Abstract
Purpose
This study aimed to compare midflexion rotational laxity between two different design concept models of cruciate-retaining total knee arthroplasty: symmetrical surface design of neutral joint line obliquity and asymmetrical surface design of varus joint line obliquity.
Methods
Sixty-three knees that underwent cruciate-retaining total knee arthroplasty were evaluated. Manual maximum passive rotational stress without acceleration was applied to the knees under navigation monitoring. Pre-operative and post-operative internal and external rotational angles were measured at 30°, 45°, 60°, and 90° knee flexion.
Results
The post-operative internal rotational laxity was significantly increased compared with pre-operative levels at 30°, 45°, 60°, and 90° flexion among all subjects (mean 9.7° vs 11.1°, 10.6° vs 11.6°, 11.2° vs 12.9°, and 13.2° vs 14.9°; p = 0.01, 0.04, 0.001, and 0.008, respectively). The post-operative external rotational laxity was significantly decreased compared to pre-operative levels at 30°, 45°, 60°, and 90° flexion among all subjects (mean 10.8° vs 6.8°, 12.5° vs 9.4°, 12.8° vs 10.0°, and 11.3° vs 9.5°; p < 0.0001, < 0.0001, < 0.0001, and 0.0008, respectively). The post-operative total rotational laxity significantly decreased, compared with pre-operative levels, at 30° and 45° flexion among all subjects (mean 20.4° vs 17.9°, and 23.1° vs 21.1°; p = 0.002 and 0.04, respectively). The post-operative total rotational laxity was significantly smaller in asymmetrically designed total knee arthroplasty than in symmetrically designed total knee arthroplasty at 30°, 45°, and 60° flexion (mean 19.3° vs 15.8°, 22.8° vs 18.7°, and 24.4° vs 20.8°; p = 0.03, 0.03, and 0.02, respectively), whereas no significant difference was observed at 90° flexion.
Conclusion
Compared to symmetrical surface design, asymmetrical surface design resulted in lower rotational laxity at the midflexion range in cruciate-retaining total knee arthroplasty.
Level of evidence
III.
Similar content being viewed by others
Background
Appropriate stability and soft-tissue balance are crucial factors for successful clinical outcomes in total knee arthroplasty (TKA), because joint instability is considered to lead to a significant risk of the need for revision TKA [23, 40]. Recently, several researchers have insisted on achieving anatomical joint stability and normal kinematics [27, 29, 35, 38, 43]. Kinoshita et al. highlighted the high correlation between rotational soft tissue balance and overall kinematics flexion angle between pre- and post-operative TKA [21]. Hence, rotational laxity is considered as one of the key factors for accomplishing proper joint functional reconstruction in TKA.
Image-free navigation systems are optional tools for achieving appropriate bone resection and placement of components [25, 39]. Furthermore, navigation systems are useful for measuring intraoperative midflexion laxity, joint positioning, and knee kinematics [12,13,14,15,16,17]. Hino et al. demonstrated that the midflexion rotational laxity increased owing to the implantation of posterior-stabilised TKA (PS-TKA) [13], because the cruciate ligaments distribute towards the stabiliser against rotational stress [2, 4]. Nonetheless, there are few reports on midflexion rotational laxity in cruciate-retaining TKA (CR-TKA) [21, 28].
Recently, several studies have investigated the effects of changes in lower-limb alignment and joint line obliquity on the balance between the joint gap and tibial force [8, 9, 34, 37]. However, the effects on midflexion laxity remain unclear. We hypothesised that rotational laxity is affected by differences in the implant design including joint-line obliquity with the preservation of the posterior cruciate ligament (PCL). Thus, the present study aimed to evaluate changes in the midflexion rotational laxity between two different design concept models of CR-TKA: symmetrical surface design and asymmetrical surface design of joint line obliquity in the coronal plane.
Methods
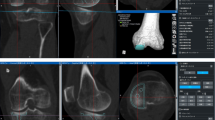
In total, 88 patients with medial osteoarthritis who underwent CR-TKA using a navigation system (Precision Knee Navigation software version 4.0; Stryker, Kalamazoo, MI, USA) in our hospital were enrolled in this retrospective study. Those with valgus alignment knees, existing inflammatory arthritis, and incomplete rotational laxity data were excluded to unify the conditions of the patients.
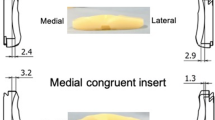
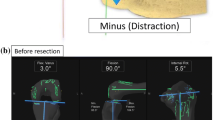
Overall, 63 knees of 55 patients with a mean age of 72.4 ± 8.1 years (range: 45–85 years) were enrolled in the study. The average pre-operative hip–knee–ankle angle was 10.6 ± 5.8° in varus knees. The implants used were NexGen CR-Flex, Persona CR (Zimmer, Warsaw, IN, USA, n = 37), and FINE Total Knee System (Nakashima Medical, Okayama, Japan, n = 26). Further patient characteristics are listed in Table 1. The patients were divided into two groups according to the TKA design concept. NexGen CR-Flex and Persona CR, which induce kinematics to the inherent restraint of implants by adopting the symmetrical surface design of neutral joint-line obliquity between the femoral condyle and the tibial insert, were classified as group S. On the other hand, the anatomical approach that prioritises the kinematics inherent in soft tissues, as the FINE Total Knee System has an asymmetrical design with 3° of joint line obliquity on the insert of the coronal alignment to build in anatomical elements, was classified as group A (Fig. 1) [31, 33]. Both group models adopt multi-radius designs for the femoral component. Meanwhile, there are differences in the radius size between the medial and lateral condyle of group A to reproduce the anatomical joint line. The medial parapatellar approach and measured resection technique were used for all knees. Femoral and tibial joints were resected by mechanical alignment.
The femoral rotational axis was defined as being perpendicular to the Whiteside line. The tibial rotational axis was set parallel to the line connecting one-third of the tibial tubercle to the centre of the cut surface. Anchoring pins with an infrared signal transducer were fixed into the femur and tibia as reference points, and the joint capsule was temporarily closed with four strands of suture after registration. The investigator gently applied physiologically allowable maximal manual internal and external rotation stress to the knee without angular acceleration, and the mechanical femoral–tibial rotational angle was measured automatically by the navigation system at 30°, 45°, 60°, and 90° of knee flexion. The measurements obtained directly following joint-capsule closure, with the presence of osteophytes, soft tissues, meniscus, and the cruciate ligaments, were defined as the pre-operative record. The articular surfaces of the distal femur and the proximal tibia were resected using the navigation-assisted measured resection technique. The largest sized components without both anteroposterior and mediolateral overhang were selected, after utilising the femoral-sizing guide and tibial-sizing plate. After trial components were placed, the medial–lateral balance of the knee was assessed throughout ROM. When the soft tissue balance was inappropriate, a minimal-released stepped adjustment was applied for accurate ligament balance as necessary: the release of medial collateral ligament, posterior knee capsule or PCL, or bone additional resection.
After confirming that the TKA components and inserts were firmly placed in an appropriate position, the surgical incision was completely closed. Thereafter, the same procedure as described for the pre-operative measurements was repeated to measure and record the rotational angles at 30°, 45°, 60°, and 90° as post-operative rotational laxity. Total rotational laxity was recorded as the sum of the absolute internal and external stress angles. Positive values indicate internal orientation, and negative values indicate external orientation. The accuracy of the navigation system has been established at 0.5°.
The test–retest reliability of these internal and external rotational stress angles indicated that interclass and intraclass correlation coefficients (ICCs) were sufficiently high, with values > 0.9 at 30°, 45°, 60°, and 90°, respectively.
Statistical analyses
Statistical analyses were performed using JMP software version 16.0.0 (SAS Institute, Tokyo, Japan). The Mann–Whitney U test and Fisher’s exact test were performed to compare groups S and A, whereas the Wilcoxon signed-rank test was performed for pre- versus post-operative comparisons, respectively. In all studies, a probability level of 95% (p < 0.05) was considered statistically significant.
Statistical analyses for ICCs were performed using IBM SPSS version 23 (IBM Corp., Armonk, NY, USA). An ICC > 0.81 was considered to be indicative of an almost perfect correlation. The sample size was calculated using Power and Sample Size Calculations software version 3.1.2 (Vanderbilt University, Nashville, TN, USA). After measuring the rotational laxity in the first 10 patients, the mean and standard deviation of the pre- and post-operative TKA data were calculated. To achieve a correlation of δ = 3 and σ = 5 with 80% power and α = 0.05, we determined that a minimum sample size of 39 knees would be required. To compensate for the small sample size, 63 knees were assessed.
Results
Table 2 summarises the mean internal, external, and total rotational laxity. The post-operative internal rotational laxity was significantly increased, compared with pre-operative levels, at 30°, 45°, 60°, and 90° of knee flexion (mean 9.7° vs 11.1°, 10.6° vs 11.6°, 11.2° vs 12.9°, and 13.2° vs 14.9°; p = 0.01, 0.04, 0.001, and 0.008, respectively; Table 2, Fig. 2). On the other hand, the post-operative external rotational laxity was significantly decreased, compared with pre-operative levels, at 30°, 45°, 60°, and 90° of knee flexion (mean 10.8° vs 6.8°, 12.5° vs 9.4°, 12.8° vs 10.0°, and 11.3° vs 9.5°; p < 0.0001, < 0.0001, < 0.0001, and 0.0008, respectively; Table 2, Fig. 2). Moreover, the post-operative total rotational laxity was significantly decreased, compared with pre-operative levels, at 30° and 45° of knee flexion (mean 20.4° vs 17.9°, and 23.1° vs 21.1°; p = 0.002 and 0.04, respectively; Table 2, Fig. 3).
Subsequently, the mean difference in post-operative rotational laxity was analysed between groups S and A. No significant difference in internal or external laxity was observed (Table 2, Fig. 4). The total rotational laxity in group A was significantly smaller than that in group S at flexion of 30°, 45°, and 60° (mean 19.3° vs 15.8°, 22.8° vs 18.7°, and 24.4° vs 20.8°; p = 0.03, 0.03, and 0.02, respectively; Table 2, Fig. 5). In contrast, no significant difference in total rotational laxity was observed at flexion of 90° among all comparisons.
Discussion
The most important finding of the present study is that the difference in the design concept affects midflexion rotational laxity in CR-TKA. The results indicated that the rotational laxity at the initial flexion angle of asymmetrically designed implants had significantly decreased, compared with that of the symmetrically designed implants. FINE Total Knee System was developed to reconstruct an anatomical normal knee; the femoral medial condyle has greater radius than the lateral condyle to reproduce 3° of joint line obliquity in coronal alignment. When combined with the insert, it enhances the conformity of the medial condyle joint surface, and the post-operative analysis of kinematics using image-matching has shown tibial internal rotation with medial pivot motion [31, 33]. Furthermore, several cadaveric studies have indicated that the medial structures such as the superficial medial collateral ligament (sMCL), deep medial collateral ligament (dMCL), and posterior oblique ligament resist tibial internal rotational stress during the early stage of flexion [5, 10, 32, 44, 45]. It is inferred from the previous study that the characteristic of FINE seemingly affects the ligament tension pattern, especially with medial structures. As several researchers have emphasised the importance of medial stability for good clinical outcomes in TKA [20, 41, 46], patient-reported outcome measures remain to be investigated further.
The present study also demonstrated that the post-operative rotational laxity at the midflexion range significantly decreased compared with the pre-operative level in CR-TKA. Several studies have shown that the post-operative midflexion gap and varus-valgus laxity in PS-TKA are greater than those in CR-TKA [12, 27], and PCL deficiency resulted in an increased flexion gap [30, 42]. Regarding biomechanics, the PCL is recognised as comprising several small bundles, and the length pattern of each bundle varies throughout flexion [1, 3, 11, 36]. Hence, preservation of the PCL and TKA implantation appear to affect the tension pattern affecting each PCL bundle, resulting in changes in the midflexion rotational laxity.
Contrary to our opinion, Banks et al. [6, 7] reported that CR-TKA had greater rotational laxity than PS or mobile-bearing (MB) TKA, with demonstrated lateral pivot pattern. Their studies were different from our study in that applying the other implant designs, the method of obtaining intraoperative balance varied including soft-tissue releases, and the measurements were performed by image-matching with weight bearing. The clinical significance of the differences between our study and those of Banks et al. leaves room for additional research.
Another key finding of the present study was that no significant difference in total rotational laxity was observed at flexion of 90° among all comparisons. Matsuzaki et al. [28] demonstrated the association between the amount of internal rotation from intermediate to deep flexion and post-operative maximum flexion angle. Kobayashi et al. [22] also reported the correlation of lateral laxity at 80° of flexion with the post-operative flexion angle. These findings indicated that appropriate joint laxity at deep flexion angle was required to obtain favourable maximum flexion angle. Therefore, it seems reasonable to consider that CR-TKA, the focus of our study, ensures the post-operative flexion angle, regardless of whether it is symmetrical or asymmetrical.
The present study has some limitations. First, the operations were performed under general anaesthesia with inflated tourniquet, and navigation data were measured under non-weight bearing conditions. Second, only osteoarthritis knees with varus deformity were covered by the study, and the sample size was limited. Furthermore, the osteoarthritis change varied among the patients, with possible changes in knee kinematics or ligament balance. Finally, despite the quantification and validation of the rotational stress by multiple investigators, measurements were obtained by manual passive stress of the surgeons.
Nevertheless, our study has originality in the assessment of pre- and post-operative midflexion rotational laxity in clinical practice, which has seldom been attempted. Although numerous studies have been conducted to clarify the proper ligament balance in TKA, the relationships between patient outcomes remain controversial [17,18,19, 24, 26, 46]. Although the present study clarified changes in midflexion rotational laxity in CR-TKA, their association with clinical results has not been fully investigated. Future research could focus on the clinical course and validation of previous results. Our study suggests that variations in joint line obliquity due to the difference in design concepts and the existence of PCL affect midflexion rotational laxity in CR-TKA.
Conclusions
The asymmetrically designed implant, which reproduces varus joint-line obliquity, resulted in lower rotational laxity in the midflexion range than in the symmetrically designed implant with neutral joint-line obliquity. Furthermore, in CR-TKA, post-operative rotational laxity decreased compared to pre-operative levels in the initial flexion range.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- dMCL:
-
Deep medial collateral ligament
- ICC:
-
Intraclass correlation coefficient
- MB-TKA:
-
Mobile-bearing total knee arthroplasty
- PCL:
-
Posterior cruciate ligament
- PS-TKA:
-
Posterior-stabilised total knee arthroplasty
- sMCL:
-
Superficial medial collateral ligament
- TKA:
-
Total knee arthroplasty
References
Ahmad CS, Cohen ZA, Levine WN, Gardner TR, Ateshian GA, Mow VC (2003) Codominance of the individual posterior cruciate ligament bundles. An analysis of bundle lengths and orientation. Am J Sports Med 31:221–225
Amis AA (2012) The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc 20:613–620
Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR (2003) Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 11:271–281
Athwal KK, Hunt NC, Davies AJ, Deehan DJ, Amis AA (2014) Clinical biomechanics of instability related to total knee arthroplasty. Clin Biomech (Bristol, Avon) 29:119–128
Ball S, Stephen JM, El-Daou H, Williams A, Amis AA (2020) The medial ligaments and the ACL restrain anteromedial laxity of the knee. Knee Surg Sports Traumatol Arthrosc 28:3700–3708
Banks SA, Hodge WA (2004) 2003 Hap Paul Award Paper of the International Society for Technology in Arthroplasty. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty 19:809–816
Banks SA, Hodge WA (2004) Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res 426:187–193
Blakeney W, Beaulieu Y, Kiss MO, Rivière C, Vendittoli PA (2019) Less gap imbalance with restricted kinematic alignment than with mechanically aligned total knee arthroplasty: simulations on 3-D bone models created from CT-scans. Acta Orthop 90:602–609
Blakeney W, Beaulieu Y, Puliero B, Kiss MO, Vendittoli PA (2020) Bone resection for mechanically aligned total knee arthroplasty creates frequent gap modifications and imbalances. Knee Surg Sports Traumatol Arthrosc 28:1532–1541
Cavaignac E, Carpentier K, Pailhé R, Luyckx T, Bellemans J (2015) The role of the deep medial collateral ligament in controlling rotational stability of the knee. Knee Surg Sports Traumatol Arthrosc 23:3101–3107
Hatsushika D, Nimura A, Mochizuki T, Yamaguchi K, Muneta T, Akita K (2013) Attachments of separate small bundles of human posterior cruciate ligament: an anatomic study. Knee Surg Sports Traumatol Arthrosc 21:998–1004
Hino K, Ishimaru M, Iseki Y, Watanabe S, Onishi Y, Miura H (2013) Mid-flexion laxity is greater after posterior-stabilised total knee replacement than with cruciate-retaining procedures: a computer navigation study. Bone Joint J 95-B:493–497
Hino K, Kutsuna T, Oonishi Y, Watamori K, Kiyomatsu H, Iseki Y et al (2017) Assessment of the midflexion rotational laxity in posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3495–3500
Hino K, Kutsuna T, Watamori K, Ishimaru Y, Kiyomatsu H, Shiraishi Y et al (2018) Bi-cruciate substituting total knee arthroplasty provides varus-valgus stability throughout the midflexion range. Knee 25:897–902
Hino K, Kutsuna T, Watamori K, Kiyomatsu H, Ishimaru Y, Takeba J et al (2017) Varus-valgus stability at 90° flexion correlates with the stability at midflexion range more widely than that at 0° extension in posterior-stabilized total knee arthroplasty. Arch Orthop Trauma Surg 137:1429–1434
Hino K, Oonishi Y, Kutsuna T, Watamori K, Iseki Y, Kiyomatsu H et al (2016) Preoperative varus-valgus kinematic pattern throughout flexion persists more strongly after cruciate-retaining than after posterior-stabilized total knee arthroplasty. Knee 23:637–641
Ishida K, Shibanuma N, Matsumoto T, Sasaki H, Takayama K, Matsuzaki T et al (2016) Navigation-based femorotibial rotation pattern correlated with flexion angle after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:89–95
Ishii Y, Matsuda Y, Ishii R, Sakata S, Omori G (2003) Coronal laxity in extension in vivo after total knee arthroplasty. J Orthop Sci 8:538–542
Ishii Y, Matsuda Y, Ishii R, Sakata S, Omori G (2005) Sagittal laxity in vivo after total knee arthroplasty. Arch Orthop Trauma Surg 125:249–253
Kamenaga T, Muratsu H, Kanda Y, Miya H, Kuroda R, Matsumoto T (2018) The influence of postoperative knee stability on patient satisfaction in cruciate-retaining total knee arthroplasty. J Arthroplasty 33:2475–2479
Kinoshita T, Hino K, Kutsuna T, Watamori K, Miura H (2021) Rotational soft-tissue balance is highly correlated with rotational kinematics in total knee arthroplasty. J Knee Surg 36(1):47–53
Kobayashi T, Suzuki M, Sasho T, Nakagawa K, Tsuneizumi Y, Takahashi K (2012) Lateral laxity in flexion increases the postoperative flexion angle in cruciate-retaining total knee arthroplasty. J Arthroplasty 27:260–265
Le DH, Goodman SB, Maloney WJ, Huddleston JI (2014) Current modes of failure in TKA: infection, instability, and stiffness predominate. Clin Orthop Relat Res 472:2197–2200
Longo UG, Candela V, Pirato F, Hirschmann MT, Becker R, Denaro V (2021) Midflexion instability in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 29:370–380
Lützner J, Günther KP, Kirschner S (2010) Functional outcome after computer-assisted versus conventional total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc 18:1339–1344
Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Varus-valgus balance and range of movement after total knee arthroplasty. J Bone Joint Surg Br 87:804–808
Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R (2012) Intraoperative soft tissue balance reflects minimum 5-year midterm outcomes in cruciate-retaining and posterior-stabilized total knee arthroplasty. J Arthroplasty 27:1723–1730
Matsuzaki T, Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kawakami Y et al (2013) Kinematic factors affecting postoperative knee flexion after cruciate-retaining total knee arthroplasty. Int Orthop 37:803–808
Meneghini RM, Deckard ER, Ishmael MK, Ziemba-Davis M (2017) A dual-pivot pattern simulating native knee kinematics optimizes functional outcomes after total knee arthroplasty. J Arthroplasty 32:3009–3015
Mihalko WM, Krackow KA (1999) Posterior cruciate ligament effects on the flexion space in total knee arthroplasty. Clin Orthop Relat Res 360:243–250
Miyazaki Y, Nakamura T, Kogame K, Saito M, Yamamoto K, Suguro T (2011) Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty 26:1038–1044
Moslemian A, Arakgi ME, Roessler PP, Sidhu RS, Degen RM, Willing R et al (2021) The Medial structures of the knee have a significant contribution to posteromedial rotational laxity control in the PCL-deficient knee. Knee Surg Sports Traumatol Arthrosc 29:4172–4181
Nakajima A, Yamada M, Sonobe M, Akatsu Y, Saito M, Yamamoto K et al (2021) Three-year clinical and radiological results of a cruciate-retaining type of the knee prosthesis with anatomical geometry developed in Japan. BMC Musculoskelet Disord 22:241
Niki Y, Sassa T, Nagai K, Harato K, Kobayashi S, Yamashita T (2017) Mechanically aligned total knee arthroplasty carries a risk of bony gap changes and flexion-extension axis displacement. Knee Surg Sports Traumatol Arthrosc 25:3452–3458
Nishio Y, Onodera T, Kasahara Y, Takahashi D, Iwasaki N, Majima T (2014) Intraoperative medial pivot affects deep knee flexion angle and patient-reported outcomes after total knee arthroplasty. J Arthroplasty 29:702–706
Papannagari R, DeFrate LE, Nha KW, Moses JM, Moussa M, Gill TJ et al (2007) Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med 35:1507–1512
Roth JD, Howell SM, Hull ML (2018) Kinematically aligned total knee arthroplasty limits high tibial forces, differences in tibial forces between compartments, and abnormal tibial contact kinematics during passive flexion. Knee Surg Sports Traumatol Arthrosc 26:1589–1601
Seito N, Onodera T, Kasahara Y, Kondo E, Iwasaki N, Majima T (2017) Preoperative knee deformity and kinematics impact postoperative knee kinematics in total knee arthroplasty. Knee 24:1462–1468
Song EK, Agrawal PR, Kim SK, Seo HY, Seon JK (2016) A randomized controlled clinical and radiological trial about outcomes of navigation-assisted TKA compared to conventional TKA: long-term follow-up. Knee Surg Sports Traumatol Arthrosc 24:3381–3386
Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R (2015) Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am 97:715–720
Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H et al (2017) Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee 24:1478–1484
Tsuneizumi Y, Suzuki M, Miyagi J, Tamai H, Tsukeoka T, Moriya H et al (2008) Evaluation of joint laxity against distal traction force upon flexion in cruciate-retaining and posterior-stabilized total knee arthroplasty. J Orthop Sci 13:504–509
Warth LC, Ishmael MK, Deckard ER, Ziemba-Davis M, Meneghini RM (2017) Do medial pivot kinematics correlate with patient-reported outcomes after total knee arthroplasty? J Arthroplasty 32:2411–2416
Wierer G, Milinkovic D, Robinson JR, Raschke MJ, Weiler A, Fink C et al (2021) The superficial medial collateral ligament is the major restraint to anteromedial instability of the knee. Knee Surg Sports Traumatol Arthrosc 29:405–416
Willinger L, Shinohara S, Athwal KK, Ball S, Williams A, Amis AA (2020) Length-change patterns of the medial collateral ligament and posterior oblique ligament in relation to their function and surgery. Knee Surg Sports Traumatol Arthrosc 28:3720–3732
Yoshihara Y, Arai Y, Nakagawa S, Inoue H, Ueshima K, Fujiwara H et al (2016) Assessing coronal laxity in extension and flexion at a minimum of 10 years after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2512–2516
Acknowledgements
The authors thank Editage (www.editage.com) for the support with English language editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
KH, TK, KW, TK, and TT substantially contributed to conception and design, data acquisition, or data analysis and interpretation. MT and KH provided the final approval for the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The procedures in the study were undertaken in accordance with the ethical standards of the Helsinki Declaration and were approved by the local ethics committee. This study was approved by the institutional review board of Ehime University (Identification Number: 1411020), and informed consent was obtained from all patients.
Consent for publication
Informed consent was obtained from all individual participants in the study.
Competing interests
Kazunori Hino received research support from Teijin Nakashima Medical. The other authors have no conflict of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsuda, T., Hino, K., Kutsuna, T. et al. Difference in implant design affects midflexion rotational laxity in cruciate-retaining total knee arthroplasty: a computer navigation study. J EXP ORTOP 10, 85 (2023). https://doi.org/10.1186/s40634-023-00652-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00652-6