Abstract
Background
There was a wider disparity in the diet characterization among most studies on diet and pregnancy outcomes in different countries, and the research in northern China is limited. Therefore, the purpose of the present study that was conducted in northwest China was to understand the dietary characteristics of periconceptional women and to explore the relationship between and specific dietary patterns with adverse pregnancy outcomes.
Methods
A nested case-control study was conducted from October 2017 to November 2018 in Shaanxi, China. Based on a prospective cohort of 368 women who were pregnant or prepared for pregnancy, 63 participants who developed the outcomes of gestational hypertension, gestational diabetes, preterm birth, low birth weight, and birth defects were included in the case group. A total of 237 healthy pregnant women were included during the same period in the control group. Dietary intake was assessed using a validated food frequency questionnaire for the three months before pregnancy and the first trimester. Information on delivery details and antenatal pregnancy complications was obtained from the hospital maternity records. Dietary patterns were derived using factor analysis. Stratified analysis was performed on the overall, single and multiple adverse pregnancy outcomes categories. Adjustment was made for sociodemographic characteristics and nutritional supplement status.
Results
Six major dietary patterns were identified. The ‘starchy’ dietary pattern, composed of high intake in noodle and flour products and/or rice and its products, was associated with the odds of developing of adverse pregnancy outcomes (OR: 2.324, 95% CI: 1.293–4.178). This risk remained significant following adjustment for potential confounders of maternal demographic characteristics and nutritional status (aOR: 2.337, 95% CI:1.253–4.331). Strong association were found during the first trimester of pregnancy, but showed no association during the three months before pregnancy (aOR:1.473, 95% CI: 0.682–3.234).
Conclusions
High starchy food intake was associated with adverse pregnancy outcomes, particularly during the first trimester of pregnancy. Health education focusing on periconceptional dietary patterns could be a practical strategy for preventing adverse pregnancy outcomes.
Similar content being viewed by others
Introduction
Recent epidemiological evidence of an association between poor fetal growth and adult disease highlights the need to reconsider the influences which act on the fetus, and the role maternal nutrition may play [1]. From a prevention perspective, epidemiological research into the relationship between diet and pregnancy outcomes is essential. The use of dietary patterns is considered an estimation of the overall dietary habits of a subject and has become widespread in nutrition research as an alternative approach to study individual components of the diet [2,3,4,5,6,7]. The investigation of the association between different dietary structures and pregnancy outcomes has shown that specific dietary constituents can exert high risk or protection with regard to preterm birth [2, 3], shorter birth length [2], hypertensive disorders in pregnancy (HDP) [4], gestational diabetes mellitus (GDM) [5, 6] and small for gestational age infants (SGA) [7]. However, most of the results of these studies are inconsistent because of the cultural differences among various geographical regions and countries result in distinct dietary sources. There was a wider disparity in the diet characterization among most studies on diet and pregnancy outcomes in different countries [8]. For example, Chinese traditional staple foods are mainly rice and flour products based starchy foods. Although the components of starchy foods are included in some specific dietary patterns in some researches, the extraction of starchy foods with proven healthy foods such as vegetables/fruits [9,10,11], or with proven non-healthy foods such as fat /deep fried food [12] as a dietary structure may mask or exaggerate their effect. It raises the need for additional studies on specific dietary patterns to provide evidence on potentially preventative interventions to reduce the burden of adverse pregnancy outcomes.
Concomitantly, dietary patterns and adverse pregnancy outcomes are also associated with sociodemographic characteristics, such as family income, urbanization, and individual education [13, 14]. However, at present, the associations between the periconceptional dietary structure and adverse pregnancy outcomes in northern China have not been examined in detail. Also, there is a close relationship between periconceptional nutritional supplementation and pregnancy outcomes [15], but this important confounding factor is still often ignored in many studies.
We therefore analyzed the observational data collected for a nested case-control study in the northwest of China, to understand the dietary characteristics of periconceptional women and to explore the relationship between specific dietary pattern and adverse pregnancy outcomes based on the adjustment of nutrient intake and other important confounding factors.
Material and methods
Study population
We conducted a case-control study nested in a cohort. The cohort conducted from October 2017 in the First Affiliated Hospital of the Xi’an Jiaotong University, which encompassed a population of 368, to evaluate the associations between maternal environmental exposure during the periconceptional period and the cognitive development of offspring. The subjects were randomly selected from the women who were admitted to the hospital for pre-pregnancy examination or those who were already pregnant and within their 13+ 6 weeks’ gestation period. The medical record number, telephone number and home address of each participant were recorded at the time of recruitment to facilitate follow-up.
Case control selection
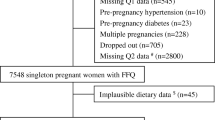
The nested case-control was conducted on the impact of periconceptional dietary patterns on adverse pregnancy outcomes between October 2017 to November 2018. We excluded women who were not pregnant within three months (n = 21), women with abnormal pre-pregnancy examinations(n = 23), including gynecological inflammation, polycystic ovaries, tumors, anemia, hypertension, diabetes, and metabolic diseases, such as thyroid dysfunction. In addition, women with a history of genetic defects in birth (n = 1) and women who had been pregnant through assisted reproduction were also excluded (n = 1). The follow-up method was mainly used to track the prenatal and postnatal examination results recorded by the hospital maternity records, and the women who were transferred to other hospitals were followed-up by phone. During follow-up, subjects with the following five adverse outcomes that most common in northwest China [16] were included in the case group: gestational hypertension, gestational diabetes, preterm birth, low birth weight and birth defects. After excluding subjects who were stillborn and other outcomes (n = 6), lost to follow-up (n = 11) and nonresponse (n = 5) during the investigation, 63 participants were included in the case group. The remaining 237 healthy pregnant women recruited in the same period were included in the control group. The ratio between the case and the control groups was approximately 1:4. The women in the case group were divided into single and multiple adverse pregnancy outcome subgroups according to whether they had two or more adverse pregnancy outcomes. (Additional file 2: Fig. S1).
The blood pressure of pregnant women was monitored and recorded in each regular prenatal examination. The gestational hypertension was defined a systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg on two occasions 4 h apart, developing after 20 weeks of gestation in a previously normotensive case in the absence of significant proteinuria [17]. Gestational diabetes was defined by the following cutoff endpoints according to the Chinese guidelines on obstetrics and gynecology: fasting plasma glucose concentration ≥ 5.1 mmol/l, and a plasma glucose concentration at 1 and 2 h after oral administration of 75 g oral glucose that was ≥10.0 mmol/l and ≥ 8.5 mmol/l, as determined by the oral glucose tolerance test (OGTT) instructions [18]. The results of the screening method for gestational diabetes were followed up after the 24 to 28 weeks’ period of prenatal examination. Preterm birth was defined as delivery between 28 and 37 weeks of pregnancy. Low birth weight was defined as a neonate weighing less than 2500 g within 72 h of birth. Birth defects refer to the physical structure and function abnormalities that occur before birth, including congenital malformations, chromosomal abnormalities, genetic metabolic diseases and functional abnormalities.
Exposure assessment
Dietary information was collected at baseline through a 19-item validated food-frequency questionnaire (FFQ), these have been shown to represent the daily diet of Chinese women adequately [19] (details see Additional file 1). All participants were investigated and questioned twice by trained investigators via face-to-face interviews when they are recruited (collected the information during three months before pregnancy) and during their 13–16+ 6 weeks’ prenatal examination (collected the information during the first trimester of pregnancy). The FFQ included noodles and flour products, rice and their products, fruits and vegetables, meat, dairy products, beverages and fried food. For the majority of the food types, the participants provided information concerning how often they were consuming each food type according to the three months before pregnancy and the first trimester of gestation. The following options were used: 1) more than once a day; 2) 3–6 times a week; 3) 1–2 times a week; 4) 2–3 times a month; 5) less than once a month and 6) never or rarely.
Covariate assessment
The baseline questionnaire inquired information about socio-demographic (age, residence, economic situation, occupation, education), smoking, alcohol intake and nutrient supplementation variables. The survey of nutrient supplementation was conducted at the same time as the dietary intake survey, that mainly included the types of nutrient and the supplemental dosage and duration during the three months before pregnancy and/or the first trimester of pregnancy, respectively. According to the type of nutrients that pregnant women consumed in addition to folic acid, they were divided into groups that received pure folic acid tablets, multivitamin tablets containing folic acid and other vitamins. The supplement dose was defined as a large dose supplement and a small dose supplement depending on whether the daily dose of folic acid was more than 0.4 mg. Similarly, the supplement dose was defined as long-term and short-term supplementation according to whether the duration of nutrient supplementation exceeded 90 days. In addition, we also recorded the pre-pregnancy BMI of pregnant women to assess their basic preliminary nutritional status, and we defined specific BMI levels of < 18.5 kg/m2, 18.5 kg/m2 to 24.0 kg/m2 and > 24.0 kg/m2 as emaciation, normal and overweight and obesity, respectively.
Statistical analysis
All data were coded and assigned the following data cleaning and quality check. Epidata3.1 was used for data entry and logic error detection. Quantitative data were described as mean ± standard deviation and categorical data were presented by the composition ratio.
In order to describe the dietary patterns of the subjects, factor analysis with varimax rotation was performed to calculate the components on the 19 standardized food items. This analysis was based on the principal component method. The number of components that described this information was selected on the basts of the screen plot and the interpretability of the factor loading [20]. Food items with factor loading (absolute value) above 0.3 on a component were considered to have a significant association with that component. The explained variance for the individual components was subjected to rotation redistribution to achieve a simpler structure. The factor scores were computed for each woman by summing the food items consumed according to their factor loadings. According to the quartile of factor score, the 1st and 4th were divided into low intake and high intake subgroups.
The associations [odds ratios (ORs) and 95% confidence intervals (CIs)] between maternal dietary patterns and nutritional status, and adverse pregnancy outcomes were examined by logistic regression analysis. Possible confounding factors that were suggested by sociodemographic characteristics and nutritional supplement status were included as covariates in the multivariate logistic regression analysis for the dietary patterns. In addition, all analyses were stratified by overall, single, and multiple adverse pregnancy outcome subgroups.
All data were analyzed by the SPSS 18.0 software and the effect estimates were considered to be significant if the p-value was < 0.05.
Results
A total of 300 pregnant women were included in the nested case-control study, with an average age of 29.75 ± 3.854 years. These were divided to 237 in the control group and 63 in the case group. Of the 63 patients in the case group, 35 (55.6%) women were single adverse pregnancy outcome, and 28 (44.4%) women were multiple adverse pregnancy outcomes (two or more).
Association between sociodemographic characteristics and adverse pregnancy outcomes
The noted covariates of sociodemographic characteristics were age and residence, economic situation, smoking and alcohol intake (Table 1). From Table 2, we found that the risk of adverse pregnancy outcomes in subjects with age higher than 35 years old and was significantly increased (OR: 4.228, 95% CI: 1.762–10.149). In addition, the women who lived in the countryside (OR: 2.467, 95% CI: 1.025–5.937), and with a history of alcohol intake (OR: 6.724, 95% CI: 1.562–28.952) and smoking (OR: 62.142, 95% CI: 8.931–432.397) during the periconceptional pregnancy were also associated with increased risk of adverse pregnancy outcomes. Following multivariate analysis, only maternal age, smoking and alcohol intake were significantly associated with adverse pregnancy outcomes.
Association between nutritional status and adverse pregnancy outcomes
From Table 3, the noted covariates were pre-pregnancy BMI and the nutrient supplementation during the first trimester. It can be deduced that pre-pregnancy overweight or obesity were significantly associated with adverse pregnancy outcomes (OR: 2.927, 95% CI: 1.534–5.587). Positive associations were also noted between pregnant women with short-term and low dose nutrient supplementation and adverse pregnancy outcomes, particularly during the first trimester of pregnancy (OR: 2.885, 95% CI: 1.262–6.593). The results from the adjusted model indicated that only pre-pregnancy BMI was noted, whereas the adjusted OR values decreased slightly to 2.412 (95% CI: 1.143–5.089).
Dietary pattern identification
The KMO and Bartlett sphere tests were performed for the dietary frequencies of 19 food items during the three months before pregnancy and first trimester of pregnancy, and the statistics were 0.707 and 0.680, respectively. The Bartlett’s spherical test suggested a nonvalid independent hypothesis test. Six dietary patterns were selected to best describe the dietary patterns of the women after factor analysis. The variability of these patterns for the period of three months before pregnancy and the first trimester of pregnancy was estimated to 53.690 and 54.273%, respectively as determined by these six patterns.
The factor loadings obtained from the factor analysis are shown in Additional file 3: Table S1 and Additional file 4: Table S2. The first pattern was described as ‘animal protein’ due to the high loadings of poultry, beef and mutton, fish and shrimp, and pork. The second pattern yielded a dietary pattern high in the consumption of green tea, coffee and cola, which was denoted as ‘caffeine’. The third pattern was characterized by high intake of food with high-quality protein contents such as beans and their products, milk and its products, nuts and eggs, and was therefore classified as ‘healthy’. The fourth pattern was labeled ‘processed’ as the predominant foods with high loadings were processed or high-fat foods, such as pickles/sauerkraut, fried food, animal organs and garlic. The fifth pattern with high loadings was composed of noodle and flour products, rice and its products, and was thus labeled ‘starchy’. Finally, the sixth ‘vegetarian’ pattern comprised high contents of fresh vegetables and fruits.
Association between dietary patterns and adverse pregnancy outcomes
Univariate analysis (Additional file 5: Table S3) demonstrated that the pregnant women in the case group exhibited more ‘caffeine’ and ‘starchy’ food diets in the three months before pregnancy and more ‘animal protein’ and ‘starchy’ diets in the first trimester of pregnancy. Among them, the high intake of ‘starchy’ foods in early pregnancy significantly increased the risk of overall adverse pregnancy outcomes (OR: 2.324, 95% CI: 1.293–4.178) and the risk of single adverse pregnancy outcomes (OR: 3.307, 95% CI: 1.479–7.395). After adjusting noted covariates that were suggested by sociodemographic characteristics and nutritional supplement status, the multivariate analysis did not alter the significant association between the high intake of ‘starchy’ foods with the overall and single adverse pregnancy outcomes. The increased OR rates of 2.337(95% CI:1.253–4.331) and 3.321 (95% CI:1.373–7.250) were retained for both of these analyses, respectively (Fig. 1, Additional file 5: Table S3). No significant association was noted between other components and pregnancy outcomes.
Associations between dietary patterns and adverse pregnancy outcomes during the three months before pregnancy (a) and the first trimester of pregnancy (b). The values presented are adjusted ORs (aOR) with 95% CIs and corresponded to the results derived from the multivariate analysis. The analysis was based on the noted covariates which were indicated in Tables 1 and 2. ORs adjusted for age, residence, economic situation, smoking and alcohol intake, and pre-pregnancy BMI. For the first trimester of pregnancy (b), ORs were additionally adjusted the nutrient supplementation
Discussion
Main findings
In this nested case-control study, we identified an association between ‘starchy’ dietary pattern (characterized by high intake in noodle and flour products and/or rice and its products) and adverse pregnancy outcomes. Strong association were found during the first trimester of pregnancy but showed no association during the three months before pregnancy.
Interpretation
We found that the dietary structure of China was mainly characterized by the “plant-animal balanced” pattern, which high in the consumption of grains, protein contents such as beans and their products, milk and its products and comprised high contents of poultry meat. It is similar to Japan which is also an Asian country [21]. However, it is quite different from the ‘plant-based’ dietary structure of India and Pakistan [22], the ‘animal-based’ dietary pattern of European and American countries [23], and the ‘Mediterranean’ dietary structure of Italy, Greece (comprised high contents of deep-sea fish, olive oil and fresh fruits) [24].
Besides, our results further demonstrated that high-starchy dietary patterns were associated with adverse pregnancy outcomes, but the existing researches on starchy foods were limited [14, 15, 25, 26]. Similar to our findings, Okubo et al. found that the maternal dietary pattern of excessive intake of ‘wheat products’ was more prone to nutritional imbalance than the high-protein dietary maternal pattern, resulting in a higher tendency to lower birth weight and the incidence of small for gestational age infants [27]. A research in Colorado also found a link that starchy foods such as potatoes, rice and other starchy vegetables, were associated with higher fasting glucose and greater newborn adiposity. These findings were also consistent with previous studies reporting inverse associations between the intake of dietary whole grains and insulin resistance [28, 29]. However, our results were not coherent with those from the study in Iran, which have shown that higher starchy food such as potato consumption was negatively associated with GDM risk, and there was no significant association with the consumption of total starchy or other starchy vegetables with GDM [30]. This possibly due to the confounding factors in their study did not take into account nutritional supplement. Additionally, there was a wider disparity in the diet characterization when compared to most studies on diet and pregnancy outcomes [9,10,11, 25, 26]. And the extraction of rice/flour products with proven healthy food [9,10,11], or with proven non-healthy food [25, 26] as a dietary structure may mask or exaggerate the effect.
Some researchers have considered the potential that high starchy food intake may influence the metabolic system [25, 31]. The possible reasons may be ascribed to the cereal and extensive processing of the starchy foods used in daily life that may result in the lack of dietary fibers, minerals and proteins in foods [32]. Moreover, these diets comprise fine grains that can be digested rapidly, thus increasing the dietary burden of the pancreas [25]. In addition, the refined grains and tubers have high glycemic index (GI) and glycemic load (GL) [32] that induce pathological glycemia and insulin resistance [33]. Other studies have revealed that the high GI group exhibited significantly higher risks of hyperlipidemia and metabolic disorders [31]. Besides, a previous research also confirmed that rice, as a principal component in the ‘Traditional’ diet pattern, has been positively associated with abnormal high-density lipoprotein in Chinese adults [34]. Larger cohort studies are required to examine this association in detail and to validate the findings of this study. It is beneficial to provide evidence on periconceptional preventative interventions to reduce the burden of adverse pregnancy outcomes.
Strengths and limitations
Although the present study exhibited a small sample size, our case-to-control ratio reached a value of 1:4, which is in accordance with the highest statistical efficiency of case-control requirements. There was enough power with the nested case–control design to detect an odds ratio of 3 for the adverse pregnancy outcomes. In addition, smaller selection bias and information bias were the consequences of the collection of the exposure data prior to disease diagnosis. Moreover, additional comparable cases and controls were used in the present study as a result of the use of the same cohort. Because this was not a randomized controlled trial, we cannot rule out the possibility that residual confounding may be contributing to this apparent association. There may be unmeasured confounders resulting in the apparent positive relationship between high starchy foods taking in the first trimester and adverse pregnancy outcomes. However, we have adjusted for major factors known to confound this relationship. Nutritional supplementation was an important confounding factor. In this study, folic acid and folic acid-related multivitamins were adjusted in multivariate analysis, which was the main supplementary nutrients in periconceptional period [35, 36]. Besides, by focusing on diagnosis made after collection of the FFQ data we attempted to avoid bias due to changes in diet after diagnosis, which strengthened the reliability of our results.
One of the limitations of this study was the use of an unquantified food frequency questionnaire (FFQ) without any portion size information. As thus, the accuracy of derived food item information was lower than that of the gold standard method for collecting weighed dietary records. However, when studying the relationship between diet and disease, the use of dietary patterns has advantages over the usual methods of examining a single food [37]. And the results of previous studies comparing the use of factor analysis using FFQ with the weighed dietary records suggested that the two methods were comparable in the efficient when investigating the diet-disease associations [38, 39].
Conclusion
High intake of starchy foods (characterized by high intake in noodle and flour products and/or rice and its products) during the first trimester of pregnancy may associated with increased risk for adverse pregnancy outcomes. Our work highlights the importance of promoting a healthy diet during pregnancy and suggests that behavior-change strategies may be necessary to improve perinatal outcomes and the health of the fetuses.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- aOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- Cis:
-
Confidence intervals
- FFQ:
-
Food-frequency questionnaire
- GDM:
-
Gestational diabetes mellitus
- HDP:
-
Hypertensive disorders in pregnancy
- OR:
-
Odds ratio
- SGA:
-
Small for gestational age
References
Jackson AA, Robinson SM. Dietary guidelines for pregnancy: a review of current evidence. Public Health Nutr. 2001;4(2b):625–30.
Grieger JA, Grzeskowiak LE, Clifton VL. Preconception dietary patterns in human pregnancies are associated with preterm delivery. J Nutr. 2014;1(7):15–6.
Martin CL, Sotres-Alvarez D, Siega-Riz AM. Maternal dietary patterns during the second trimester are associated with preterm birth. J Nutr. 2015;145(8):1857–64.
Schoenaker DA, Soedamah-Muthu SS, Callaway LK, Mishra GD. Prepregnancy dietary patterns and risk of developing hypertensive disorders of pregnancy: results from the Australian longitudinal study on Women's health. Am J Clin Nutr. 2015;102(1):94–101.
Schoenaker DA, Mishra GD. The role of energy, nutrients, foods, and dietary patterns in the development of gestational diabetes mellitus: a systematic review of observational studies. Diabetes Care. 2016;39(1):16–23.
He JR, Yuan MY, Chen NN, Lu JH, Hu CY, Mai WB, Zhang RF, Pan YH, Qiu L, Wu YF, et al. Maternal dietary patterns and gestational diabetes mellitus: a large prospective cohort study in China. Br J Nutr. 2015;113(8):1292–300.
Martinez-Galiano JM, Amezcua-Prieto C, Salcedo-Bellido I, Gonzalez-Mata G, Bueno-Cavanillas A, Delgado-Rodriguez M. Maternal dietary consumption of legumes, vegetables and fruit during pregnancy, does it protect against small for gestational age? BMC Pregnancy Childbirth. 2018;18(1):486.
Kibret KT, Chojenta C, Gresham E, Tegegne TK, Loxton D. Maternal dietary patterns and risk of adverse pregnancy (hypertensive disorders of pregnancy and gestational diabetes mellitus) and birth (preterm birth and low birth weight) outcomes: a systematic review and meta-analysis. Public Health Nutr. 2018:1–15.
de Castro MB, Freitas Vilela AA, de Oliveira AS, Cabral M, de Souza RA, Kac G, Sichieri R. Sociodemographic characteristics determine dietary pattern adherence during pregnancy. Public Health Nutr. 2016;19(7):1245–51.
Starling AP, Sauder KA, Kaar JL, Shapiro AL, Siega-Riz AM, Dabelea D. Maternal dietary patterns during pregnancy are associated with newborn body composition. J Nutr. 2017;147(7):1334–9.
Chen LW, Aris IM, Bernard JY, Tint MT, Chia A, Colega M, Gluckman PD, Shek LP, Saw SM, Chong YS, et al. Associations of maternal dietary patterns during pregnancy with offspring adiposity from birth until 54 months of age. Nutrients. 2016;9(1):2–17.
Abubakari A, Jahn A. Maternal dietary patterns and practices and birth weight in northern Ghana. PLoS One. 2016;11(9):e0162285.
Nana A, Zema T. Dietary practices and associated factors during pregnancy in northwestern Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):183.
Ramirez-Velez R, Correa-Bautista JE, Triana-Reina HR, Gonzalez-Jimenez E, Schmidt-RioValle J, Gonzalez-Ruiz K. Use of dietary supplements by pregnant women in Colombia. BMC Pregnancy Childbirth. 2018;18(1):117.
Sengpiel V, Bacelis J, Myhre R, Myking S, Devold Pay AS, Haugen M, Brantsaeter AL, Meltzer HM, Nilsen RM, Magnus P, et al. Folic acid supplementation, dietary folate intake during pregnancy and risk for spontaneous preterm delivery: a prospective observational cohort study. BMC Pregnancy Childbirth. 2014;14:375.
Guo L, Qu P, Zhang R, Zhao D, Wang H, Liu R, Mi B, Yan H, Dang S. Propensity score-matched analysis on the association between pregnancy infections and adverse birth outcomes in rural northwestern China. Sci Rep. 2018;8(1):5154.
Xiong T, Mu Y, Liang J, Zhu J, Li X, Li J, Liu Z, Qu Y, Wang Y, Mu D. Hypertensive disorders in pregnancy and stillbirth rates: a facility-based study in China. Bull World Health Organ. 2018;96(8):531–9.
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, Li Y, Zhao Z, Qin X, Jin D, et al. Prevalence and ethnic pattern of diabetes and Prediabetes in China in 2013. JAMA. 2017;317(24):2515–23.
Shu L, Shen XM, Li C, Zhang XY, Zheng PF. Dietary patterns are associated with type 2 diabetes mellitus among middle-aged adults in Zhejiang Province, China. Nutr J. 2017;16(1):81.
Cattell RB. The scree test for the number of factors. Multivariate Behav Res. 1966;1(2):245–76.
Murakami K, Livingstone MBE, Sasaki S. Establishment of a meal coding system for the characterization of meal-based dietary patterns in Japan. J Nutr. 2017;147(11):2093–101.
Yakub M, Iqbal MP, Iqbal R. Dietary patterns are associated with hyperhomocysteinemia in an urban Pakistani population. J Nutr. 2010;140(7):1261–6.
Haveman-Nies A, Tucker KL, de Groot LC, Wilson PW, van Staveren WA. Evaluation of dietary quality in relationship to nutritional and lifestyle factors in elderly people of the US Framingham heart study and the European SENECA study. Eur J Clin Nutr. 2001;55(10):870–80.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608.
Wolff CB, Wolff HK. Maternal eating patterns and birth weight of Mexican American infants. Nutr Health. 1995;10(2):121–34.
Coelho Nde L, Cunha DB, Esteves AP, Lacerda EM, Theme Filha MM. Dietary patterns in pregnancy and birth weight. Rev Saude Publica. 2015;49:62.
Okubo H, Miyake Y, Sasaki S, Tanaka K, Murakami K, Hirota Y, Kanzaki H, Kitada M, Horikoshi Y, Ishiko O, et al. Maternal dietary patterns in pregnancy and fetal growth in Japan: the Osaka maternal and child health study. Br J Nutr. 2012;107(10):1526–33.
Ylonen K, Saloranta C, Kronberg-Kippila C, Groop L, Aro A, Virtanen SM. Associations of dietary fiber with glucose metabolism in nondiabetic relatives of subjects with type 2 diabetes: the Botnia dietary study. Diabetes Care. 2003;26(7):1979–85.
Lutsey PL, Jacobs DR Jr, Kori S, Mayer-Davis E, Shea S, Steffen LM, Szklo M, Tracy R. Whole grain intake and its cross-sectional association with obesity, insulin resistance, inflammation, diabetes and subclinical CVD: the MESA study. Br J Nutr. 2007;98(2):397–405.
Goshtasebi A, Hosseinpour-Niazi S, Mirmiran P, Lamyian M, Moghaddam Banaem L, Azizi F. Pre-pregnancy consumption of starchy vegetables and legumes and risk of gestational diabetes mellitus among Tehranian women. Diabetes Res Clin Pract. 2018;139:131–8.
Feng R, Du S, Chen Y, Zheng S, Zhang W, Na G, Li Y, Sun C. High carbohydrate intake from starchy foods is positively associated with metabolic disorders: a cohort study from a Chinese population. Sci Rep. 2015;5:16919.
Gulland A. Eating overcooked starchy food is linked to cancer, agency warns. BMJ. 2017;356:j354.
Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care. 2008;31(12):2281–3.
Shi Z, Taylor AW, Hu G, Gill T, Wittert GA. Rice intake, weight change and risk of the metabolic syndrome development among Chinese adults: the Jiangsu nutrition study (JIN). Asia Pac J Clin Nutr. 2012;21(1):35–43.
Alwan NA, Greenwood DC, Simpson NA, McArdle HJ, Cade JE. The relationship between dietary supplement use in late pregnancy and birth outcomes: a cohort study in British women. BJOG. 2010;117(7):821–9.
Teixeira JA, Castro TG, Wall CR, Marchioni DM, Berry S, Morton SM, Grant CC. Effects of folic acid food fortification scenarios on the folate intake of a multi-ethnic pregnant population. Public Health Nutr. 2019;22(4):738–49.
Northstone K, Emmett PM, Rogers I. Dietary patterns in pregnancy and associations with nutrient intakes. Br J Nutr. 2008;99(2):406–15.
Togo P, Heitmann BL, Sorensen TI, Osler M. Consistency of food intake factors by different dietary assessment methods and population groups. Br J Nutr. 2003;90(3):667–78.
Khani BR, Ye W, Terry P, Wolk A. Reproducibility and validity of major dietary patterns among Swedish women assessed with a food-frequency questionnaire. J Nutr. 2004;134(6):1541–5.
Acknowledgements
We would like to thank all the women who participated in this survey. We are also grateful to all the investigators for their contribution to data collection.
Funding
This work was supported by the Science and Technology Bureau of Xi’an city [201805098YX6SF32(1)]; Chinese Center for Disease Control and Prevention (2015FYJ002); The Health and Family Planning Bureau of Xi’an City (HX201549) and Key Science and Technology Program of Shaanxi Province(2019SF-100). The funding body was not involved in: the design of the study; the collection, analysis, interpretation of data; the writing the manuscript.
Author information
Authors and Affiliations
Contributions
L.H., W.Y, M.C.C, D.L., L.Z. conceived the study; L.H., D.L. analyzed, interpreted of data, L.H. wrote the manuscript; L.H., L.S., C.Q., J.X., S.W., L.Y. collated data. All authors have been involved in revising the manuscript critically for important intellectual content; and they have given final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee for the Science of Medical center, at the First Affiliated Hospital of the Xi’an Jiaotong University approved all study protocols on 13 October, 2017 (No: XJTU1AF2017LSK-45). The patient’s informed consent regarding the analysis of their medical records and the hospital’s permission were obtained. Written informed consent forms were obtained from the participants who took part in this survey.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Questionnaire in English version.
Additional file 2: Figure S1.
Flow chart of participants in the study.
Additional file 3: Table S1.
The rotation matrix of dietary patterns and factor loading distribution during the three months before pregnancy.
Additional file 4: Table S2.
The rotation matrix of dietary patterns and factor loading distribution during the first trimester of pregnancy.
Additional file 5: Table S3.
The association between six principal dietary patterns and adverse pregnancy outcomes.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Huang, L., Shang, L., Yang, W. et al. High starchy food intake may increase the risk of adverse pregnancy outcomes: a nested case-control study in the Shaanxi province of Northwestern China. BMC Pregnancy Childbirth 19, 362 (2019). https://doi.org/10.1186/s12884-019-2524-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-019-2524-z