Abstract
Background
Arsenic is a carcinogenic heavy metal that contaminates the environment, predisposing the exposed populace to its detrimental health effects. This study investigated the liver protective effect of ethanol leaf extract of Irvingia gabonensis (ELEIG) in sodium arsenite (SA)-exposed Wistar rats and its nitric oxide (NO.) and hydrogen peroxide (H2O2)-scavenging properties in vitro.
Methods
Eleven experimental groups made up of five (5) rats each (weight range 100 - 161 g) were used in this study. Group 1 (normal control) had normal rat chow and water. Group 2 received 4.1 mg/kg body weight (kgbw) of SA. Groups 3–8 received SA and graded doses of ELEIG and groups 9-11 had varied doses of ELEIG. Treatment, which spanned 14 days, was by oral gavage. Concentrations of catalase (CAT), superoxide dismutase (SOD), glutathione peroxidase (GPx), malondialdehyde (MDA) as well as activities of liver enzymes (AST, ALT, ALP, and GGT) and concentrations of total bilirubin (TBIL) and direct bilirubin (DBIL) were determined using standard procedures. Standard methods were also used to determine the in vitro NO. and H2O2-scavenging properties of the extract.
Results
Exposure to SA orchestrated significant (p ˂ 0.05) increases in CAT, MDA, AST, ALT, ALP and GGT and significant (p ˂ 0.05) decreases in SOD and GPx, relative to control. There were insignificant (p ˃ 0.05) differences in TBIL and DBIL concentrations, compared with control. Simultaneous and post-treatment with ELEIG at graded doses, alleviated the noxious effects of SA. In addition, ELEIG scavenged NO. and H2O2 in concentration-dependent manner.
Conclusion
The results suggest that ELEIG possesses potent antioxidant property and combats SA-induced hepatic oxidative stress/toxicity in Wistar rats.
Similar content being viewed by others
Background
Environmental pollution is a global menace that negatively impacts the health of a myriad of individuals, resulting in the development of various disease conditions. Arsenic is an environmental pollutant and a carcinogen, that pollutes the environment naturally and by human activities [1]. Arsenic poisoning could occur by the consumption of arsenic-contaminated food and drinking water [1, 2]. High levels of arsenic in groundwater, has been detected in some countries like Nigeria [3, 4]. It is on record that an estimated 200 million people Worldwide are susceptible to health impairment due to high levels of arsenic in drinking water [5]. Arsenic has been reported to orchestrate hepatotoxicity via the induction of oxidative stress [6]. Furthermore, studies have shown that, liver function is compromised in different animal species by exposure to sodium arsenite [7].
The use of plants as medicine has been embraced by most Locals for several reasons, mostly because of the very high cost of orthodox drugs, and the recent re-emergence and dependence on medicinal plants in the treatment of disease conditions. Different parts of Irvingia gabonensis (edible bush mango) are utilized as medicines by Locals in combating various ailments [8]. The leaves are used as anti-poisons [9]. The Senegalese use the decoction of the stem bark in treating ailments such as gonorrhea, liver and gastrointestinal diseases and the root bark is used to treat wounds [9]. The stem bark has also been documented to possess bactericidal and fungicidal properties as well as in the treatment of yellow fever, hernias, dysentery and to mitigate poisons [10, 11]. In addition, the antitoxic effects of the leaves in Wistar rats have been documented by various researchers [12,13,14,15]. However, there is paucity of information on the antioxidant and medicinal effects of ethanol leaf extract of Irvingia gabonensis against arsenic-induced hepatic dysfunction.
Materials and methods
Leaf extract preparation
Fresh leaves of Irvingia gabonensis were harvested from Itak Ikot Akap community in Akwa Ibom State, Nigeria. They were authenticated in the Department of Pharmacognosy and Natural Medicine, University of Uyo with the voucher number: JAMES DANIEL UUH 042116 (Uyo). The leaves were washed with clean water to decontaminate them, air-dried for 7 days and pulverized using a manual grinder. The pulverized leaves were then macerated in absolute ethanol for 72 hours, with intermittent stirring to achieve adequate extraction of the bioactive phytoconstituents. The mixture was filtered repeatedly with the aid of a clean muslin cloth and the filtrate was concentrated at 45 °C, using a water bath. The dried extract was stored at 4 °C prior to analyses.
Determination of in vitro nitric oxide and hydrogen peroxide scavenging properties of ELEIG
Nitric oxide (NO.) radical-scavenging property was investigated as described by Green et al. [16]. Hydrogen Peroxide (H2O2)-scavenging property was determined according to the method of Ruch et al. [17].
Experimental animals and design
A total of 55 healthy and non-pregnant female Wistar albino rats (100 g – 161 g), were obtained from the animal house of Faculty of Basic Medical Sciences, University of Uyo, Uyo, and used for this study. They were acclimatized for seven (7) days in the same facility under standard conditions in a well-ventilated room, with free access to feed and water. After 7 days of acclimatization, the experimental animals were assigned to eleven (11) groups of five rats each in standard animal cages and their initial body weights were obtained using a digital weighing balance (Camry electronic scale EK5350, China) after overnight fast. The experimental design is shown in Table 1.
Blood sample collection and excision of liver tissues for analyses
At the end of the treatment period, the animals were anesthetized with chloroform and sacrificed by lower abdominal incision. Blood samples were collected by cardiac puncture using sterile syringes and needles into plain sample bottles for analyses and spun at 3000 rpm for 15 min using a table top centrifuge (Model 800-1, Zeny Inc. Salt Lake, USA) to obtain sera used for analyses. Liver tissues were harvested and rinsed with 1.15% ice-cold potassium chloride (KCl) solution to expunge traces of blood. Small portions of the liver tissues were fixed in 10% neutral buffered formalin for histological assessment. The remaining portions of the liver tissues were placed in sterile universal container and frozen for homogenization.
Homogenization of liver tissues
The liver tissues were homogenized, following the procedure reported by Ewere et al. [18].
Assessment of oxidative stress biomarkers
The concentrations of catalase (CAT), superoxide dismutase (SOD), glutathione peroxidase (GPx) and of malondialdehyde (MDA) in liver homogenates were determined by Enzyme-linked Immunosorbent Assay (ELISA) using Sunlong Biotech Co. (Zhejiang, China) assay kits according to manufacturer’s protocol.
Determination of serum liver enzymes activities and serum total bilirubin (TBIL) and direct bilirubin (DBIL) concentrations
TECO diagnostic assay kits (Anahaema, USA) were used for the determination of serum liver enzymes activities and serum total bilirubin (TBIL) and direct bilirubin (DBIL) concentrations. Aspartate aminotransferase (AST) activity was determined according to the method of Young [19]. Alanine aminotransferase (ALT) activity was determined according to the method of Young et al. [20]. Alkaline phosphatase (ALP) activity was determined by the method of Kochmar and Moss [21] and the method of Young et al. [20] was used to determine the activity of gamma glutamyltransferase (GGT). Serum total bilirubin (TBIL) and direct bilirubin (DBIL) concentrations were determined by the method of Tietz [22].
Histological assessment of liver tissues excised from experimental rats
Histological assessment of the excised liver tissues was carried out, using the procedure reported by Ewere et al. [23]. The liver tissues were prepared for histological assessment using haematoxylin and eosin staining method (H&E). After the tissues were stained, sections were examined under a Leica DM500 microscope and results were reported by a Consultant Histopathologist. An attached Leica ICC50 digital camera was used to take photomicrographs.
Statistical analysis
For NO. and H2O2 scavenging assays, the experiments were performed in triplicates and the data obtained were calculated and expressed as mean ± standard deviation (SD) with the aid Microsoft Excel. Data obtained from the animal study are presented as mean ± standard deviation (SD) and were analyzed using one-way analysis of variance (ANOVA). Post hoc analysis was carried out using least significant difference (LSD) with the aid of SPSS Software (IBM, version 20). Mean difference between groups were considered statistically significant at p ˂ 0.05.
Results
Hydrogen peroxide (H2O2) scavenging properties of ELEIG
Results obtained revealed that ELEIG possesses potent H2O2 scavenging properties when compared with ascorbic acid standard. Percentage of H2O2 scavenged measured at concentrations of 10, 20, 40, 80 and 160 μg/mL of the extract were: 34.55 ± 1.39%, 37.70 ± 0.53%, 41.88 ± 0.53%, 42.93 ± 0.53%, 43.63 ± 0.30%, respectively, and 36.82 ± 0.30%, 38.22 ± 0.52%, 42.76 ± 1.68%, 50.43 ± 2.58%, 59.16 ± 2.77%, respectively, for ascorbic acid (standard). The I.C50 of ELEIG and ascorbic acid (standard) were 258.47 μg/mL and 91.95 μg/mL, respectively. The results are shown in Fig. 1.
Nitric oxide (NO.) scavenging properties of ELEIG
Results obtained revealed that ELEIG possesses potent NO. scavenging properties, relative to ascorbic acid standard. Percentage of NO. scavenged measured at concentrations of 10, 20, 40, 80 and 160 μg/mL of ELEIG were: 23.55 ± 0.17%, 25.45 ± 0.08%, 28.26 ± 0.18%, 28.71 ± 0.10%, 30.44 ± 0.20%, respectively and 33.76 ± 0.18%, 35.17 ± 0.26%, 44.43 ± 0.07%, 48.50 ± 3.12%, 54.96 ± 0.07%, respectively for ascorbic acid (standard). The I.C50 of ELEIG and ascorbic acid (standard) were 640.05 μg/mL and 109.72 μg/mL, respectively. The results are shown in Fig. 2.
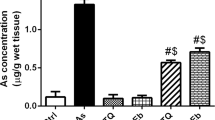
Effect of ELEIG on hepatic function of SA-intoxicated experimental rats
Results obtained revealed that, intoxication with sodium arsenite caused significant (p ˂ 0.05) increases in serum AST, ALT, ALP and GGT activities, relative to the control group. Post-treatment with ELEIG culminated in significant (p ˂ 0.05) decreases in serum ALT, ALP and GGT activities, in dose-dependent fashion and non-significant (p ˃ 0.05) decreases in serum AST activities in dose-dependent manner except group 5, whose serum AST activity was significantly (p ˂ 0.05) decreased, when compared with group 2, administered sodium arsenite only. Simultaneous treatment with ELEIG followed the same trend as the post-treatment. Comparison of ELEIG exclusively-treated groups and the normal control group, showed no significant (p ˃ 0.05) differences in serum activities of the liver enzymes, with the exception of ALP. However, ELEIG at the highest dose (400 mg/kgbw), produced significant (p ˂ 0.05) decreases in serum AST and ALT activities, relative to the normal control. Furthermore, there were no significant (p ˃ 0.05) differences in serum TBIL and DBIL concentrations across all the treatment groups, after sodium arsenite intoxication. The results are shown in Table 2.
Effect of ELEIG on oxidative stress biomarkers of experimental rats
Results obtained showed that oral exposure of the experimental animals to sodium arsenite (group 2), culminated in significant (p ˂ 0.05) decreases in hepatic SOD and GPx concentrations and significant (p ˂ 0.05) increases in hepatic CAT and MDA concentrations, relative to the normal control. Post-treatment with ELEIG, at graded doses, led to significant (p ˂ 0.05) increases in SOD and GPx concentrations as well as significant (p ˂ 0.05) decreases in CAT and MDA concentrations, in dose-dependent and independent manner, relative to group 2. Similar trends were observed following simultaneous treatment with ELEIG. In addition, administration of ELEIG alone at various doses, produced similar results for the oxidative stress biomarkers with that of the control group. The results are presented in Table 3.
Effect of ELEIG on liver histology of experimental rats
Intoxication with sodium arsenite (group 2), induced severe vascular ulceration, portal congestion and periportal infiltrates of inflammatory cells (portal hepatitis) as well as severe microvesicular steatosis in the liver of the experimental rats. Simultaneous and post-treatment with graded doses (100, 200, and 400 mg/kgbw) of ELEIG, achieved dose-dependent ameliorative and therapeutic effects. The results are shown in the photomicrographs (Figs. 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 and 13).
Discussion
Reactive oxygen species (ROS) and reactive nitrogen species (RNS), when in excess, are generally known to orchestrate the induction of oxidative stress in vivo, which underlies the etiologies of various disease conditions [24]. Bioactive agents, especially those of plant origin, that have the capacity to mitigate the noxious effects of ROS, are of promise in combating the plethora of diseases, linked to oxidative stress [25]. Enzymes called nitric oxide synthases, are involved in the production of the free radical, nitric oxide (NO.) in biological tissues [26]. The enzymes catalyze the conversion of the amino acid, arginine to citrulline, while forming NO. via a five-electron oxidative reaction [27]. Some negative health conditions such as dizziness, blurred vision, unusual bleeding, confusion, headache, and rapid heart rate, have been linked to excessive production of NO.. Hydrogen peroxide (H2O2) is a reactive oxygen species that is capable of decomposing rapidly into water and oxygen, which may ultimately lead to the generation of hydroxyl radical (OH.) that could initiate lipid peroxidation and DNA damage. Exposure to H2O2 could be through eye/skin contact or by the inhalation of vapour or mist [26]. In the present study, ELEIG scavenged NO. and H2O2 in a concentration-dependent manner, comparable to ascorbic acid (standard). This implies the potent antioxidant property of the extract which may not be unconnected with its inherent phytochemicals that have been reported to possess high antioxidant properties [28].
The liver is a rich source of the aminotransferases, AST and ALT [29]. These enzymes are involved in transamination reactions [30]. In hepatocellular damage (which could by exposure to toxic elements), the blood levels of these enzymes are elevated. Their blood levels directly reveal the extent of tissue damage [31].
In this study, administration of sodium arsenite (SA) culminated in significant increases in serum levels of AST and ALT, relative to the normal control. This implies hepatocellular damage by SA, leading to the leakage of the enzymes into the blood stream [32]. This is corroborated by findings from previous studies [33, 34]. Treatment with ELEIG (concomitant and post-treatment), achieved significant decreases in AST levels at the highest dose of 400 mg/kgbw when compared group 2 (administered sodium arsenite only). In the same vein, treatment with ELEIG produced significant decreases in ALT levels in dose-dependent manner when administered after 2 weeks of SA intoxication (post-treatment) and in dose-independent manner when administered concomitantly, compared with group 2 (administered SA only). This connotes that the extract could be ameliorative or curative. Administration of graded doses of ELEIG alone produced non-significant differences in AST and ALT levels, but significant decreases at the highest dose of 400 mg/kgbw, when compared with the normal control. The observed positive effect of the ethanol leaf extract may not be unconnected to its constituent antioxidant phytochemicals [28], since sodium arsenite / arsenic has been reported to elicit its negative health effects by induction of oxidative stress, among others [6].
Alkaline phosphatases (ALPs), catalyze hydrolysis of organic phosphate in proteins, nucleotides and alkaloids at alkaline pH [35]. They are found in several tissues but high concentrations occur in liver, bone and kidney tissues as well as placenta and intestinal wall [36]. An increase in serum ALP activity connotes occurrence of liver and bone diseases [37]. It is also indicative of obstruction of bile ducts [36]. Xenobiotic-induced hepatotoxicity, may also increase serum ALP activity [38]. The degradation of glutathione in mammalian cells is catalyzed by gamma-glutamyltransferase (GGT), a cell-surface protein found in several tissues [39]. However, a higher percentage of serum GGT is derived from the liver [40]. Diseases of the liver, biliary system and pancreas, are associated with increased serum GGT activity. High blood level of GGT is closely related to hepatic steatosis [41].
In this study, oral exposure of the experimental rats to sodium arsenite caused significant increases in serum ALP and GGT activities, relative to the normal control. However, treatment with graded doses of ELEIG (concomitant and post-treatment), led to significant decreases in serum ALP levels in dose-dependent manner compared with group 2 (administered sodium arsenite only). In the same vein, concomitant and post-treatment with graded doses of ELEIG also led to significant decreases in serum GGT levels in dose-independent manner compared with group 2 (administered sodium arsenite only). Furthermore, administration of graded doses of ELEIG alone produced non-significant differences in GGT levels and significant increases in ALP levels compared with control. This is therefore suggestive of the hepatoprotective effect of ethanol leaf extract of Irvingia gabonensis which may have been influenced by its inherent antioxidant phytochemicals [28]. Previous studies had also reported the hepatoprotective effects of ethanol leaf extract of Irvingia gabonensis under conditions of induced toxicity [13, 14].
Bilirubin, the end product of haemoglobin catabolism [32], is a biomarker of hepatic and blood disorders. An increase in serum bilirubin level indicates the occurrence of liver disease. Increase in blood levels of conjugated (direct) bilirubin, occurs in diseases such as hepatocellular damage, toxic or ischemic liver injury and viral hepatitis [32, 42]. In this study, oral exposure of the experimental animals to sodium arsenite caused non-significant increases in serum total bilirubin (TBIL) and direct bilirubin (DBIL) concentrations, relative to the control. This indicates the interference with the transport function of the liver by sodium arsenite [32]. However, there were no significant differences in serum TBIL and DBIL concentrations on treatment with ELEIG. Administration of ELEIG alone also produced non-significant differences in serum TBIL and DBIL concentrations as compared with control.
Arsenic, a heavy metal, induces oxidative stress by generating free radicals / ROS [43] that culminate in cellular damage via depletion of enzyme activities through lipid peroxidation and reaction with nuclear proteins and DNA [44]. Inorganic arsenic compounds can also induce oxidative stress by inhibiting antioxidant enzymes via binding to their sulfhydryl (−SH) groups [45].
In this study, administration of sodium arsenite alone produced significant decreases in hepatic SOD and GPx levels and significant increases in CAT and MDA levels when compared with the control group. Endogenous enzymes act as the first line of cellular defense against reactive oxygen species [46]. Oxidative stress leads to a loss in the balance between ROS production and antioxidant defense systems due to the overwhelming power of prooxidants generated, which deregulates cellular functions that can lead to hepatic necrosis [47]. The observed significant increase in hepatic CAT level in this study may be due to significant induction in catalase activity as an adaptive response for combating the induced oxidative stress. This is consistent with the findings of Gbadegesin et al. [13]. Catalase is the antioxidant enzyme that degrades hydrogen peroxide (a reactive oxygen species) produced during metabolism. It catalyzes the removal of hydrogen peroxide formed in the reaction catalyzed by superoxide dismutase [48]. Superoxide dismutase (SOD) enhances dismutation of superoxide radical to hydrogen peroxide that is then removed by catalase [49]. It may therefore serve as a primary defense and mitigates further production of free radicals. Glutathione peroxidases (GPx) facilitate the reduction of hydrogen peroxide and lipid hydroperoxides (products of lipid peroxidation) to their corresponding alcohols [50]. Malondialdehyde (MDA) is a product of lipid peroxidation whose concentration in increased in oxidative stress that can lead to the destabilization of membranes [34]. The mechanism of sodium arsenite-induced toxicity in this study may therefore be by its inhibition of antioxidant defense systems via the generation of ROS, culminating in the destabilization of cell membranes by lipid peroxidation. Other studies have also reported the induction of oxidative stress orchestrated by sodium arsenite which are consistent with the findings from this study [34].
Treatment with ELEIG (concomitant and post-treatment), produced significant increases in the levels of SOD and GPx in dose-dependent manner, and significant decreases in CAT and MDA concentrations in dose-dependent manner, when compared with group 2 administered sodium arsenite only. However, the significant decreases in CAT concentrations after post treatment with the extract were not dose-dependent. The significant decreases in CAT concentration by ELEIG, indicates an alleviation of oxidative damage by sodium arsenite which had led to induction of CAT level as an adaptive response. This connotes that the ethanol leaf extract could be ameliorative and curative. Administration of ELEIG alone at various doses also produced similar results for the oxidative stress biomarkers with that of the control group. It is therefore possible that the ethanol leaf extract mitigated sodium arsenite-induced toxicity / oxidative stress by enhancing the antioxidant defense systems in the treated rats, thereby enhancing the mopping up of the ROS generated. This may be due to the constituent antioxidant phytochemicals present in the extract. This is corroborated by the findings of Gbadegesin et al. [13].
There were no visible lesions in the liver tissues of the control group animals, following histological assessment. On the contrary, oral intoxication with sodium arsenite (group 2) caused severe vascular ulceration, portal congestion, infiltrates of inflammatory cells (portal hepatitis), and severe micro vesicular steatosis in the liver. Treatment with graded doses of ELEIG (concomitant and post-treatment), achieved dose-dependent ameliorative and therapeutic effects. Thus, the ethanol leaf extract proved effective in attenuating the sodium arsenite-induced steatohepatitis in the liver of the experimental animals. This is consistent with findings of Gbadegesin and co-workers [13].
Conclusion
On the premise of the results obtained from this study, it may be concluded that, ethanol leaf extract of Irvingia gabonensis possesses potent antioxidant property and has the capacity to mitigate sodium arsenite-induced hepatic oxidative stress and hepatotoxicity in Wistar rats, by enhancing the antioxidant defense systems in the intoxicated rats.
Availability of data and materials
All data obtained from this study are included in this article.
Abbreviations
- ELEIG:
-
Ethanol leaf extract of Irvingia gabonensis
- SA:
-
Sodium arsenite
- TBIL:
-
Total bilirubin
- DBIL:
-
Direct bilirubin
- CAT:
-
Catalase
- SOD:
-
Superoxide dismutase
- GPx:
-
Glutathione peroxidase
- MDA:
-
Malondialdehyde
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- ALP:
-
Alkaline phosphatase
- GGT:
-
Gamma glutamyltransferase
- PT:
-
Post-treatment
- ST:
-
Simultaneous treatment
- mg/kgbw:
-
Milligram per kilogram body weight
- ROS:
-
Reactive oxygen species
- RNS:
-
Reactive nitrogen species
References
WHO. Arsenic and Arsenic Compounds (Environmental Health Criteria 224), 2nd ed. Geneva: World Health Organization, International Programme on Chemical Safety. 2001.
IARC. Arsenic and arsenic compounds. IARC Monogr Eval Carcinog Risks Hum. 2012;100C:41–93.
Pandey PK, Yadav S, Nair S, Bhui A. Arsenic contamination of the environment: a new perspective from central-East India. Environ Int. 2002;28:235–45.
Ezeabasili ACC, Anike OL, Okoro BU, Dominic CM. Arsenic pollution of surface and subsurface water in Onitsha, Nigeria. Afr J Environ Sci Technol. 2014;8:491–7.
Ravenscroft P, Brammer H, Richards K. Arsenic pollution: a global synthesis. RGS-IBG Book Series, Wiley-Blackwell: Chichester UK; 2009.
Singh AP, Goel RK, Kaur T. Mechanisms pertaining to arsenic toxicity. Toxicol Int. 2011;18:87–93.
Sharma A, Sharma MK, Kumar M. Modulatory role of Emblica officinalis fruit extract against arsenic induced oxidative stress in Swiss albino mice. Chem Biol Interact. 2009;180:20–30.
Anegbeh PO, Usoro C, Ukafor V, Tchoundjeu Z, Leakey RRB, Schreckenberg K. Domestication of Irvingia gabonensis 3: phenotypic variation of fruits and kernels in a Nigeria village. Agrofor Syst. 2003;58:213–8.
Hubert DJ, Wabo FG, Ngameni B, Ngheguin TF, Tchoukoua A, Ambassa P. et.al. In vitro Hepatoprotective and antioxidant activities of the crude extract and isolated compounds from Irvingia gabonensis. Asian J Traditional Med 2010;5: 79-88.
Kuete V, Wabo GF, Ngameni B, Mbaveng AT, Metuno R, Etoa FX. et.al. Antimicrobial activity of the Methanolic extract, fractions and compounds from the stem bark of Irvingia gabonensis (Ixonanthaceae). J Ethnopharmacol 2007;114: 54-60.
Etta HE, Olisaeke CC, Iboh CI. Effect of Irvingia gabonensis (Aubry-Lecomte ex O’Rorke) seeds on the liver and gonads of male albino rats. J Biol, Agriculture Healthcare. 2014;4:10–5.
Raji IA, Ogunwande AJM, Bolarinwa AF. Anti- Diarrhegenic and anti-ulcer properties of Irvingia gabonensis in rats. Pharm Biol. 2001;39:340–5.
Gbadegesin MA, Adegoke AM, Ewere EG, Odunola OA. Hepatoprotective and anticlastogenic effects of ethanol extract of Irvingia gabonensis (IG) leaves in sodium arsenite-induced toxicity in male Wistar rats. Nigerian J Physiol Sci. 2014;29:029–36.
Ewere EG, Oyebadejo SA, Peter VC. Ethanolic leaf extract of Irvingia gabonensis (O’ Rorke) Baill protects against nephrotoxicity and Hepatotoxocity in cadmium-induced Wistar albino rats. Int J Pharmacol Toxicol. 2016a;4:105–10.
Ewere EG, Okolie NP, Avan ED, Umoh PE. Comparative effects of ethanol leaf and stem bark extracts of Irvingia gabonensis (BUSH MANGO) on sodium Arsenite-induced lipid profile perturbations in Wistar rats. Clinical Phytoscience. 2021;7:3.
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR. Analysis of nitrate and nitrite in biological fluids. Anal Biochem. 1982;126(Suppl 1):131–8.
Ruch RJ, Cheng SJ, Klaunig JE. Prevention of cytotoxicity and inhibition of intercellular communication by antioxidants isolated from Chinese Green tea. Carcinogenesis. 1989;10(Suppl 6):1003–8.
Ewere EG, Okolie NP, Etim OE, Oyebadejo SA. Mitigation of arsenic-induced increases in pro-inflammatory cytokines and Haematological derangements by ethanol leaf extract of Irvingia gabonensis. Asian J R Biochem. 2020;7(Suppl 1):36–47.
Young DS. Effects of drugs on clinical laboratory tests. 3rd ed: AACC Press; 1990.
Young DS, Pestaner LC, Gibberman V. Effects of drugs on clinical laboratory tests. Clin Chem. 1975;21(Suppl 5):1D–432D.
Kochmar JF, Moss DW. In: Tietz NW, editor. Fundamentals of clinical chemistry. Philadephia: W.B. Saunders Co; 1974. p. 604.
Tietz NW. Fundamentals of clinical chemistry. Philadelphia, PA: W.B. Saunders; 1976. p. 897.
Ewere EG, Okolie NP, Eze GI, Jegede DA. (2019). Irvingia gabonensis leaves mitigate arsenic-induced renal toxicity in Wistar rats. Asian J Biomed Pharma Sci. 2019; 9 Suppl 68: 17-25.
Fitzpatrick AM, Teague WG, Holguin F, Yeh M, Brown LA. Severe asthma research program. Airway glutathione homeostasis is altered in children with severe asthma: evidence for oxidant stress. J Allergy Clin Immunol. 2009;123:146–52.
Covacci V, Torsello A, Palozza P, Sgambato A, Romano G, Boninsegna A, et.al. DNA oxidative damage during differentiation of HL-60 human promyelocytic leukemia cells. Chem Res Toxicol 2001; 14 Suppl 11: 1492-1497.
Alam MN, Bristi NJ, Rafiquzzaman M. Review on in vivo and in vitro methods of evaluation of antioxidant activity. Saudi Pharma J. 2013;21(Suppl 2):143–52.
Ghafourifar P, Cadenas E. Mitochondrial nitric oxide synthase. Trends Pharmacol Sci. 2005;26:190–5.
Ewere EG, Uka E, Usunobun U. Phytochemical composition, in vitro antioxidant activity and acute toxicity of Irvingia gabonensis (O’Rorke) Baill Ethanolic leaf extract. Int J Biomed Res. 2016b;4:36–41.
Weibrecht K, Dayno M, Darling C, Bird SB. Liver aminotransferases are elevated with rhabdomyolysis in the absence of significant liver injury. J Med Toxicol. 2010;6:294–300.
McGill MR. The past and present of serum aminotransferases and the future of liver injury biomarkers. EXCLI J. 2016;15:817–28.
Liu Z, Que S, Xu J, Peng T. Alanine aminotransferase-old biomarker and new concept: a review. Int J Med Sci. 2014;11:925–35.
Thapa BR, Walia A. Liver function tests and their interpretation. Indian J Pediatr. 2007;74:663–71.
Aras S, Gerin F, Aydin B, Ustunsoy S, Sener U, Turan BC et.al. Effects of sodium arsenite on some laboratory signs and therapeutic role of thymoquinone in the rats. Eur Rev Med Pharmacol Sci 2015; 19 Suppl 4: 658-663.
Bashandy SAE, Amin MM, Morsy FA. Spirulina platensis, reduced liver and kidney injuries induced by sodium arsenite. Int J PharmTech Res. 2018;11:35–48.
Rani K, Datt S, Rana R. Brief review on alkaline phosphatases-an overview. Int J Microbiol Bioinform. 2012;2:1–4.
Sharma U, Pal D, Prasad R. Alkaline phosphatase: an overview. Indian J Clin Biochem. 2014;29:269–78.
Epstein E, Kiechle FL, Artiss JD, Zak B. The clinical use of alkaline phosphatase enzymes. Clin Lab Med. 1986;6:491–505.
Bodansky O. Enzymes in cancer: the phosphohydrolases. In: Bodansky O, editor. Biochemistry of human cancer. New York: Academic Press; 1995.
Koenig G, Seneff S. Gamma-Glutamyltransferase: a predictive biomarker of cellular antioxidant inadequacy and disease risk. Dis Markers. 2015;2015:1–18.
Emdin M, Pompella A, Paolicchi A. Gamma-glutamyltransferase, atherosclerosis, and cardiovascular disease: triggering oxidative stress within the plaque. Circulation. 2005;112:2078–80.
Ludtke A, Genschel J, Brabant G, Bauditz J, Taupitz M, Koch M, et.al. Wermke W, Worman HJ and Schmidt HH. Hepatic steatosis in Dunnigan-type familial partial lipodystrophy. Am J Gastroenterol 2005; 100: 2218 -2224.
Gowda S, Desai PB, Hull VV, Math AAK, Vernekar SN, Kulkarni SS. A review on laboratory liver function tests. Pan African Med J. 2009;3:1–11.
Shi H, Shi X, Liu KJ. Oxidative mechanism of arsenic toxicity and carcinogenesis. Mol Cell Biochem. 2004;255:67–78.
Stohs SJ, Bagchi D. Oxidative mechanisms in the toxicity of metal ions. Free Radic Biol Med. 1995;18:321–36.
Waalkes MP, Liu J, Ward JM, Diwan LA. Mechanisms underlying arsenic carcinogenesis: hypersensitivity of mice exposed to inorganic arsenic during gestation. Toxicol Ind Health. 2004;198:31–8.
Ramanathan K, Balakumar BS, Panneerselvam C. Effects of ascorbic acid and alpha-tocopherol on arsenic-induced oxidative stress. Hum Exp Toxicol. 2002;21:675–80.
Amresh G, Rao CV, Singh PN. Antioxidant activity of Cissampelos pareira on benzo(a)pyrene-induced mucosal injury in mice. Nutr Res. 2007;27:625–32.
Manna P, Sinha M, Sil PC. A 43 kD protein isolated from the herb Cajanus indicus L attenuates sodium fluoride-induced hepatic and renal disorders in vivo. J Biochem Mol Biol. 2007;40:382–95.
Usoh IF, Akpan EJ, Etim OE, Farombi EO. Antioxidant actions of dried flower extracts of Hibiscus sabdariffa L. on sodium arsenite-induced oxidative stress in rats. Pak J Nutr. 2005;4:135–41.
Birben E, Sahiner UM, Sackesen C, Erzurum S, Kalayci O. Oxidative stress and antioxidant defense. WAO Journal. 2012;5:9–19.
Acknowledgements
Special thanks to Derindam Research Institute of Biotechnology, Akwa Ibom State, Nigeria for providing the laboratory space for this study.
Funding
This study was self-sponsored and received no funding whatsoever.
Author information
Authors and Affiliations
Contributions
EGE and NPO designed the study. EGE performed the statistical analysis and wrote the first draft of the manuscript. NPO supervised the study. EGE and SAO managed the analyses of the study. EGE managed experimental animal treatment and literature searches. JIN and NPO played major roles in writing the manuscript. GIE performed the histological assessments. All Authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent for publication
All authors hereby declare that the “Principles of laboratory animal care” (NIH publication No. 85–23, revised 1985) were followed as well as specific national laws, where applicable. All experiments were examined and approved by the appropriate Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
There are none.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ewere, E.G., Okolie, N.P., Ndem, J.I. et al. Irvingia gabonensis leaf extract scavenges nitric oxide and hydrogen peroxide in vitro and modulates arsenic-induced hepatic oxidative stress in wistar rats. Clin Phytosci 8, 15 (2022). https://doi.org/10.1186/s40816-022-00346-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40816-022-00346-z