Abstract
Background
Mechanical power (MP) is the energy delivered by the ventilator to the respiratory system and combines factors related to the development of ventilator-induced lung injury (VILI). Flow-controlled ventilation (FCV) is a new ventilation mode using a constant low flow during both inspiration and expiration, which is hypothesized to lower the MP and to improve ventilation homogeneity. Data demonstrating these effects are scarce, since previous studies comparing FCV with conventional controlled ventilation modes in ICU patients suffer from important methodological concerns.
Objectives
This study aims to assess the difference in MP between FCV and pressure-controlled ventilation (PCV). Secondary aims were to explore the effect of FCV in terms of minute volume, ventilation distribution and homogeneity, and gas exchange.
Methods
This is a physiological study in post-cardiothoracic surgery patients requiring mechanical ventilation in the ICU. During PCV at baseline and 90 min of FCV, intratracheal pressure, airway flow and electrical impedance tomography (EIT) were measured continuously, and hemodynamics and venous and arterial blood gases were obtained repeatedly. Pressure–volume loops were constructed for the calculation of the MP.
Results
In 10 patients, optimized FCV versus PCV resulted in a lower MP (7.7 vs. 11.0 J/min; p = 0.004). Although FCV did not increase overall ventilation homogeneity, it did lead to an improved ventilation of the dependent lung regions. A stable gas exchange at lower minute volumes was obtained.
Conclusions
FCV resulted in a lower MP and improved ventilation of the dependent lung regions in post-cardiothoracic surgery patients on the ICU.
Trial registration Clinicaltrials.gov identifier: NCT05644418. Registered 1 December 2022, retrospectively registered.
Similar content being viewed by others
Background
In mechanically ventilated patients with the acute respiratory distress syndrome (ARDS), the development of secondary lung injury and inflammation—also known as ventilator-induced lung injury (VILI), is a major contributor to mortality in the intensive care unit (ICU). Variables associated with the development of VILI have been unified in the mechanical power (MP), a parameter that provides an estimate of the resistive, static and dynamic elastic forces that are transferred from the ventilator to the respiratory system [1]. MP can in part be modulated by ventilator strategy and settings [2]. In conventional controlled mechanical ventilation modes, the inspiratory phase is controlled and expiration is a passive process. The energy that is dissipated to the lung parenchyma during the expiratory phase has largely been ignored in the assessment of VILI risks. However, a sudden decrease in airway pressure may also contribute to VILI development considering alveolar heterogeneity and the potential for alveolar collapse and atelectrauma [3, 4].
Flow-controlled ventilation (FCV) is a new ventilation mode that uses a constant low flow during both inspiration and expiration, resulting in a linear increase in airway pressure during inspiration and a linear decrease in airway pressure during expiration [5]. The controlled expiration is accomplished by forcing the continuous flow through a nozzle in the ventilator, thereby generating a negative pressure in the tubing system. Through this Bernoulli effect, the ventilator controls the expiratory flow rate and thereby generates the linear decrease in airway pressure [5]. Theoretically, this could lower the energy dissipation during expiration, and hence lower the MP as compared to volume- or pressure-controlled ventilation (VCV and PCV, respectively) [5, 6]. Furthermore, FCV reduced alveolar heterogeneity and improved lung aeration on CT scan in a porcine model of ARDS [7], which also resulted in increased ventilation efficiency (lower minute volume with stable PaCO2) and attenuated lung injury. By lowering the MP and providing more homogeneous ventilation, FCV could thus be especially beneficial in critically ill patients requiring prolonged mechanical ventilation in the ICU.
To date, only two small pilot studies examined the physiological effects of FCV in the ICU, where a lower MP [8] and better oxygenation [9] with FCV were reported. However, results cannot be interpreted reliably since in both studies airway pressures were measured at different levels (at the circuit valve in volume-targeted ventilation versus intratracheally with FCV), thereby directly affecting MP calculations. The effects of FCV on lung homogeneity in ventilated ICU patients have not yet been investigated.
To better understand the concept and potential beneficial effects of FCV, we designed a physiological study comparing FCV and PCV in postoperative cardiothoracic surgery patients with relatively healthy lungs requiring mechanical ventilation at the ICU. The primary aim of this report was to assess the differences in MP, hypothesizing a lower MP with FCV. Secondary aims were to explore the effect of FCV in terms of minute volume, dissipated energy, ventilation distribution and homogeneity, and gas exchange.
Methods
For additional details, see online additional data, which is accessible from this issue’s table of content online at https://www.icm-experimental.springeropen.com.
Study design and patients
This prospective interventional study was conducted at the ICU of the Erasmus Medical Center, Rotterdam, The Netherlands, from February 2022 to May 2023 (ClinicalTrials.gov: NCT05644418), after approval by the local Medical Ethics Committee. Adult cardiothoracic surgery patients requiring postoperative controlled mechanical ventilation in the ICU were screened and provided written informed consent prior to their surgery. Eligibility was reassessed at ICU arrival. Enrollment criteria were (1) invasive controlled mechanical ventilation, (2) FiO2 ≤ 50%, (3) positive end-expiratory pressure (PEEP) ≤ 10 cmH2O. Exclusion criteria were: (1) severe sputum stasis, (2) severe respiratory insufficiency (i.e., PaO2/FiO2 < 100 mmHg, or moderate-to-severe ARDS according to the Berlin definition [10]), (3) untreated pneumothorax, (4) hemodynamic instability, (5) contraindications to EIT monitoring and (6) an inner tube diameter ≤ 6 mm.
Data collection
At enrollment, we collected sex, age, body mass index (BMI), ideal body weight (IBW), medical history, type of surgery, and hemodynamic status [noradrenalin dose, central venous oxygen saturation (ScvO2) and arterial-venous CO2 gap].
Continuous monitoring
A conventional tube adapter (Ventinova Medical BV, The Netherlands) and flow sensor (Hamilton Medical, Switzerland) were placed in between the endotracheal tube and ventilator tubing. This tube adapter is an essential part of FCV (Evone ventilator, Ventinova Medical BV) and consists of a thin pressure probe with a length of approximately 25 cm from the endotracheal tube opening, hence allowing the measurement of intratracheal pressures. Output of this pressure probe and the flow sensor were connected to a dedicated signal acquisition system (MP160, BIOPAC Systems Inc., USA) for a synchronized recording of waveforms sampled at 200 Hz (AcqKnowledge, BIOPAC Systems Inc., USA) during the full protocol. To assess homogeneity of ventilation, continuous monitoring with electrical impedance tomography (EIT) was initiated with a belt placed at the 4th–5th intercostal space (PulmoVista 500, Dräger Medical, Germany).
Study procedures
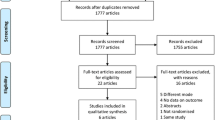
The study protocol was initiated directly after surgery when the patient arrived on the ICU. No recruitment maneuvers were performed after weaning from the cardiopulmonary bypass. Study steps are presented in Fig. 1 and lasted 30 min each. Arterial blood gases (ABG), central venous blood gases, SpO2, and hemodynamic and respiratory mechanics measurements were obtained at the end of each step. We aimed for a SpO2 of 95–100%, PaO2 < 15 kPa and end-tidal CO2 (EtCO2) and PaCO2 between 4.5 and 6.5 kPa throughout the protocol.
-
Baseline: PCV. Settings were optimized according to our local protocol (with PEEP as per a decremental PEEP trial aiming for the highest dynamic compliance (maximum PEEP 24 cmH2O), and tidal volumes of 6–8 mL/kg IBW) and were kept for at least 15 min to reach a stable condition before initiating continuous EIT, pressure and flow recordings for another 10 min at this step.
-
Step 1: FCV at ‘similar’ PCV settings. To directly compare FCV and PCV, the ventilation mode was switched to FCV with the same PEEP and FiO2 settings as baseline. Ppeak was titrated to reach the same tidal volumes as with PCV. Continuous set flow (determining the minute ventilation) was titrated to maintain a stable EtCO2. Inherent to the FCV working mechanism with an I:E ratio of 1:1, respiratory rate is the direct result of the combination of the set flow, the pressure difference between PEEP and Ppeak and the patient’s respiratory mechanics (resistance and compliance). Settings were kept for 30 min.
-
Step 2: FCV initial optimization. To maximally utilize the FCV working mechanism, FCV was optimized according to the ABG at the end of step 1 and the manufacturer’s instructions. PEEP was kept constant and FiO2 was adapted, if necessary, based on the PaO2 and target values mentioned at baseline. Ppeak was titrated in steps of 1 cmH2O to reach the highest dynamic compliance: if tidal volume increased more than expected (based on the dynamic compliance) when increasing the Ppeak, then Ppeak was further increased with 1 cmH2O. This sequence was repeated until tidal volumes did not increase more than expected (thus decreasing dynamic compliance) or until a safety limit of 10 mL/kg IBW was reached. Flow was adjusted to maintain PaCO2 within target values. Settings were kept for 30 min.
-
Step 3: FCV final optimization. Based on the ABG of step 2, flow and FiO2 were adjusted, if necessary, to maintain PaO2 and PaCO2 within target values.
The patient’s management was then resumed as per local clinical protocol (with PCV settings similar as baseline).
Offline analysis
Computation of parameters was performed for the steps baseline, step 1 and step 3.
Flow and pressure tracings
Breath-by-breath analysis of flow and intratracheal pressure was performed (Matlab 2021a, MathWorks, USA) for a period of 8–10 min at the end of each step. From the flow tracings, inspiratory time (Ti), RR, tidal volume (time-integral of inspiratory flow) and minute volume were calculated. Ppeak, total PEEP, and mean pressure were derived from the pressure waveforms. From the constructed pressure–volume (PV) loops (Additional file 1: Figure S1), the total energy per breath was computed as the integral of the PV loop times 0.098 (conversion to Joule), including the elastic dynamic and resistive components, but not the static part (unknown PEEP volume). The MP (Joule/min) was calculated by multiplying the total energy per breath by the RR. Dissipated energy was computed as the hysteresis area of the PV loop per breath (in Joule/Liter). For comparison, we also calculated the MP using bedside formulas for PCV [11] and using the simplified equation from Gattinoni [12] for FCV (which is similar to VCV during inspiration with its continuous flow).
EIT
Pixel-level EIT data were obtained (PV500 Data Analysis SW130) and processed using a custom software developed in Python. At the end of each step, a stable period of at least 10 breaths was manually selected. For each pixel, an average inspiration was computed over this stable period (Additional file 1: Figure S2). Pixels with a tidal impedance change (∆Z) of at least 15% of the maximum pixel ∆Z were included in the analysis (Additional file 1: Figure S3), assuming significant contribution to the ventilated lung space and to minimize influence of cardiac-related artifacts, in line with [13].
Regions of interest (ROIs; ventral, mid-ventral, mid-dorsal and dorsal) were defined with a physiological approach utilizing the ventilated lung space: per patient, we first computed an average pixel impedance map of all three steps (baseline, step 1 and step 3). Then, ROIs were defined with each ROI representing 25% of the total variation in lung impedance of this average map (Additional file 1: Figures S4, S5). This computation allowed to assess subtle changes in regional EIT parameters between PCV and FCV.
For each step, the global ∆Z and regional ∆Z (per ROI) were calculated, as well as the global and regional static compliance (per ROI) (i.e., ∆Z/driving pressure, with driving pressure being the difference between plateau pressure and total PEEP derived from the intratracheal pressure tracings during both PCV and FCV), and the change in global end-expiratory lung impedance (∆EELI). Furthermore, we visualized and quantified the overall, spatial and temporal ventilation homogeneity as follows:
-
Global inhomogeneity index (GI) [14]; GI(%) = ((∑[x,y ∈ lung]|∆Zxy – Median(∆Zlung)|)/(∑[x, ∈ lung]∆Zxy)) × 100%; with ∆Zxy the impedance change of a ventilated pixel (x,y) and ∆Zlung the impedance change of the ventilated lung space.
-
Regional spatial volume distribution: first, to provide a visualization of the continuous regional inspiratory volume distribution, impedance waveforms per ROI were normalized over time and visualized as a percentage of the global ∆Z (Additional file 1: Figure S6). Second, regional intra-tidal impedance distribution was visualized by dividing the global inspiration into five parts of equal ∆Z and then computing the ∆Z for each ROI (Additional file 1: Figure S7) [15].
-
Regional ventilation delay index (RVDi) [16]: regional ventilation delay (RVD) was first computed as RVD = ΔtRVD/Δtmax–min, with ΔtRVD the time between the start of inspiration (as per the global ∆Z) until pixel ∆Z reached 40% of the maximal ∆Z; this was normalized to the global inspiration time (Δtmax–min) and expressed as percentage (Additional file 1: Figure S8). RVDi was then calculated as the standard deviation of all pixel RVDs; a lower RVDi reflects a more homogeneous temporal lung inflation.
Hemodynamics and gas exchange
PaO2, PaCO2, PaO2/FiO2 ratio, central venous oxygen saturation (ScvO2), arterial-venous CO2 gap, ventilatory ratio [17], and noradrenalin dose were obtained per step.
Primary endpoint and secondary exploratory endpoints
Initially, our primary endpoint (see Clinicaltrials.gov: NCT05644418) was the EELI difference between PCV and FCV (step 1) to assess direct changes in lung aeration. FCV at step 1 was chosen for comparison because subsequent FCV optimization could influence EELI due to tidal recruitment. Upon reviewing preliminary data halfway during the study, however, it became apparent that EELI changes could not be evaluated reliably due to EELI changes likely related to clinical fluid therapy in this selected cohort; this was confirmed after enrolling another five patients where continuous EIT monitoring for 2 h on PCV was performed (Additional file 1: Figures S9, S10). Since EELI changes can only be reliably assessed when hemodynamics and fluid administration are relatively stable over the period of interest—which was especially challenging in our population of interest, we changed our primary endpoint to the difference in MP between PCV and optimized FCV for a more robust evaluation. Secondary endpoints were the difference in minute volume, dissipated energy, ventilation distribution and homogeneity, and gas exchange between PCV and (optimized) FCV.
Sample size
Due to the lack of comparator data, our sample size was based on the reported effect of FCV on minute volume in healthy pigs [18]. Using a matched pairs T-test approach (alpha, 0.05; power, 0.80) G*Power (Statistical Power Analyses, Universität Düsseldorf, Germany), the sample size was 6 patients. Since the effect size of FCV on other physiological parameters was unknown, we decided to enroll 10 patients in total. After changing the primary endpoint to the mechanical power, we did not re-power the sample size, because a good estimation of the difference in mechanical power between PCV and FCV could not be established using the previous literature, concerning that in those studies airway pressures during PCV and FCV were measured at different levels.
Statistical analysis
Statistical analysis was performed using SPSS (IBM, Armonk, USA). Values are presented as median (interquartile range) and were tested for normality using the Shapiro–Wilk test. Steps were compared using the repeated measures ANOVA or the related-samples Friedman’s test depending on the distribution, and with Bonferroni correction for multiple comparisons. p < 0.05 was considered statistically significant.
Results
Population and characteristics
In total, 21 patients provided informed consent prior to their planned surgery for participating in the full study protocol, of which 10 patients finally participated; their main characteristics are presented in Table 1. Reasons for withdrawal of 11 patients were direct postoperative extubation (n = 2), technical problem with the FCV ventilator (n = 1), a last-minute canceled and rescheduled surgery (to another day without availability of the study team) (n = 6), limited study staff (n = 1) and a surgical complication with need to return the patient to the operating theatre (n = 1). All patients underwent a median sternotomy (no minimally invasive procedures or off-pump procedures were performed). No serious adverse events were reported. One patient was excluded from EIT analysis due to artifacts in the recordings, likely due to a small ventral pneumothorax that was missed at enrollment.
Switch from PCV to FCV with similar settings (baseline vs. step 1)
FCV with ‘similar’ PCV settings did not affect MP [9.4 (8.0–11.1) vs. 11.0 (8.5–12.8) J/min, p = 0.286] but resulted in a lower dissipated energy [0.22 (0.17–0.26) vs. 0.34 (0.21–0.43) J/L, p = 0.008] for FCV vs. PCV, respectively. For all results comparing FCV step 1 and PCV, see Additional file 1: Tables S1 and S2. Although the global inhomogeneity index did not change (Additional file 1: Table S2), FCV with similar PCV settings did result in a more homogeneous spatial ventilation distribution with increased participation of the dorsal lung regions (Additional file 1: Figure S11).
FCV optimization (baseline vs. step 3)
Since maintaining similar tidal volumes as to conventional controlled ventilation does not utilize the potential of the FCV mode (i.e., tidal recruitment followed by controlled expiration to keep the lungs open), we optimized FCV in the following steps. Optimization of FCV (step 3) resulted in a significantly lower MP and dissipated energy compared to PCV at baseline while the minute volume and ventilatory ratio decreased (Table 2 & Fig. 2). FCV also resulted in a significantly lower RR, lower airway resistance and higher mean airway pressure. Despite changes in ventilation, oxygenation (PaO2 and PaO2/FiO2), PaCO2 and hemodynamics remained stable (Table 2). Two patients demonstrated a relatively high static respiratory system compliance in combination with a high airway resistance; their results are additionally presented in Additional file 1: Table S3.
EIT results are presented in Table 3. Whereas the dorsal ROI participated less to tidal ventilation during PCV at baseline, there was a significant increase in contribution of the dorsal ROI to tidal ventilation during optimized FCV, even exceeding ΔZ values of the ventral ROI (Table 3 and Fig. 3). The higher tidal volumes during optimized FCV did not result in overdistension of the ventral lung as demonstrated by the increase in regional static compliance during optimized FCV compared to PCV for all four ROIs (Table 3). Overall lung homogeneity and temporal ventilation homogeneity, reflected by the GI and RVDi respectively, did not differ between modes. For detailed comparison of ventilation homogeneity parameters of all three study steps, see Additional file 1: Figures S11 and S12.
Continuous regional volume distribution: average normalized impedance waveforms with 95% confidence interval per ROI over time and as a percentage of the global ∆Z. A During PCV (baseline), B during optimized FCV (step 3). Compared to PCV at baseline, optimized FCV resulted in a more homogeneous spatial ventilation distribution with increased participation of the dorsal lung regions
Discussion
The main finding of this study comparing flow-controlled mechanical ventilation with PCV in postoperative cardiothoracic patients in the ICU is that optimized FCV provides ventilation with significantly lower MP. As secondary endpoints we found that a stable gas exchange can be achieved with FCV at lower minute volumes and with lower dissipated energy, and that FCV did not provide a better overall lung homogeneity, but resulted in a more homogeneous spatial ventilation distribution with increased participation of the dorsal lung regions.
FCV to lower mechanical power
MP is independently associated with clinical outcomes, both in patients with and without lung injury [1, 19]. Our results are comparable with the studies of Grassetto and colleagues [8] and Spraider and colleagues [20] who also demonstrated a significantly lower MP on FCV, but important differences should be acknowledged. First, they used pressure and volume data measured before the tube with VCV or PCV, and after the tube during FCV [8, 20]. This makes a comparison between MP calculations unreliable since the energy needed to overcome the tube resistance was not incorporated with FCV. It also explains why the peak pressure was lower with FCV as compared to VCV in the study of Grassetto et al. (23 vs. 27 cmH2O for FCV vs. VCV, respectively, p < 0.001) [8]. In addition, Grasetto et al. [8] used VCV instead of PCV. We choose to compare FCV with PCV since this is the most commonly used controlled mechanical ventilation mode in the Netherlands. However, since both PCV and VCV modes make use of relatively high flow rates (while FCV flow rate is maximized to 20 L/min) and have a passive expiratory phase, differences in MP compared with FCV are expected to be rather similar for VCV and PCV (at most a small decrease in MP can be achieved with VCV compared to PCV because of the continuous inspiratory flow) [5].
Obtaining all pressure and flow tracings at the same location in the ventilator circuit during both PCV and FCV enabled us to reliably compare respiratory mechanics between both modes. Furthermore, this allowed us to generate detailed PV loops to calculate the MP and the dissipated energy that is considered to contribute to VILI development [5]. This is in contrast with earlier work [8, 20] where only bedside formulas for MP were used and compared. Note that the elastic static component (i.e., PEEP volume) was not integrated in our PV-loop-based calculation due to the unknown PEEP volume, but PEEP levels were similar in both PCV and FCV. We also computed the MP using bedside formulas (that tend to overestimate the true MP [12]) which also confirmed a significantly lower MP on FCV compared to PCV.
Effects of FCV on lung recruitment and homogeneity
Using a robust EIT analysis of the overall, spatial and temporal homogeneity, we demonstrated that FCV compared to PCV resulted in a more homogeneous spatial ventilation distribution with increased participation of the dorsal lung regions, despite no change in overall ventilation homogeneity and temporal ventilation homogeneity (assessed with the GI and RVDi, respectively).
Previously, in a randomized crossover study, Weber et al. [21] showed that the EELI and mean lung volume decreased less during FCV than during VCV in 23 obese patients undergoing abdominal surgery, indicating improved lung recruitment with FCV. Such trend was not observed in our study. As previously mentioned, it became apparent that EELI changes could not be evaluated reliably in our study, likely due to variations in EELI resulting from clinical fluid management in our selected cohort, as also previously reported [22]. Furthermore, Weber et al. reported that FCV improved regional ventilation distribution [21]. Although the latter conclusion is similar to ours, the data substantiating these conclusions are not. First, their patients only underwent 7 min of ventilation in each mode [21], making it challenging to quantify the amount of lung (de)recruitment owing to FCV and limiting the ability to fully evaluate the effects on regional ventilation. Moreover, they compared two equal-sized ROIs based on 50% of the ventrodorsal diameter [21]. Inherent to such computation, the amount of pixels participating in the ventral and dorsal ventilation could differ between ventilation modes, making it challenging to interpret subtle changes in EIT parameters. Our physiological approach to ROI definition allowed the assessment of more subtle changes in regional EIT parameters between PCV and FCV. Last, Weber [21] presented the decrease in tidal volume per 25% of expiratory impedance change as a parameter to conclude that FCV improves regional ventilation distribution. However, such parameter does not inform about ventilation homogeneity. In fact, they simply demonstrated that the FCV working principle indeed provides a continuous flow during both inspiration and expiration, thereby leading to a linear decrease in tidal volume (impedance) during expiration on FCV. In the study performed by Spraider et al. [20], cardiac surgery patients were either ventilated with FCV or PCV in the operating theatre. A CT scan made directly postoperatively showed a significantly lower amount of non-aerated lung tissue with FCV, which is in line with our findings that FCV leads to increased participation of the dorsal lung regions to ventilation.
Effects of FCV on ventilation efficiency
The ventilatory ratio is a useful bedside measurement to estimate the amount of dead space and thereby respiratory efficiency during mechanical ventilation [17]. The lower ventilatory ratio during FCV suggests that it could potentially be a parameter of interest when titrating FCV, since the ventilatory ratio is expected to increase when higher tidal volumes result in lung overdistension. Furthermore, a ventilatory ratio < 1 during FCV in our population with relatively healthy lungs suggest that ventilation was more efficient than predicted and/or the CO2 production was lower than predicted.
FCV optimization method
We optimized tidal volumes during FCV based on the best dynamic compliance after stepwise increasing the Ppeak, while not exceeding tidal volumes of 10 mL/kg IBW for safety reasons. This is different from the approach of Grassetto et al. [8] who kept tidal volumes constant and low, and also different from Van Dessel et al. [9] where FCV was applied with even lower tidal volumes and the same respiratory rate as with VCV. Our optimization method maximizes the FCV concept for multiple reasons. First, an improvement in dynamic compliance may indicate recruitment of lung regions, while a decrease in dynamic compliance would indicate that overdistension prevails. We showed that during optimized FCV the compliance as assessed by EIT increased in all lung regions, which is in line with the study by Spraider et al. who used a similar optimization method and CT assessment [20]. Inherent to the FCV working mechanism with an I:E ratio of 1:1, respiratory rate is the direct result of the combination between the set flow, the pressure difference between Ppeak and PEEP, and the patient’s respiratory mechanics (mainly resistance and compliance). Hence, by increasing tidal volumes, the respiratory rate will further decrease, thereby lowering the MP. In addition, with this lower respiratory rate the lung units with a longer time constant have sufficient time for lung inflation, further supporting recruitment [5].
Strengths and limitations
To date, this is the first physiological study in an ICU population that evaluates the differences in MP, dissipated energy, and detailed ventilation distribution between FCV and PCV with the use of intratracheal pressure and flow sensors and EIT. This overcomes methodological limitations of previous work and creates new evidence for FCV as a novel ventilation mode. However, our study does have some limitations that should be mentioned. First, upon reviewing preliminary data during the study, we changed our primary endpoint from the difference in end-expiratory lung impedance (EELI) to a more robust measure of the MP as derived from PV loops. Of note, the changes in EELI that were likely the result of fluid management in our specific population did not affect the computation of other EIT parameters. Second, we did not randomize between a ventilation sequence, which could have resulted in order effects and the influence of slow recruitment of partly collapsed lungs postoperatively; this may affect results in favor of FCV (more efficient gas exchange). However, by performing a decremental PEEP trial before the start of the study we expect that fast recruitment took place before measurements started. We explored the significance of this potential order effect by analyzing the minute volume and EtCO2 of the 5 patients that were additionally enrolled for undergoing EIT measurements during PCV only, and found that minute volume decreased by only 7% in those patients after 90 min of PCV (from 7.7 to 7.2 L/min), with stable ETCO2 values. This is in large contrast with the 40% reduction in minute volume that we found with optimized FCV. Third, by increasing tidal volumes during FCV optimization the ventilatory efficiency increased (i.e., the ratio of ventilatory dead space to tidal volume decreased); this could partly explain the decrease in MP in our study. Indeed, Haudebourg et al. [23] found a reduction in MP of 7% when ventilating patients with 7.7 mL/kg IBW (using a low driving pressure strategy that required an increase in tidal volume), as compared to using low tidal volume ventilation (6.1 mL/kg IBW), both in PCV mode. In contrast, the MP decreased with 30% during optimized FCV in our study. Although our tidal volumes during optimized FCV were slightly higher (8.4 mL/kg IBW), there is likely an additional mechanistic effect of the FCV mode on decreasing the MP (i.e., not explained by the increase in tidal volume alone).
Clinical implications
Our study was performed in postoperative ICU patients with relatively healthy lungs, with degrees of atelectasis primarily influenced by the surgical procedure and cardiopulmonary bypass time instead of lung disease. We choose this population as we first wanted to systematically evaluate the concept and physiological consequences of the FCV mode prior to moving toward ICU patients with hyperinflammatory and heterogeneous lungs. The role of FCV in such population and within a lung-protective ventilation strategy in ARDS is yet unknown and of further ongoing study (see Clinicaltrials.gov: NCT06051188). A point of debate is the acceptation of higher tidal volumes (and driving pressures) in an ARDS population, considering the current guidelines with tidal volumes limited to 4–8 mL/kg IBW [24]. However, ARDS guidelines are based upon research in an era where FCV was not clinically available. With our work we would rather stimulate discussion and potentially a mindset change to the general approach to mechanical ventilation: not primarily focusing on tidal volumes and driving pressures, but increasingly considering viscoelastic properties of the lung tissue, the time it takes to achieve a certain tidal volume, and the potential benefit of additionally controlling the expiratory phase.
In conclusion, optimized FCV as compared to PCV in postoperative cardiothoracic surgery ICU patients resulted in a significantly lower MP and dissipated energy, as well as in a more homogeneous spatial ventilation distribution with increased participation of the dorsal lung regions. The current study provides a good rationale for assessing the role of FCV in ARDS patients where high MP and alveolar heterogeneity resulting in VILI are still major contributors to ICU morbidity and mortality.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABG:
-
Arterial blood gas
- ARDS:
-
Acute respiratory distress syndrome
- a.u.:
-
Arbitrary units
- AVR:
-
Aortic valve replacement
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass graft
- COPD:
-
Chronic obstructive pulmonary disease
- Crs:
-
Compliance respiratory system
- EELI:
-
End-expiratory lung impedance
- EIT:
-
Electrical impedance tomography
- EtCO2:
-
End-tidal CO2
- FCV:
-
Flow-controlled ventilation
- FiO2:
-
Fraction of inspired oxygen
- GI:
-
Global inhomogeneity index
- IBW:
-
Ideal body weight
- ICU:
-
Intensive care unit
- I:E ratio:
-
Inspiratory:expiratory ratio
- IQR:
-
Inter quartile range
- MP:
-
Mechanical power
- MVP:
-
Mitral valve repair
- MVR:
-
Mitral valve replacement
- PaCO2:
-
Arterial partial carbon dioxide pressure
- PaO2:
-
Arterial partial oxygen pressure
- PCV:
-
Pressure-controlled ventilation
- Pdrive:
-
Driving pressure
- PEEP:
-
Positive end-expiratory pressure
- P/F ratio:
-
PaO2/FiO2 ratio
- Pmean:
-
Mean airway pressure
- Ppeak:
-
Peak pressure
- Pplat:
-
Plateau pressure
- PV-loop:
-
Pressure–volume loop
- ROI:
-
Region of interest
- RR:
-
Respiratory rate
- RVDi:
-
Regional ventilation delay index
- ScvO2:
-
Central venous oxygen saturation
- SpO2:
-
Peripheral oxygen saturation
- Ti:
-
Inspiratory time
- VCV:
-
Volume-controlled ventilation
- VILI:
-
Ventilator-induced lung injury
References
Costa E, Slutsky A, Brochard L, Brower R, Serpa-Neto A, Cavalcanti A et al (2021) Ventilatory variables and mechanical power in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 204(3):303–311
Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M et al (2016) Mechanical power and development of ventilator-induced lung injury. Anesthesiology 124(5):1100–1108
Kollisch-Singule M, Emr B, Smith B, Ruiz C, Roy S, Meng Q et al (2014) Airway pressure release ventilation reduces conducting airway micro-strain in lung injury. J Am Coll Surg 219(5):968–976
Slutsky AS, Ranieri VM (2013) Ventilator-induced lung injury. N Engl J Med 369(22):2126–2136
Barnes T, van Asseldonk D, Enk D (2018) Minimisation of dissipated energy in the airways during mechanical ventilation by using constant inspiratory and expiratory flows—flow-controlled ventilation (FCV). Med Hypotheses 121:167–176
Barnes TE, Enk D (2018) Ventilation for low dissipated energy achieved using flow control during both inspiration and expiration. Trends Anaesthe Crit Care 1(1):1–8
Schmidt J, Wenzel C, Spassov S, Borgmann S, Lin Z, Wollborn J et al (2020) Flow-controlled ventilation attenuates lung injury in a porcine model of acute respiratory distress syndrome: a preclinical randomized controlled study. Crit Care Med 48(3):e241–e248
Grassetto A, Pettenuzzo T, Badii F, Carlon R, Sella N, Navalesi P (2023) Flow-controlled ventilation may reduce mechanical power and increase ventilatory efficiency in severe coronavirus disease-19 acute respiratory distress syndrome. Pulmonology 29(2):154–156
Van Dessel E, De Meyer G, Morrison S, Jorens P, Schepens T (2022) Flow-controlled ventilation in moderate acute respiratory distress syndrome due to COVID-19: an open-label repeated-measures controlled trial. Intensive Care Med Exp 10:19
The ARDS Definition Task Force (2012) Acute respiratory distress syndrome—the Berlin definition. JAMA 307(23):2526–2533
Trinkle CA, Broaddus RN, Sturgill JL, Waters CM, Morris PE (2022) Simple, accurate calculation of mechanical power in pressure controlled ventilation (PCV). Intensive Care Med Exp 10:22
Giosa L, Busana M, Pasticci I, Bonifazi M, Macri MM, Romitti F et al (2019) Mechanical power at a glance: a simple surrogate for volume-controlled ventilation. Intensive Care Med Exp 7:61
Heines SJH, de Jongh SAM, Strauch U, van der Horst ICC, van de Poll MCG, Bergmans DCJJ (2022) The global inhomogeneity index assessed by electrical impedance tomography overestimates PEEP requirement in patients with ARDS: an observational study. BMC Anesthesiol 22(1):258
Zhao Z, Möller K, Steinmann D, Frerichs I, Guttmann J (2009) Evaluation of an electrical impedance tomography-based global inhomogeneity index for pulmonary ventilation distribution. Intensive Care Med 35(11):1900–1906
Lowhagen K, Lundin S, Stenqvist O (2010) Regional intratidal gas distribution in acute lung injury and acute respiratory distress syndrome assessed by electric impedance tomography. Minerva Anestesiol 76(12):1024–1035
Muders T, Hentze B, Simon P, Girrbach F, Doebler MRG, Leonhardt S et al (2019) A modified method to assess tidal recruitment by electrical impedance tomography. J Clin Med 8(8):1161
Sinha P, Calfee C, Beitler J, Soni N, Ho K, Matthay M et al (2019) Physiologic analysis and clinical performance of the ventilatory ratio in acute respiratory distress syndrome. Am J Respir Crit Care Med 199(3):333–341
Schmidt J, Wenzel C, Mahn M, Spassov S, Schmitz CH, Borgmann S et al (2018) Improved lung recruitment and oxygenation during mandatory ventilation with a new expiratory ventilation assistance device: a controlled interventional trial in healthy pigs. Eur J Anaesthesiol 35(10):736–744
Van Meenen DMP, Algera AG, Schuijt MTU, Simonis FD, Van der Hoeven SM, Neto AS et al (2023) Effect of mechanical power on mortality in invasively ventilated ICU patients without the acute respiratory distress syndrome—an analysis of three randomized clinical trials. Eur J Anaesthesiol 40(1):21–28
Spraider P, Abram J, Martini J, Putzer G, Glodny B et al (2023) Flow-controlled versus pressure-controlled ventilation in cardiac sugery with cardiopulmonary bypass—a single-center, prospective, randomized, controlled trial. J Clin Anesth 91:111279
Weber J, Straka L, Borgmann S, Schmidt J, Wirth S, Schumann S (2020) Flow-controlled ventilation (FCV) improves regional ventilation in obese patients—a randomized controlled crossover trial. BMC Anesthesiol 20(1):24
Becher T, Wendler A, Eimer C, Weiler N, Frerichs I (2019) Changes in electrical impedance tomography findings of ICU patients during rapid infusion of a fluid bolus: a prospective observational study. Am J Respir Crit Care Med 199(12):1572–1575
Haudeborg AF, Tuffet S, Perier F, Razazi K, De Prost N et al (2022) Driving pressure-guided ventilation decreases the mechanical power compared to predicted body weight-guided ventilation in the Acute Respiratory Distress Syndrome. Crit Care 26:185
Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey A et al (2017) An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of critical care medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 195(9):1253–1263
Acknowledgements
Not applicable.
Funding
Supported in part by Ventinova Medical B.V. and the European Union Horizon 2020 research and innovation program under grant agreement number 961787. Funders played no role in the design and conduct of the study; interpretation of the data; preparation, review, or approval of the manuscript; nor in the decision to submit the manuscript for publication. The opinions, results and conclusions reported in this paper are those of the authors.
Author information
Authors and Affiliations
Contributions
Concept: PvdZ, HE, DAMPJG; design: JPvO, PvdZ, HE, DAMPJG; data acquisition: JPvO, AHJ; data analysis: JPvO, JEF, PS, AHJ; data interpretation: all authors; manuscript drafting: JPvO, JEF, AHJ; manuscript revising for intellectual content and final approval: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the local medical ethics committee of the Erasmus Medical Center (MEC-2019-0074).
All patients provided written informed consent prior to their surgery.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary methods and results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Van Oosten, J.P., Francovich, J.E., Somhorst, P. et al. Flow-controlled ventilation decreases mechanical power in postoperative ICU patients. ICMx 12, 30 (2024). https://doi.org/10.1186/s40635-024-00616-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-024-00616-9