Abstract
Large animal models play a crucial role in sports surgery of the knee, as they are critical for the exploration of new experimental strategies and the clinical translation of novel techniques. The purpose of this contribution is to provide critical aspects of relevant animal models in this field, with a focus on paediatric anterior cruciate ligament (ACL) reconstruction, high tibial osteotomy, and articular cartilage repair. Although there is no single large animal model strictly replicating the human knee joint, the sheep stifle joint shares strong similarities. Studies in large animal models of paediatric ACL reconstruction identified specific risk factors associated with the different surgical techniques. The sheep model of high tibial osteotomy is a powerful new tool to advance the understanding of the effect of axial alignment on the lower extremity on specific issues of the knee joint. Large animal models of both focal chondral and osteochondral defects and of osteoarthritis have brought new findings about the mechanisms of cartilage repair and treatment options. The clinical application of a magnetic device for targeted cell delivery serves as a suitable example of how data from such animal models are directly translated into in clinical cartilage repair. As novel insights from studies in these translational models will advance the basic science, close cooperation in this important field of clinical translation will improve current reconstructive surgical options and open novel avenues for regenerative therapies of musculoskeletal disorders.
Similar content being viewed by others
Introduction
Large animal models play a crucial role in orthopaedic sports surgery, as they are critical for the exploration of new experimental strategies and the clinical translation of novel techniques (Espregueira-Mendes & Karahan 2014). On December 3rd, 2014, about 100 clinicians and basic scientists from Europe, North America, and Asia, met on the occasion of the Research Day of the Annual Congress of the Société Française d’Arthroscopie in Luxembourg to discuss requirements for such translational animal models (Table 1). This research day was organized together with the Cartilage Net of the Greater Region, a multinational forum for exploring basic scientific and translational research, development and clinical applications in the diverse field of articular cartilage.
The purpose of this contribution is to provide critical aspects of relevant animal models in experimental knee sports surgery, including paediatric anterior cruciate ligament (ACL) reconstruction, high tibial osteotomy, and articular cartilage repair. These three models discussed are based on the individual presentations (Table 1) and thought to provide a representative and clinically relevant, although by no means exhaustive selection of translational animal models in this field. This paper is aimed at the diverse community of those engaging in experimental orthopaedics, among which orthopaedic surgeons, biomaterial scientists, cell and molecular biologists, biochemists, biotechnologists, and biomechanical engineers. It intends to highlight new developments and to display how far knowledge gathered from these models is already (or will be in the near future) translatable in humans. An emphasis is placed on the “transferability” to patients.
General requirements for translational animal models in experimental orthopaedics and sports medicine
General requirements for large animal experiments in translational orthopaedic research are manifold: 1) the model needs to be comparable to the human species, 2) comparison data need to be available, 3) the results must be transferable, 4) surgery must be technically feasible, 5) a specialized animal facility must be available with acceptable related expenditures, 6) animals need to be affordable and available, 7) surgery should be ethically accepted, and finally 8) anaesthesia, surgery, and rehabilitation need to be tolerated by the selected animals. Nevertheless, for the human knee joint, no gold standard exists, as the models differ in many important structural and functional aspects compared with the clinical situation (Poole et al. 2010). There is no large animal model replicating the human knee joint perfectly (Aigner et al. 2010). In addition, the activity pattern of animals is different compared with the bipedal locomotion of humans. For example, their quadruped gait results in altered biomechanics compared to the human knee (Rudert et al. 2000), together with differences in the knee range of motion and resting positions. Also, the biomechanical properties of knee joint cartilage are species-specific (Simon 1971), resulting in significant differences of the mechanical properties (Athanasiou et al. 1991).
Review
Large animal models for paediatric anterior cruciate ligament reconstruction
The treatment of ligamentous ACL lesions in the paediatric population causes a therapeutic dilemma for physicians because of the lack of current international guidelines. To overcome this problem, a variety of experimental studies concerning the growth plates and paediatric ACL reconstruction have been performed in small and large animal models (Edwards et al. 2001; Guzzanti et al. 1994; Janarv et al. 1998; Ono et al. 1998; Meller et al. 2009a; Meller et al. 2009b; Meller et al. 2008a; Meller et al. 2008b; Seil et al. 2008; Stadelmaier et al. 1995). The complexity of paediatric ACL reconstruction makes the interpretation of this surgical technique and the transferability of its results to humans difficult when small animal models are used. However, there are strong similarities between the stifle joint and the human knee joint. From an anatomical point of view, these joints have asymmetric collateral as well as cruciate ligaments and menisci and the articulating surface is covered with articular cartilage (Dye 1987; Arnoczky & Marshall 1977; Bosch & Kasperczyk 1993). Based on our own experiments (Seil et al. 2008), the sheep model seems to be appealing for the above-mentioned study purpose. Merino sheep are easily available, they are easy to handle and are ethically better accepted than dogs or primates (Allen et al. 1998). Three gross anatomic features have the potential to interfere with ACL surgery and must be known by the surgeon to avoid potential pitfalls: the very narrow intercondylar notch of this species, the different -much more undulating- form of the distal femoral growth plate in comparison to the human knee and the range of motion of the stifle joint with spontaneous 30-40° extension deficit.
Paediatric ligamentous ACL injuries do rarely occur before the age of 8 or 9 years (Chotel et al. 2013). Therefore, a critical point to perform ACL reconstructions in growing sheep is the fact that surgery should be performed at a moment corresponding to the age where ligamentous ACL injuries in children appear to be the most frequent and problematic. In their early growth studies in humans, Bailey and Pinneau showed that at a skeletal age between 8 and 12 years, humans reach 79-92% of their adult height in females and 72-83% in males (Bayley & Pinneau 1952). In the absence of precise data from veterinary studies, sheep should therefore ideally be operated when they reach between 70% and 90% of the adult height. However, information on animals is rarely available (Salomon 2001). Studies on the longitudinal growth of the sheep forearm revealed that they reached 70% of their adult height at day 20 and 90% at day 167 (Salomon 2001). Supposing that these data could be transferred to the hind limb of this species, the use of 4-months old sheep appears justified, and grossly 4 cm of longitudinal hind limb growth could be expected at this age (Seil 2003). This sheep model was used to evaluate the risk for growth disturbances of transphyseal drilling and ACL reconstruction (Seil et al. 2008). Three technical variants were used. In group I, the ACL was resected and 5-mm tunnels were drilled and left empty in four-months-old Merino sheep. Unilateral ACL reconstruction using an autologous Achilles tendon graft and rigid button fixation was performed in group II. A double-stranded graft with a diameter of 5 mm was used in group II-A, and a single stranded graft with a diameter of 3 mm in group II-B. The tunnel diameter was 5 mm in both groups. Six months after the procedure, the combination of peripheral, posterolateral growth plate injuries and empty tunnels led to severe growth deformities on the femoral side with a shortening of the lateral femur of 8 mm (7–10 mm), a valgus deformity of 12.8° (12-14°) and a flexion deformity of 8.6° (5-15°). Histological examination revealed a strong bone bridge formation over the physis and an injury to the perichondral structures. Central growth plate lesions on the tibia did not induce growth abnormalities. Transphyseal ACL replacements did not cause clinically relevant growth disturbances, neither on the tibia, nor on the femur, even if the drilling injury damaged the perichondral structures on the posterolateral physis.
Clinical relevance for paediatric anterior cruciate ligament reconstruction
This study showed that the sheep model is useful to analyze the outcome of paediatric ACL reconstruction with open growth plates. In terms of risk for growth changes, we identified major differences between femoral and tibial growth plate injuries caused by tunnel drilling. On the tibial side the central positioning of the drill hole in the proximal tibial growth plate appeared to be safe in terms of growth abnormalities. On the femoral side, however, the eccentrically placed femoral tunnel is at risk to injure the periphery of the growth plate. In the paediatric knee, this may either occur during the drilling procedure, for instance if the posterior wall of the tunnel gets injured (posterior blow-out) or if the surgeon chooses to perform an extraepiphyseal graft placement during which this zone might be rasped for better graft adherence to the bone (Kocher et al. 2002). Injuries of the perichondral structures have shown to be at risk to develop major growth abnormalities due to an asymmetric remaining growth (Koman & Sanders 1999; Robert & Casin 2010; Kocher et al. 2002; Chotel & Seil 2013). In the Ogden classification, they are classified as type VI injuries and correspond to a localized peripheral bone bridge (Ogden 1981).
Furthermore, large animal models showed that filling the tunnels with tendon grafts prevented growth abnormalities in transphyseal ACL replacement procedures. Several other studies confirmed the suitability of this model for the study of paediatric ACL reconstruction (Meller et al. 2009a; Meller et al. 2009b; Meller et al. 2008a; Meller et al. 2008b).
The preclinical sheep model of high tibial osteotomy
HTO is an excellent alternative to knee arthroplasty, especially for younger and physically active patients with knee OA of the medial tibiofemoral compartment and varus malalignment (Brinkman et al. 2008; Pape et al. 2010; Lobenhoffer & Agneskirchner 2003a; Lobenhoffer & Agneskirchner 2014; W-Dahl et al. 2012; Prodromos et al. 2015). The weightbearing axis is shifted away from the medial compartment. Consequently, the load distribution between the medial and lateral compartments of the knee is altered (Van Thiel et al. 2011). Loading is transferred towards the lateral tibiofemoral compartment -especially when a valgus overcorrection is performed- and loading of the medial compartment is decreased (Agneskirchner et al. 2007). Preclinical large animal models of HTO can be used to test different types of osteotomies and to evaluate the effects of lower limb alignment on the reconstructive therapy of articular cartilage lesions and on the development and progression of OA. Traditionally, our experimental knowledge about osteotomies was chiefly based on cadaver studies (Agneskirchner et al. 2007; Lim et al. 2011), models of below-knee amputation or femur valgus osteotomy in guinea-pigs (Wei et al. 2001), on data from cartilage samples obtained from patients undergoing total knee replacement (Otsuki et al. 2008; Wei et al. 2001) and on CT-osteoabsorptiometric investigations in patients (Muller-Gerbl et al. 1992; Madry et al. 2010). More recently, the sheep has emerged as a suitable preclinical animal model of HTO (Pape & Madry 2013). In these studies, adult Merino sheep underwent an HTO of their tibiae. Either a medial open-wedge technique inducing a normal and an excessive valgus alignment or a closed-wedge technique inducing a varus alignment were applied (Table 2). Relevant steps of the surgical technique were essentially performed according to the clinical recommendations of osteotomy experts (Lobenhoffer & Agneskirchner 2003b). During the course of the surgeries, no intraoperative complications occurred, and the popliteal artery and femoral vein were never injured. Some species-specific complications emerged in the post-operative course (Table 3). These included instability of the osteotomy which occurred as a consequence of performing a classical monocortical fixation of the three proximal screws of the implant as in patients. Also, chronic patella dislocation was seen, caused by excessive valgus osteotomy and subsequently insufficient closure after medial arthrotomy, and intraarticular infection. Taken these specific complications into account, the following surgical principles were identified as a prerequisite for solid bone healing and the maintenance of the correction in sheep: 1) a medial and longitudinal approach to the proximal tibia, 2) biplanar osteotomy to increase the initial rotatory stability regardless of the direction of correction (Pape et al. 2011), 3) application of a small, narrow but long implant with locking screws (e.g. small stature HTO plate; Synthes, Umkirch, Germany), 4) posterior plate placement to avoid slope changes, and 5) use of bicortical screws to account for the brittle bone of the tibial head and to avoid tibial head displacement (Tables 2 and 3). Thus, although successful HTO in sheep is complex and requires attention to these principles, the sheep represents because of its similarities with humans (Allen et al. 1998) an elegant model to induce axial malalignment in a clinically relevant environment, and osteotomy healing under challenging mechanical conditions (Pape & Madry 2013).
Clinical relevance for high tibial osteotomy
Published studies using this model have focused so far on the effect of axial alignment on the lateral tibiofemoral compartment. Specifically, effects on the articular cartilage and the development of OA, the lateral meniscus and the subchondral bone were investigated (Madry et al. 2013b; Madry et al. 2014b; Ziegler et al. 2013; Ziegler et al. 2014). The data first revealed interesting and specific topographical relationships that are present in the central region of lateral tibiofemoral compartment, regardless of correction. For example, there exists a correlation between the thickness of the articular cartilage layer and the subchondral bone. The important protective role of the lateral meniscus for the cartilage (Beaufils et al. 2006) is reflected in the correlation of thickness between the articular cartilage in the submeniscal periphery and the lateral meniscus. The clinical observation that cartilage lesions proceed much faster after lateral than after medial meniscectomy, and that the clinical outcomes of lateral meniscectomy are significantly worse than after medial meniscectomy underscore the delicate balance between the lateral meniscus and the articular cartilage (Bolano & Grana 1993; Hoser et al. 2001; Macnicol & Thomas 2000; Scheller et al. 2001; Heijink et al. 2012).
As valgus HTO leads to an increase in the pressure in the lateral compartment, the subsequent question was whether HTO results in structural changes in the lateral tibiofemoral osteochondral unit and lateral meniscus, and whether these changes depend in the extent of correction; reflective of the pressure in the lateral compartment. Importantly, the pressure increase in the lateral compartment following standard correction valgus HTO (with 4.5° tibial valgus) did not lead to mid-term morphological alterations in the lateral tibiofemoral compartment. In contrast, the higher increase in pressure following valgus overcorrection (with 9.5° tibial valgus) induced adaptive subchondral bone changes, reflected by an increased specific bone surface (BS/BV) in the subarticular spongiosa compared with unloading by varisation. Also, in the lateral menisci, a decrease in the number of cells in the red–red (peripheral) zone of the middle third was noted, however without structural changes (such as meniscal lesions). The lateral meniscus (Beaufils et al. 2006) is of specific importance, since the peak contact stress and maximum shear stress in the cartilage increased 200% more after a lateral than a medial meniscectomy under axial femoral compressive loads (Pena et al. 2006). Altogether, these results show that for the clinical situation, opening wedge HTO is a safe surgical procedure for the lateral tibial osteochondral unit and the lateral meniscus.
Animal models for cartilage repair
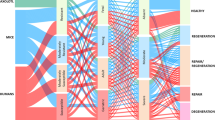
Animal models for articular cartilage repair are vital for basic scientific and translational studies (Hunziker 2009; Blaney Davidson et al. 2014). They need to reflect the different appearances and aetiologies of cartilage defects, which may be caused by OA, trauma, osteochondritis dissecans, and osteonecrosis (Madry et al. 2010). Such models may be used to study spontaneous cartilage repair or improved reconstructive surgical options. These currently include the removal or refixation of chondral or osteochondral fragments, autologous or allogeneic osteochondral transplantation, marrow stimulation, articular chondrocyte implantation, or HTO (Hunziker 2002; Madry et al. 2011). Importantly, the difference between focal, non-OA cartilage defects and the often ill-defined OA lesions needs to be appreciated (Figure 1). Focal defects are usually surrounded by a normal cartilaginous tissue, while OA lesions are often larger in size and thus may affect the entire joint surface and are of different depths (Madry et al. 2011; Pritzker et al. 2006). Animal models also play an important role in evaluating novel experimental treatments (Cucchiarini et al. 2014), such as application of bioinspired scaffolds or defined cell populations (Henderson & La Valette 2005; Deie et al. 2007; Bosch & Kasperczyk 1993; Frisbie et al. 2006b).
When contemplating on the use of animal models of articular cartilage defects, the important difference between focal, non-OA cartilage defects and OA lesions needs to be kept in mind. Focal defects are usually surrounded by a normal cartilaginous tissue (left side, shown is a lesion caused by osteochondritis dissecans of the human knee). The often ill-defined OA lesions are often larger in size and may affect the entire joint (right side, shown is a case of tricompartimental osteoarthritis of the human knee).
Focal cartilage defect models can be created in a variety of small and large animals, among which the mouse, rat, rabbit, dog, minipig, sheep, goat, and horse (Hunziker 1999b; Hunziker 1999a; Hunziker 2000; Hunziker 2009). Major considerations of focal articular cartilage defect models are summarized in Table 4. Here, not only the cartilage thickness is important, but also cartilage microstructure such as cellularity (Aigner et al. 2010; Poole et al. 2010), the age of animals, defect size, depth, anatomy, and subchondral bone plate thickness (Chevrier et al. 2015). For example, a full-thickness chondral defect does not extend into the subchondral bone, but merely ends at the junction of calcified cartilage and the subchondral bone plate (Figure 2) (Frisbie et al. 2006b; Hunziker 1999b; Madry et al. 2010).
Classification of cartilage defects. Both partial- and full-thickness chondral defects involve, by definition, only the cartilage layer. Osteochondral defects extend through the subchondral bone plate into the subchondral bone. Light blue: articular cartilage; dark blue: calcified cartilage; dark orange: subchondral bone plate; orange: subarticular spongiosa.
Goat, sheep, minipigs, and horses are well suited to induce chondral defects (Hunziker 1999b; Hunziker 1999a; Hunziker 2000; Hunziker 2009). Particular attention has to be paid to a meticulous surgical technique when creating chondral defect models, as the defect should not extend into the subchondral bone (Frisbie et al. 2006b; Frisbie et al. 2006a; Drobnic et al. 2010). Reflecting this important point, displaying in a publication a photomicrograph of a histological section of the chondral defect resulting from the surgical technique applied in an ex vivo setting of the animal model might, in some cases, be helpful to see how deep the created lesion extends. The spontaneous repair of chondral defects is rather limited, as Hunziker and Rosenberg have shown that only a few cells from the synovial membrane migrate into the lesion over time (Hunziker & Rosenberg 1996). In contrast, when marrow stimulation is applied at the base of those defects by Pridie drilling (Smillie 1957; Pridie 1959), microfracture (Steadman et al. 2001), or abrasion arthroplasty (Johnson 2001), pluripotent progenitor cells from the subchondral bone marrow migrate into the defect, differentiate into chondrocytes, and form a cartilaginous repair tissue (Frisbie et al. 1999; Frisbie et al. 2003; Shapiro et al. 1993). Interestingly, articular cartilage repair depends also on the topographic location of the defect. Clinical investigations indicate that the femoral condyles and the trochlear groove are the key locations where articular cartilage defects occur (Hjelle et al. 2002; Curl et al. 1997), and that small chondral lesions in the human femoral condyles repair better than in the trochlea (Kreuz et al. 2006b). This finding is not always reflected in the animal models. For example, articular cartilage repair in sheep is better at the trochlea than at the condyle, and therefore the repair pattern of the sheep trochlea is more reflective of the human femoral condyle (Orth et al. 2013c).
A recent focus has been to simultaneously investigate the subchondral bone in the context of osteochondral repair (Chen et al. 2011; Chen et al. 2009; Hoemann et al. 2012; Madry 2010; Goebel et al. 2012; Orth et al. 2013a; Orth et al. 2013b; Orth et al. 2012b). Data from large animal models have shown that subchondral bone changes such as the upward migration of the subchondral bone plate, intralesional osteophytes, subchondral bone cysts, and a generalized impairment of the osseous microarchitecture below the defect persist for a longer period of time than previously acknowledged (Orth et al. 2013a). Osteochondral defects, in contrast to partial- or full-thickness chondral defects, heal with the sequence of osteochondral repair (Orth et al. 2012a; Shapiro et al. 1993). Current translational studies have shown a variety of subchondral bone changes which are associated with osteochondral repair, among which the upward migration of the subchondral bone plate, the formation of intralesional osteophytes, the appearance of subchondral bone cysts, and generalized changes of the subchondral bone microarchitecture (Qiu et al. 2003; Orth et al. 2013a; Chen et al. 2009; Chen et al. 2011). These spatial and temporal alterations proceed in a defined manner (Orth et al. 2012a). Clinical studies in patients have identified similar changes of the subchondral bone below a cartilage lesion (Niemeyer et al. 2015; Bert 2015; Gomoll et al. 2010). These chiefly include the upward migration of the subchondral bone plate, intralesional osteophytes, and subchondral bone cysts (Orth et al. 2013a; Niemeyer et al. 2015; Bert 2015). Whether their development over the long-term shows a similar pattern as seen in animal models remains to be elucidated. Also, the relationship of these alterations to the degradation of the cartilaginous repair tissue remains elusive. While many animal studies did not find a correlation between the structural quality of the cartilaginous repair tissue and the advancement of the subchondral bone plate, our current understanding on the (long-term) clinical effect of such subchondral bone changes is even more limited (Niemeyer et al. 2015; Bert 2015; Sansone et al. 2015; Orth et al. 2013a; Cole et al. 2011; Vasiliadis et al. 2010; Brown et al. 2004; Kreuz et al. 2006a; Mithoefer et al. 2005; Saris et al. 2009; Dhollander et al. 2011; Henderson & La Valette 2005).
OA models are mainly established in the mouse, rat, guinea pig, rabbit, sheep, goat, and horse (Little & Zaki 2012). Notably, the Osteoarthritis Research Society International (OARSI) devoted an entire issue of their journal Osteoarthritis Cartilage for recommendations for the use of animal models in the study of OA (Johnstone et al. 1998; Agung et al. 2006). In general, utmost importance has to be given to the selection of the method for an OA induction, as this should reflect the clinical entity which is studied (Cook et al. 2010; Gerwin et al. 2010; Glasson et al. 2010; Kraus et al. 2010; Laverty et al. 2010; Little et al. 2010; McIlwraith et al. 2010). Moreover, the time of therapeutic intervention has to be carefully selected following or during OA induction.
To evaluate experimental osteochondral repair, a large variety of methods can be used and should be applied simultaneously. These include, but are not limited to macroscopic evaluation of the repair tissue and the treated joint (Goebel et al. 2012), non destructive structure evaluation by high field MRI (Goebel et al. 2014) and micro CT (Eldracher et al. 2014), biochemical (Kiss et al. 2014) and molecular biological evaluation of the repair tissue (Cucchiarini & Madry 2014), and histological (Orth et al. 2012c), and immunohistochemical evaluations (Madry et al. 2013a). Histological scoring remains the gold standard (Getgood et al. 2014). Here, both elementary and comprehensive histological scores are well suited to quantify the structure of cartilaginous repair tissue (Orth et al. 2012c). Interestingly, when evaluating osteochondral repair, only the Sellers and the Pineda score allow for an assessment of the osteochondral junction in subchondral bone (Sellers et al. 1997; Pineda et al. 1992). Close attention should be paid to sample size requirements, as a bilateral research design (where cartilage defects are established in both joints of the same animal) reduces sample sizes (Orth et al. 2013d). Recently, high field MRI at 9.4 Tesla has been shown to correlate with macroscopic and histological scoring (Goebel et al. 2014; Goebel et al. 2012). When performing micro CT analysis of the subchondral bone, a separation of the subchondral bone into subchondral bone plate and subarticular spongiosa, based on their anatomy, appears useful (Orth et al. 2012b). In the context of OA, similar principles apply, with the additional focus of the evaluation of the synovial membrane (Pastoureau et al. 2010).
Clinical application of a magnetic device for targeted cell delivery in cartilage repair
The clinical application of a magnetic device for targeted cell delivery in cartilage repair serves as a suitable example of how data from animal models are directly translated into clinical cartilage repair (Cucchiarini et al. 2014). Current cartilage repair techniques do suffer from two weak points (Johnstone et al. 2013). One weak point is that the number of mesenchymal stem cells (MSCs) obtained in the knee with an arthroscopic procedure is limited (Min et al. 2013). The simplest strategy to increase the number of the cells is the intra-articular injection of MSCs after increase of autologous MSCs by cultivation (Frisch et al. 2014). MSCs are the cell population of undifferentiated cells isolated from adult tissue that have the capacity to differentiate into mesodermal lineages, such as bone, cartilage, fat, muscle or other tissues (Johnstone et al. 1998; Johnstone & Yoo 1999). MSCs from the bone marrow can be cultured and differentiated into the desired lineage in vitro with the application of specific growth factors or bioactive molecules (Zellner et al. 2014). Intra-articular injection of too many MSCs, however, generated free bodies of scar tissue (Agung et al. 2006). A novel stem cell delivery system for cartilage repair using magnetically labelled MSCs and an external magnetic device was therefore developed, aiming at accumulating a relatively small number of MSCs to a desired location. Ferumoxides are dextran-coated superparamagnetic iron oxide nanoparticles approved by the US Food and Drug Administration (FDA) as a magnetic resonance contrast agent by intravenous injection for hepatic imaging of humans (Wang et al. 2001). By employing ferumoxides, it is easy to generate magnetically labelled MSCs. The ability to deliver magnetically labelled MSCs to a cartilage defect that is a desired place under arthroscopy was demonstrated in rabbit and swine knee joints using an external magnetic device at 0.6 Tesla (Kobayashi et al. 2008).
This result indicates that this minimally invasive system under arthroscopy can be applicable for a focal osteochondral defect in the knee joint. The next step was to examine if this external magnetic system is effective for OA. Here, the question was investigated if a cartilage layer on degenerated human cartilage could successfully be regenerated in vitro using this external magnetic system (Kobayashi et al. 2009). MSCs from human bone marrow were cultured and magnetically labelled. Degenerated human cartilage was obtained during total knee arthroplasty. The osteochondral fragments were attached to the sidewall of tissue culture flasks, and magnetically labelled MSCs were injected into the flasks. Using an external magnetic device, a magnetic force was applied for 6 h to the direction of the cartilage, and then the degenerated osteochondral fragment was cultured in chondrogenic differentiation medium for 3 weeks. In the control group, a magnetic force was not applied. Histological evaluated revealed that a new cell layer has formed on the surface of the degenerated cartilage. Positive staining of this cell layer with Toluidine blue, Safranin O, and with anti-type-II collagen immunostaining indicated that is contained a cartilage-like extracellular matrix. In the control group, such a cell layer was not observed. In conclusion, these findings demonstrate that the magnetic system can deliver MSCs onto degenerated human cartilage, which then form an abundant extracellular matrix in vitro. Another experimental study was conducted using minipigs to further demonstrate the effectiveness of this system for cartilage repair (Kamei et al. 2013). The safety of the cell application and the capability of the cell proliferation were also investigated and confirmed (Kamei et al. 2013). The first-in-men to apply this procedure to human with a cartilage defect will be started in 2015.
Another weak point is the overload of the focal area treated by marrow-stimulation as a result of early postoperative weight-bearing (Orth et al. 2012b). A novel approach to solve this problem is to reduce the load to the repaired area to protect immature tissue regenerated at the repaired area against destruction caused by overloading. A new distraction arthroplasty device was introduced (Meira, Nagoya, Japan), which allows the range of motion with knee joint distraction (Deie et al. 2007). After an experimental study using rabbits, this technique was applied to patients with OA. After drilling or microfracture under arthroscopy, the new external device was fixed with four 6-mm pins drilled into the distal femur and the proximal tibia. After the appropriate distractive tension was applied, the ROM and the post-distraction and pre-distraction tibiofemoral joint spaces at 30° of flexion were measured. Although this device is usually applied for 3 months, full weight bearing is allowed one month after surgery. Until now, this device has been demonstrated to function well to repair human articular cartilage defects.
Conclusions
The complexity of reconstructive surgical approaches for musculoskeletal disorders complicates the development of novel therapies. Large animal models continue to play a major role to translate new surgical techniques to patients. Although there is no single large animal model replicating the human knee joint perfectly, the sheep stifle joint shares strong similarities with the human knee joint. Large animal models for the treatment of ligamentous ACL lesions may help to overcome the therapeutic dilemma of how to treat such tears in the paediatric population. The newly developed preclinical large animal model of HTO can be applied to evaluate different types of osteotomies and to the effect of lower limb alignment on the reconstructive cartilage therapy. Animal models for cartilage repair need to precisely reflect the clinically very different aetiologies of articular cartilage defects, appearances and appropriate surgical options. This results in the currently large variety of different animal models for focal defects and OA. In the clinical situation, the combination of injection of magnetically labelled MSCs under magnetic field and external arthroplasty device may be an option to successfully treat large osteochondral defects or OA in the near future. As novel insights from studies using these translational models will advance the basic science, and close cooperation in this important field of clinical translation (Madry et al. 2014a) will improve current reconstructive surgical options, the clinical application of such innovative approaches will open novel avenues for regenerative therapies of musculoskeletal disorders.
References
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23(8):852–861, doi:S0749-8063(07)00585-3 [pii] 10.1016/j.arthro.2007.05.018
Agung M, Ochi M, Yanada S, Adachi N, Izuta Y, Yamasaki T, Toda K (2006) Mobilization of bone marrow-derived mesenchymal stem cells into the injured tissues after intraarticular injection and their contribution to tissue regeneration. Knee Surg Sports Traumatol Arthrosc 14(12):1307–1314, doi:10.1007/s00167-006-0124-8
Aigner T, Cook JL, Gerwin N, Glasson SS, Laverty S, Little CB, McIlwraith W, Kraus VB (2010) Histopathology atlas of animal model systems - overview of guiding principles. Osteoarthritis Cartilage 18(Suppl 3):S2–6, doi:S1063-4584(10)00250-5 [pii] 10.1016/j.joca.2010.07.013
Allen MJ, Houlton JE, Adams SB, Rushton N (1998) The surgical anatomy of the stifle joint in sheep. Vet Surg 27(6):596–605, doi:S0161349998000672 [pii]
Arnoczky SP, Marshall JL (1977) The cruciate ligaments of the canine stifle: an anatomical and functional analysis. Am J Vet Res 38(11):1807–1814
Athanasiou KA, Rosenwasser MP, Buckwalter JA, Malinin TI, Mow VC (1991) Interspecies comparisons of in situ intrinsic mechanical properties of distal femoral cartilage. J Orthop Res 9(3):330–340, doi:10.1002/jor.1100090304
Bayley N, Pinneau SR (1952) Tables for predicting adult height from skeletal age: revised for use with the Greulich-Pyle hand standards. J Pediatr 40(4):423–441
Beaufils P, Hardy P, Chambat P, Clavert P, Djian P, Frank A, Hulet C, Potel JF, Verdonk R (2006) Adult lateral meniscus. Rev Chir Orthop Reparatrice Appar Mot 92(5 Suppl):2S169–162S194, doi:MDOI-RCO-09-2006-92-S5-0035-1040-101019-200518962 [pii]
Bert JM (2015) Arthroscopy 31(3):501–505, doi:S0749-8063(14)01029-9 [pii] 10.1016/j.arthro.2014.12.018
Blaney Davidson EN, van de Loo FA, van den Berg WB, van der Kraan PM (2014) How to build an inducible cartilage-specific transgenic mouse. Arthritis Res Ther 16(3):210, doi:ar4573 [pii] 10.1186/ar4573
Bolano LE, Grana WA (1993) Isolated arthroscopic partial meniscectomy. Functional radiographic evaluation at five years. Am J Sports Med 21(3):432–437
Bosch U, Kasperczyk WJ (1993) The healing process after cruciate ligament repair in the sheep model. Orthopade 22(6):366–371
Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ (2008) Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br 90(12):1548–1557, doi:90-B/12/1548 [pii] 10.1302/0301-620X.90B12.21198
Brown WE, Potter HG, Marx RG, Wickiewicz TL, Warren RF (2004) Magnetic resonance imaging appearance of cartilage repair in the knee. Clin Orthop Relat Res (422):214–223. doi:00003086-200405000-00036 [pii]
Chen H, Sun J, Hoemann CD, Lascau-Coman V, Ouyang W, McKee MD, Shive MS, Buschmann MD (2009) Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res 27(11):1432–1438, doi: 10.1002/jor.20905
Chen H, Chevrier A, Hoemann CD, Sun J, Ouyang W, Buschmann MD (2011) Characterization of subchondral bone repair for marrow-stimulated chondral defects and its relationship to articular cartilage resurfacing. Am J Sports Med 39(8):1731–1740, doi:0363546511403282 [pii] 10.1177/0363546511403282
Chevrier A, Kouao AS, Picard G, Hurtig MB, Buschmann MD (2015) Interspecies comparison of subchondral bone properties important for cartilage repair. J Orthop Res 33(1):63–70, doi: 10.1002/jor.22740
Chotel F, Seil R (2013) Growth disturbances after transphyseal ACL reconstruction in skeletally immature patients: who is more at risk? Young child or adolescent? J Pediatr Orthop 33(5):585–586, doi:10.1097/BPO.0b013e318286c161 01241398-201307000-00022 [pii]
Chotel F, Seil R, Greiner P, Chaker MM, Berard J, Raux S (2013) The difficult diagnosis of cartilaginous tibial eminence fractures in young children. Knee Surg Sports Traumatol Arthrosc 22(7):1511–1516, doi:10.1007/s00167-013-2518-8
Cole BJ, Farr J, Winalski CS, Hosea T, Richmond J, Mandelbaum B, De Deyne PG (2011) Outcomes after a single-stage procedure for cell-based cartilage repair: a prospective clinical safety trial with 2-year follow-up. Am J Sports Med 39(6):1170–1179, doi:0363546511399382 [pii] 10.1177/0363546511399382
Cook JL, Kuroki K, Visco D, Pelletier JP, Schulz L, Lafeber FP (2010) The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the dog. Osteoarthritis Cartilage 18(Suppl 3):S66–79, doi:S1063-4584(10)00237-2 [pii] 10.1016/j.joca.2010.04.017
Cucchiarini M, Madry H (2014) Overexpression of human IGF-I via direct rAAV-mediated gene transfer improves the early repair of articular cartilage defects in vivo. Gene Ther 21(9):811–819, doi:gt201458 [pii] 10.1038/gt.2014.58
Cucchiarini M, Madry H, Guilak F, Saris DB, Stoddart MJ, Koon Wong M, Roughley P (2014) A vision on the future of articular cartilage repair. Eur Cell Mater 27:12–16, doi:vol027sa03 [pii]
Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG (1997) Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy 13(4):456–460
Deie M, Ochi M, Adachi N, Kajiwara R, Kanaya A (2007) A new articulated distraction arthroplasty device for treatment of the osteoarthritic knee joint: a preliminary report. Arthroscopy 23(8):833–838, doi:S0749-8063(07)00237-X [pii] 10.1016/j.arthro.2007.02.014
Dhollander AA, De Neve F, Almqvist KF, Verdonk R, Lambrecht S, Elewaut D, Verbruggen G, Verdonk PC (2011) Autologous matrix-induced chondrogenesis combined with platelet-rich plasma gel: technical description and a five pilot patients report. Knee Surg Sports Traumatol Arthrosc 19(4):536–542, doi:10.1007/s00167-010-1337-4
Drobnic M, Radosavljevic D, Cor A, Brittberg M, Strazar K (2010) Debridement of cartilage lesions before autologous chondrocyte implantation by open or transarthroscopic techniques: a comparative study using post-mortem materials. J Bone Joint Surg Br 92(4):602–608, doi:92-B/4/602 [pii] 10.1302/0301-620X.92B3.22558
Dye SF (1987) An evolutionary perspective of the knee. J Bone Joint Surg Am 69(7):976–983
Edwards TB, Greene CC, Baratta RV, Zieske A, Willis RB (2001) The effect of placing a tensioned graft across open growth plates. A gross and histologic analysis. J Bone Joint Surg Am 83-A(5):725–734
Eldracher M, Orth P, Cucchiarini M, Pape D, Madry H (2014) Small subchondral drill holes improve marrow stimulation of articular cartilage defects. Am J Sports Med 42(11):2741–2750, doi:0363546514547029 [pii] 10.1177/0363546514547029
Espregueira-Mendes J, Karahan M (2014) Orthopaedic sports surgery: art or science? Knee Surg Sports Traumatol Arthrosc 22(5):959–960, doi:10.1007/s00167-014-2921-9
Frisbie DD, Trotter GW, Powers BE, Rodkey WG, Steadman JR, Howard RD, Park RD, McIlwraith CW (1999) Arthroscopic subchondral bone plate microfracture technique augments healing of large chondral defects in the radial carpal bone and medial femoral condyle of horses. Vet Surg 28(4):242–255
Frisbie DD, Oxford JT, Southwood L, Trotter GW, Rodkey WG, Steadman JR, Goodnight JL, McIlwraith CW (2003) Early events in cartilage repair after subchondral bone microfracture. Clin Orthop Relat Res 407:215–227
Frisbie DD, Cross MW, McIlwraith CW (2006a) A comparative study of articular cartilage thickness in the stifle of animal species used in human pre-clinical studies compared to articular cartilage thickness in the human knee. Vet Comp Orthop Traumatol 19(3):142–146, doi:06030142 [pii]
Frisbie DD, Morisset S, Ho CP, Rodkey WG, Steadman JR, McIlwraith CW (2006b) Effects of calcified cartilage on healing of chondral defects treated with microfracture in horses. Am J Sports Med 34(11):1824–1831
Frisch J, Venkatesan JK, Rey-Rico A, Madry H, Cucchiarini M (2014) Current progress in stem cell-based gene therapy for articular cartilage repair. Curr Stem Cell Res Ther. doi:CSCRT-EPUB-62443 [pii]
Gerwin N, Bendele AM, Glasson S, Carlson CS (2010) The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the rat. Osteoarthritis Cartilage 18(Suppl 3):S24–34, doi:S1063-4584(10)00247-5 [pii] 10.1016/j.joca.2010.05.030
Getgood A, Henson F, Skelton C, Brooks R, Guehring H, Fortier L, Rushton N (2014) Osteochondral tissue engineering using a biphasic collagen/GAG scaffold containing rhFGF18 or BMP-7 in an ovine model. J Exp Orthop 1 (13). doi:doi:10.1186/s40634-014-0013-x
Glasson SS, Chambers MG, Van Den Berg WB, Little CB (2010) The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the mouse. Osteoarthritis Cartilage 18(Suppl 3):S17–23, doi:S1063-4584(10)00238-4 [pii] 10.1016/j.joca.2010.05.025
Goebel L, Orth P, Muller A, Zurakowski D, Bucker A, Cucchiarini M, Pape D, Madry H (2012) Experimental scoring systems for macroscopic articular cartilage repair correlate with the MOCART score assessed by a high-field MRI at 9.4 T - comparative evaluation of five macroscopic scoring systems in a large animal cartilage defect model. Osteoarthritis Cartilage 20(9):1046–1055, doi:S1063-4584(12)00839-4 [pii] 10.1016/j.joca.2012.05.010
Goebel L, Zurakowski D, Muller A, Pape D, Cucchiarini M, Madry H (2014) 2D and 3D MOCART scoring systems assessed by 9.4 T high-field MRI correlate with elementary and complex histological scoring systems in a translational model of osteochondral repair. Osteoarthritis Cartilage 22(10):1386–1395, doi:S1063-4584(14)01109-1 [pii] 10.1016/j.joca.2014.05.027
Gomoll AH, Madry H, Knutsen G, van Dijk N, Seil R, Brittberg M, Kon E (2010) The subchondral bone in articular cartilage repair: current problems in the surgical management. Knee Surg Sports Traumatol Arthrosc 18(4):434–447, doi:10.1007/s00167-010-1072-x
Guzzanti V, Falciglia F, Gigante A, Fabbriciani C (1994) The effect of intra-articular ACL reconstruction on the growth plates of rabbits. J Bone Joint Surg Br 76(6):960–963
Heijink A, Gomoll AH, Madry H, Drobnic M, Filardo G, Espregueira-Mendes J, Van Dijk CN (2012) Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 20(3):423–435, doi: 10.1007/s00167-011-1818-0
Henderson IJ, La Valette DP (2005) Subchondral bone overgrowth in the presence of full-thickness cartilage defects in the knee. Knee 12(6):435–440, doi:S0968-0160(05)00065-7 [pii] 10.1016/j.knee.2005.04.003
Hjelle K, Solheim E, Strand T, Muri R, Brittberg M (2002) Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy 18(7):730–734, doi:S0749806302000257 [pii]
Hoemann CD, Lafantaisie-Favreau CH, Lascau-Coman V, Chen G, Guzman-Morales J (2012) The cartilage-bone interface. J Knee Surg 25(2):85–97
Hoser C, Fink C, Brown C, Reichkendler M, Hackl W, Bartlett J (2001) Long-term results of arthroscopic partial lateral meniscectomy in knees without associated damage. J Bone Joint Surg Br 83(4):513–516
Hunziker EB (1999a) Articular cartilage repair: are the intrinsic biological constraints undermining this process insuperable? Osteoarthritis Cartilage 7(1):15–28
Hunziker EB (2000) Articular cartilage repair: problems and perspectives. Biorheology 37(1–2):163–164
Hunziker EB (2002) Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthritis Cartilage 10(6):432–463, doi:10.1053/joca.2002.0801 S1063458402908010 [pii]
Hunziker EB (2009) The elusive path to cartilage regeneration. Adv Mater 21(32–33):3419–3424, doi: 10.1002/adma.200801957
Hunziker EB (1999) Biologic repair of articular cartilage. Defect models in experimental animals and matrix requirements. Clin Orthop (367 Suppl):S135-146
Hunziker EB, Rosenberg LC (1996) Repair of partial-thickness defects in articular cartilage: cell recruitment from the synovial membrane. J Bone Joint Surg Am 78(5):721–733
Janarv PM, Wikstrom B, Hirsch G (1998) The influence of transphyseal drilling and tendon grafting on bone growth: an experimental study in the rabbit. J Pediatr Orthop 18(2):149–154
Johnson LL (2001) Arthroscopic abrasion arthroplasty: a review. Clin Orthop (391 Suppl):S306-317
Johnstone B, Yoo JU (1999) Autologous mesenchymal progenitor cells in articular cartilage repair. Clin Orthop Relat Res (367 Suppl):S156-162
Johnstone B, Hering TM, Caplan AI, Goldberg VM, Yoo JU (1998) In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Exp Cell Res 238(1):265–272, doi:S0014-4827(97)93858-1 [pii] 10.1006/excr.1997.3858
Johnstone B, Alini M, Cucchiarini M, Dodge GR, Eglin D, Guilak F, Madry H, Mata A, Mauck RL, Semino CE, Stoddart MJ (2013) Tissue engineering for articular cartilage repair--the state of the art. Eur Cell Mater 25:248–267, doi:vol025a18 [pii]
Kamei G, Kobayashi T, Ohkawa S, Kongcharoensombat W, Adachi N, Takazawa K, Shibuya H, Deie M, Hattori K, Goldberg JL, Ochi M (2013) Articular cartilage repair with magnetic mesenchymal stem cells. Am J Sports Med 41(6):1255–1264, doi:0363546513483270 [pii] 10.1177/0363546513483270
Kiss A, Cucchiarini M, Menger MD, Kohn D, Hannig M, Madry H (2014) Enamel matrix derivative inhibits proteoglycan production and articular cartilage repair, delays the restoration of the subchondral bone and induces changes of the synovial membrane in a lapine osteochondral defect model in vivo. J Tissue Eng Regen Med 8(1):41–49, doi: 10.1002/term.1495
Kobayashi T, Ochi M, Yanada S, Ishikawa M, Adachi N, Deie M, Arihiro K (2008) A novel cell delivery system using magnetically labeled mesenchymal stem cells and an external magnetic device for clinical cartilage repair. Arthroscopy 24(1):69–76, doi:S0749-8063(07)00755-4 [pii] 10.1016/j.arthro.2007.08.017
Kobayashi T, Ochi M, Yanada S, Ishikawa M, Adachi N, Deie M, Arihiro K (2009) Augmentation of degenerated human cartilage in vitro using magnetically labeled mesenchymal stem cells and an external magnetic device. Arthroscopy 25(12):1435–1441, doi:S0749-8063(09)00521-0 [pii] 10.1016/j.arthro.2009.06.009
Kocher MS, Saxon HS, Hovis WD, Hawkins RJ (2002) Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop 22(4):452–457
Koman JD, Sanders JO (1999) Valgus deformity after reconstruction of the anterior cruciate ligament in a skeletally immature patient. A case report. J Bone Joint Surg Am 81(5):711–715
Kraus VB, Huebner JL, DeGroot J, Bendele A (2010) The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the guinea pig. Osteoarthritis Cartilage 18(Suppl 3):S35–52, doi:S1063-4584(10)00234-7 [pii] 10.1016/j.joca.2010.04.015
Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P, Ghanem N, Uhl M, Sudkamp N (2006a) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy 22(11):1180–1186
Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, Sudkamp N (2006b) Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage 14(11):1119–1125
Laverty S, Girard CA, Williams JM, Hunziker EB, Pritzker KP (2010) The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the rabbit. Osteoarthritis Cartilage 18(Suppl 3):S53–65, doi:S1063-4584(10)00244-X [pii] 10.1016/j.joca.2010.05.029
Lim HC, Bae JH, Song HR, Teoh SH, Kim HK, Kum DH (2011) High tibial osteotomy using polycaprolactone-tricalcium phosphate polymer wedge in a micro pig model. J Bone Joint Surg Br 93(1):120–125, doi:93-B/1/120 [pii] 10.1302/0301-620X.93B1.24767
Little CB, Zaki S (2012) What constitutes an “animal model of osteoarthritis”--the need for consensus? Osteoarthritis Cartilage 20(4):261–267, doi:S1063-4584(12)00054-4 [pii] 10.1016/j.joca.2012.01.017
Little CB, Smith MM, Cake MA, Read RA, Murphy MJ, Barry FP (2010) The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in sheep and goats. Osteoarthritis Cartilage 18(Suppl 3):S80–92, doi:S1063-4584(10)00235-9 [pii] 10.1016/j.joca.2010.04.016
Lobenhoffer P, Agneskirchner JD (2003a) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11(3):132–138, doi:10.1007/s00167-002-0334-7
Lobenhoffer P, Agneskirchner JD (2014) Osteotomy around the knee vs. unicondylar knee replacement. Orthopade 43(10):923-9. doi: 10.1007/s00132-014-3011-x
Macnicol MF, Thomas NP (2000) The knee after meniscectomy. J Bone Joint Surg Br 82(2):157–159
Madry H (2010) The subchondral bone: a new frontier in articular cartilage repair. Knee Surg Sports Traumatol Arthrosc 18(4):417–418, doi:10.1007/s00167-010-1071-y
Madry H, van Dijk CN, Mueller-Gerbl M (2010) The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc 18(4):419–433, doi:10.1007/s00167-010-1054-z
Madry H, Grun UW, Knutsen G (2011) Cartilage repair and joint preservation: medical and surgical treatment options. Dtsch Arztebl Int 108(40):669–677, doi: 10.3238/arztebl.2011.0669
Madry H, Kaul G, Zurakowski D, Vunjak-Novakovic G, Cucchiarini M (2013a) Cartilage constructs engineered from chondrocytes overexpressing IGF-I improve the repair of osteochondral defects in a rabbit model. Eur Cell Mater 25:229–247, doi:vol025a17 [pii]
Madry H, Ziegler R, Orth P, Goebel L, Ong MF, Kohn D, Cucchiarini M, Pape D (2013b) Effect of open wedge high tibial osteotomy on the lateral compartment in sheep. Part I: Analysis of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 21(1):39–48, doi: 10.1007/s00167-012-2176-2
Madry H, Alini M, Stoddart MJ, Evans C, Miclau T, Steiner S (2014a) Barriers and strategies for the clinical translation of advanced orthopaedic tissue engineering protocols. Eur Cell Mater 27:17–21, doi:vol027sa04 [pii]
Madry H, Ziegler R, Pape D, Cucchiarini M (2014b) Structural changes in the lateral tibiofemoral compartment after high tibial osteotomy. Orthopade 43(11):958–965, doi: 10.1007/s00132-014-3024-5
McIlwraith CW, Frisbie DD, Kawcak CE, Fuller CJ, Hurtig M, Cruz A (2010) The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the horse. Osteoarthritis Cartilage 18(Suppl 3):S93–105, doi:S1063-4584(10)00251-7 [pii] 10.1016/j.joca.2010.05.031
Meller R, Kendoff D, Hankemeier S, Jagodzinski M, Grotz M, Knobloch K, Krettek C (2008a) Hindlimb growth after a transphyseal reconstruction of the anterior cruciate ligament: a study in skeletally immature sheep with wide-open physes. Am J Sports Med 36(12):2437–2443, doi:0363546508322884 [pii] 10.1177/0363546508322884
Meller R, Willbold E, Hesse E, Dreymann B, Fehr M, Haasper C, Hurschler C, Krettek C, Witte F (2008b) Histologic and biomechanical analysis of anterior cruciate ligament graft to bone healing in skeletally immature sheep. Arthroscopy 24(11):1221–1231, doi:S0749-8063(08)00515-X [pii] 10.1016/j.arthro.2008.06.021
Meller R, Brandes G, Drogemuller C, Fritz F, Schiborra F, Fehr M, Hankemeier S, Krettek C, Hurschler C (2009a) Graft remodeling during growth following anterior cruciate ligament reconstruction in skeletally immature sheep. Arch Orthop Trauma Surg 129(8):1037–1046, doi: 10.1007/s00402-008-0784-6
Meller R, Haasper C, Westhoff J, Brand J, Knobloch K, Hankemeier S, Hesse E, Krettek C, Jagodzinski M (2009b) An animal model to study ACL reconstruction during growth. Technol Health Care 17(5–6):403–410, doi:FJ024610011H62Q0 [pii] 10.3233/THC-2009-0561
Min BH, Choi WH, Lee YS, Park SR, Choi BH, Kim YJ, Jin LH, Yoon JH (2013) Effect of different bone marrow stimulation techniques (BSTs) on MSCs mobilization. J Orthop Res 31(11):1814–1819, doi:10.1002/jor.22380
Mithoefer K, Williams RJ 3rd, Warren RF, Potter HG, Spock CR, Jones EC, Wickiewicz TL, Marx RG (2005) The microfracture technique for the treatment of articular cartilage lesions in the knee. A prospective cohort study. J Bone Joint Surg Am 87(9):1911–1920
Muller-Gerbl M, Putz R, Kenn R (1992) Demonstration of subchondral bone density patterns by three-dimensional CT osteoabsorptiometry as a noninvasive method for in vivo assessment of individual long-term stresses in joints. J Bone Miner Res 7(Suppl 2):S411–418, doi:10.1002/jbmr.5650071409
Niemeyer P, Uhl M, Salzmann GM, Morscheid YP, Sudkamp NP, Madry H (2015) Evaluation and analysis of graft hypertrophy by means of arthroscopy, biochemical MRI and osteochondral biopsies in a patient following autologous chondrocyte implantation for treatment of a full-thickness-cartilage defect of the knee. Arch Orthop Trauma Surg. doi:10.1007/s00402-015-2194-x
Ogden JA (1981) Injury to the growth mechanisms of the immature skeleton. Skeletal Radiol 6(4):237–253
Ono T, Wada Y, Takahashi K, Tsuchida T, Minamide M, Moriya H (1998) Tibial deformities and failures of anterior cruciate ligament reconstruction in immature rabbits. J Orthop Sci 3(3):150–155
Orth P, Cucchiarini M, Kaul G, Ong MF, Graber S, Kohn DM, Madry H (2012a) Temporal and spatial migration pattern of the subchondral bone plate in a rabbit osteochondral defect model. Osteoarthritis Cartilage 20(10):1161–1169, doi:S1063-4584(12)00863-1 [pii] 10.1016/j.joca.2012.06.008
Orth P, Goebel L, Wolfram U, Ong MF, Graber S, Kohn D, Cucchiarini M, Ignatius A, Pape D, Madry H (2012b) Effect of subchondral drilling on the microarchitecture of subchondral bone: analysis in a large animal model at 6 months. Am J Sports Med 40(4):828–836, doi:0363546511430376 [pii] 10.1177/0363546511430376
Orth P, Zurakowski D, Wincheringer D, Madry H (2012c) Reliability, reproducibility, and validation of five major histological scoring systems for experimental articular cartilage repair in the rabbit model. Tissue Eng Part C Methods 18(5):329–339, doi: 10.1089/ten.TEC.2011.0462
Orth P, Cucchiarini M, Kohn D, Madry H (2013a) Alterations of the subchondral bone in osteochondral repair--translational data and clinical evidence. Eur Cell Mater 25:299–316, doi:vol025a21 [pii]
Orth P, Cucchiarini M, Zurakowski D, Menger MD, Kohn DM, Madry H (2013b) Parathyroid hormone [1–34] improves articular cartilage surface architecture and integration and subchondral bone reconstitution in osteochondral defects in vivo. Osteoarthritis Cartilage 21(4):614–624, doi:S1063-4584(13)00023-X [pii] 10.1016/j.joca.2013.01.008
Orth P, Meyer HL, Goebel L, Eldracher M, Ong MF, Cucchiarini M, Madry H (2013c) Improved repair of chondral and osteochondral defects in the ovine trochlea compared with the medial condyle. J Orthop Res 31(11):1772–1779, doi:10.1002/jor.22418
Orth P, Zurakowski D, Alini M, Cucchiarini M, Madry H (2013d) Reduction of sample size requirements by bilateral versus unilateral research designs in animal models for cartilage tissue engineering. Tissue Eng Part C Methods 19(11):885–891, doi: 10.1089/ten.TEC.2012.0699
Otsuki S, Nakajima M, Lotz M, Kinoshita M (2008) Hyaluronic acid and chondroitin sulfate content of osteoarthritic human knee cartilage: site-specific correlation with weight-bearing force based on femorotibial angle measurement. J Orthop Res 26(9):1194–1198, doi: 10.1002/jor.20571
Pape D, Madry H (2013) The preclinical sheep model of high tibial osteotomy relating basic science to the clinics: standards, techniques and pitfalls. Knee Surg Sports Traumatol Arthrosc 21(1):228–236, doi: 10.1007/s00167-012-2135-y
Pape D, Filardo G, Kon E, van Dijk CN, Madry H (2010) Disease-specific clinical problems associated with the subchondral bone. Knee Surg Sports Traumatol Arthrosc 18(4):448–462, doi:10.1007/s00167-010-1052-1
Pape D, Kohn D, van Giffen N, Hoffmann A, Seil R, Lorbach O (2011) Differences in fixation stability between spacer plate and plate fixator following high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):82–89, doi:10.1007/s00167-011-1693-8
Pastoureau PC, Hunziker EB, Pelletier JP (2010) Cartilage, bone and synovial histomorphometry in animal models of osteoarthritis. Osteoarthritis Cartilage 18(Suppl 3):S106–112, doi:S1063-4584(10)00232-3 [pii] 10.1016/j.joca.2010.05.024
Pena E, Calvo B, Martinez MA, Palanca D, Doblare M (2006) Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study. J Orthop Res 24(5):1001–1010, doi: 10.1002/jor.20037
Pineda S, Pollack A, Stevenson S, Goldberg V, Caplan A (1992) A semiquantitative scale for histologic grading of articular cartilage repair. Acta Anat (Basel) 143(4):335–340
Poole R, Blake S, Buschmann M, Goldring S, Laverty S, Lockwood S, Matyas J, McDougall J, Pritzker K, Rudolphi K, van den Berg W, Yaksh T (2010) Recommendations for the use of preclinical models in the study and treatment of osteoarthritis. Osteoarthritis Cartilage 18(Suppl 3):S10–16, doi:S1063-4584(10)00241-4 [pii] 10.1016/j.joca.2010.05.027
Pridie KH (1959) A method of resurfacing osteoarthritic knee joints. Proceedings of the British Orthopaedic Association J Bone Joint Surg (Br) 41:618–619
Pritzker KP, Gay S, Jimenez SA, Ostergaard K, Pelletier JP, Revell PA, Salter D, van den Berg WB (2006) Osteoarthritis cartilage histopathology: grading and staging. Osteoarthritis Cartilage 14(1):13–29, doi:S1063-4584(05)00197-4 [pii] 10.1016/j.joca.2005.07.014
Prodromos CC, Amendola A, Jakob RP (2015) High tibial osteotomy: indications, techniques, and postoperative management. Instr Course Lect 64:555–565
Qiu YS, Shahgaldi BF, Revell WJ, Heatley FW (2003) Observations of subchondral plate advancement during osteochondral repair: a histomorphometric and mechanical study in the rabbit femoral condyle. Osteoarthritis Cartilage 11(11):810–820
Robert HE, Casin C (2010) Valgus and flexion deformity after reconstruction of the anterior cruciate ligament in a skeletally immature patient. Knee Surg Sports Traumatol Arthrosc 18(10):1369–1373, doi: 10.1007/s00167-009-0988-5
Rudert M, Moller HD, Schulze M, Wirth CJ (2000) Tissue engineering for therapy of osteochondral cartilage lesions. Zentralbl Chir 125(6):509–515
Salomon FV (2001) Personal Communication. Department of Veterinary Medicine, University of Leipzig, Leipzig, Germany
Sansone V, de Girolamo L, Pascale W, Melato M, Pascale V (2015) Long-term results of abrasion arthroplasty for full-thickness cartilage lesions of the medial femoral condyle. Arthroscopy 31(3):396–403, doi:S0749-8063(14)00841-X [pii] 10.1016/j.arthro.2014.10.007
Saris DB, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, Luyten FP (2009) Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med 37(Suppl 1):10S–19S, doi:0363546509350694 [pii] 10.1177/0363546509350694
Scheller G, Sobau C, Bulow JU (2001) Arthroscopic partial lateral meniscectomy in an otherwise normal knee: Clinical, functional, and radiographic results of a long-term follow-up study. Arthroscopy 17(9):946–952, doi:S0749-8063(01)57748-8 [pii] 10.1053/jars.2001.28952
Seil R (2003) Die Ersatzplastik des vorderen Kreuzbandes bei offenen Wachstumsfugen - eine experimentelle Untersuchung. Saarland University, Homburg, Habilitation thesis
Seil R, Pape D, Kohn D (2008) The risk of growth changes during transphyseal drilling in sheep with open physes. Arthroscopy 24(7):824–833, doi:S0749-8063(08)00149-7 [pii] 10.1016/j.arthro.2008.02.007
Sellers RS, Peluso D, Morris EA (1997) The effect of recombinant human bone morphogenetic protein-2 (rhBMP-2) on the healing of full-thickness defects of articular cartilage. J Bone Joint Surg Am 79(10):1452–1463
Shapiro F, Koide S, Glimcher MJ (1993) Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg Am 75(4):532–553
Simon WH (1971) Scale effects in animal jointsII. Thickness and elasticity in the deformability of articular cartilage. Arthritis Rheum 14(4):493–502
Smillie IS (1957) Treatment of osteochondritis dissecans. J Bone Joint Surg Br 39(2):248–260
Song EK, Seon JK, Park SJ, Jeong MS (2010) The complications of high tibial osteotomy: closing- versus opening-wedge methods. J Bone Joint Surg Br 92(9):1245–1252, doi:92-B/9/1245 [pii] 10.1302/0301-620X.92B9.23660
Stadelmaier DM, Arnoczky SP, Dodds J, Ross H (1995) The effect of drilling and soft tissue grafting across open growth plates. A histologic study. Am J Sports Med 23(4):431–435
Steadman JR, Rodkey WG, Rodrigo JJ (2001) Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop (391 Suppl):S362-369
Van Thiel GS, Frank RM, Gupta A, Ghodadra N, Shewman EF, Wang VM, Bach BR, Verma NN, Cole BJ, Provencher MT (2011) Biomechanical evaluation of a high tibial osteotomy with a meniscal transplant. J Knee Surg 24(1):45–53
Vasiliadis HS, Danielson B, Ljungberg M, McKeon B, Lindahl A, Peterson L (2010) Autologous chondrocyte implantation in cartilage lesions of the knee: long-term evaluation with magnetic resonance imaging and delayed gadolinium-enhanced magnetic resonance imaging technique. Am J Sports Med 38(5):943–949, doi:0363546509358266 [pii] 10.1177/0363546509358266
Wang YX, Hussain SM, Krestin GP (2001) Superparamagnetic iron oxide contrast agents: physicochemical characteristics and applications in MR imaging. Eur Radiol 11(11):2319–2331, doi:10.1007/s003300100908
W-Dahl A, Robertsson O, Lohmander LS (2012) High tibial osteotomy in Sweden, 1998–2007. Acta Orthop. doi:10.3109/17453674.2012.688725
Wei L, Hjerpe A, Brismar BH, Svensson O (2001) Effect of load on articular cartilage matrix and the development of guinea-pig osteoarthritis. Osteoarthritis Cartilage 9(5):447–453, doi:10.1053/joca.2000.0411 S1063-4584(00)90411-4 [pii]
Zellner J, Kujat R, Koch M, Angele P (2014) Role of mesenchymal stem cells in meniscal repair. J Exp Orthop 1 (12). doi:10.1186/s40634-014-0012-y
Ziegler R, Goebel L, Cucchiarini M, Pape D, Madry H (2013) Effect of open wedge high tibial osteotomy on the lateral tibiofemoral compartment in sheep. Part II: standard and overcorrection do not cause articular cartilage degeneration. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2410-6
Ziegler R, Goebel L, Seidel R, Cucchiarini M, Pape D, Madry H (2014) Effect of open wedge high tibial osteotomy on the lateral tibiofemoral compartment in sheep. Part III: analysis of the microstructure of the subchondral bone and correlations with the articular cartilage and meniscus. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3134-y
Acknowledgments
The authors thank the presenters, discussion moderators, and all the participants to the Symposium for their valuable input and contributions. We wish to confirm that there are no known conflicts of interests associated with this publication and there has been no financial support for this work that could have influenced its outcome.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HM, MO, MC participated equally in drafting the manuscript in particular the cartilage defect section. HM, DP participated equally in drafting the manuscript in particular the osteotomy section. RS participated equally in drafting the manuscript in particular the section about the paediatric ACL reconstruction. All of the authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Madry, H., Ochi, M., Cucchiarini, M. et al. Large animal models in experimental knee sports surgery: focus on clinical translation. J EXP ORTOP 2, 9 (2015). https://doi.org/10.1186/s40634-015-0025-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-015-0025-1