Abstract
Background
Maintaining a healthy and diverse diet during pregnancy is crucial for maternal well-being and fetal development. The first trimester marks the beginning of vital developmental processes influenced by maternal nutritional status. Therefore, we aimed to determine dietary adequacy and diversity among first-trimester pregnant women.
Methods
In this cross-sectional study, we recruited 306 first-trimester pregnant women from the antenatal clinics of Aga Khan University Hospital, Karachi (January 2020 to September 2021). Eligible women possessed smartphones (for the mHealth intervention trial) and reported no major comorbidities or medication use. Data about socio-demographic, obstetric, and dietary history were collected through interviews using a structured questionnaire. Booking weight, height, blood pressure, and haemoglobin levels were extracted from medical records. An aggregate dietary risk score (DRS) was calculated separately for quantity and quality by summing the DRS for each of the six major food groups. A score of 0 was assigned to adequate, 1.5 to intermediate, and 3 to inadequate quantity or quality categories. Data were analysed using STATA 14.0.
Results
The mean ± SD for DRS quantity and quality were 10.6 ± 2.4 and 7.5 ± 2.5, respectively. Adequate dietary quantity and quality per week for starch-based food were reported by 14.4% and 21.2%, for vegetables by 0.3% and 49%, for fruits by 41.2% and 88.6%, for animal and plant protein by 19% and 0%, for milk and milk products by 1% and 37.6% and for oils and fats by 90.5% and 8.8%, respectively. Sweet and savoury snacks were eaten by 74.8% and 53.9%, respectively. Ready-made meals, carbonated beverages, packaged juices, and additional salt were consumed by 55.2%, 46.4%, 34.3%, and 7.5%, respectively. The median (IQR) water intake was 6 (4–8) glasses/day.
Conclusions
During the early stages of pregnancy, women enrolled for antenatal care at an urban private tertiary care hospital report inadequate dietary intake for various food groups, except for the quantity of oils/fats and the quality of fruit consumption. Poor dietary practices underscore the need for focused and impactful dietary counselling during the initial stages of pregnancy.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Pregnancy marks the critical period of accelerated physiological changes from conception until birth [1]. The first trimester is particularly significant, involving placental development, organogenesis, and maternal endocrine and metabolic systems’ adaptation for the subsequent trimesters. For clinicians and health care practitioners, it is the most accessible period for identifying suboptimal lifestyle behaviours, with the opportunity for early intervention [2].
One such behaviour is the dietary choices during pregnancy that significantly influence the in-utero environment, fetal metabolic programming, and growth trajectories. In particular, dietary intake during the first trimester may serve as a harbinger of dietary patterns throughout pregnancy. Adequate dietary intake involves both quantity and quality, ensuring sufficient intake of macronutrients and micronutrients and a variety of food choices to meet biological needs [3,4,5].
An adequate diet during pregnancy has been linked to favourable pregnancy outcomes [6, 7]. A diet rich in fruits and dairy products significantly reduces the risk of gestational diabetes mellitus (GDM) (aOR: 0.50, CI: 0.284–0.882) [8]. Additionally, eating fish, poultry, dairy products, unrefined grains, fruits, vegetables, legumes, and oils lowers the risk of preterm birth (RR: 0.10, CI: 0.01, 0.77) [9].
Conversely, a Western diet high in red and processed meat, processed grains, sugar, and fried items increases the risk of GDM (RR: 1.63, 95% CI: 1.20–2.21) [10]. Similarly, low adherence to the Mediterranean diet, comprising vegetables, fish, pulses, legumes, and vegetable oils, raises the risk of high systolic blood pressure early in pregnancy (β: 1.1, 95% CI: 0.2–2.2). This risk intensifies with high adherence to a traditional diet, including red meat and potatoes (β: 1.8, 95% CI: 0.7–2.9) [11]. Furthermore, inadequate dietary diversity is associated with an increased risk of low birth weight (LBW) (aRR: 6.4, 95% CI: 3.4, 12) and preterm birth (aRR: 6.3, 95% CI: 3.3, 11.95) [12].
Despite evidence suggesting the importance of a well-balanced diet during pregnancy, many women in low- and middle-income countries (LMICs), particularly in South Asia, face poor nutrition. Their diet often consists of staple foods, lacks diversity, and is nutritionally deficient [5, 13]. As these regions experience nutritional transition, demonstrated by a shift towards unhealthy dietary choices, a triple burden of malnutrition emerges.
A similar situation is observed in Pakistan, where a notable proportion of women of reproductive age (WRA) are underweight (14.5%), overweight (24%), or obese (14%) and only 27.6% meet the minimum dietary diversity. These nutritional indicators differ by the area of residence, with rural women (R) more underweight (R: 16% vs. U: 12.1%) and urban women (U) more overweight (R: 17.3% vs. U: 26.8%) or obese (R: 11.8% vs. U: 22.7%). Sindh Province, in particular, exhibits worse nutritional indicators, with 22.8% of women being underweight and only 16.5% achieving the minimum dietary diversity [14]. These conditions perpetuate an intergenerational cycle of malnutrition when undernourished women become pregnant.
In Pakistan, limited small-scale studies have examined dietary intake during pregnancy. A study conducted in Faisalabad revealed that 67.5% of pregnant women consumed balanced diets [15] and in Islamabad 89% achieved medium-level dietary diversity (scores of 5–7 out of 10) [16]. However, none of these studies explicitly studied the quantity and quality of each food group during the first trimester.
Addressing malnutrition, crucial for sustainable development goals (SDGs), demands a comprehensive approach. Many SDGs are intricately connected to the developmental origin of health and disease, emphasising how experiences during the first 1000 days profoundly shape future health risks [17].
Optimal nutrition from preconception is vital for ensuring a positive pregnancy experience. However, in Pakistan, where preconception care is uncommon, the first trimester becomes the closest point of contact to address dietary inadequacies through counselling. To our knowledge, limited studies have examined the dietary intake of pregnant women with minimal emphasis on the first trimester.
Therefore, in this study, we aimed to determine the dietary adequacy (quantity-consumption of adequate portions) and diversity (quality-inclusion of a variety of food items) among first-trimester pregnant women visiting a tertiary care hospital in Karachi.
Methods
Study design, setting, and population
A hospital-based cross-sectional study was conducted from January 13, 2020, to September 30, 2021, at the Aga Khan University Hospital (AKUH) in Karachi, Pakistan [18]. As the provincial capital of Sindh and the largest metropolis in Pakistan, Karachi is the commercial hub that accommodates migrants from across the country. AKUH is a private, not-for-profit tertiary care institution that is Joint Commission International Accredited and provides a comprehensive array of medical services to residents of Karachi and people from different parts of the country [19]. The hospital has various specialities, with trained and competent consultants who provide compassionate and quality care to patients for various diseases and conditions. The antenatal clinics at AKUH are run by trained obstetricians specialised in caring for normal and complicated pregnancies. An obstetrician sees 25 to 30 expectant women daily for consultations.
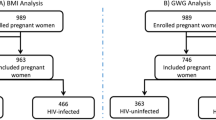
All pregnant women visiting the antenatal clinics at AKUH during the study duration were eligible for inclusion if they were at least 18 years old, in their first trimester, possessed a personal smartphone with an internet connection (for delivery of a mobile health intervention in the later stage of the study), and agreed to participate. Pregnant women who had comorbidities such as cardiovascular diseases, hypertension, diabetes, autoimmune disorders, kidney or liver diseases, were using medications regularly (antiplatelet aggregators, hypoglycaemic or antihypertensive drugs), and were unable to read and write due to language barriers were excluded. We initially approached 1955 pregnant women for the study; however, 1307 were excluded for various reasons as indicated in Fig. 1. Out of 648 eligible women, 342 did not consent to participate. Ultimately, 306 women were enrolled in the study (Fig. 1).
Sample size determination and sampling strategy
We calculated a sample size of 306 pregnant women using OpenEpi (version 3.01). The calculation was based on a minimum dietary diversity of 27.6% among WRA [14], an α error of 0.05, and a β error of 0.2, using the formula n = Z2 P (1-P)/d2, where ‘n’ is the sample size, ‘Z’ is the statistic corresponding to the level of confidence, ‘P’ is prevalence, and ‘d’ is precision [20].
Study participants were identified from the assessment rooms of the antenatal clinics using a purposive sampling strategy to ensure the recruitment of women meeting the eligibility criteria. The clinic list was reviewed a day before to identify the first-trimester pregnant women scheduled for the next day. Potential participants were approached for their written informed consent, and the study objectives were explained in detail to allow an informed decision. Women who agreed to participate were provided with a copy of informed consent.
Data collection tools and procedures
Through a comprehensive and structured questionnaire (supplementary file 1), we collected data about socio-demographic, obstetric, and dietary characteristics through face-to-face interviews. The socio-demographic information included age, ethnicity, religion, education, and occupation of women and spouses, monthly household income, family structure, house ownership, and household size. The obstetrics information comprised gravida, the experience of nausea, vomiting, and antiemetic use.
For dietary history, we developed a comprehensive food frequency questionnaire with relevance to the Pakistani context. We expanded the questionnaire used in the Smarter Pregnancy Program for Dutch pregnant women and couples contemplating pregnancy [21, 22] by incorporating additional questions about consuming locally available food items within appropriate food groups. Some examples of local food items include paratha (fried flatbread), dahi (yogurt), lassi (buttermilk), laal chawal (red rice), baajre ka aata (pearl millet flour), kaleji (liver), and makai (corn). We collected data about portions (< 1 to ≥ 5) and frequency of consumption over the past week (1 to 7 days) for the various food items, which were classified into the following food groups.
-
1.
Starch-based food (bread, chapatti, bun, naan, paratha, rice, pasta, cereal, corn, and potato).
-
2.
Animal and plant protein (fish, seafood, poultry, red and organ meat, liver, eggs, pulses, legumes, and beans).
-
3.
Vegetable (cooked, raw, fresh, and frozen).
-
4.
Fruit (fresh, dried, frozen, shakes, and fresh juices).
-
5.
Milk and milk products (milk, lassi, yogurt, milkshakes, custard, kheer).
-
6.
Oil and fats (cooking oil, ghee, butter, margarine).
For the oil and fats group, we calculated the monthly cooking oil consumption based on women’s average daily caloric requirement of 2300 calories during pregnancy [23]. Adequate quantity was determined using the guidelines that fats should constitute 30% of the total caloric intake [24], equivalent to 690 calories. Since each gram of fat contains 9 calories [25], 690 calories correspond to approximately 76.66 g of fat or approximately 80 ml. To account for fats from other sources, such as snacks or ready-made foods, we set a limit of 75 ml per day.
We also collected data on snacks, ready-made and homemade meals, beverages, additional salt use, water intake, and food allergies and avoidance. The questionnaire was pretested on 10% of the sample and modified as necessary. We obtained information about booking height, weight, blood pressure, and haemoglobin measurements from the medical records.
The study was implemented by a data collector with extensive experience in antenatal research, along with a doctoral student specializing in maternal nutrition and public health. The data collector was hired and extensively trained over five days to implement the questionnaire, followed by demonstrations, post-training evaluation, and quarterly refresher training. The face-to-face interviews were conducted by the data collector and a doctoral student in a quiet setting such as a treatment room or a secluded area within the clinic’s waiting room, to maintain privacy and confidentiality. Women were guided through each section of the questionnaire and provided assistance as needed. The dietary assessment inquired about the frequency of consumption of items within each food group over the past 7 days. If the response was affirmative, portion sizes ranging from < 1 to ≥ 5 portions per day were determined and recorded accordingly. This process was repeated for each food item across all food groups and for snacks and beverages as well. Women were given ample time to recall information accurately. To minimize recall limitation, a comprehensive list of potential food choices was provided for each food group, supplemented by open-ended questions for additional details. Furthermore, due to the subjective nature of dietary assessment, women were informed of the importance of reporting their actual consumption rather than what they believed should be consumed. Additionally, they were assured that all information provided would be kept confidential and treated without judgement. Model utensils, including plates, bowls, and cups, were utilized to illustrate portion sizes. On an average, the interviews lasted 25–30 min. The data collection initially planned for 6–8 months, was significantly delayed due to the Covid-19 pandemic causing a sharp decline in recruitment, which was stabilized after January 2021.
Data analysis
The data were entered and analysed using STATA version 14.0. Routine checks for completeness, clarity, and missing information were performed on-site. Based on the normality assessment, for quantitative variables such as age and blood pressure, we report the mean (SD) or medians and IQRs as appropriate. Monthly household income in PKR was categorised as less than 50,000, 50,000–99,999, 100,000–199,999 and 200,000 and above, and household size as ≤ 5 and > 5, respectively. For categorical variables such as ethnicity, religion, house ownership and family income, size and structure, frequency, and percentages are reported.
We assessed dietary quantity and quality using the dietary risk scores (DRS), which were calculated based on the World Health Organization’s (WHO) recommendations for healthy eating during pregnancy and lactation [26]. DRS is a composite score widely used to assess dietary inadequacies based on questions assessing portions and frequency of weekly consumption of items from the six major food groups. In our study, we extended the DRS in addition to fruit and vegetable intake to other main food groups (Table 1), following a similar approach as van Dijk et al., 2020. For each food group, women can score 0 (adequate), 1.5 (intermediate), or 3 (inadequate) separately for dietary quantity and quality [27]. The total score based on the sum of individual food group scores could range from 0 to 18, where 18 indicates an inadequate diet for all food groups.
Ethical considerations
The study was approved by the Ethics Review Committee of Aga Khan University (Reference Number 2021-5749-18595). Written informed consent was obtained from all participating women.
Results
Socio-demographic characteristics
The study included 306 pregnant women with a mean age of 28.4 years (range of 18–45 years). Most were Muslim (96.4%) and belonged to the Mohajir ethnicity (48%). A majority had attained university-level education, but only a third were employed. Most women lived in owned houses (72.9%) and in extended family arrangements (80.1%). Two-thirds of the sample reported their monthly household income, with over half earning less than 100,000 PKR. The minimum wage in Pakistan from 2019 to 2021 was 17,500 PKR per month [28]. Spouses generally had higher educational and employment statuses than women (Table 2).
Obstetric history and physical assessment
The gestational age of women ranged from 4.4 to 13.4 weeks. Our sample had slightly more multigravida women. Over half experienced nausea and vomiting, but only a third used antiemetics. Additionally, a greater proportion were obese. Blood pressure and haemoglobin levels were generally normal, however, one-fourth were anaemic (Table 3).
Dietary intake of pregnant women during the first trimester
The mean ± SD DRS for quantity and quality were 10.6 ± 2.4 and 7.5 ± 2.5, respectively. Oil and fats (90.5%) had the highest adequate intake, while vegetables and milk products were the lowest at 0.3% and 1%, respectively. Regarding dietary quality, 88.6% of the participants scored adequately for fruit, but none for animal and plant proteins (Fig. 2). Around 5.6% reported food allergies to meat, eggs, milk/cheese, nuts/peanuts, fruits, honey, and mushrooms, while 3.9% avoided meat, vegetables, fish/seafood, and milk in their diet. Most women ate three homemade meals daily, drank a median of six glasses of water, and a few used additional salt in their food.
Dietary intake of pregnant women for the six food groups
Starch-based food
White rice was the most consumed item, followed by whole wheat chapatti, potato, white bread/bun, and paratha. Most of these items were consumed once daily, except for paratha, which was usually eaten in at least four portions. Whole grain intake, apart from whole wheat chapatti, was very low (Table 4).
Fruit
Most women consumed fruits daily and half reported eating nuts and dried fruits regularly. Nearly half of the sample consumed fresh fruit juices and one-third had milkshakes up to twice a week, usually in a single portion (Table 4).
Vegetable
The habit of eating cooked vegetables was more common than that of raw vegetables. Most women ate no more than one portion daily (Table 4).
Animal and Plant Protein
Red meat, poultry, and eggs were the most consumed items from animal sources. Eggs were eaten daily by a higher proportion of women, while only a quarter consumed fish no more than twice a week. Plant-based sources such as pulses, legumes, and beans were consumed by most women, but not more than twice a week. Other food items, such as seafood, liver, and organ meat were less commonly eaten (Table 4).
Milk and milk product
Most women consumed milk more frequently than milk products, typically limiting their intake to one portion per day (Table 4).
Oil and Fats
Nearly all women used cooking oil, while a few used clarified butter (ghee). Canola was most common, followed by soybean, and olive oil. Mono-saturated fat consumption predominated.
Consumption of unhealthy food items: snacks, ready-made meals, and beverages
Over half of the sample consumed ready-made meals and snacks, with sweet snacks more common than savoury ones. Tea was the most consumed beverage, followed by carbonated drinks. One in three women reported consuming packaged juices (Table 5).
Discussion
This cross-sectional study provides a comprehensive snapshot of the dietary habits of first-trimester pregnant women attending a tertiary care hospital in Karachi, Pakistan. Our findings indicate that, on average, these women do not adhere to recommended dietary guidelines, leading to inadequate and imbalanced diets. Starch-based food, vegetables, animal and plant protein, and milk and milk products were insufficiently consumed, and dietary quality was inadequate for all food groups except fruits.
Starch-based food plays a crucial role in supporting maternal health and fetal development [26]; however, we found that only 14.4% of women met the recommended intake (≥ 6 portions). This finding is consistent with low compliance reported in studies from Thailand (13.2%) [30], Canada (8.6%) [31], and New Zealand (26%) [32]. In contrast, 98% of Indian pregnant women predominantly consumed starch-based foods [33]. Quality-wise, only 21% of women achieved an adequate score, including items like corn (16.3%), brown bread (14%), and brown rice (2.9%). We also observed excessive use of refined sources, in particular white rice (98%), white bread/bun (73.9%), paratha (60.5%), and noodles/pasta (46.1%), comparable to the study findings from Lahore [34].
Although whole grain consumption was similarly low in Singapore (29.6%) [35] and Iceland (14.9%) [36], recent research in rural Sindh found two-thirds of pregnant women mainly consumed brown rice or wheat-flour chapattis [37]. In Gujarat, India, commonly consumed sources included rice, sorghum, millet, wheat, and semolina [33], suggesting better choices, though processing details were not provided. The low whole grain intake may result from limited awareness of their health benefits [38], perceived higher cost, taste preferences, or family choices [39]. Nutrition counselling should promote adequate consumption and raise awareness about superior health benefits of whole grains in reducing pregnancy complications, obesity, excessive gestational weight gain (GWG), and constipation [1].
Being rich in essential vitamins, minerals, and dietary fibre, daily fruit consumption reduces the risk of adverse pregnancy outcomes [40]. While most women in our study (98.7%) consumed fruits regularly, only 41.2% met the recommended quantity (≥ 2 portions). Similar patterns were found in China (77.5%) [41], India (59%) [33], and the Netherlands (56.9% with DRS 0) [27]. In contrast, pregnant women in Southern India exceeded recommended fruit intake by threefold [42], while lower consumptions were observed in Nepal [43], Spain [44], Australia [45], and Canada [7]. Compared to pregnant women in rural Sindh (< 3%) [37] and Lahore (59%) [34], our sample had higher fruit intake and quality but also consumed more fruit juices (44.8% vs. 23%) [34]. Thus, nutrition counselling should encourage seasonal fruit and nut consumption while discouraging excessive fruit juice intake.
Vegetables are an essential part of a healthy diet to support normal physiological functions and prevent adverse outcomes during pregnancy [46]. We observed that 91.5% of women consumed vegetables weekly, higher than reported among pregnant women in Lahore (54%) [34]. However, only 0.3% met the recommended quantity (≥ 3 portions/day), and 49% met the recommended quality. These findings align with studies from India [47], Nepal [43], Bangladesh [48, 49], and rural Malawi [50]. In comparison, the Western population reported more vegetable consumption [27, 31]. In Pakistan, as observed in rural Sindh (1%) [37] and in Rawalpindi (2%) [51], vegetable consumption is extremely low. The inadequate vegetable intake may result from factors such as taste preferences, traditional beliefs favouring calorie-dense food, family customs prioritising other foods and limited awareness of the health benefits. Addressing these factors during antenatal care is important to promote recommended vegetable intake.
Similarly, protein is a major macronutrient required to support blood volume expansion, growth of maternal and fetal tissues, and placental development [52]. However, in our study, both the quantity (18.5%) and, notably, the quality (0%) of protein intake fell below the recommended levels. Similar findings are reported by Morton et al., where only 21% of women met the recommendations [32]. In contrast, higher than recommended protein intake was reported among first-trimester pregnant women in China [41, 53]. Regarding different protein sources, our study showed similar consumption of lentils/beans (81% vs. 84%) compared to Lahori pregnant women [34] but greater meat (90% vs. 75%), eggs (72% vs. 60% weekly; 30% vs. 4% daily) and fish (25% vs. 0%) consumption [34]. We also found a higher poultry intake (76.1%) compared to pregnant women in Rawalpindi (14%) [51]. Despite these improved dietary practices, women in our study did not meet adequate dietary quality requirements.
Furthermore, milk and dairy products are nutrient-rich sources, and their adequate intake during pregnancy improves fetal growth, development, and birth weight and size [54]. While over half of our sample consumed them weekly, only 1% met the recommended quantity, and 37.6% met the recommended quality. Our findings are consistent with previous studies from various countries, including China [41], Iran [55], India [56], Spain [57], LMICs [37], and Pakistan [34]. Conversely, in Gujarat, India, a higher proportion of pregnant women (82.6%) reported dairy consumption, but adequacy was not established [33]. A similar pattern of higher dairy intake during pregnancy compared to non-pregnant women was reported in Belgium [58] and New Zealand [32]. Insufficient dairy consumption may arise due to typical dietary patterns and poor recognition of its significance during pregnancy, hence requiring nutrition counselling to encourage adherence to recommended consumption.
Dietary fats, particularly polyunsaturated fatty acids (PUFAs), are important in supporting energy needs and promoting fetal development [59, 60]. Since the human body cannot synthesise PUFAs, their inclusion in the diet through sources such as fish is essential. Nutritionists also stress the significance of vegetable oils due to their rich content of beneficial fatty acids [61]. In our study, most women (90.52%) met the recommended quantity for oil and fats, but only 8.8% met the recommended quality. Monounsaturated fatty acids (MUFAs) were more commonly consumed (89.5%) than PUFAs, reporting similar patterns in India [62], Spain [57], and Belgium [58]. However, a Thai study found that 78% of pregnant women had inadequate fat intake [30].
In addition to major food groups, our study also evaluated the consumption of unhealthy dietary items. In this regard, we found consumption patterns similar to the Western world [32, 63], with comparable consumption of sweet (74.8% weekly; 10% daily) and savoury snacks (53.9% weekly; 8% daily) and carbonated beverages (Weekly 50%; 11.3% daily). However, we observed a higher intake of ready-made meals (55.2% weekly; 4% daily). Contrastingly, a Singaporean study involving different ethnicities showed reduced consumption of confectioneries during pregnancy [64].
In our study, women reported a median daily water intake of 6 glasses, comparable to Australian pregnant women [65] and higher than Chinese pregnant women [66]. Tea was more frequently consumed (61.4%) than coffee (6.5%) on most days, contrasting with Chinese data showing low tea consumption in the first trimester [67]. It is important to note that tea can reduce iron absorption, and a quarter of our participants were anaemic, emphasising the need for quality nutrition counselling to minimise absorption interference. Furthermore, only 3.9% of women reported food avoidance for religious and cultural reasons, much lower than reported in China (80%) [68], Tanzania (70.1%) [69], and other settings [58].
Strengths and limitations
This is one of the few studies in Pakistan to evaluate the dietary adequacy of pregnant women during the first trimester. We individually assessed both the quantity and quality of six major food groups, considering locally available and seasonal options. We developed a DRS using a comprehensive dietary algorithm, aligning with dietary guidelines, and gathered detailed insights into participants’ consumption patterns through open-ended questions.
However, the study has several limitations that need to be acknowledged. First, the cross-sectional study design limits tracking dietary inadequacies during preconception and provides a snapshot of dietary status at one point in time. Another limitation is related to the generalizability of the findings. Our sample was selective, comprising women with personal smartphones (for the planned RCT) who attended antenatal clinics at a private tertiary care hospital indicating a relatively better socio-economic standing than the general population, which might influence their dietary habits and access to healthcare resources. Despite the selective sample, we identified dietary inadequacies across major food groups, potentially suggesting significant deficiencies in pregnant women from impoverished backgrounds. Furthermore, we observed that a greater proportion of eligible women opted out of participating in the study, potentially leading to non-response bias, suggesting that their characteristics may differ from those of the respondents. Therefore, the results may not be representative of the broader population and should be interpreted within the context.
In addition, we anticipated recall bias concerning dietary information collected over the past one week. However, we minimized it by obtaining the data using an item checklist and included open-ended questions to capture any additional information. Further, due to cost and other constraints, we could not verify the dietary assessment through biochemical nutrient evaluation; although it is not possible to biochemically assess all nutrients. Lastly, seasonal variations could have impacted dietary quantity and diversity across the study participants, which we have not taken into account.
Implications
The findings of our study have several important implications. First, they reveal dietary inadequacies during the first trimester, indicating a need for targeted public health interventions early in pregnancy. Additionally, these findings relate to women from better socioeconomic backgrounds, implying the existence of potentially greater deficiencies among those from impoverished backgrounds. Hence, there is a need for widespread awareness campaigns and quality nutritional counselling as early as the first trimester. Secondly, there is a pressing need for nutritional guidelines specific to the Pakistani population, incorporating local food choices and tailored to context-specific dietary requirements for different stages of life including pregnancy. Further, innovative methods for monitoring dietary habits, providing repeated feedback and ensuring compliance with the recommendations should be explored and tested for effectiveness to ensure personalized and effective nutritional support during pregnancy.
Conclusion
Overall, first-trimester pregnant women consume an inadequate diet. Substantial inadequacies are evident in the amount and quality of starch-based food, animal and plant protein, and milk and milk products. Vegetable intake falls below the recommendations, while the quality of oils and fats is suboptimal. Addressing maternal malnutrition is critical to achieving SDG and promoting offspring’s growth and development during gestation and beyond. Hence, antenatal nutrition counselling in the first trimester should emphasise adequate and diverse choices from various food groups, which should be maintained throughout the subsequent trimesters. Additionally, potentially innovative and impactful approaches such as employing digital technology in creating awareness and promoting healthy dietary choices can be explored for personalised dietary counselling during the antenatal period.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AKUH:
-
Aga Khan University Hospital
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- DRS:
-
Dietary Risk Score
- GDM:
-
Gestational Diabetes Mellitus
- IQR:
-
Interquartile Range
- LBW:
-
Low birth weight
- LMICs:
-
Low-and Middle-Income Countries
- MUFAs:
-
Monounsaturated fatty acids
- PKR:
-
Pakistani Rupees
- PUFAs:
-
Polyunsaturated fatty acids
- SD:
-
Standard deviation
- SDGs:
-
Sustainable Development Goals
- WHO:
-
World Health Organization
- WRA:
-
Women of reproductive age
References
Mousa A, Naqash A, Lim S. Macronutrient and micronutrient intake during pregnancy: an overview of recent evidence. Nutrients. 2019;11(2):443. https://doi.org/10.3390/nu11020443.
Poon LC, McIntyre HD, Hyett JA, da Fonseca EB, Hod M. The first-trimester of pregnancy–A window of opportunity for prediction and prevention of pregnancy complications and future life. Diabetes Res Clin Pract. 2018;145:20–30. https://doi.org/10.1016/j.diabres.2018.05.002.
Castro-Quezada I, Román-Viñas B, Serra-Majem L. The Mediterranean diet and nutritional adequacy: a review. Nutrients. 2014;6(1):231–48. https://doi.org/10.3390/nu6010231.
Trijsburg L, Talsma EF, De Vries JH, Kennedy G, Kuijsten A, Brouwer ID. Diet quality indices for research in low-and middle-income countries: a systematic review. Nutr Rev. 2019;77(8):515–40. https://doi.org/10.1093/nutrit/nuz017.
Baxter JAB, Wasan Y, Islam M, Cousens S, Soofi SB, Ahmed I, et al. Dietary diversity and social determinants of nutrition among late adolescent girls in rural Pakistan. Matern Child Nutr. 2022;18(1):e13265. https://doi.org/10.1111/mcn.13265.
Emond JA, Karagas MR, Baker ER, Gilbert-Diamond D. Better diet quality during pregnancy is associated with a reduced likelihood of an infant born small for gestational age: an analysis of the prospective new hampshire birth cohort study. J Nutr. 2018;148(1):22–30. https://doi.org/10.1093/jn/nxx005.
Savard C, Lemieux S, Carbonneau É, Provencher V, Gagnon C, Robitaille J, et al. Trimester-specific assessment of diet quality in a sample of canadian pregnant women. Int J Environ Res Public Health. 2019;16(3):311. https://doi.org/10.3390/ijerph16030311.
Roustazadeh A, Mir H, Jafarirad S, Mogharab F, Hosseini SA, Abdoli A, et al. A dietary pattern rich in fruits and dairy products is inversely associated to gestational diabetes: a case-control study in Iran. BMC Endocr Disord. 2021;21(1):1–9. https://doi.org/10.1186/s12902-021-00707-8.
Khoury J, Henriksen T, Christophersen B, Tonstad S. Effect of a cholesterol-lowering diet on maternal, cord, and neonatal lipids, and pregnancy outcome: a randomized clinical trial. Am J Obstet Gynecol. 2005;193(4):1292–301. https://doi.org/10.1016/j.ajog.2005.05.016.
Schoenaker DA, Mishra GD, Callaway LK, Soedamah-Muthu SS. The role of energy, nutrients, foods, and dietary patterns in the development of gestational diabetes mellitus: a systematic review of observational studies. Diabetes Care. 2016;39(1):16–23. https://doi.org/10.2337/dc15-0540.
Timmermans S, Steegers-Theunissen RP, Vujkovic M, Bakker R, den Breeijen H, Raat H, et al. Major dietary patterns and blood pressure patterns during pregnancy: the Generation R Study. Am J Obstet Gynecol. 2011;205(4):337. e1-12. https://doi.org/10.1016/j.ajog.2011.05.013.
Wondemagegn AT, Tsehay B, Lake A, Negesse A. Effects of dietary diversification during pregnancy on birth outcomes in east Gojjam, northwest Ethiopia: a prospective cohort study. Front Public Health. 2022:4596. https://doi.org/10.3389/fpubh.2022.1037714.
Khan A, Shaheen MA, Knight F, Baldi G. Filling the nutrient gap in Pakistan: insights to address malnutrition. Nutr Exch. 2017;8:17.
UNICEF. Pakistan National Nutrition Survey 2018: volume 1. Islamabad, Pakistan: UNICEF; 2018.
Batool Z, Zafar MI, Anwar S, Bano S, Gul M, Nazir F. An investigation into socio-economic factors explaining dietary intake in pregnant women: a study in urban areas of District Faisalabad, Punjab, Pakistan. Pak J Nutr. 2012;11(7):568. https://doi.org/10.3923/pjn.2012.666.671.
Ali F, Thaver I, Khan SA. Assessment of dietary diversity and nutritional status of pregnant women in Islamabad, Pakistan. J Ayub Med Coll Abbottabad. 2014;26(4):506–9.
Likhar A, Patil MS. Importance of maternal nutrition in the first 1,000 days of life and its effects on child development: a narrative review. Cureus. 2022;14(10). https://doi.org/10.7759/cureus.30083.
Nuruddin R, Vadsaria K, Mohammed N, Sayani S. The efficacy of a personalized mHealth coaching program during pregnancy on maternal diet, supplement use, and physical activity: protocol for a parallel-group randomized controlled trial. JMIR Res Protoc. 2021;10(11):e31611. https://doi.org/10.2196/31611.
Hospital AKU. The Aga Khan University Hospital, main campus, Karachi . 2023. https://hospitals.aku.edu/pakistan/karachi/pages/default.aspx
Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol bed Bench. 2013;6(1):14–17.
van Dijk MR, Oostingh EC, Koster MP, Willemsen SP, Laven JS, Steegers-Theunissen RP. The use of the mHealth program smarter pregnancy in preconception care: rationale, study design and data collection of a randomized controlled trial. BMC Pregnancy Childbirth. 2017;17:1–7. https://doi.org/10.1186/s12884-017-1228-5.
MC E. Smarter Pregnancy: For couples who are or wish to get pregnant. Rotterdam: Mijn Leefstijlzorg - Erasmus MC; 2019. https://www.mijnleefstijlzorg.nl/smarterpregnancy/.
Kominiarek MA, Rajan P. Nutrition recommendations in pregnancy and lactation. Med Clin. 2016;100(6):1199–215. https://doi.org/10.1016/j.mcna.2016.06.004.
Leyvraz M, Neufeld LM. Nutrient requirements and recommendations during pregnancy. The biology of the first 1,000 days. CRC; 2017. pp. 35–52. https://doi.org/10.1201/9781315152950-4.
FAO G. Pakistan dietary guidelines for better nutrition. Food and Agriculture Organization of the United Nations and Ministry of Planning Development and Reform, Government of Pakistan. 2018.
Organization WH. Healthy eating during pregnancy and breastfeeding: booklet for mothers. Copenhagen: WHO Regional Office for Europe; 2001.
van Dijk MR, Koster MP, Oostingh EC, Willemsen SP, Steegers EA, Steegers-Theunissen RP. A mobile app lifestyle intervention to improve healthy nutrition in women before and during early pregnancy: single-center randomized controlled trial. J Med Internet Res. 2020;22(5):e15773. https://doi.org/10.2196/15773.
WageIndicator. Minimum wage – Sindh Pakistan. 2024. https://paycheck.pk/salary/minimum-wages.
Girdhar S, Sharma S, Chaudhary A, Bansal P, Satija M. An epidemiological study of overweight and obesity among women in an urban area of North India. Indian J Community Med. 2016;41(2):154-7. https://doi.org/10.4103/0970-0218.173492.
Sukchan P, Liabsuetrakul T, Chongsuvivatwong V, Songwathana P, Sornsrivichai V, Kuning M. Inadequacy of nutrients intake among pregnant women in the deep south of Thailand. BMC Public Health. 2010;10:1–8. https://doi.org/10.1186/1471-2458-10-572.
Fowler JK, Evers SE, Campbell MK. Inadequate dietary intakes: among pregnant women. Can J Diet Pract Res. 2012;73(2):72–7. https://doi.org/10.3148/73.2.2012.72.
Morton SM, Grant CC, Wall CR, Carr PEA, Bandara DK, Schmidt JM, et al. Adherence to nutritional guidelines in pregnancy: evidence from the growing up in New Zealand birth cohort study. Public Health Nutr. 2014;17(9):1919–29. https://doi.org/10.1017/S1368980014000482.
Umallawala TM, Shah P, Puwar T, Saha S, Pandya A, Wanjari MB et al. Food consumption pattern and dietary diversity among pregnant and lactating women, children, and adolescent girls in Devbhumi Dwarka District, Gujarat: a cross-sectional study. Cureus. 2022;14(8). https://doi.org/10.7759/cureus.28168.
Saeed A, Humayun A, Raana T. Maternal dietary intake and its associated socio demographic factors: evidence from Lahore, Pakistan. Prog Nutr. 2018;20:345–51. https://doi.org/10.23751/pn.v20i1-S.5577.
Ross AB, Colega MT, Lim AL, Silva-Zolezzi I, Mace K, Saw SM, et al. Whole grain intake, determined by dietary records and plasma alkylresorcinol concentrations, is low among pregnant women in Singapore. Asia Pac J Clin Nutr. 2015;24(4):674–82. https://doi.org/10.6133/apjcn.2015.24.4.19.
Tryggvadottir EA, Halldorsson TI, Landberg R, Hrolfsdottir L, Birgisdottir BE, Magnusdottir OK, et al. Higher Alkylresorcinol concentrations, a consequence of whole-grain intake, are inversely associated with gestational diabetes mellitus in Iceland. J Nutr. 2021;151(5):1159–66. https://doi.org/10.1093/jn/nxaa449.
Lander RL, Hambidge KM, Westcott JE, Tejeda G, Diba TS, Mastiholi SC, et al. Pregnant women in four low-middle income countries have a high prevalence of inadequate dietary intakes that are improved by dietary diversity. Nutrients. 2019;11(7):1560. https://doi.org/10.3390/nu11071560.
Lang R, Jebb SA. Who consumes whole grains, and how much? Proc Nutr Soc. 2003;62(1):123–7. https://doi.org/10.1079/pns2002219.
McMackin E, Dean M, Woodside JV, McKinley MC. Whole grains and health: attitudes to whole grains against a prevailing background of increased marketing and promotion. Public Health Nutr. 2013;16(4):743–51. https://doi.org/10.1017/S1368980012003205.
Yonezawa Y, Obara T, Yamashita T, Sugawara J, Ishikuro M, Murakami K, et al. Fruit and vegetable consumption before and during pregnancy and birth weight of new-borns in Japan: the Tohoku medical megabank project birth and three-generation cohort study. Nutr J. 2020;19(1):1–11. https://doi.org/10.1186/s12937-020-00595-z.
Yang W, Han N, Jiao M, Chang X, Liu J, Zhou Q, et al. Maternal diet quality during pregnancy and its influence on low birth weight and small for gestational age: a birth cohort in Beijing, China. Br J Nutr. 2023;129(8):1360–9. https://doi.org/10.1017/S0007114522000708.
Andersen LT, Thilsted SH, Nielsen BB, Rangasamy S. Food and nutrient intakes among pregnant women in rural Tamil Nadu, South India. Public Health Nutr. 2003;6(2):131–7. https://doi.org/10.1079/PHN2002367.
Acharya O, Zotor FB, Chaudhary P, Deepak K, Amuna P, Ellahi B. Maternal nutritional status, food intake and pregnancy weight gain in Nepal. J Health Manage. 2016;18(1):1–12. https://doi.org/10.1177/0972063415625537.
Jardí C, Aparicio E, Bedmar C, Aranda N, Abajo S, March G, et al. Food consumption during pregnancy and post-partum. ECLIPSES study. Nutrients. 2019;11(10):2447. https://doi.org/10.3390/nu11102447.
Wen LM, Flood VM, Simpson JM, Rissel C, Baur LA. Dietary behaviours during pregnancy: findings from first-time mothers in southwest Sydney, Australia. Int J Behav Nutr Phys Act. 2010;7:1–7. https://doi.org/10.1186/1479-5868-7-13.
Marshall NE, Abrams B, Barbour LA, Catalano P, Christian P, Friedman JE, et al. The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obstet Gynecol. 2022;226(5):607–32. https://doi.org/10.1016/j.ajog.2021.12.035.
Panwar B, Punia D. Food intake of rural pregnant women of Haryana State, northern India: relationship with education and income. Int J Food Sci Nutr. 1998;49(3):243–7. https://doi.org/10.3109/09637489809086418.
Shamim AA, Mashreky SR, Ferdous T, Tegenfeldt K, Roy S, Rahman AF, et al. Pregnant women diet quality and its sociodemographic determinants in southwestern Bangladesh. FoodNutr Bull. 2016;37(1):14–26. https://doi.org/10.1177/0379572116632137.
Mridha MK, Matias SL, Arnold CD, Dewey KG. Factors associated with nutritional status and dietary practices of Bangladeshi adolescents in early pregnancy. Ann N Y Acad Sci. 2018;1416(1):66–76. https://doi.org/10.1111/nyas.13568.
Hjertholm KG, Iversen PO, Holmboe-Ottesen G, Mdala I, Munthali A, Maleta K, et al. Maternal dietary intake during pregnancy and its association to birth size in rural Malawi: a cross‐sectional study. Matern Child Nutr. 2018;14(1):e12433. https://doi.org/10.1111/mcn.12433.
Qureshi Z, Khan R. Dietary intake trends among pregnant women in rural area of Rawalpindi, Pakistan. J Ayub Med Coll Abbottabad. 2015;27(3):684–8.
Elango R, Ball RO. Protein and amino acid requirements during pregnancy. Adv Nutr. 2016;7(4):S839–44. https://doi.org/10.3945/an.115.011817.
Yang J, Dang S, Cheng Y, Qiu H, Mi B, Jiang Y, et al. Dietary intakes and dietary patterns among pregnant women in Northwest China. Public Health Nutr. 2017;20(2):282–93. https://doi.org/10.1017/S1368980016002159.
Achón M, Úbeda N, García-González Á, Partearroyo T, Varela-Moreiras G. Effects of milk and dairy product consumption on pregnancy and lactation outcomes: a systematic review. Adv Nutr. 2019;10(suppl2):S74–87. https://doi.org/10.1093/advances/nmz009.
Karandish M, Mohammadpour-Ahranjani B, Rashidi A, Maddah M, Vafa M-R, Neyestani T-R. Inadequate intake of calcium and dairy products among pregnant women in Ahwaz City, Iran. Malays J Nutr. 2005;11(2):111–20.
Agrahar-Murugkar D, Pal P. Intake of nutrients and food sources of nutrients among the Khasi tribal women of India. Nutrition. 2004;20(3):268–73. https://doi.org/10.1016/j.nut.2003.11.008.
Rocamora Irles JA, Bravo Iglesias EM, Mejías Avilés S, López Bernal E, Valle Galindo BdP, López Moriones L, et al. Nutritional value of the diet in healthy pregnant women. Results of a nutrition survey of pregnant women. Nutr Hosp. 2003;18(5):248–52
Verbeke W, De Bourdeaudhuij I. Dietary behaviour of pregnant versus non-pregnant women. Appetite. 2007;48(1):78–86. https://doi.org/10.1016/j.appet.2006.07.078.
Mani I, Dwarkanath P, Thomas T, Thomas A, Kurpad AV. Maternal fat and fatty acid intake and birth outcomes in a south Indian population. Int J Epidemiol. 2016;45(2):523–31. https://doi.org/10.1093/ije/dyw010.
Laitinen K. Fat requirements in pregnancy and infancy; 2021. https://doi.org/10.1039/9781839165078-00001.
Orsavova J, Misurcova L, Ambrozova JV, Vicha R, Mlcek J. Fatty acids composition of vegetable oils and its contribution to dietary energy intake and dependence of cardiovascular mortality on dietary intake of fatty acids. Int J Mol Sci. 2015;16(6):12871–90. https://doi.org/10.3390/ijms160612871.
Jood S, Bishnoi S, Khetarpaul N. Nutritional status of rural pregnant women of Haryana State, Northern India. Nutr Health. 2002;16(2):121–31. https://doi.org/10.1177/026010600201600206.
Dominguez LJ, Martinez-Gonzalez MA, Basterra-Gortari FJ, Gea A, Barbagallo M, Bes-Rastrollo M. Fast food consumption and gestational diabetes incidence in the SUN project. PLoS ONE. 2014;9(9):e106627. https://doi.org/10.1371/journal.pone.0106627.
Chen L-W, Low YL, Fok D, Han WM, Chong YS, Gluckman P, et al. Dietary changes during pregnancy and the postpartum period in Singaporean Chinese, malay and Indian women: the GUSTO birth cohort study. Public Health Nutr. 2014;17(9):1930–8. https://doi.org/10.1017/S1368980013001730.
Wen LM, Flood VM, Simpson JM, Rissel C, Baur LA. Dietary behaviours during pregnancy: findings from first-time mothers in southwest Sydney, Australia. Int J Behav Nutr Phys Activity. 2010;7:1–7. https://doi.org/10.1186/1479-5868-7-13.
Zhou Y, Zhu X, Qin Y, Li Y, Zhang M, Liu W, et al. Association between total water intake and dietary intake of pregnant and breastfeeding women in China: a cross-sectional survey. BMC Pregnancy Childbirth. 2019;19:1–10. https://doi.org/10.1186/s12884-019-2301-z.
Lu JH, He JR, Shen SY, Wei XL, Chen NN, Yuan MY, et al. Does tea consumption during early pregnancy have an adverse effect on birth outcomes? Birth. 2017;44(3):281–9. https://doi.org/10.1111/birt.12285.
Gao H, Stiller CK, Scherbaum V, Biesalski HK, Wang Q, Hormann E, et al. Dietary intake and food habits of pregnant women residing in urban and rural areas of Deyang City, Sichuan Province, China. Nutrients. 2013;5(8):2933–54. https://doi.org/10.3390/nu5082933.
Myaruhucha C. Food cravings, aversions and pica among pregnant women in Dar Es Salaam, Tanzania. Tanzan J Health Res. 2009;11(1).
Acknowledgements
We acknowledge the support from the Department of Obstetrics and Gynaecology, Aga Khan University, the data collector, and the study participants. We also acknowledge Mr. Iqbal Azam for his advice on data analysis.
Funding
Funding for the study was received from the University Research Council of Aga Khan University, Grant Number 164003CHS.
Author information
Authors and Affiliations
Contributions
Study was conceptualised by RN, KV and NM. The study methodology was developed by RN., KV and SA. The study implementation on field and data management and analysis were performed by KV under the supervision of RN. The initial and revised manuscript drafts were prepared by KV and critically reviewed and edited by RN and NM. The study funding was acquired by RN and NM. RN provided supervision for all aspects of the study. All the authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Ethics Review Committee of Aga Khan University. Written informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vadsaria, K., Mohammed, N., Aamir, S. et al. Are first-trimester pregnant women consuming adequate and diverse diet? A hospital-based cross-sectional study in Karachi, Pakistan. BMC Nutr 10, 104 (2024). https://doi.org/10.1186/s40795-024-00912-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-024-00912-3