (35%) is caused by idiopathic dilated cardiomyopathy, and only 4.5% is due to hypertension itself. In contrast, HFpEF has a different etiology, with 18% of cases occurring due to hypertension, approximately a quarter due to ischemic heart disease, and 12% due to idiopathic dilated cardiomyopathy.
An analysis of the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry based on the United States population mirrors these distinctions [14]. The etiology of HF was ischemic in a higher percentage of patients with HFrEF than in those with HFpEF (54% vs. 38%, P < 0.0001), whereas the hypertensive etiology was more common in patients with HFpEF than in those with HFrEF (28% vs. 17%, P < 0.0001). Interestingly, when further stratified by LVEF, a hypertensive etiology was significantly predominant in HFpEF (LVEF, > 50%) than in HFmrEF (LVEF, 41–49%) at a rate of 31% versus 22% (P < 0.0001). In the Korean Acute Heart Failure (KorAHF) registry, which is a prospective multicenter cohort registry including more than 5600 patients with acute heart failure from 10 tertiary hospitals in the Republic of Korea, the prevalence of hypertension was 62.2%; ischemic etiology accounted for 37.6%, and idiopathic dilated cardiomyopathy comprised 15.3% of the cases [22], which is in line with the European HF registry. When divided based on LVEF, the prevalence of hypertension was higher in patients with HFpEF (64%) than in those with HFrEF (56%).
These observations suggest that while some variability may be influenced by factors such as race, region, and specific registry characteristics, a stronger association exists between high BP and HFpEF than between high BP and HFrEF in the overall population with HF.
Hypertensive AHF
Acute HF (AHF) is caused by the acute or subacute deterioration of heart function, leading to pulmonary edema and subsequent symptoms such as dyspnea or edema. Given that these symptoms are primarily caused by volume overload, treatment strategies are based on this assumption [23]. However, a closer look reveals that the aggravating factors of HF are diverse, resulting in distinct phenotypes of AHF that necessitate more specialized treatments. These phenotypes can occur as acute exacerbation of preexisting chronic HF, or as a new onset (de novo) HF. Concerning the relationship between BP and AHF, lowering the ventricular filling pressure plays a crucial role in AHF management, especially when hypertension is concurrently present [24].
AHF is a complex and multifaceted condition characterized by diverse etiologies, distinct pathophysiological mechanisms, varying risk profiles, and treatment responses [25, 26]. This heterogeneity poses significant challenges when conducting randomized controlled trials aimed at comprehensively investigating AHF. In this context, we often encounter a specific form of AHF where “high BP” is clearly the cause or is strongly suspected of contributing to the pathogenesis, which is commonly referred to as “hypertensive acute heart failure (H-AHF)”. This clinical phenomenon is characterized by a dramatic improvement in clinical signs and symptoms by BP-lowering treatment, which is also the goal of treatment. In previous studies, the H-AHF has often been defined by the following two features [23, 24, 27, 28]: (1) SBP ≥ 140 mmHg and (2) acute cardiogenic pulmonary edema, often with rapid onset.
Within the spectrum of AHF, approximately half of the patients may exhibit an SBP > 140 mmHg [29,30,31], although not all cases are categorized as H-AHF. H-AHF is particularly characterized by the sudden onset of symptoms, notably pulmonary edema, which distinguishes it from other forms of AHF [23, 28]. A more obvious characteristic of H-AHF is the presence of severely elevated BP (≥160–180 mmHg), with pulmonary edema developing in a matter of hours, and no other cause of AHF except hypertension [24, 31]. However, because of this vague definition and characterization, there is a large variation in prevalence between the registries; this phenotype is reported as 4% in the KorAHF registry [22] and approximately 11% in the European or US HF registries [21, 30, 31]. In particular, for HFrEF, hypertensive etiology is reported as 4.5% in the European registry [21] and 2.9% in the KorAHF registry [22]. This difference is thought to be due to demographic variations and ambiguity in the definition of diagnosis.
Several studies have investigated the association between symptom duration and the clinical features of patients with H-AHF. One study examined whether dyspnea occurred in ≤7 or > 7 days, and found that the latter was associated with higher in-hospital worsening of HF and 1-year cardiovascular mortality and less improvement in symptoms within 48 hours [32] . In the group with onset ≤7 days, SBP was significantly higher (138 mmHg vs. 121 mmHg) and moderate-to-severe pulmonary edema was more frequent (33% vs. 8%) compared to cases with onset > 7 days. Although these findings do not precisely delineate the threshold for a “rapid” onset indicative of H-AHF pathophysiology, they do provide knowledge regarding the phenotype. In other words, H-AHF may manifest as the most severe form of AHF with high BP; however, it also exhibits a relatively favorable prognosis [24, 32,33,34,35,36]. This is supported by studies showing that among patients with AHF presenting to the emergency department, high BP is often a predictor of low risk [27, 34,35,36].
A recent post hoc analysis demonstrated that treatment effectiveness varied with BP [37]. It has been recommended that SBP should be lowered by ≤25% in H-AHF [24, 27, 38]. Patients treated with vasodilators who achieved an SBP reduction ≤25% within 6 hours of emergency room arrival had a better diuretic response and lower 1-year mortality than those with SBP reduction > 25% [39]. In this regard, vasodilators are hypothesized to improve outcomes by mitigating end-organ damage in patients with H-AHF, potentially by influencing both preload and/or afterload [24], and they can generally be used safely in H-AHF and may provide benefits when applied to appropriate patients. Unfortunately, despite numerous randomized clinical trials in this population over the past two decades, no vasodilator has shown any mortality benefit [40]. This is due to the fact that AHF is a heterogeneous condition with diverse etiologies and pathophysiology, and stratifying and enrolling specific subgroups with predictable treatment responses is challenging. Although there is a lack of evidence from randomized clinical trials, intravenous nitroglycerin, which is still the most familiar vasodilative agent among clinicians, can be administered safely and effectively to improve outcomes in patients with AHF and severely high BP [41].
Prognostic value of BP in HF
We recognize that there is no alternative to BP measurement as a source of clinical information regarding the hemodynamic status of patients with HF. Indeed, owing to its simplicity in measurement and widespread availability, BP is of paramount clinical importance in guiding the treatment of patients with HF. Furthermore, arterial hypertension is considered one of the most common comorbidities [3] and a precursor of HF [4]. Table 1 [42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57] shows the previous clinical trials and observational studies on the prognosis of BP in patients with and without HF.
In general, associating a higher BP with a greater incidence of HF is reasonable. In a population-based longitudinal observational study including 5888 adults aged ≥65 years, isolated systolic hypertension (SBP ≥140 mmHg) was associated with an increased risk of incident HF compared to subjects without isolated systolic hypertension during a follow-up duration of 8.7 years [54]. Regarding the clinical prognosis of low versus high BP, the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) trial, which enrolled a high-risk population of 15,244 hypertensive patients, showed no evidence for an increased risk of adverse outcome in patients with low BP [56]. This observation holds true for hypertensive patients in general and for those at high risk of cardiovascular disease without a history of HF. However, in patients who have already been diagnosed with HF, the clinical significance of BP appears to differ from that in the general population or in those with other cardiovascular diseases.
A retrospective longitudinal study showed that a low SBP (< 90 mmHg) was associated with poor survival in patients with chronic HF [21]. Notably, when the subjects were categorized based on SBP levels (< 90, 90–109, 110–129, and > 129 mmHg), as BP increased, the prognosis tended to improve in the group with SBP > 129 mmHg. Interestingly, this study also showed that pronounced long-term changes in SBP were associated with poor prognosis in this population. This result is in line with a previous study, which suggested the concept of “reverse epidemiology” that implies an improved survival rate in patients with HF with an elevated BP [58]. Several studies have reported a similar association, and this correlation is reminiscent of the “obesity paradox,” the relationship between HF and obesity. A post hoc analysis of OPTIMIZE-HF registry showed that, compared to SBP ≥ 130 mmHg at discharge, SBP < 130 mmHg was not associated with outcomes, but SBP < 120 mmHg at discharge was associated with a higher risk of death among hospitalized elderly HFpEF patients with hypertension [52]. Recent observational studies have also indicated that low SBP is associated with poor prognosis in patients with HFpEF [59, 60].
It is not surprising that low BP might be considered harmful, as it can serve as a marker of worse health conditions. Even among patients on maximal guideline-directed medication therapy (GDMT), those with SBP < 110 mmHg have been shown to be at increased risk of readmission for HF [44], and this association remained significant despite no evidence of more severe disease or a greater burden of comorbidities in those with low BP [46].
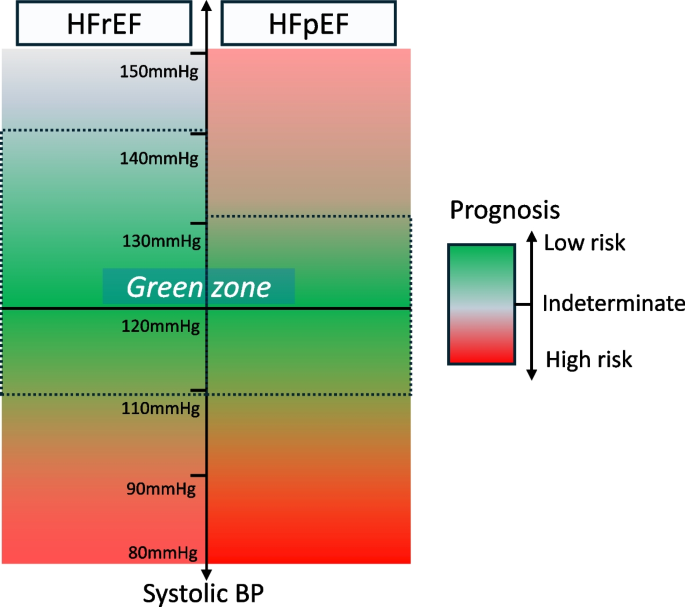
While most of these data analyzed prognosis based on baseline BP, the analysis from the KorAHF registry focused on on-treatment BP during follow-up [50]. Among the 4487 patients hospitalized for acute HF, SBP and diastolic BP (DBP) above and below the reference BP were associated with increased mortality. A nadir of 132.4/74.2 mmHg was associated with the lowest mortality rate in this cohort, especially for those with HFpEF. However, in patients with HFrEF, the mortality risk increased significantly only in the lower BP range and not in the higher BP range. In detail, the lowest risk of mortality was observed at an SBP/DBP of 136.0/76.6 mmHg for HFrEF, and at 127.9/72.7 mmHg for HFpEF. This pattern of association with BP profile was also described in a previous study [61], although the classification of HF was comparatively different; patients with mild-to-moderate LV systolic dysfunction (LVEF, 30–50%) had a U-shaped association with mortality, but patients with severe LV systolic dysfunction (LVEF, < 30%) had a linear relationship with lower SBP, which was associated with increased mortality. Thus, it can be inferred that the association among HFrEF, HFpEF, and BP had a relatively different pattern. Taken together, these results suggest that there may be a safer BP range in HF, although it is not clear-cut; lower BP is associated with a higher risk in HFrEF and HFpEF, and while HFrEF has a wider margin of safety for higher BP, HFpEF has a narrower margin of safety because higher BP is also associated with increased risk in HFpEF compared to that in HFrEF (Fig. 1).
A conceptual safety margin (“green zone”) for blood pressure (BP) in each heart failure group. Heart failure with reduced ejection fraction (HFrEF) has a wide safety margin for BP, with a lower BP being at higher risk. Heart failure with preserved ejection fraction (HFpEF) has a relatively narrow safety margin for BP, with both higher and lower BP being at higher risk
Medication affecting BP in HF
Most agents proven to have a survival benefit in HF have the potential to lower BP (such as ACEis, ARBs, β-blockers, angiotensin receptor-neprilysin inhibitors [ARNIs], MRAs, and sodium glucose cotransporter 2 [SGLT2] inhibitors) to a greater or lesser extent; however, not all BP-lowering treatments have the same beneficial effects, as summarized in Table 2 [12, 13, 16, 42, 62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78]. It is challenging to establish a direct relationship between the probability of clinical benefit and BP-lowering alone, particularly in more recent studies where the number of medications used in the study population was higher than that in previous studies. Additionally, in some cases, lowering the BP was neither beneficial nor detrimental, thereby complicating the assessment of contribution of BP to the benefits of GDMT in HF. These conflicting results have raised the question of whether reduction in BP is due to the positive effects of drugs with BP-lowering effects or, conversely, whether these drugs have deleterious effects that are offset by the benefits of neurohumoral regulation [79]. Nevertheless, the importance of treating BP in HF is consensually recognized in the HF and hypertension guidelines [38, 80, 81] both of which recommend drugs that have been reliably demonstrated in randomized clinical trials to improve outcomes as first-line therapy, especially for HFrEF [82].
Given that certain agents (such as metoprolol, carvedilol, and MRAs) without clear evidence of BP-lowering effect, significantly improved outcomes in HFrEF [70, 83] and that some agents (such as calcium channel blockers [CCBs], moxonidine, and α-blockers) with significant BP-lowering effects in the general hypertensive population had no/harmful effects on HFrEF [84, 85], it is now established that lowering BP per se is not associated with improved outcomes in HF. Instead, the focus has shifted to the class of drugs and how early they are initiated, forming the foundation of the current HF pharmacotherapy with individualized combination therapy in addition to existing agents. In this regard, patients with HF who have low BP are often undertreated, and as the Change the Management of Patients with Heart Failure (CHAMP-HF) registry data show, low BP is an independent predictor of the underuse or underdosing of neurohormonal antagonists [86]. Emphasizing that in certain cases, optimizing GDMT can be advantageous when patient tolerance permits, rather than refraining from medication solely due to BP concerns remains crucial.
Treatment for BP in patients with HF
Management of BP for incident HF
Recognizing the explicit risk of cardiovascular disease progression in patients with uncontrolled BP, considering hypertension as a precursor to HF remains crucial. The Staging Classification of Heart Failure (A, B, C, D), introduced by the American College of Cardiology/American Heart Association in 2003, highlights the preventive aspect of HF and underscores the significance of risk factor management [87, 88]. Accumulating evidence shows that that antihypertensive treatment is beneficial for incident HF. In a meta-analysis that demonstrated substantial reductions in cardiovascular death, stroke, and HF compared to placebo, the most significant benefit derived from antihypertensive therapy was the prevention of HF [89]. This analysis included 42 clinical trials with a total of 192,478 randomized patients and showed that low-dose diuretics significantly reduced the risk of stroke, cardiovascular mortality, and total mortality compared to placebo, with relative risks of 0.71, 0.81, and 0.90, respectively. The greatest reduction was observed in the risk of HF (relative risk, 0.51; 95% confidence interval, 0.42–0.62). More specifically, another meta-analysis by Ettehad et al. [90] showed that for each 10-mmHg reduction in SBP, the risk of HF significantly decreased by 28%.
In Hypertension in the Very Elderly Trial (HYVET) study, active antihypertensive treatment with indapamide, with or without perindopril, reduced the risk of incident HF by 64% in patients aged ≥80 years [91]. When comparing BP after 2 years of treatment, BP reduction was more modest in the perindopril group than that in the placebo group, with an additional reduction in SBP/DBP of 15.0/6.1 mmHg. In addition to placebo-controlled trials, several studies comparing active treatment with standard treatment for hypertension have reported data on the incidence of HF. The Systolic Blood Pressure Intervention Trial (SPRINT), which assessed the role of intensive antihypertensive treatment with a target SBP < 120 mmHg, showed a 38% reduction of relative risk in the development of HF in the intensive treatment group [57].
Despite increasing evidence highlighting the significant burden of HF associated with hypertensive heart disease, current hypertension treatment guidelines lack specific pharmacological strategies for managing patients beyond BP reduction [80, 81]. However, a position paper by the Heart Failure Association, in collaboration with the European Association of Preventive Cardiology, suggests utilizing diuretics, ACEis, and ARBs to prevent HF in hypertensive patients [92]. This recommendation is based on a network meta-analysis encompassing 26 trials, which showed that these three classes of antihypertensive drugs were most effective in lowering the incidence of HF compared to placebo. Furthermore, the 2023 European Society of Hypertension guidelines recommended lowering BP with five major antihypertensive drugs including CCBs and β-blockers, in addition to the above three classes of drugs, to prevent HF development [93]. In addition, if the target blood pressure is not achieved with these medications alone, additional medications (e.g., α-blockers) are recommended as needed.
Management of BP in established HF
For patients with established HF, the prognostic meaning of BP is relatively different. Given that many HF drugs have BP-lowering effects, and that BP is one of the most important hemodynamic markers in cardiovascular disease and one of the few that can be measured directly in the clinic, BP targeting in HF is always of interest. However, there is no compelling evidence or guidelines on this aspect. Interestingly, standard HF therapy (with ACEi/ARBs, ARNIs, and β-blockers) may induce hypotension, occasionally leading to drug discontinuation. However, current HF guidelines recommend uptitrating medications to the tolerance of patients and emphasize that repeated attempts at uptitration can result in optimization, even if the initial attempts may fail [9, 94]. This is a substantial challenge and a gap between the ideal and the reality frequently encountered in clinical practice. The following questions arise: Should we aggressively pursue different classes of HF medications, even in those who have low BP, high frailty, and especially, intolerance to BP-lowering medications? Alternatively, should we maintain a certain target BP, for example, an SBP between 110 and 130 mmHg, even if it means discontinuing certain medications? The answers to these questions can be estimated through previous literature, and we should at least attempt to learn from existing evidence.
Recommendations on BP in the treatment of HF from several guidelines for HF and hypertension are summarized in Table 3 [9, 38, 81, 93, 95, 97, 98]. The 2021 European Society of Cardiology HF guideline emphasizes striving to achieve target dose of each HF medication, and the 2023 European Society of Hypertension guideline recommends combining the medications (ACEis [ARBs if not tolerated], ARNIs, BBs, MRAs, and SGLT2 inhibitors) that have been shown to have outcome benefits, particularly in HFrEF. It was common across guidelines that nondihydropyridine CCB agents were not recommended in HFrEF.
Target BP in established HF
The 2017 American College of Cardiology Foundation/American Heart Association guidelines for the management of HF recommend that optimal BP in those with hypertension and an increased risk of HF (stage A) should be < 130/80 mmHg [81]. In addition, patients with HFrEF and hypertension should be treated by GDMT titration to attain a target SBP < 130 mmHg. The target BP was also updated based on several clinical trials, primarily the SPRINT trial [99]. The 2022 focused update of Korean Hypertension Society guideline for the management of hypertension also mentioned that in patients with hypertension who are at high risk for HF or with HF, it is reasonable to control BP below 130/80 mmHg [98]. However, thus far, there are no compelling data to identify a simple BP target in patients with established HF.
In 2022, the American Heart Association/American College of Cardiology/Heart Failure Society of America updated guidelines for the management of HF, which stated that the optimal BP or antihypertensive regimens are not known for HFpEF and did not mention any BP goals for HFrEF at all [100]. As more pharmacological options become available in the modern era, the recent trend is toward maximizing GDMT within a tolerable range rather than providing a target BP. Here, the tolerability of an individual to treatment is assessed using safety indicators such as hypotension or renal insufficiency. If there are no adverse events, maximizing GDMT is deemed more important, suggesting that clinicians should not passively treat by solely providing a target BP.
Differences in BP management between those with HFrEF and HFpEF
In general, guideline-recommended BP management for HFpEF was not significantly different from that for HFrEF. The difference is that hypertension is not as prevalent in HFrEF as in HFpEF, and patients with HFrEF rarely have uncontrolled BP [95]. In hypertensive patients, CCB is an option for BP control, although as mentioned above, the role of CCBs in HFrEF is limited (Table 2). However, the role of CCBs in HFpEF in the current era is not necessarily associated with worse HF outcomes. Although the Prospective Randomized Amlodipine Survival Evaluation-2 (PRAISE-2) study, which did not show the efficacy of amlodipine in HFrEF, had limited baseline medical treatment to ACEi (99%) and β-blocker use (19%) [78], a recent observational study on CCBs in HFpEF showed the noninferiority of CCBs, both dihydropyridines and nondihydropyridines, in addition to multiple drug usage, with β-blocker being used in more than two-thirds and MRA in one-quarter of the cases [101]. Although randomized clinical studies are required, evidence from studies on HFpEF suggests that CCB may still be effective in lowering BP and improving outcomes. In other words, it suggests that more aggressive BP management is feasible and effective by utilizing conventional antihypertensive agents to improve outcomes in patients with HFpEF compared to those with HFrEF. The 2023 European Society of Hypertension guideline also mentioned that the use of all major antihypertensive drugs including CCBs are recommended in HFpEF, and the use of ARNIs or MRAs can be considered in HFpEF with lower LVEF spectrum (Table 3).
Time in BP target range in HF
A practical limitation of what we learn from clinical research is that BP measurements are taken only at a certain point in time. BP is a continuous metric that changes over time, so continuous BP monitoring and “time in target range” is also important for BP management, and some recent studies reinforce this point of view. Huang et al. [102] reported a post hoc analysis of the Treatment of Preserved Cardiac Function HF with an Aldosterone Antagonist (TOPCAT) trial, which compared the efficacy of spironolactone in patients with HFpEF and showed that the duration in the target range of SBP between 110 and 130 mmHg was associated with better clinical outcomes, including mortality and hospitalizations for HF. Moreover, subgroup analyses showed that it was more significant in younger patients than in older patients.
In addition, Chen et al. [103] reported another post hoc analysis of data from the TOPCAT trial and the Beta-Blocker Evaluation of Survival Trial (BEST), which showed that a longer duration of BP in the target range of SBP between 120 and 130 mmHg was associated with a lower risk of major adverse cardiovascular events in hypertensive patients with HF. Since the BEST trial enrolled patients with HFrEF and the TOPCAT trial enrolled patients with HFpEF, this post hoc study concluded that a longer duration in the target range was highly associated with better cardiovascular outcomes regardless of LVEF. However, these studies were still limited by the fact that they did not analyze different combinations of various HF drug classes. Therefore, additional studies with similar designs are anticipated to provide additional insights into BP management in the HFrEF population.
Conclusions
Most of the HF medications have a mechanism and effect of lowering BP. Addressing patients with marginal BP poses significant therapeutic challenges, particularly considering that several other medications or clinical situations can also lower BP. Given the association of low BP with adverse prognosis, establishing a target BP and determining the ideal treatment strategy are critical, yet complex.
Many of these questions remain unanswered. How do we set a target BP? Can we unify all patients with HF using a single target BP? How do we individualize treatment and divide that subgroup? What evidence should we base our treatment on, and how do we categorize these patients for clinical research? How do we identify those who can benefit from further BP reduction and those who cannot? Which of the various HF medications should be titrated first for BP, when, and how much? Determining the optimal timing, dosage adjustments, and titration strategies for HF medication in the context of BP management requires further investigation.
Furthermore, the target BP varies depending on factors such as the patient’s condition, underlying comorbidities, etiology of HF, and the response of BP to medications. Some individuals have preserved tissue perfusion and no symptoms or signs of exercise intolerance or organ hypoperfusion even at lower BP, whereas others develop these dysfunctions even at normal or high BP. This highlights the difficulty of adopting a one-size-fits-all approach for treating HF, and it is hoped that more targeted treatments will become available depending on the underlying pathogenesis of HF.
Availability of data and materials
Not applicable.
Abbreviations
- ACEi:
-
Angiotensin-converting enzyme inhibitor
- AHA:
-
American Heart Association
- AHF:
-
Acute heart failure
- ARB:
-
Angiotensin receptor blocker
- ARNI:
-
Angiotensin receptor-neprilysin inhibitor
- BB:
-
β-blocker
- BEST:
-
Beta-blocker Evaluation of Survival Trial
- BP:
-
Blood pressure
- CCB:
-
Calcium channel blocker
- CHAMP-HF:
-
Change the Management of Patients with Heart Failure
- CHARM:
-
Candesartan in Heart failure Assessment of Reduction in Mortality and Morbidity
- CI:
-
Confidence interval
- COPERNICUS:
-
Carvedilol Prospective Randomized Cumulative Survival
- CV:
-
Cardiovascular
- DAPA-HF:
-
Dapagliflozin and Prevention of Adverse outcomes in Heart Failure
- DBP:
-
Diastolic blood pressure
- DELIVER:
-
Dapagliflozin Evaluation to Improve the Lives of patients with Preserved Ejection Fraction Feart Failure
- DIG:
-
Digitalis Investigation Group
- EMPEROR:
-
Empagliflozin Outcome Trial in patients with Chronic Heart Failure
- EMPHASIS-HF:
-
Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure
- ESC:
-
European Society of Cardiology
- ESH:
-
European Society of Hypertension
- GDMT:
-
Guideline-Directed Medication Therapy
- H-AHF:
-
Hypertensive acute heart failure
- HF:
-
Heart failure
- HFmrEF:
-
Heart failure with mildly reduced ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- HHF:
-
Hospitalization for heart failure
- HR:
-
Hazard ratio
- HYVET:
-
Hypertension in the Very Elderly Trial
- I-PRESERVE:
-
Irbesartan in heart failure with Preserved ejection fraction
- KorAHF:
-
Korean Acute Heart Failure
- KSH:
-
Korean Society of Hypertension
- LV:
-
Left ventricular
- LVEF:
-
Left ventricular ejection fraction
- LVH:
-
Left ventricular hypertrophy
- MERIT-HF:
-
Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure
- MI:
-
Myocardial infarction
- MRA:
-
Mineralocorticoid receptor antagonist
- NA:
-
Not applicable
- NYHA:
-
New York Heart Association
- OPTIMIZE-HF:
-
Organized Program to Initiate Lifesaving Treatment In Hospitalized patients with Heart Failure
- PARADIGM-HF:
-
Prospective Comparison of ARNI with ACEi to determine Impact on Global Mortality and Morbidity in Heart Failure
- PARAGON-HF:
-
Prospective Comparison of ARNI with ARB Global Outcomes in Heart Failure with preserved ejection fraction
- PEP-CHF:
-
Perindopril in Elderly People with Chronic Heart Failure
- PRAISE-2:
-
Prospective Randomized Amlodipine Survival Evaluation-2
- PRECISE:
-
Prospective Randomized Trial of the Optimal Evaluation of Cardiac Symptoms and Revascularization
- RAS:
-
Renin-angiotensin system
- RCT:
-
Randomized controlled trial
- SBP:
-
Systolic blood pressure
- SENIORS:
-
Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors with Heart Failure
- SGLT2:
-
Sodium glucose cotransporter 2
- SOLVD:
-
Studies Of Left Ventricular Dysfunction
- SPRINT:
-
Systolic Blood Pressure Intervention Trial
- TNT:
-
Treating to new targets
- TOPCAT:
-
Treatment Of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist
- Val-HeFT:
-
Valsartan-Heart Failure Trial
- VALUE:
-
Valsartan Antihypertensive Long-term Use Evaluation
- VICTORIA:
-
Vericiguat Global study in subjects with Heart Failure with Reduced Ejection Fraction
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics: 2014 update: a report from the American Heart Association. Circulation. 2014;129:e28-292.
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–19.
Meta-analysis global Group in Chronic Heart Failure (MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012;33:1750–7.
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41.
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62.
Messerli FH, Rimoldi SF, Bangalore S. The transition from hypertension to heart failure: contemporary update. JACC Heart Fail. 2017;5:543–51.
Oh GC, Cho HJ. Blood pressure and heart failure. Clin Hypertens. 2020;26:1.
Cho JY, Cho DH, Youn JC, Kim D, Park SM, Jung MH, et al. Korean Society of Heart Failure Guidelines for the management of heart failure: definition and diagnosis. Int J Heart Fail. 2023;5:51–65.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022;145:e895-1032.
Tsuji K, Sakata Y, Nochioka K, Miura M, Yamauchi T, Onose T, et al. Characterization of heart failure patients with mid-range left ventricular ejection fraction-a report from the CHART-2 study. Eur J Heart Fail. 2017;19:1258–69.
Borlaug BA, Redfield MM. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation. 2011;123:2006–14.
Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet. 2003;362:777–81.
Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J, et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338–45.
Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF registry. J Am Coll Cardiol. 2007;50:768–77.
Arnold SV, Silverman DN, Gosch K, Nassif ME, Infeld M, Litwin S, et al. Beta-blocker use and heart failure outcomes in mildly reduced and preserved ejection fraction. JACC Heart Fail. 2023;11(8 Pt 1):893–900.
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383–92.
Lupón J, Gavidia-Bovadilla G, Ferrer E, de Antonio M, Perera-Lluna A, López-Ayerbe J, et al. Heart failure with preserved ejection fraction infrequently evolves toward a reduced phenotype in long-term survivors. Circ Heart Fail. 2019;12:e005652.
Lee CJ, Park S. Hypertension and heart failure with preserved ejection fraction. Heart Fail Clin. 2021;17:337–43.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–60.
Styron JF, Jois-Bilowich P, Starling R, Hobbs RE, Kontos MC, Pang PS, et al. Initial emergency department systolic blood pressure predicts left ventricular systolic function in acute decompensated heart failure. Congest Heart Fail. 2009;15:9–13.
Chioncel O, Lainscak M, Seferovic PM, Anker SD, Crespo-Leiro MG, Harjola VP, et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC heart failure long-term registry. Eur J Heart Fail. 2017;19:1574–85.
Cho JH, Choe WS, Cho HJ, Lee HY, Jang J, Lee SE, et al. Comparison of characteristics and 3-year outcomes in patients with acute heart failure with preserved, mid-range, and reduced ejection fraction. Circ J. 2019;83:347–56.
Viau DM, Sala-Mercado JA, Spranger MD, O’Leary DS, Levy PD. The pathophysiology of hypertensive acute heart failure. Heart. 2015;101:1861–7.
Collins SP, Levy PD, Martindale JL, Dunlap ME, Storrow AB, Pang PS, et al. Clinical and research considerations for patients with hypertensive acute heart failure: a consensus statement from the Society of Academic Emergency Medicine and the Heart Failure Society of America acute heart failure working group. J Card Fail. 2016;22:618–27.
Collins SP, Levy PD, Fermann GJ, Givertz MM, Martindale JM, Pang PS, et al. What’s next for acute heart failure research? Acad Emerg Med. 2018;25:85–93.
Girbes ARJ, de Grooth HJ. Time to stop randomized and large pragmatic trials for intensive care medicine syndromes: the case of sepsis and acute respiratory distress syndrome. J Thorac Dis. 2020;12(Suppl 1):S101–9.
Collins S, Martindale J. Optimizing hypertensive acute heart failure management with afterload reduction. Curr Hypertens Rep. 2018;20:9.
Liu JX, Uppal S, Patel V. Management of acute hypertensive heart failure. Heart Fail Clin. 2019;15:565–74.
Adams KF Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the acute decompensated heart failure National Registry (ADHERE). Am Heart J. 2005;149:209–16.
Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, et al. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: findings from OPTIMIZE-HF. Arch Intern Med. 2008;168:847–54.
Arrigo M, Gayat E, Parenica J, Ishihara S, Zhang J, Choi DJ, et al. Precipitating factors and 90-day outcome of acute heart failure: a report from the intercontinental GREAT registry. Eur J Heart Fail. 2017;19:201–8.
Sokolska JM, Sokolski M, Zymliński R, Biegus J, Siwołowski P, Nawrocka-Millward S, et al. Patterns of dyspnoea onset in patients with acute heart failure: clinical and prognostic implications. ESC Heart Fail. 2019;6:16–26.
Lee DS, Lee JS, Schull MJ, Borgundvaag B, Edmonds ML, Ivankovic M, et al. Prospective validation of the emergency heart failure mortality risk grade for acute heart failure. Circulation. 2019;139:1146–56.
Rosman Y, Kopel E, Shlomai G, Goldenberg I, Grossman E. The association between admission systolic blood pressure of heart failure patients with preserved systolic function and mortality outcomes. Eur J Intern Med. 2015;26:807–12.
Collins SP, Jenkins CA, Harrell FE Jr, Liu D, Miller KF, Lindsell CJ, et al. Identification of emergency department patients with acute heart failure at low risk for 30-day adverse events: the STRATIFY decision tool. JACC Heart Fail. 2015;3:737–47.
Chioncel O, Mebazaa A, Harjola VP, Coats AJ, Piepoli MF, Crespo-Leiro MG, et al. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC heart failure long-term registry. Eur J Heart Fail. 2017;19:1242–54.
Cotter G, Davison BA, Butler J, Collins SP, Ezekowitz JA, Felker GM, et al. Relationship between baseline systolic blood pressure and long-term outcomes in acute heart failure patients treated with TRV027: an exploratory subgroup analysis of BLAST-AHF. Clin Res Cardiol. 2018;107:170–81.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Kitai T, Tang WH, Xanthopoulos A, Murai R, Yamane T, Kim K, et al. Impact of early treatment with intravenous vasodilators and blood pressure reduction in acute heart failure. Open Heart. 2018;5:e000845.
Harrison N, Pang P, Collins S, Levy P. Blood pressure reduction in hypertensive acute heart failure. Curr Hypertens Rep. 2021;23:11.
Levy P, Compton S, Welch R, Delgado G, Jennett A, Penugonda N, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med. 2007;50:144–52.
Rouleau JL, Roecker EB, Tendera M, Mohacsi P, Krum H, Katus HA, et al. Influence of pretreatment systolic blood pressure on the effect of carvedilol in patients with severe chronic heart failure: the carvedilol prospective randomized cumulative survival (COPERNICUS) study. J Am Coll Cardiol. 2004;43:1423–9.
Lee TT, Chen J, Cohen DJ, Tsao L. The association between blood pressure and mortality in patients with heart failure. Am Heart J. 2006;151:76–83.
Desai RV, Banach M, Ahmed MI, Mujib M, Aban I, Love TE, et al. Impact of baseline systolic blood pressure on long-term outcomes in patients with advanced chronic systolic heart failure (insights from the BEST trial). Am J Cardiol. 2010;106:221–7.
Banach M, Bhatia V, Feller MA, Mujib M, Desai RV, Ahmed MI, et al. Relation of baseline systolic blood pressure and long-term outcomes in ambulatory patients with chronic mild to moderate heart failure. Am J Cardiol. 2011;107:1208–14.
Böhm M, Young R, Jhund PS, Solomon SD, Gong J, Lefkowitz MP, et al. Systolic blood pressure, cardiovascular outcomes and efficacy and safety of sacubitril/valsartan (LCZ696) in patients with chronic heart failure and reduced ejection fraction: results from PARADIGM-HF. Eur Heart J. 2017;38:1132–43.
Selvaraj S, Claggett BL, Böhm M, Anker SD, Vaduganathan M, Zannad F, et al. Systolic blood pressure in heart failure with preserved ejection fraction treated with sacubitril/valsartan. J Am Coll Cardiol. 2020;75:1644–56.
Lam CS, Mulder H, Lopatin Y, Vazquez-Tanus JB, Siu D, Ezekowitz J, et al. Blood pressure and safety events with vericiguat in the VICTORIA trial. J Am Heart Assoc. 2021;10:e021094.
Vidán MT, Bueno H, Wang Y, Schreiner G, Ross JS, Chen J, et al. The relationship between systolic blood pressure on admission and mortality in older patients with heart failure. Eur J Heart Fail. 2010;12:148–55.
Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, et al. Reverse J-curve relationship between on-treatment blood pressure and mortality in patients with heart failure. JACC Heart Fail. 2017;5:810–9.
Arundel C, Lam PH, Gill GS, Patel S, Panjrath G, Faselis C, et al. Systolic blood pressure and outcomes in patients with heart failure with reduced ejection fraction. J Am Coll Cardiol. 2019;73:3054–63.
Faselis C, Lam PH, Zile MR, Bhyan P, Tsimploulis A, Arundel C, et al. Systolic blood pressure and outcomes in older patients with HFpEF and hypertension. Am J Med. 2021;134:e252–63.
D’Agostino RB, Belanger AJ, Kannel WB, Cruickshank JM. Relation of low diastolic blood pressure to coronary heart disease death in presence of myocardial infarction: the Framingham study. BMJ. 1991;303:385–9.
Ekundayo OJ, Allman RM, Sanders PW, Aban I, Love TE, Arnett D, et al. Isolated systolic hypertension and incident heart failure in older adults: a propensity-matched study. Hypertension. 2009;53:458–65.
Bangalore S, Messerli FH, Wun CC, Zuckerman AL, DeMicco D, Kostis JB, et al. J-curve revisited: an analysis of blood pressure and cardiovascular events in the treating to new targets (TNT) trial. Eur Heart J. 2010;31:2897–908.
Kjeldsen SE, Berge E, Bangalore S, Messerli FH, Mancia G, Holzhauer B, et al. No evidence for a J-shaped curve in treated hypertensive patients with increased cardiovascular risk: the VALUE trial. Blood Press. 2016;25:83–92.
Upadhya B, Rocco M, Lewis CE, Oparil S, Lovato LC, Cushman WC, et al. Effect of intensive blood pressure treatment on heart failure events in the systolic blood pressure reduction intervention trial. Circ Heart Fail. 2017;10:e003613.
Güder G, Frantz S, Bauersachs J, Allolio B, Wanner C, Koller MT, et al. Reverse epidemiology in systolic and nonsystolic heart failure: cumulative prognostic benefit of classical cardiovascular risk factors. Circ Heart Fail. 2009;2:563–71.
Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol. 2018;263:69–74.
Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic blood pressure and outcomes in patients with heart failure with preserved ejection fraction. JAMA Cardiol. 2018;3:288–97.
Ather S, Chan W, Chillar A, Aguilar D, Pritchett AM, Ramasubbu K, et al. Association of systolic blood pressure with mortality in patients with heart failure with reduced ejection fraction: a complex relationship. Am Heart J. 2011;161:567–73.
Investigators SOLVD, Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302.
Cohn JN, Tognoni G. Valsartan heart failure trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–75.
McMurray JJ, Ostergren J, Swedberg K, Granger CB, Held P, Michelson EL, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-added trial. Lancet. 2003;362:767–71.
Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456–67.
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004.
Solomon SD, McMurray JJ, Anand IS, Ge J, Lam CS, Maggioni AP, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381:1609–20.
Packer M, Fowler MB, Roecker EB, Coats AJ, Katus HA, Krum H, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002;106:2194–9.
Packer M, Colucci WS, Sackner-Bernstein JD, Liang CS, Goldscher DA, Freeman I, et al. Double-blind, placebo-controlled study of the effects of carvedilol in patients with moderate to severe heart failure. The PRECISE trial. Prospective randomized evaluation of carvedilol on symptoms and exercise. Circulation. 1996;94:2793–9.
Effect of metoprolol CR/XL in chronic heart failure. Metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet. 1999;353:2001–7.
Flather MD, Shibata MC, Coats AJ, Van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26:215–25.
Zannad F, McMurray JJ, Krum H, van Veldhuisen DJ, Swedberg K, Shi H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–24.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61.
McMurray JJ, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Solomon SD, Vaduganathan M, Claggett BL, de Boer RA, DeMets D, Hernandez AF, et al. Baseline characteristics of patients with HF with mildly reduced and preserved ejection fraction: DELIVER trial. JACC Heart Fail. 2022;10:184–97.
Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, Butler J, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382:1883–93.
Packer M, Carson P, Elkayam U, Konstam MA, Moe G, O’Connor C, et al. Effect of amlodipine on the survival of patients with severe chronic heart failure due to a nonischemic cardiomyopathy: results of the PRAISE-2 study (prospective randomized amlodipine survival evaluation 2). JACC Heart Fail. 2013;1:308–14.
Hartupee J, Mann DL. Neurohormonal activation in heart failure with reduced ejection fraction. Nat Rev Cardiol. 2017;14:30–8.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127–248.
Pinho-Gomes AC, Rahimi K. Management of blood pressure in heart failure. Heart. 2019;105:589–95.
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. carvedilol heart failure study group. N Engl J Med. 1996;334:1349–55.
Udelson JE, DeAbate CA, Berk M, Neuberg G, Packer M, Vijay NK, et al. Effects of amlodipine on exercise tolerance, quality of life, and left ventricular function in patients with heart failure from left ventricular systolic dysfunction. Am Heart J. 2000;139:503–10.
Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure: results of a veterans administration cooperative study. N Engl J Med. 1986;314:1547–52.
Greene SJ, Butler J, Albert NM, DeVore AD, Sharma PP, Duffy CI, et al. Medical therapy for heart failure with reduced ejection fraction: the CHAMP-HF registry. J Am Coll Cardiol. 2018;72:351–66.
Pfeffer MA. Heart failure and hypertension: importance of prevention. Med Clin North Am. 2017;101(1):19–28.
Jessup M, Brozena S. Heart failure. N Engl J Med. 2003;348:2007–18.
Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289:2534–44.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
Piepoli MF, Adamo M, Barison A, Bestetti RB, Biegus J, Böhm M, et al. Preventing heart failure: a position paper of the heart failure association in collaboration with the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2022;29:275–300.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European renal association (ERA). J Hypertens. 2023;41:1874–2071.
Greene SJ, Butler J, Fonarow GC. Simultaneous or rapid sequence initiation of quadruple medical therapy for heart failure-optimizing therapy with the need for speed. JAMA Cardiol. 2021;6:743–4.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Khan SS, Ning H, Shah SJ, Yancy CW, Carnethon M, Berry JD, et al. 10-year risk equations for incident heart failure in the general population. J Am Coll Cardiol. 2019;73:2388–97.
Park SM, Lee SY, Jung MH, Youn JC, Kim D, Cho JY, et al. Korean Society of Heart Failure Guidelines for the management of heart failure: management of the underlying etiologies and comorbidities of heart failure. Int J Heart Fail. 2023;5:127–45.
Kim HL, Lee EM, Ahn SY, Kim KI, Kim HC, Kim JH, et al. The 2022 focused update of the 2018 Korean hypertension society guidelines for the management of hypertension. Clin Hypertens. 2023;29:11.
SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. 2022;79:e263–421.
Matsumoto S, Kondo T, Yang M, Campbell RT, Docherty KF, de Boer RA, et al. Calcium channel blocker use and outcomes in patients with heart failure and mildly reduced and preserved ejection fraction. Eur J Heart Fail. 2023;25:2202–14.
Huang R, Lin Y, Liu M, Xiong Z, Zhang S, Zhong X, et al. Time in target range for systolic blood pressure and cardiovascular outcomes in patients with heart failure with preserved ejection fraction. J Am Heart Assoc. 2022;11:e022765.
Chen K, Li C, Cornelius V, Yu D, Wang Q, Shi R, et al. Prognostic value of time in blood pressure target range among patients with heart failure. JACC Heart Fail. 2022;10:369–79.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
KHC wrote the draft and SMK edited and supervised the whole article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chun, KH., Kang, SM. Blood pressure and heart failure: focused on treatment. Clin Hypertens 30, 15 (2024). https://doi.org/10.1186/s40885-024-00271-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40885-024-00271-y