Abstract
Purpose
The aim of this study was to analyze the clinical results provided by multi-layer cell-free scaffolds for the treatment of knee osteochondral defects.
Methods
A systematic review was performed on PubMed, Web of Science, and Cochrane to identify studies evaluating the clinical efficacy of cell-free osteochondral scaffolds for knee lesions. A meta-analysis was performed on articles reporting results of the International Knee Documentation Committee (IKDC) and Tegner scores. The scores were analyzed as improvement from baseline to 1, 2, and ≥ 3 years of follow-up. The modified Coleman Methodology Score was used to assess the study methodology.
Results
A total of 34 studies (1022 patients) with a mean follow-up of 35 months was included. Only three osteochondral scaffolds have been investigated in clinical trials: while TruFit® has been withdrawn from the market for the questionable results, the analysis of MaioRegen and Agili-C™ provided clinical improvements at 1, 2, and ≥ 3 years of follow-up (all significantly higher than the baseline, p < 0.05), although with a limited recovery of the sport-activity level. A low rate of adverse events and an overall failure rate of 7.0% were observed, but the overall evidence level of the available studies is limited.
Conclusions
Multi-layer scaffolds may provide clinical benefits for the treatment of knee osteochondral lesions at short- and mid-term follow-up and with a low number of failures, although the sport-activity level obtained seems to be limited. Further research with high-level studies is needed to confirm the role of multi-layer scaffold for the treatment of knee osteochondral lesions.
Similar content being viewed by others
Background
Knee osteochondral lesions have always represented a problem for the orthopedic surgeon because of the poor regenerative potential of the cartilage tissue coupled with the challenge of concomitantly addressing the affected subchondral bone [32, 61]. Several techniques have been developed over the years to address knee osteochondral lesions, in order to relieve pain, restore function and possibly delay osteoarthritis (OA) onset [14]. Traditional surgical approaches consist of autologous or allogenic osteochondral tissue transplantation to provide an immediate viable tissue at the lesion site [23, 25, 31]. These techniques demonstrated promising results up to long-term follow-up, but they also showed several drawbacks, such as a significant donor site morbidity for autologous osteochondral transplantation (OAT), and high cost, limited availability, and contamination risk for osteochondral allograft transplantation (OCA) [21, 31, 75]. Also, chondrocyte-based regenerative treatments developed to overcome these limitations did not provide an optimal solution for osteochondral lesions [26, 42, 54]. The reasons might be found in the complexity of cartilage-bone interface and the differences between cartilage and subchondral bone layers, including both biological and biomechanical properties. In this light, an optimal treatment should aim at addressing the entire osteochondral unit [53, 61].
Progress in the field of biomaterials has led to the development of various scaffolds to address the entire osteochondral unit, based on the rationale of reproducing the different biological and functional requirements for the growth of both bone and cartilage tissues [1, 35, 57]. In this regard, multi-layer cell-free osteochondral scaffolds have been introduced with the aim to provide a biomimetic and biodegradable three-dimensional structure that favors subchondral bone and cartilage-like tissue regeneration [22, 50, 51]. They showed a potential to act as stimuli for the differentiation of resident bone marrow stromal cells, by inducing an “in situ” tissue regeneration that allows a durable osteochondral tissue without the need for any cell augmentation [45, 52]. From a clinical point of view, these scaffolds showed to be easy to handle and exploitable in one-step procedures, avoiding issues related to cell manipulation and culture [44]. However, among the different solutions explored in the preclinical setting, only few cell-free multi-layer scaffolds have currently been investigated in clinical trials, and their results and effectiveness are still debated.
The aim of this study was to review the available literature and to analyze the clinical results provided by multi-layer cell free scaffolds for the treatment of knee osteochondral defects.
Materials and methods
A systematic review and meta-analysis were performed on the literature of cell-free osteochondral scaffold implantation for knee lesions. The search was conducted on three electronic databases (PubMed, Web of Science, and Cochrane) on May 10, 2021, with no time limitation and without any filter, using the following string: (osteochondral) AND (scaffold OR matrix OR implant) AND (knee). The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines were used [59]. A flowchart of the studies selection for qualitative and quantitative data synthesis is reported in Fig. 1. The screening process and analysis were conducted separately by 2 independent observers (LS and AP). In the first step, the articles were screened by title and abstract and the following inclusion criteria for relevant articles were used: clinical studies, written in the English language, on cell-free osteochondral scaffolds for the treatment of osteochondral lesions of the knee. Exclusion criteria were articles written in other languages, pre-clinical studies, studies reporting other osteochondral procedures such as cell-based scaffolds, OAT, OCA, case reports, and reviews. In the second step, the full texts of the selected articles were retrieved and screened, with further exclusions according to the previously described criteria. Reference lists from the selected papers and from the reviews of the field, found with the first and second screening, were also checked, and all selected studies were included in the qualitative data synthesis.
For the included studies, relevant data (year of publication, study design, number of patients evaluated, patient sex, age, and BMI, lesion size, lesion location, lesion grade, type of scaffold, scores reported, final follow-up, overall results) were extracted from article texts, tables, and figures, and then collected in a database with consensus of the two observers, to be analyzed for the purposes of the present study. To assess the methodological quality of the collected data, the Coleman Methodology Score (CMS), modified by Kon et al. [48] to better suit the cartilage repair field, was determined for each study. Two reviewers (LS and AP) independently evaluated the studies, and discrepancies were resolved through discussion and consensus with a third author (AB). Safety was evaluated through the reported adverse effects, while the failure rate was calculated through the documented surgical failures (patients requiring a joint replacement or a new surgery related to the scaffold implantation). Finally, the articles reporting clinical outcomes were selected and included in the meta-analysis. The scores were analyzed as improvement from baseline to 1, 2, and ≥ 3 years of follow-up, in order to investigate clinical results over time of cell-free osteochondral scaffold implantation. The articles included in the systematic review were excluded from the meta-analysis in the following cases: the same survey was reported at different follow-up times and the most recent articles also reported the intermediate follow-up results; mean basal scores or follow-up scores (including standard deviation) not reported; articles on multi-layer scaffolds withdrawn from the market.
Statistical analysis
The statistical analysis and the Forest plot were carried out according to Neyeloff et al. [60] using Microsoft Excel. The comparisons among the follow-up times was based on the analysis of variance of the difference between basal and follow-up score (MD) [58]. With no heterogeneity, the estimation of the MD and its 95% confidence interval was based on fixed effect analysis of variance; the random effect model was preferred otherwise. P-value of 0.05 was used as the level of statistical significance. Statistical heterogeneity was evaluated by t using Cochran's Q statistic and I2 metric and was considered significant when I2 > 25%.
Results
The search identified 1914 records after duplicates removal, whose titles and abstracts were screened and selected according to the inclusion/exclusion criteria: 1835 records were excluded and a total of 79 full-text articles were assessed for eligibility; 45 full-text articles were further excluded (Fig. 1). Thus, a total of 34 studies were included in the qualitative data synthesis and reported in detail in Table 1. Since the first reports in 2011, beside a peak in 2014 (8 articles), the publication trend was stable over time (Fig. 2).
Qualitative data synthesis
Among the 34 articles included in the qualitative data synthesis, the evaluation of the study type showed only one randomized clinical trial (RCT), three retrospective/prospective comparative studies, and 30 case series (Table 1). Regarding the type of osteochondral scaffold investigated, 20 studies analyzed the results of MaioRegen (Finceramica, Faenza, Italy) with 19 case series and one RCT versus microfracture technique, 11 studies described the results of TruFit® (Smith & Nephew, Andover, MA) with nine case series and two retrospective comparative study (versus OAT and microfracture technique, respectively), and three studies reported the results of Agili-C™ (CartiHeal (2009) Ltd, Israel) with two case series and one retrospective study comparing two different versions of the same scaffold.
The evaluation with the CMS showed an overall poor quality of the included studies, with a mean of 44.4 ± 9.8 (range 24—67). Only two studies scored higher than 60, seven studies reached a score between 50 and 59, whereas 16 studies had a score between 40 and 49, and nine studies obtained a score lower than 40. No improvement over time was found for the CMS score of the published articles, as reported in Fig. 3. There was a 68% agreement between the two authors involved in the evaluation of CMS.
A total of 1022 patients were treated with cell-free osteochondral scaffolds (522 with MaioRegen, 304 with TruFit®, and 196 with Agili- C™), with a mean age of 35.6 ± 9.9 years (range 16.2—64.4). Patients were evaluated at a mean follow-up of 35.2 ± 19.3 months. In particular, 19 studies reported the outcome at short-term follow-up (≤ 24 months), eight at short/mid-term follow-up (24–60 months), and seven at mid/long-term follow-up (≥ 60 months), including the longest mean follow-up available in the literature (121 months) [69]. A wide range of heterogeneous clinical scores were used to evaluate patients. The most commonly used scores were: IKDC subjective score (25 articles), Tegner score (22 articles), IKDC objective score (16 articles), Knee Injury and Osteoarthritis Outcome Score (KOOS, 14 articles), Lysholm score (10 articles), and Visual Analogue Score (VAS) for pain (seven articles). Twenty-seven studies also reported an imaging evaluation, with the Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) score used in 24 studies (MOCART 2.0 in two studies) to evaluate scaffold integration and defect filling [66]. Due to the limited outcome data available, a quantitative data analysis was performed on the two most common scores reported at the follow-up times (IKDC subjective score and Tegner score).
Safety and failures
Adverse events were documented in 23 of the included studies for a total of 806 evaluated patients. Most of these were mild symptoms (knee pain and effusion) complained by the patients and some cases of post-operative fever solved in a few days. Moreover, 13 cases of knee effusion that required knee arthrocentesis were described [68]. Different severe adverse events, requiring hospitalization or intervention to prevent permanent impairment or damage, were reported. In particular, post-operative joint stiffness was documented in 33 patients (4.3%) and required a knee mobilization under narcosis or an arthroscopic release to improve knee functionality (2.1% for TruFit®, 2.0% for Agili-C™, and 5.8% for MaioRegen, respectively). In studies evaluating TruFit® implantation, Gelber et al. [29] described one case of deep vein thrombosis and one case of acute septic arthritis solved after arthroscopic implant removal combined to specific antibiotic therapy over a period of six week. Hindle et al. [36] reported one case of suspected infection (developing a liquefied hematoma at one month post-operatively, and then solved after a six week of antibiotic therapy). Finally, Wang et al. [74] treated one patient presenting deep infection with irrigation and debridement.
A total of 65 failures was reported in the included studies, for an overall 7.0% failure rate at a mean follow-up of 31.0 months. Patients who failed underwent implant removal and subsequent alternative cartilage treatment or a partial/total knee replacement (36 and 29, respectively). Considering the failures reported in each scaffold group, patients treated with TruFit® had an overall 9.9% failure rate at a mean follow-up of 39.8 months, patients treated with Agili-C™ had an overall 8.2% failure rate at a mean follow-up of 18.0 months, and patients treated with MaioRegen had an overall 4.6% failure rate at a mean follow-up of 28.4 months.
Quantitative data analysis
Among the 28 studies evaluating IKDC subjective or Tegner scores, six studies were excluded from the meta-analysis for the following reasons: no standard deviation reported (four studies) or no pre-operative clinical data reported (two studies). Thus, a total of 22 studies evaluating MaioRegen or Agili-C™ was included in the quantitative synthesis.
The IKDC subjective score was available for 640 patients in 18 studies (14 for MaioRegen and 4 for Agili-C™). In detail, 1-year follow-up was available for 565 patients (16 studies), 2-year follow-up for 476 patients (15 studies), and ≥ 3-year follow-up (mean 55.2 ± 13.7) for 113 patients (5 studies). Compared with the basal score, the meta-analysis showed a mean improvement of 26.0 (95% CI 23.3–28.8, I2 = − 89%) at 1-year follow-up, 31.1 (95% CI 28.0–34.3, I2 = − 69%) at 2-year follow-up, and 34.8 (95% CI 30.6–39.1, I2 = − 59%) at ≥ 3-year follow-up (Fig. 4), all significantly higher than the baseline (p < 0.05), with a further statistically significant improvement from 1 to 3 years of follow-up (p = 0.003).
The activity level evaluated with Tegner score was available for 499 patients in 16 studies (15 for MaioRegen and one for Agili-C™). In detail, 1-year follow-up was available for 341 patients (10 studies), 2-year follow-up for 347 patients (12 studies), and ≥ 3-year follow-up (mean 54.0 ± 15.5) for 86 patients (4 studies). Compared with the basal score, the meta-analysis showed a mean improvement of 1.4 (95% CI 0.9–1.9, I2 = − 40%) at 1-year follow-up, 2.0 (95% CI 1.5–2.5, I2 = − 50%) at 2-year follow-up, and 1.9 (95% CI 1.4–2.4, I2 = − 80%) at ≥ 3-year follow-up (Fig. 5), all significantly higher than baseline (p < 0.05), but without any significant difference among follow-up times.
In Figs. 4 and 5, the results have been reported separately for MaioRegen and Agili-C™ scaffolds.
Discussion
The main finding of this study is that the available literature supports the use of multi-layer cell-free scaffolds for the treatment of patients with knee osteochondral defects. These scaffolds provided promising clinical improvement at short/mid-term follow-up, with a low rate of adverse events and an overall failure rate of 7.0% at a mean 31.0 months of follow-up. Nevertheless, the evidence level of the available studies was limited and high-level trials at longer follow-up are still missing.
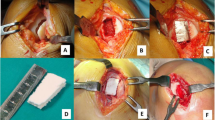
Among the developed osteochondral scaffolds, only three have currently been documented in clinical trials. TruFit® was the first one introduced in the clinical practice. It is a bilayer scaffold made of a semiporous poli-lactic (PLGA), poli-glycolic acid (PGA), and calcium sulfate biopolymer. The different size cylinders (from 5 to 11 mm and with a maximum depth of 18 mm) were initially introduced with the indication to backfill graft donor sites during OAT procedures, but they were later mainly used as a one-step osteochondral treatment [5]. MaioRegen is the most widely studied multi-layer scaffold. It is a nanostructured implant consisting of different ratios of collagen and hydroxyapatite organized in three-layers. The composition of this scaffold reproduces the extracellular matrix structures of cartilage and bone tissues and is based on the nucleation of hydroxyapatite nanocrystals onto self-assembled collagen fibers to generate a chemically and morphologically graded biomimetic material [71]. Initially, this scaffold was obtained from a square of 35 × 35 mm (manual sizing) with a depth of 6 ± 2 mm. Currently, the scaffold is available also in a cylindrical shape with different sizes (12—18 mm) and different depths (2 to 6 mm). Agili-C™ is the most recent osteochondral scaffold studied in the clinical practice. It is an aragonite-based scaffold consisting of two layers: a bone phase made of calcium carbonate in the aragonite crystalline form, and a superficial cartilage phase composed of modified aragonite and hyaluronic acid. This scaffold was developed in the shape of cylinders, with different sizes in terms of width and depth. Recently, a tapered version of the implants, with an angle of 2 degrees from the longitudinal axis, has been designed to improve the press-fit implantation of the cylinder [47].
These multi-layer scaffolds have been investigated in several clinical studies for the treatment of osteochondral defects of the knee. Studies investigating the safety and effectiveness of the TruFit® implant often reported poor outcomes in terms of clinical results, failure rate, and histological evaluation. Dhollander et al. [19] documented a failure rate of 20% at 1 year of follow-up with the histological analysis showing fibrous vascularized repair tissue. Shivji et al. [69] evaluated this scaffold also at long-term follow-up (121 months), reporting no statistically significant improvement in any score from baseline, while the MRI evaluation showed incomplete or no evidence of plug incorporation and persistent chondral loss. Based on these poor results, the TruFit® scaffold has been withdrawn from the market. Regarding the scaffolds still available in the clinical practice, since the first trial published in 2011, numerous studies showed promising results in terms of safety profile and clinical improvement [38]. In particular, this meta-analysis demonstrated that at 1-year follow-up the IKDC subjective score improved significantly compared with the baseline scores, demonstrating the efficacy of these techniques. Moreover, the evaluation at follow-up showed a further improvement from 1 to 3 years, suggesting that most of the benefit is achieved in the first year, but also that the osteochondral regeneration might need more time to reach stable results. This seems to be different from the trend previously reported for cell-free chondral scaffolds, as in a recent meta-analyses stable results were documented after 1 year using chondral cell-free matrices for the treatment of knee cartilage lesions [3, 70]. Still, despite the more complex lesion pattern due to the subchondral bone involvement, the osteochondral scaffolds provided a satisfactory clinical improvement. Unfortunately, the current literature does not allow to draw conclusions on the long-term results for osteochondral scaffolds, with no studies investigating the results over six years.
Another important aspect evaluated in this study was the activity level. Sport represents a fundamental parameter to consider for cartilage lesions, especially in young and active patients [2]. The meta-analysis on the Tegner activity level documented a significant improvement from baseline to 1-year follow-up, whit stable values at the at 2-year and at ≥ 3-year follow-up evaluations. This stable trend is in line with that reported for the other cartilage procedures, ranging from autologous chondrocyte implantation (ACI) to OAT [10, 65]. Conversely, some authors described a significantly deterioration in activity level from 2 years of follow-up after microfracture technique [10, 30, 33]. However, this meta-analysis reported a lower mean improvement of the Tegner score at 1- and 2-year follow-ups compared with the literature values offered by microfracture, OAT and ACI procedures at the same follow-ups [49]. The lower results in term of activity level found for the osteochondral scaffold could be due to the complexity of the treated lesions affecting the entire osteochondral unit and the heterogeneity of the investigated populations, which involved several complex cases ranging from early OA patients to knee osteonecrosis [7, 12, 39, 67]. For example, Maioregen scaffold was also used to address complex lesions, and the most recent article of Agili-C™ was targeted to the complex population of patients with OA joints, challenging conditions where other procedures focused only on the cartilage layer failed to provide satisfactory outcomes [26, 28, 39]. Further studies should explore if the lower activity level reached in these studies is due to the more challenging treatment indications of osteochondral scaffolds, or to a lower regenerative potential of these osteochondral scaffolds versus the chondral and cell-based treatments largely documented in the literature of the last two decades.
Besides the clinical results, most of the included studies also performed an imaging assessment, in order to evaluate the scaffold maturation over time. MRI evaluation demonstrated controversial and heterogeneous findings. On one side, some studies described complete filling of the cartilage layer and a good integration of the graft, on the other side, most of the included studies reported the presence of subchondral bone alterations after the scaffold implantation [11, 40]. Moreover, the maturation of the scaffold appeared slow, especially in the subchondral bone area, even though the majority of the studies highlighted a positive evolution over time. In fact, several authors reported a significant increase of the defect filling and a significant subchondral bone status improvement over time, although with persistent signal abnormalities over time [40, 68]. However, no correlation was found between imaging findings and clinical outcomes. The persistence of an altered signal and a slow maturation process of the subchondral layer suggest that further improvements are still needed to obtain better tissue regeneration and optimal durable clinical results [44].
The systematic review and meta-analysis also underline the overall low-quality level of the studies in this field, with only one RCT and three retrospective/prospective comparative studies. In a retrospective comparative study, Wang et al. [74] compared the results of TruFit® scaffold to microfracture for the treatment of 132 patients with knee chondral or osteochondral defects. While no significant differences in clinical outcomes were reported up to 5 years, the scaffold group reported better activity level and MRI appearance of the defect, resulting in a more frequent good-quality tissue fill and cartilage isointensity. The same scaffold has been also compared with osteochondral mosaicplasty in a retrospective study conducted by Hindle et al. on 66 patients with knee articular cartilage defects [36]. At the final follow-up (22 months for the scaffold group and 30 for the mosaicplasty group), the authors demonstrated significantly better clinical outcomes and a higher rate of return to sport after mosaicplasty, indicating that mosaicplasty may be more effective than TruFit® approach. In the only RCT available in this field, Kon et al. [40] evaluated 100 patients affected by symptomatic knee chondral and osteochondral lesions treated with MaioRegen or microfracture. While comparable results were found in the overall population, the osteochondral scaffold provided significantly better clinical results compared to microfracture in the treatment of deep osteochondral lesions and sport active patients at 2 years of follow-up. The authors concluded that microfracture technique can be considered a treatment option for purely chondral lesions, while offers worse results for osteochondral lesions, where osteochondral scaffolds showed to be a more suitable therapeutic solution.
This study presents some limitations, that reflect the weakness of the literature on the field. In fact, the lack of studies at long-term follow-up needs to be underlined, particularly given that the earliest scaffolds should have already reached a long-term follow-up with relatively numerous cohorts of patients. The overall quality level of the included studies is generally low, as confirmed by the low CMS and by the presence of only 1 RCT and 3 comparative studies. Moreover, the analysis of the CMS did not show any improvement over time. Moreover, only a small percentage of studies evaluated the treatment of isolated osteochondral lesions, while the treatment was often performed in association with other procedures, given the complexity of patients treated with osteochondral scaffold. Finally, numerous and heterogeneous scores were adopted, therefore hindering the possibility of comparison among studies. Accordingly, a weakness of the meta-analysis is represented by the low number of patients included and the high proportion of level IV studies. Despite the heterogeneous patient populations, lesion locations, the different scaffold used, and the different follow-up times, an overall short- to mid-term benefit was described for the two osteochondral scaffolds currently available in the clinical practice. Further high-level studies with longer follow-up are needed, as well as comparative trials with the other osteochondral procedures including mosaicplasty and OCA, to clarify the potential and indication of these techniques to restore a functional osteochondral unit. Moreover, comparative studies among osteochondral scaffolds could help improving the field. Finally, while these cell-free scaffolds have been developed to overcome the problems related to cell-expansion, the possibility to augment them with cell concentrates, to exploit their regenerative and homeostatic potential [27, 55, 63], in one-step procedures should be explored to help addressing challenging lesions such as those presenting an OA joint environment.
Conclusions
The current literature suggested that multi-layer osteochondral scaffolds may provide clinical benefits for the treatment of knee osteochondral lesions at short- and mid-term follow-up and with a low number of failures, although the sport activity level obtained seems to be limited. Further research with high-level studies is needed to confirm the role of multi-layer scaffold for the treatment of osteochondral lesions of the knee.
Availability of data and materials
Not applicable.
Abbreviations
- ACI:
-
Autologous chondrocyte implantation
- BMI:
-
Body mass index
- CI:
-
Confidence Interval
- CMS:
-
Modified Coleman Methodology Score
- ICRS:
-
International Cartilage Repair Society score
- KOOS:
-
Knee Injury and Osteoarthritis Outcome score
- MOCART:
-
Magnetic Resonance Observation of Cartilage Repair Tissue score
- MRI:
-
Magnetic resonance imaging
- OA:
-
Osteoarthritis
- OAT:
-
Autologous osteochondral transplantation
- OCA:
-
Osteochondral allograft transplantation
- PGA:
-
Poli-glycolic acid
- PLGA:
-
Poly lactic-co-glycolic acid
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- RCT:
-
Randomized clinical trial
- VAS:
-
Visual Analogue Score
References
Andjelkov N, Riyadh H, Ivarsson M, Kacarevic-Popovic Z, Krstic J, Wretenberg P (2021) The enhancement of cartilage regeneration by use of a chitosan-based scaffold in a 3D model of microfracture in vitro: a pilot evaluation. J Exp Orthop 8:12
Andrade R, Vasta S, Papalia R, Pereira H, Oliveira JM, Reis RL et al (2016) Prevalence of articular cartilage lesions and surgical clinical outcomes in football (soccer) players' knees: a systematic review. Arthroscopy 32:1466–1477
Andriolo L, Reale D, Di Martino A, Boffa A, Zaffagnini S, Filardo G (2019) Cell-free Scaffolds in cartilage knee surgery: a systematic review and meta-analysis of clinical evidence. Cartilage. https://doi.org/10.1177/19476035198524061947603519852406
Azam A, Forster M, Robertson A (2018) Clinical and radiological outcome for Trufit Plug in the treatment of chondral and osteochondral lesions at a minimum of 2 years. J Orthop 15:47–51
Bedi A, Foo LF, Williams RJ 3rd, Potter HG (2010) The maturation of synthetic scaffolds for osteochondral donor sites of the knee: an MRI and T2-mapping analysis. Cartilage 1:20–28
Berruto M, Delcogliano M, de Caro F, Carimati G, Uboldi F, Ferrua P et al (2014) Treatment of large knee osteochondral lesions with a biomimetic Scaffold: results of a multicenter study of 49 patients at 2-year follow-up. Am J Sports Med 42:1607–1617
Berruto M, Ferrua P, Uboldi F, Pasqualotto S, Ferrara F, Carimati G et al (2016) Can a biomimetic osteochondral scaffold be a reliable alternative to prosthetic surgery in treating late-stage SPONK? Knee 23:936–941
Brix M, Kaipel M, Kellner R, Schreiner M, Apprich S, Boszotta H et al (2016) Successful osteoconduction but limited cartilage tissue quality following osteochondral repair by a cell-free multilayered nano-composite scaffold at the knee. Int Orthop 40:625–632
Bugelli G, Ascione F, Dell’Osso G, Zampa V, Giannotti S (2018) Biphasic bioresorbable scaffold (TruFit((R))) in knee osteochondral defects: 3-T MRI evaluation of osteointegration in patients with a 5-year minimum follow-up. Musculoskelet Surg 102:191–199
Chalmers PN, Vigneswaran H, Harris JD, Cole BJ (2013) Activity-related outcomes of articular cartilage surgery: a systematic review. Cartilage 4:193–203
Christensen BB, Foldager CB, Jensen J, Jensen NC, Lind M (2016) Poor osteochondral repair by a biomimetic collagen scaffold: 1- to 3-year clinical and radiological follow-up. Knee Surg Sports Traumatol Arthrosc 24:2380–2387
Condello V, Filardo G, Madonna V, Andriolo L, Screpis D, Bonomo M et al (2018) Use of a biomimetic Scaffold for the treatment of osteochondral lesions in early osteoarthritis. Biomed Res Int 2018:7937089
D’Ambrosi R, Giacco F, Ragone V, Ursino N (2019) Arthroscopic treatment of osteochondral knee defects with resorbable biphasic synthetic scaffold: clinical and radiological results and long-term survival analysis. Int Orthop 43:2183–2189
de Windt TS, Vonk LA, Brittberg M, Saris DB (2013) Treatment and prevention of (early) osteoarthritis using articular cartilage repair-fact or fiction? a systematic review. Cartilage 4:5S-12S
Delcogliano M, de Caro F, Scaravella E, Ziveri G, De Biase CF, Marotta D et al (2014) Use of innovative biomimetic scaffold in the treatment for large osteochondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc 22:1260–1269
Delcogliano M, Menghi A, Placella G, Speziali A, Cerulli G, Carimati G et al (2014) Treatment of osteochondritis dissecans of the knee with a biomimetic scaffold A prospective multicenter study. Joints 2:102–108
Dell’Osso G, Bottai V, Bugelli G, Manisco T, Cazzella N, Celli F et al (2016) The biphasic bioresorbable scaffold (Trufit((R))) in the osteochondral knee lesions: long-term clinical and MRI assessment in 30 patients. Musculoskelet Surg 100:93–96
Dhollander A, Verdonk P, Almqvist KF, Verdonk R, Victor J (2015) Clinical and MRI outcome of an osteochondral scaffold plug for the treatment of cartilage lesions in the knee. Acta Orthop Belg 81:629–638
Dhollander AA, Liekens K, Almqvist KF, Verdonk R, Lambrecht S, Elewaut D et al (2012) A pilot study of the use of an osteochondral scaffold plug for cartilage repair in the knee and how to deal with early clinical failures. Arthroscopy 28:225–233
Di Martino A, Kon E, Perdisa F, Sessa A, Filardo G, Neri MP et al (2015) Surgical treatment of early knee osteoarthritis with a cell-free osteochondral scaffold: results at 24 months of follow-up. Injury 46(Suppl 8):S33-38
Farr J, Gracitelli GC, Shah N, Chang EY, Gomoll AH (2016) High failure rate of a decellularized osteochondral allograft for the treatment of cartilage lesions. Am J Sports Med 44:2015–2022
Filardo G, Andriolo L, Angele P, Berruto M, Brittberg M, Condello V, et al. (2020) Scaffolds for knee chondral and osteochondral defects: indications for different clinical scenarios. A consensus statement. Cartilage. https://doi.org/10.1177/19476035198947291947603519894729
Filardo G, Andriolo L, Soler F, Berruto M, Ferrua P, Verdonk P et al (2019) Treatment of unstable knee osteochondritis dissecans in the young adult: results and limitations of surgical strategies-The advantages of allografts to address an osteochondral challenge. Knee Surg Sports Traumatol Arthrosc 27:1726–1738
Filardo G, Kon E, Di Martino A, Busacca M, Altadonna G, Marcacci M (2013) Treatment of knee osteochondritis dissecans with a cell-free biomimetic osteochondral scaffold: clinical and imaging evaluation at 2-year follow-up. Am J Sports Med 41:1786–1793
Filardo G, Kon E, Perdisa F, Balboni F, Marcacci M (2014) Autologous osteochondral transplantation for the treatment of knee lesions: results and limitations at two years' follow-up. Int Orthop 38:1905–1912
Filardo G, Kon E, Perdisa F, Di Matteo B, Di Martino A, Iacono F et al (2013) Osteochondral scaffold reconstruction for complex knee lesions: a comparative evaluation. Knee 20:570–576
Filardo G, Perdisa F, Roffi A, Marcacci M, Kon E (2016) Stem cells in articular cartilage regeneration. J Orthop Surg Res 11:42
Filardo G, Vannini F, Marcacci M, Andriolo L, Ferruzzi A, Giannini S et al (2013) Matrix-assisted autologous chondrocyte transplantation for cartilage regeneration in osteoarthritic knees: results and failures at midterm follow-up. Am J Sports Med 41:95–100
Gelber PE, Batista J, Millan-Billi A, Patthauer L, Vera S, Gomez-Masdeu M et al (2014) Magnetic resonance evaluation of TruFit(R) plugs for the treatment of osteochondral lesions of the knee shows the poor characteristics of the repair tissue. Knee 21:827–832
Gobbi A, Nunag P, Malinowski K (2005) Treatment of full thickness chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc 13:213–221
Gomoll AH, Filardo G, Almqvist FK, Bugbee WD, Jelic M, Monllau JC et al (2012) Surgical treatment for early osteoarthritis. Part II: allografts and concurrent procedures. Knee Surg Sports Traumatol Arthrosc 20:468–486
Gomoll AH, Madry H, Knutsen G, van Dijk N, Seil R, Brittberg M et al (2010) The subchondral bone in articular cartilage repair: current problems in the surgical management. Knee Surg Sports Traumatol Arthrosc 18:434–447
Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G et al (2005) A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 21:1066–1075
Guerin G, Pujol N (2020) Repair of large condylar osteochondral defects of the knee by collagen scaffold. Minimum two-year outcomes. Orthop Traumatol Surg Res 106:475–479
Hede K, Christensen BB, Olesen ML, Thomsen JS, Foldager CB, Lind MC (2020) CARGEL Bioscaffold improves cartilage repair tissue after bone marrow stimulation in a minipig model. J Exp Orthop 7:26
Hindle P, Hendry JL, Keating JF, Biant LC (2014) Autologous osteochondral mosaicplasty or TruFit plugs for cartilage repair. Knee Surg Sports Traumatol Arthrosc 22:1235–1240
Joshi N, Reverte-Vinaixa M, Diaz-Ferreiro EW, Dominguez-Oronoz R (2012) Synthetic resorbable scaffolds for the treatment of isolated patellofemoral cartilage defects in young patients: magnetic resonance imaging and clinical evaluation. Am J Sports Med 40:1289–1295
Kon E, Delcogliano M, Filardo G, Busacca M, Di Martino A, Marcacci M (2011) Novel nano-composite multilayered biomaterial for osteochondral regeneration: a pilot clinical trial. Am J Sports Med 39:1180–1190
Kon E, Di Matteo B, Verdonk P, Drobnic M, Dulic O, Gavrilovic G et al (2021) Aragonite-based Scaffold for the treatment of joint surface lesions in mild to moderate osteoarthritic knees: results of a 2-year multicenter prospective study. Am J Sports Med 49:588–598
Kon E, Filardo G, Brittberg M, Busacca M, Condello V, Engebretsen L et al (2018) A multilayer biomaterial for osteochondral regeneration shows superiority vs microfractures for the treatment of osteochondral lesions in a multicentre randomized trial at 2 years. Knee Surg Sports Traumatol Arthrosc 26:2704–2715
Kon E, Filardo G, Di Martino A, Busacca M, Moio A, Perdisa F et al (2014) Clinical results and MRI evolution of a nano-composite multilayered biomaterial for osteochondral regeneration at 5 years. Am J Sports Med 42:158–165
Kon E, Filardo G, Di Martino A, Marcacci M (2012) ACI and MACI. J Knee Surg 25:17–22
Kon E, Filardo G, Perdisa F, Di Martino A, Busacca M, Balboni F et al (2014) A one-step treatment for chondral and osteochondral knee defects: clinical results of a biomimetic scaffold implantation at 2 years of follow-up. J Mater Sci Mater Med 25:2437–2444
Kon E, Filardo G, Perdisa F, Venieri G, Marcacci M (2014) Clinical results of multilayered biomaterials for osteochondral regeneration. J Exp Orthop 1:10
Kon E, Filardo G, Roffi A, Andriolo L, Marcacci M (2012) New trends for knee cartilage regeneration: from cell-free scaffolds to mesenchymal stem cells. Curr Rev Musculoskelet Med 5:236–243
Kon E, Filardo G, Venieri G, Perdisa F, Marcacci M (2014) Tibial plateau lesions. Surface reconstruction with a biomimetic osteochondral scaffold: results at 2 years of follow-up. Injury 45 Suppl 6:S121-125
Kon E, Robinson D, Verdonk P, Drobnic M, Patrascu JM, Dulic O et al (2016) A novel aragonite-based scaffold for osteochondral regeneration: early experience on human implants and technical developments. Injury 47(Suppl 6):S27–S32
Kon E, Verdonk P, Condello V, Delcogliano M, Dhollander A, Filardo G et al (2009) Matrix-assisted autologous chondrocyte transplantation for the repair of cartilage defects of the knee: systematic clinical data review and study quality analysis. Am J Sports Med 37(Suppl 1):156S-166S
Krych AJ, Pareek A, King AH, Johnson NR, Stuart MJ, Williams RJ 3rd (2017) Return to sport after the surgical management of articular cartilage lesions in the knee: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 25:3186–3196
Lemoine M, Casey SM, O’Byrne JM, Kelly DJ, O’Brien FJ (2020) The development of natural polymer scaffold-based therapeutics for osteochondral repair. Biochem Soc Trans 48:1433–1445
Liu M, Yu X, Huang F, Cen S, Zhong G, Xiang Z (2013) Tissue engineering stratified scaffolds for articular cartilage and subchondral bone defects repair. Orthopedics 36:868–873
Lopa S, Madry H (2014) Bioinspired scaffolds for osteochondral regeneration. Tissue Eng Part A 20:2052–2076
Madry H, van Dijk CN, Mueller-Gerbl M (2010) The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc 18:419–433
Marcacci M, Filardo G, Kon E (2013) Treatment of cartilage lesions: what works and why? Injury 44(Suppl 1):S11-15
Martincic D, Leban J, Filardo G, Busacca M, Barlic A, Veber M et al (2021) Autologous chondrocytes versus filtered bone marrow mesenchymal stem/stromal cells for knee cartilage repair-a prospective study. Int Orthop 45:931–939
Mathis DT, Kaelin R, Rasch H, Arnold MP, Hirschmann MT (2018) Good clinical results but moderate osseointegration and defect filling of a cell-free multi-layered nano-composite scaffold for treatment of osteochondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc 26:1273–1280
Meng W, Gao L, Venkatesan JK, Wang G, Madry H, Cucchiarini M (2019) Translational applications of photopolymerizable hydrogels for cartilage repair. J Exp Orthop 6:47
Michael Borenstein LVH JPTHaHRR (2009) Introduction to meta-analysis.
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med 3:e123-130
Neyeloff JL, Fuchs SC, Moreira LB (2012) Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes 5:52
Pape D, Filardo G, Kon E, van Dijk CN, Madry H (2010) Disease-specific clinical problems associated with the subchondral bone. Knee Surg Sports Traumatol Arthrosc 18:448–462
Perdisa F, Filardo G, Sessa A, Busacca M, Zaffagnini S, Marcacci M et al (2017) One-step treatment for patellar cartilage defects with a cell-free osteochondral Scaffold: a prospective clinical and MRI evaluation. Am J Sports Med 45:1581–1588
Perdisa F, Gostynska N, Roffi A, Filardo G, Marcacci M, Kon E (2015) Adipose-derived mesenchymal stem cells for the treatment of articular cartilage: a systematic review on preclinical and clinical evidence. Stem Cells Int 2015:597652. https://doi.org/10.1155/2015/597652. Epub 2015 Jul 9.
Perdisa F, Kon E, Sessa A, Andriolo L, Busacca M, Marcacci M et al (2018) Treatment of knee osteochondritis dissecans with a cell-free biomimetic osteochondral Scaffold: clinical and imaging findings at midterm follow-up. Am J Sports Med 46:314–321
Robinson PG, Williamson T, Murray IR, Al-Hourani K, White TO (2020) Sporting participation following the operative management of chondral defects of the knee at mid-term follow up: a systematic review and meta-analysis. J Exp Orthop 7:76
Schreiner MM, Raudner M, Marlovits S, Bohndorf K, Weber M, Zalaudek M, et al. (2019) The MOCART (Magnetic Resonance Observation of Cartilage Repair Tissue) 2.0 Knee Score and Atlas. Cartilage. https://doi.org/10.1177/19476035198653081947603519865308
Sessa A, Andriolo L, Di Martino A, Romandini I, De Filippis R, Zaffagnini S, et al. (2019) Cell-Free Osteochondral Scaffold for the treatment of focal articular cartilage defects in early knee oa: 5 years' follow-up results. J Clin Med. 8.
Sessa A, Romandini I, Andriolo L, Di Martino A, Busacca M, Zaffagnini S et al (2020) Treatment of Juvenile knee osteochondritis dissecans with a cell-free biomimetic osteochondral scaffold: clinical and mri results at mid-term follow-up. Cartilage. https://doi.org/10.1177/19476035209545001947603520954500
Shivji FS, Mumith A, Yasen S, Melton JT, Wilson AJ (2020) Treatment of focal chondral lesions in the knee using a synthetic scaffold plug: long-term clinical and radiological results. J Orthop 20:12–16
Steinwachs MR, Gille J, Volz M, Anders S, Jakob R, De Girolamo L et al (2019) Systematic review and meta-analysis of the clinical evidence on the use of autologous matrix-induced chondrogenesis in the knee. Cartilage. https://doi.org/10.1177/19476035198708461947603519870846
Tampieri A, Sandri M, Landi E, Pressato D, Francioli S, Quarto R et al (2008) Design of graded biomimetic osteochondral composite scaffolds. Biomaterials 29:3539–3546
Van Genechten W, Vuylsteke K, Struijk C, Swinnen L, Verdonk P (2021) Joint surface lesions in the knee treated with an acellular aragonite-based scaffold: a 3-year follow-up case series. Cartilage. https://doi.org/10.1177/19476035209881641947603520988164
Verdonk P, Dhollander A, Almqvist KF, Verdonk R, Victor J (2015) Treatment of osteochondral lesions in the knee using a cell-free scaffold. Bone Joint J 97-B:318–323
Wang D, Nawabi DH, Krych AJ, Jones KJ, Nguyen J, Elbuluk AM, et al. (2020) Synthetic biphasic scaffolds versus microfracture for articular cartilage defects of the knee: a retrospective comparative study. Cartilage. https://doi.org/10.1177/19476035209034181947603520903418
Zaffagnini SBA, Andriolo L, Reale D, Busacca M, Di Martino A, Filardo G (2020) Mosaicplasty versus matrix-assisted autologous chondrocyte transplantation for knee cartilage defects: a long-term clinical and imaging evaluation. Appl Sci 10(13):4615
Acknowledgements
The authors would like to acknowledge Elettra Pignotti for her help with the statistical analysis.
Funding
No funding was available for the present study.
Author information
Authors and Affiliations
Contributions
Conceptualization, A.D.M and L.A.; methodology, A.P. and L.S; data curation, A.P. and L.S; writing—original draft preparation, A.B and L.S; writing—review and editing, D.R. and L.A.; supervision, A.D.M., L.A, and D.R. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No ethical committee approval or patient consent was needed due to the nature of the study.
Consent for publication
Not applicable.
Competing interests
All authors declare no support from any organisation for the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boffa, A., Solaro, L., Poggi, A. et al. Multi-layer cell-free scaffolds for osteochondral defects of the knee: a systematic review and meta-analysis of clinical evidence. J EXP ORTOP 8, 56 (2021). https://doi.org/10.1186/s40634-021-00377-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-021-00377-4