Abstract
Purpose
Several studies have shown an excellent success rate of communication enlargement surgery for popliteal cysts (Baker’s cysts). Ultrasound-guided surgery can improve the accuracy of this procedure and may lead to better outcomes. This study describes a simple ultrasound-guided arthroscopic technique to manage popliteal cysts and reduce postoperative pain.
Methods
After routine arthroscopic observation with a standard 2-portal approach, the arthroscope is redirected toward the posteromedial compartment from the anterolateral portal through the intercondylar notch. A posteromedial portal is then placed at this view. Subsequently, a contrast dye (indigo carmine) is injected into the popliteal cyst percutaneously using ultrasonography. This procedure makes it easier to find a capsular fold or valvular opening. The valvular opening between the semimembranosus and medial gastrocnemius is enlarged with a shaver and radiofrequency ablation. Cystectomy is not performed in any case. Finally, the irrigation fluid is suctioned, and the reduced cyst is visualized by ultrasound. Additionally, a periarticular multimodal drug injection is administered into the septum and inner wall of the cyst under ultrasound guidance.
Conclusions
Ultrasound-guided arthroscopic surgery for popliteal cysts can ensure reproducibility and be effective for postoperative pain relief. Thus, this combined procedure may be an optimal treatment option.
Similar content being viewed by others
Background
Popliteal cysts are characterized by the enlargement of the gastrocnemius-semimembranosus bursa in the posteromedial region of the knee [13]. They were first reported by Adams in 1840 [1], and Baker described in 1877 that this synovial cyst communicates with the knee joint and is often associated with other intra-articular lesions [3]. Accordingly, popliteal cysts are also known as Baker’s cysts. Pathologically, it has been reported that the enlargement of the gastrocnemius-semimembranosus bursa is caused by increased joint fluid in communication channels. These channels have a valvular mechanism at the capsular fold on the posteromedial capsule, promoting a continuous unidirectional flow between the posterior joint capsule and bursa [21, 24, 25]. The prevalence of communication channels between the gastrocnemius-semimembranosus bursa and the knee joint cavity in adults varies, and previous studies have reported that a connection was observed in 30–71% of subjects [4, 11, 13, 14, 16]. Although various treatment options, including conservative treatment, open surgical resection, and arthroscopic surgery, have been reported, the optimal surgical treatment remains uncertain. The recurrence rate after a simple open resection reportedly ranges between 42% to 63% [6, 8, 10, 25]. If the valvular mechanism is not corrected during surgery, a continuous flow of joint fluid will occur. This may be why the recurrence rate after open surgery remains high in various studies. Therefore, the key to a successful surgery is the closure or enlargement of the communication between the cyst and the articular cavity [30].
In recent years, good results have been reported using arthroscopic resection of the communication, also known as communication enlargement surgery, with a recurrence rate of less than 10% [2, 7, 20, 23, 28]. At our institution, communication enlargement surgeries have been performed with ultrasound guidance, which is a more reliable and less invasive procedure. Nevertheless, no report has described the indications and surgical techniques employed in this procedure. Appropriate indications and surgical techniques are important to achieve satisfactory results. Therefore, this report describes the indications and surgical techniques for ultrasound-guided arthroscopic communication enlargement surgery.
Indications for ultrasound-guided arthroscopic communication enlargement surgery
Ultrasound-guided arthroscopic surgery is commonly performed in symptomatic cases refractory to conservative treatment. For asymptomatic cases, we highly recommend supervised neglect; however, if the patient desires to undergo active treatment, the procedure can be performed, as described below. First, ultrasound-guided percutaneous treatment is performed, as described by Koroglu et al. [19]. Subsequently, after disinfection and local anesthesia induction, popliteal cysts are punctured using an 18G needle under ultrasonography. Ultrasound-guided puncture, aspiration, and corticosteroid injection are performed using a freehand technique by a well-experienced surgeon (K.G., 8 years of interventional ultrasonography experience) in our center. The cyst is almost completely decompressed, and 4 mg of Kenacort®□ (4 mg of triamcinolone acetonide) is subsequently administered into the cyst under ultrasound guidance. This treatment has a reported success rate of 87% and should be considered a first-line intervention since it is the most minimally invasive procedure [19, 29]. After 3 months of follow-up, surgical treatment is recommended in case of recurrence.
Surgical technique
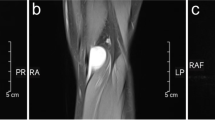
Two Wakasugi body supports (Mizuho, Bunkyo-ku, Tokyo, Japan) are attached to the side rails so that 80° of knee flexion can be maintained. Increased flexion of more than 80° makes it difficult to obtain ultrasound imaging from the posterior knee, which may lead to poor visualization. In contrast, a decreased flexion of less than 80° makes arthroscopic manipulation difficult and provides a poor arthroscopic view. Ultrasonography is used to reconfirm the location and measure the size of the cyst before surgery (Fig. 1 and Fig. 2a-b).
Ultrasound findings of the right knee before and after communication enlargement. a The short-axis view of the cyst (thin white arrow). b The long-axis view of the cyst and its size. c The size of the cyst is obviously reduced. d A periarticular multimodal drug is injected under ultrasonography (white arrow) to ensure postoperative pain relief. MG: medial gastrocnemius
A standard 2-portal approach is used for routine observation; if there is a lesion in the joint that needs to be treated, this is performed. Consequently, a camera is inserted into the posteromedial compartment from the anterolateral portal through the intercondylar notch, and a posteromedial portal is created. After creating the posteromedial portal, the shaver or radiofrequency ablation device is left in place in the joint. In this situation, the back of the knee is subjected to ultrasound, and the needle is inserted into the cyst under ultrasound guidance (Fig. 3). Subsequently, a contrast dye (approximately 10 mL of 0.4% indigo carmine) is injected into the popliteal cyst percutaneously; either the indigo carmine dye leaks out of the communication channel or, if not, the medial margin of the medial gastrocnemius is easily identified since the cyst dilates, making the fold more visible (Fig. 4a). The valve between the semimembranosus and medial gastrocnemius is enlarged using a shaver and radiofrequency ablation. Additionally, the goal of our arthroscopic surgery is to enlarge the communication channel to at least 6 cm long and 3 cm wide (Fig. 4b). Additional resection of the gastrocnemius medialis is never performed. Inner wall resection, called cystectomy, is not performed in any case. After the suction of the irrigation fluid, ultrasonography is immediately performed to confirm the disappearance of the inner cyst fluid (Fig. 2c), and a periarticular multimodal drug is injected under ultrasonography into the septum and inner cyst wall (Fig. 2d). Full knee range of motion and full weight-bearing are allowed from postoperative day 1.
Discussion
There are various treatment options available for popliteal cysts. While various studies have reported that conservative management of popliteal cysts results in a high rate of cyst persistence [12, 22], ultrasound-guided percutaneous treatment (ultrasound-guided puncture, aspiration, and corticosteroid injection) is one of the few acceptable treatment options, with a recurrence rate of 12.7%. We prefer this conservative treatment as an initial strategy. Historically, open surgery has been widely performed; however, the recurrence rate has been high, ranging from 42% to 63% [6, 8, 24]. In addition, there are concerns about cosmetic issues, wound pain, and wound complications due to the larger wound size.
A recent review reported that the arthroscopic management of intra-articular lesions and enlargement of the communication between the cyst and the articular cavity are effective strategies for popliteal cyst management [30]. Several studies have reported that arthroscopic surgery could allow the identification of the valve and communication enlargement [2, 23] without resection of the posterior horn of the medial meniscus, as first reported by Sansone et al. [28]. Moreover, the success rate of these arthroscopic enlargement procedures is better than that of arthroscopic closure surgeries (80 to 86.4%) [5, 15, 30] and simple open resection (37%) [25], reaching rates of 90 to 100% [2, 7, 17, 20, 23, 28] (Table 1). A meta-analysis by Zhou et al. [30] showed that the success rate of communication enlargement surgery was 96.7% regardless of the resection of the cyst wall, suggesting that it is an ideal strategy for popliteal cyst management.
The therapeutic benefit of inner wall resection, also described as cystectomy, remains controversial. In a review by Zhou et al. [30], the pooled success rate was 98.2% in the inner wall resection group, compared to 94.7% in the no resection group. However, the difference of approximately 3% was not statistically significant. Furthermore, there was a concern that an additional inner wall resection might increase complication rates. On the contrary, they similarly concluded that there may be a difference in long-term outcomes between the two groups. In a more recent study, Han et al. [12] compared clinical outcomes and complication rates between patients with and without cyst wall resection. Their meta-analysis showed that the recurrence rate was 0% and 6.4% in the cystectomy and the no-cystectomy groups, respectively. However, neither procedure showed an evident superiority over the other since arthroscopic cystectomy was associated with a relatively high incidence of complications. Based on these results, we did not resect the inner wall of the cyst; rather, we focused on enlarging the communication valve.
It remains unknown how large the posteromedial capsule should be resected. Previously, we had performed this procedure without an ultrasound and experienced a patient with recurrence who had undergone an enlargement of 4 cm in length and 2 cm in width. After this experience, we lengthened and widened the enlargement. There is no specific scientific evidence regarding the accurate resection size. Therefore, we enlarged the communication channel to at least 6 cm in length and 3 cm in width during the surgery. After this change, we have not experienced any cases of recurrence so far.
In adults, popliteal cysts are commonly associated with intra-articular disease, resulting in persistent and excessive synovial fluid production [9, 18]. Thus, several studies have demonstrated that the treatment of intra-articular lesions is equally important, and injuries to the medial meniscus and articular cartilage were the most common joint lesions [9, 18, 27]. However, in 16 cases wherein only the intra-articular lesions were treated, favorable therapeutic efficacy was achieved in only 5 patients [26]. Therefore, this suggests that a more important aspect of surgery is to enlarge the communication channels [30]. Nevertheless, symptomatic meniscal or cartilage lesions that are identified arthroscopically at initial routine observation should be treated as needed [2, 30].
Ultrasound-guided surgery has 3 advantages. First, it makes the injection of a contrast dye into the cyst more reliable while allowing for simultaneous accurate identification of the cyst. Similarly, it avoids the risk of neurovascular injury due to erroneous punctures, which is useful in terms of safety. Second, it is possible to evaluate the insides of the cyst immediately after the communication enlargement procedures. Complex cysts are characterized by septation [19], and the necessity of additional procedures, such as resection of the septum, can be determined intraoperatively. Finally, ultrasound-guided multimodal drug injection can supposedly provide a high degree of pain relief. In fact, many of our patients have achieved unassisted gait on the following day without postoperative pain.
Only two patients had undergone this new surgical technique with extremely short-term outcomes (4 and 2 months postoperatively). Although both patients have not shown any symptoms or signs of recurrence, the evaluation of more patients with a longer follow-up period is needed to report our clinical outcomes. However, according to previous literature, it is clear that arthroscopic enlargement surgery can obtain good clinical outcomes with a low recurrence rate [2, 7, 17, 20, 23, 28]. Therefore, we would like to focus our study on this new ultrasound-guided surgical technique for the treatment of popliteal cysts.
Conclusion
Ultrasound-guided arthroscopic communication enlargement surgery for popliteal cysts can ensure procedure reproducibility with low recurrence rates and be effective for postoperative pain relief. Thus, this combined technique may be an optimal treatment for popliteal cysts.
Availability of data and materials
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
References
Adams R (1840) Chronic rheumatic arthritis of the knee joint. Dublin J Med Sci 17:520–522
Ahn JH, Lee SH, Yoo JC, Chang MJ, Park YS (2010) Arthroscopic treatment of popliteal cysts: clinical and magnetic resonance imaging results. Arthroscopy 26:1340–1347. https://doi.org/10.1016/j.arthro.2010.02.012
Baker WM (1877) On the formation of the synovial cysts in the leg in connection with disease of the knee joint. St Barth Hosp Rep 13:245–261
Bickel WH, Burleson RJ, Dahlin DC (1956) Popliteal cyst; a clinicopathological survey. J Bone Joint Surg Am 38-A:1256–1274
Calvisi V, Lupparelli S, Giuliana P (2007) Arthroscopic all-inside suture of symptomatic Baker's cyst: a technical option for surgical treatment in adults. Knee Surg Sports Traumatol Arthrosc 15:1452–1460. https://doi.org/10.1007/s00167-007-0383-z
Childress HM (1970) Popliteal cysts associated with undiagnosed posterior lesions of the medial meniscus. The significance of age in diagnosis and treatment. J Bone Joint Surg Am 52:1487–1492
Cho JH (2012) Clinical results of direct arthroscopic excision of popliteal cyst using a posteromedial portal. Knee Surg Relat Res 24:235–240. https://doi.org/10.5792/ksrr.2012.24.4.235
Dinham JM (1975) Popliteal cysts in children. The case against surgery. J Bone Joint Surg Br 57:69–71
Field JR, Franklin PD, Kustan J (1991) Popliteal cysts: a reassessment using magnetic resonance imaging. Skelet Radiol 20:433–435
Fritschy D, Fasel J, Imbert JC, Bianchi S, Verdonk R, Wirth CJ (2006) The popliteal cyst. Knee Surg Sports Traumatol Arthrosc 14:623–628. https://doi.org/10.1007/s00167-005-0028-z
Gristina AG, Wilson PD (1964) Popliteal cysts in adults and children. A review of 90 cases. Arch Surg 88:357–363
Han JH, Bae JH, Nha KW et al (2019) A clinical study of arthroscopic cystectomy on popliteal cysts associated with rheumatoid arthritis. Knee Surg Relat Res 31:103–112. https://doi.org/10.5792/ksrr.18.068
Handy JR (2001) Popliteal cysts in adults: a review. Semin Arthritis Rheum 31:108–118
Hoffman BK (1963) Cystic lesions of the popliteal space. Surg Gynecol Obset 116:551–558
Hughston JC, Baker CL, Mello W (1991) Popliteal cyst: a surgical approach. Orthopedics 14:147–150
Jayson MI (1968) Study of a valvular mechanism in the formation of synovial cysts. Ann Phys Med 9:243–245
Ji JH, Kim WY, Park SE, Shin ES, Moon CY (2009) Arthroscopic treatment of popliteal cysts using the transseptal approach. J Korean Knee Soc 21:158–164
Johnson LL, van Dyk GE, Johnson CA, Bays BM, Gully SM (1997) The popliteal bursa (Baker’s cyst): an arthroscopic perspective and the epidemiology. Arthroscopy 13:66–72
Köroğlu M, Callıoğlu M, Eriş HN et al (2012) Ultrasound guided percutaneous treatment and follow-up of Baker's cyst in knee osteoarthritis. Eur J Radiol 81:3466–3471. https://doi.org/10.1016/j.ejrad.2012.05.015
Lie C, Ng TP (2011) Arthroscopic treatment of popliteal cyst. Hong Kong Med J 17:180–183
Lindgren PG (1978) Gastrocnemio-semimembranosus bursa and its relation to the knee joing. III. Pressure measurements in joint and bursa. Acta Radiol Diagn (Stockh) 16:377–388
Malinowski K, Koniarski A, Synder M (2009) Popliteal cyst: comparison of complete endoscopic to intensive nonoperative treatment (SS51). Arthroscopy 25:e28
Ohishi T, Takahashi M, Suzuki D et al (2015) Treatment of popliteal cysts via arthroscopic enlargement of unidirectional valvular slits. Mod Rheumatol 25:772–778. https://doi.org/10.3109/14397595.2015.1008779
Rauschning W, Lindgren PG (1980) Anatomy and function of the communication between knee joint and popliteal bursae. Ann Rheum Dis 39:354–358
Rauschning W, Lindgren PG (1979) The clinical significance of the valve mechanism in communicating popliteal cysts. Arch Orthop Trauma Surg 95:251–256
Rupp S, Seil R, Jochum P, Kohn D (2002) Popliteal cysts in adults. Prevalence, associated intraarticular lesions, and results after arthroscopic treatment. Am J Sports Med 30:112–115. https://doi.org/10.1177/03635465020300010401
Sansone V, De Ponti A, Paluello GM, Del Maschio A (1995) Popliteal cysts and associated disorders of the knee: critical review with MR imaging. Int Orthop 19:275–279
Sansone V, De Ponti A (1999) Arthroscopic treatment of popliteal cyst and associated intra-articular knee disorders in adults. Arthroscopy 15:368–372
Smith MK, Lesniak B, Baraga MG, Kaplan L, Jose J (2015) Treatment of popliteal (Baker) cysts with ultrasound-guided aspiration, fenestration, and injection: long-term follow-up. Sports Health 7:409–414. https://doi.org/10.1177/1941738115585520
Zhou XN, Li B, Wang JS, Bai LH (2016) Surgical treatment of popliteal cyst: a systematic review and meta-analysis. J Orthop Surg Res 11:22. https://doi.org/10.1186/s13018-016-0356-3
Acknowledgements
We would like to thank Editage (http://www.editage.com) for the English language editing and reviewing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing and revision of this manuscript. GK developed the study design and drafted the manuscript. GK collected and provided data. SI supervised this study. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by our Institutional Review Board. Written informed consent was obtained from both patients for the publication of this case series and the accompanying images.
Consent for publication
Written informed consent was obtained from both patients for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goto, K., Saku, I. Ultrasound-guided arthroscopic communication enlargement surgery may be an ideal treatment option for popliteal cysts – indications and technique. J EXP ORTOP 7, 93 (2020). https://doi.org/10.1186/s40634-020-00314-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-020-00314-x