Abstract
Background
The efficacy of therapeutic drug monitoring (TDM)-based antimicrobial dosing optimization strategies on pharmacokinetics/pharmacodynamics and specific drug properties for critically ill patients is unclear. Here, we conducted a systematic review and meta-analysis of randomized controlled trials to evaluate the effectiveness of TDM-based regimen in these patients.
Methods
Articles from three databases were systematically retrieved to identify relevant randomized control studies. Version two of the Cochrane tool for assessing risk of bias in randomized trials was used to assess the risk of bias in studies included in the analysis, and quality assessment of evidence was graded using the Grading of Recommendations Assessment, Development, and Evaluation approach. Primary outcome was the 28-day mortality and secondary outcome were in-hospital mortality, clinical cure, length of stay in the intensive care unit (ICU) and target attainment at day 1 and 3.
Results
In total, 5 studies involving 1011 patients were included for meta-analysis of the primary outcome, of which no significant difference was observed between TDM-based regimen and control groups (risk ratio [RR] 0.94, 95% confidence interval [CI]: 0.77–1.14; I2 = 0%). In-hospital mortality (RR 0.96, 95% CI: 0.76–1.20), clinical cure (RR 1.23, 95% CI: 0.91–1.67), length of stay in the ICU (mean difference 0, 95% CI: − 2.18–2.19), and target attainment at day 1 (RR 1.14, 95% CI: 0.88–1.48) and day 3 (RR 1.35, 95% CI: 0.90–2.03) were not significantly different between the two groups, and all evidence for the secondary outcomes had a low or very low level of certainty because the included studies had serious risk of bias, variation of definition for outcomes, and small sample sizes.
Conclusion
TDM-based regimens had no significant efficacy for clinical or pharmacological outcomes. Further studies with other achievable targets and well-defined outcomes are required.
Trial registration: Clinical trial registration; PROSPERO (https://www.crd.york.ac.uk/prospero/), registry number: CRD 42022371959. Registered 24 November 2022.
Similar content being viewed by others
Background
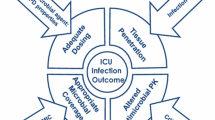
Antibiotic therapy is a cornerstone in the treatment of sepsis and severe infections, and appropriate antibiotic dosing design based on pharmacokinetics/pharmacodynamics (PK/PD) is necessary [1,2,3,4]. The Surviving Sepsis Campaign suggested that dosing strategies for antimicrobials should be optimized based on PK/PD and specific drug properties as a best practice statement [5]. However, sepsis can result in an increase in the distribution volume of antibiotics and altered clearance, leading to unpredictable blood levels if treatments are based on normal antibiotic doses [6,7,8,9,10,11]. In such cases, the usual PK/PD-based dosing regimen may result in inadequate or excessive antibiotic concentrations, leading to poor clinical outcomes or organ damage such as kidney injury [12,13,14].
Therapeutic drug monitoring (TDM), which refers the management and adjustment of the patient's drug dosing based on the measured drug concentration in the blood, has been suggested as a method of drug exposure optimization [15, 16]. Previous studies have advocated for the importance of TDM to maximize antimicrobial effectiveness and decrease adverse event. However, only few studies have clearly verified the efficacy of TDM-based antibiotic regimen in critically ill patients, regardless of the antimicrobial agent type [17].
Recent systematic review and meta-analysis evaluating TDM for beta-lactam antibiotics included five randomized control trials (RCTs), but two large RCTs on TDM have since been published, increasing the need for reevaluation [18]. Hence, we conducted a systematic review and meta-analysis of RCTs to evaluate the efficacy of TDM-based regimens in critically ill patients, focusing on both clinical and pharmacological outcomes, which includes target attainment. Studies were not restricted by type of antimicrobial agent as the primary aim was to validate the implementation of TDM-based regimens.
Materials and methods
Study design and definition
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [19], and the protocol for this systematic review was registered in the PROSPERO database on 24 November 2022 (CRD 42022371959). In the protocol, critically ill patients were defined as those meeting any of the following: (1) patients admitted to an intensive care unit (ICU) and requiring artificial support including invasive mechanical ventilation; (2) patients who were considered critically ill based on the definition in each study and had suspected or proven infection, or (3) patients diagnosed with sepsis. Sepsis was defined as Sepsis-3 or severe sepsis with Sepsis-1 or 2, which indicates organ dysfunction due to infection [20]. TDM was defined as the measurement of antimicrobial agent concentration in blood, serum, or plasma at a specific time point, and the dosing adjustment was based on the concentration.
Research question and inclusion criteria
Our research question was whether TDM should be used to adjust antimicrobial doses in patients with sepsis or treated in the ICU. Accordingly, RCTs comparing TDM to standard procedures in patients aged ≥ 18 years with either sepsis or who were critical ill were included. TDM studies that did not have a control were excluded. Case series, case reports, editorials, letters to editor, and conference abstracts were also excluded from this review.
Literature search
Two authors (N.T. and Y.O.) independently and systematically searched the MEDLINE (via PubMed), Cochrane CENTRAL databases, and Igaku-Chuo-Zasshi for peer-reviewed articles published as well as the ClinicalTrials.gov and World Health Organization International Clinical Trial Registry Platform for relevant completed trials between database inception and November 2022 (search date: 17 November 2022).
Search formulas were created based on “Sepsis”, “Systemic Inflammatory Response Syndrome”, “Multiple Organ Failure”, “Critically ill”. “Therapeutic Drug Monitoring”, and “Randomized controlled trial” with Medical Subject Heading terms and text words along with a query starting with “NOT” to exclude ineligible studies. The terms were then arranged and entered in a form suitable for each database (Additional file 1: Table S1).
Screening and data extraction
After extraction of the study list and exclusion of duplicate studies, two authors (N.T. and Y.O.) independently screened the titles and abstracts of all articles to identify eligible studies by using a study by Ryyan [21] as the first screening. If there was conflict between the authors and the disagreement persisted, a third author (Y.K.) was consulted to resolve the conflict through discussion. The second screening was reviewing full texts of the articles included in the final selection, which was independently performed by two authors (N.T. and Y.O.). Subsequently, two authors (N.T. and Y.O.) independently extracted all relevant information from the included studies, including study settings and period, design, year, study population, sample size, patient demographic, type of antibiotics regimen, intervention algorithm and strategy, minimum inhibitory concentration (MIC), target attainment, primary outcomes, and included mortality type.
Risk of bias assessment using the grading of recommendations assessment, development, and evaluation (GRADE) approach
Two authors (N.T. and Y.O.) independently assessed the risk of bias for each included study using the Cochrane tool for assessing risk of bias in randomized trials, version two (RoB 2) [22]. This tool assesses bias arising from the randomization process due to deviations from intended interventions and missing outcome data in outcome measurement and selection of reported results by classifying each domain with low, intermediate, or high risk of bias. Any conflicts were resolved through a discussion or independent evaluation by a third author (Y.K.).
Quality assessment of evidence was graded using the GRADE system that provides a systematic approach for each outcome across studies [23]. The GRADE system has four levels for the evidence: very low, low, moderate, and high. GRADE scores were reduced by risk of bias, imprecision, inconsistency, indirectness, and publication bias. Publication bias was visually assessed by evaluating the funnel plots [24].
Outcomes
The primary outcome of interest was 28-day mortality. Secondary outcomes were target attainment defined in each study at day 1 and 3, clinical cure (resolution of infection signs and symptoms, no clinical failure, or as based on definition in each study), hospital mortality, and length of stay in the ICU. If TDM was simultaneously performed for multiple antibiotics, outcomes including target attainment were analyzed separately for each antibiotic. We also performed the analysis by the subgroup for the class of antibiotics when there was more than one study.
Statistical analysis
Extracted data were collected and statistically analyzed using RevMan ver 5.4.1 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). Risk ratios (RRs) and corresponding 95% confidence intervals (CIs) were determined using a random-effects model with weights calculated using the Mantel–Haenszel method [25]. For continuous values, mean difference and 95% CIs were calculated using inverse variance-weighted method. Heterogeneity of the included studies was assessed using the estimated Cochrane Chi-square test, Tau2, and I2 statistic, in which I2 > 70% indicated severe heterogeneity. To calculate point estimates, when the mean and median were different, the mean was considered the same as the median, and the standard deviation (SD) was integrated by dividing the interquartile (IQR) by 1.35 (https://handbook-5-1.cochrane.org/chapter_7/7_7_3_5_mediansand_interquartile_ranges.htm).
A two-tailed P < 0.05 for hypothesis and < 0.1 for heterogeneity testing was considered statistically significant.
Results
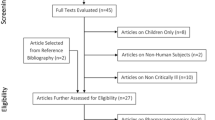
We identified 863 records from searching the three electronic databases. Of these, 769 publications were screened, and 8 studies were retrieved for full text review. Finally, 5 RCTs were included in our meta-analysis (participants, n = 1011; TDM group, n = 510; standard dosing group, n = 501) [26,27,28,29,30] (Fig. 1, Table 1). Four of the studies were conducted in Europe, three were published in 2022; four included beta-lactam antibiotics, two included quinolones, one included aminoglycoside, and one included vancomycin. There were no conflicts of interest reported in any of the studies. The PK/PD targets in the intervention groups differed across the studies. For beta-lactam, the target concentration was set at > 4 × MIC in three studies [27,28,29] and > 1 × MIC in one study [30], and the dosing was designed to achieve 100% fT > 4 × MIC or 100% fT > MIC, respectively. In these protocol, 100% fT > 4 × MIC means that the free drug concentration exceeds four times the MIC at 100% of the dosing interval. For aminoglycoside, peak and trough concentrations were used as the target, whereas area under the curve/minimum inhibitory concentration (AUC/MIC) was used for vancomycin and quinolones. TDM was not performed simultaneously for multiple antibiotics in any of the identified studies or in those found on the ClinicalTrials.gov and World Health Organization International Clinical Trial Registry Platform.
Primary outcome
All five studies had 28-day mortality data available. Of the 1011 patients, 26.9% (137 of 510 patients) in the TDM group and 28.3% (142 of 501 patients) in the control group died within 28 days of randomization (Fig. 2, Table 2). The RR was 0.94 (95% CI, 0.77–1.14). Heterogeneity was not observed for the primary outcome (I2 = 0%, χ2 = 2.52, P = 0.64).
Forest plot of TDM and control group comparing 28-day mortality (A), hospital mortality (B), ICU length of stay (C), clinical cure (D), target attainment in 24 h (E), and target attainment at day 3 (F). CI confidence interval, df degrees of freedom, M-H Mantel–Haenszel test, IV inverse variance, RR risk ratio, TDM therapeutic drug monitoring
Secondary outcomes
In the meta-analysis of included RCTs, the pooled RRs in TDM group were 1.14 (95% CI, 0.88–1.48) for target attainment at day 1, 1.35 (95% CI, 0.90–2.03) for target attainment at day 3, 1.23 (95% CI, 0.91–1.67) for clinical cure, and 0.96 (95% CI: 0.76–1.20) for in-hospital mortality. Severe heterogeneity was observed in target attainment at day 1 (I2 = 74%, χ2 = 11.54, P = 0.009) and day 3 (I2 = 77%, χ2 = 8.71, P = 0.01) (Fig. 2, Table 2). In the meta-analysis of RCTs for length of stay in the ICU, mean difference in the TDM group was 0 day (95% CI, − 2.18–2.19), and severe heterogeneity was observed (I2 = 72%, χ2 = 7.07, P = 0.03). Regarding safety outcomes, Bartal’s study reported nephrotoxicity in 2 patients (4.7%) in the TDM group and 8 patients (21.1%) in the control group, while Hagel reported adverse events in 20 patients (15.7%) in the TDM group and 27 patients (21.3%) in the control group. However, no meta-analysis was performed since there were no safety outcome that could be integrated between these two studies.
Subgroup analysis
Subgroup analysis included several analyzable studies on beta-lactam antibiotics and meta-analysis was performed. In two studies of 290 patients included for the analysis of 28-day mortality, there was no significant difference between two groups (TDM group: 20.5% [30 of 146 patients], control group: 25.7% [37 of 144 patients], RR: 0.94 [95% CI, 0.77–1.14]) (Additional file 1: Fig. S2). The pooled RRs in TDM group were 1.25 (95% CI, 0.91–1.73) for target attainment at day 1, 1.67 (95% CI, 0.98–2.85) for target attainment at day 3, and 1.47 (95% CI, 0.67–3.20) for clinical cure.
Risk of bias assessment
For primary outcome, one RCT was rated as high risk owing to bias arising from the randomization process (Fig. 3). In the study by Bartal, patients were allocated to study groups by the last digit of their national identification card number, causing a possible bias at the point of allocation concealment. Furthermore, two RCTs by Bartal and Waele were rated as high risk owing to deviations from the intended intervention. This occurred because, in both studies, the participants or clinicians might have known what groups patients were assigned to. Furthermore, whether appropriate analyses, such as ITT analyses, were performed to consider allocation effects was unclear. Consequently, the quality of evidence for primary outcome was rated as moderate; the grade was lowered by one point owing to imprecision of the study (the CIs crossed clinical decision thresholds) (Table 2). The quality of the evidence for each secondary outcome was very low to low.
Publication bias
The presence of publication bias was considered for the primary outcome of included RCT studies as indicated by the funnel plot (Additional file 1: Fig. S1). It was visually symmetric, indicating a low possibility of heterogeneity and reporting bias. However, the number of published studies was small [24].
Discussion
This systematic review and meta-analysis showed no significant difference in 28-day mortality between TDM-based regimens and standard protocols for the administration of antibiotics in critically ill patients. Similarly, target attainment, clinical cure, in-hospital mortality, and length of stay in the ICU were not associated with TDM-based regimens.
Previous studies have performed systematic reviews and meta-analysis evaluating TDM-based regimens of antibiotics compared to standard protocols for infectious patients. However, these studies were restricted by limited antibiotic types, inclusion of cohort studies, or inclusion of non-critically ill patients such as febrile neutropenic patients [31, 32]. In particular, recent systematic review and meta-analysis, which investigated the clinical efficacy of beta-lactam antibiotics in critically ill patients, included 11 studies despite limiting the type of antibiotics, making the analysis broader than our study [18]. However, only four of them were RCTs, and the remaining seven were retrospective observational studies. Furthermore, two of these retrospective observational studies were conference abstracts. Two of the RCTs were included in our study as well, but the other two were studies since one was unclear whether they clearly fit the definition of critically ill patients, and another did not have applicable outcome. Two of the RCTs included in our study were published after the publication of this study, resulting in many of the included RCTs being different. To our knowledge, our systematic reviews and meta-analysis is the first to only include RCTs and critically ill patients in evaluating the efficacy of TDM in all antibiotics.
In a systematic review examining the efficacy of TDM-guided dosing regimens of beta-lactam antibiotics, the 28-day mortality was not significantly different, which is similar to the results of our study [18]. Factors that influence the clinical outcomes such as 28-day mortality include whether drug concentrations in the blood are within the appropriate range to target the organisms causing the infection [33, 34]. In these studies, target attainment was significantly higher in the TDM group; however, the target was set differently because one study used continuous infusion of meropenem. Furthermore, the number of days was not set as a criterion for analysis, and it might pose a potential risk of greater variability in the results compared to that with a strictly defined time point. To avoid these ambiguities, we set up target attainment in day 1 and day3 as the outcome in our study. However, there was no difference between the two groups with respect to target attainments, while it is not so surprising as to day 1 since day 1 is the point at which the first blood levels are measured, and dose adjustments are made based on those results. In the individual analysis of target attainment, Ewoldt's results for both day 1 and day 3 were inversely oriented toward the other studies. This study examined the effectiveness of the optimization by model-informed precision dosing using TDM, and this study design is slightly different from the usual antibiotic dosing strategy based on TDM. Therefore, these results may be one of the reasons for the lack of valid results in the meta-analysis. The study also used two antibiotic agents, beta-lactam antibiotics and ciprofloxacin, and integrated outcomes, but these may not have been significant in our study. As a result, clinical outcomes such as 28-day mortality and clinical cure may not have differed.
Furthermore, the impact of achieving target attainment on clinical outcomes has not yet been determined. A study investigating the achievement of beta-lactam antibiotic concentration targets using TDM for critically ill patients showed that optimal exposure of unbound beta-lactams is not achieved in a significant proportion of the patients. However, failure to achieve PK/PD targets was not associated with negative clinical outcomes, suggesting that there was a discrepancy between target attainment and clinical outcomes [35]. Conversely, the DALI study, which examined beta-lactam antibiotic dosing in critically ill patients and the association between antibiotic concentrations and clinical outcome, revealed that the effect of increasing fT > MIC was more significant in patients with lower Acute Physiology and Chronic Health Evaluation II severity score [12]. Therefore, comparisons between TDM-based regimens and standard protocols for groups with different severities should be conducted in future studies.
The targets set for blood concentrations varied among studies included in the meta-analysis. For quinolones, glycopeptides, and aminoglycosides, studies commonly used AUC/MIC for target attainment, whereas two different indices, MIC and 4 × MIC, were used for beta-lactams, depending on the study. These differences may be one of the sources of variation and heterogeneity among studies, although many target attainment breakpoints are considered to be set by convention or expert opinion [36]. A study investigating the difference in efficacy among critically ill patients treated with meropenem or piperacillin–tazobactam divided the target attainment into three groups: < 100% fT > MIC, 100% fT > MIC < 4 × MIC, and 100% fT > 4 × MIC. This study showed that 100% fT > MIC was associated with improved outcome, whereas no significant benefit was observed in the 100% fT > 4 × MIC group [37]. Although the target of the included studies was different as they included both MIC and 4 × MIC, the goal of TDM might not necessarily be to achieve 4 × MIC, even in critically ill patients. Furthermore, owing to the strict criteria of reaching 4 × MIC, the included studies also showed that only 33.9% of the TDM group met target attainment on day 1 in a study by Hagel, and this may have been the reason why the meta-analysis did not show differences in target attainment. In addition, other studies did not present separate results for beta-lactams; thus, their effects were unknown. Accordingly, future studies may have to focus on beta-lactams and set attainable targets or compare the clinical and pharmacological outcomes between the fT > MIC and fT > 4 × MIC targets in continuous and intermittent infusion setting. Furthermore, a previous systematic review and meta-analysis evaluating the association between AUC/MIC and clinical outcomes for vancomycin was inconsistent owing to the lack of standardized methods and insufficient data, thereby failing to obtain a positive outcome with AUC/MIC [38]. Even in our meta-analysis, no individual data were obtained for vancomycin and ciprofloxacin using AUC/MIC, and separate studies are required to investigate TDM-based regimen using AUC/MIC.
In summary, our meta-analysis did not find significant results for any of the outcomes, suggesting that this was due to inconsistent protocol and outcome settings across studies rather than a negative effect of TDM-based antibiotic regimen. In addition, there were several favorable results for TDM-based regimen, and no clear harms from TDM were observed. Therefore, our study does not reject TDM-based antibiotic strategies, and it is believed that effective results would be obtained if they are targeted to optimal clinical cases.
Our study had several limitations. First, because we limited our inclusion criteria to only RCT studies and critically ill patients, only five studies were included for the meta-analysis, which may have resulted in reduced statistical power. If we detect a significant effect from a 26.9% mortality rate in the TDM and 28.3% in the control groups, 16,146 samples would be required for each group (alpha error; 0.05, beta error; 0.80). However, variation in patient background and inclusion of non-RCTs may ultimately lead to heterogeneity of results and compromise the certainty of the obtained results. It is necessary to conduct RCTs on TDM that clearly target sepsis in the future. Second, some of our study outcomes showed significant statistical heterogeneity, which may be caused by the variation of definitions in each study. Particularly, Waele defined clinical cure as an improvement of clinical signs, whereas Bartel used a negative culture and normalization of white blood cell counts, and Hagel used no longer requiring additional antibiotics. In such cases, a narrower definition may narrow the patient population and cause difficulties in comparing the same population. If two studies with high bias risk are excluded, only the study by Hagel in which clinical cure is strictly defined is remained, and the RR would show significant difference (RR, 2.05; 95% CI, 1.10–3.80). Therefore, a clear definition of outcomes including clinical cure and target attainment must be adequately defined in future studies. Third, we used only a limited number of search engines for the literature search in our study. In particular, we did not use EMBASE, which has the potential to provide more extensive and systematic search results [added reference]. In the future, it is necessary to plan a search strategy that includes EMBASE in order to collect more appropriate literature.
Conclusions
For critically ill patients, TDM-based antibiotic regimens were not associated with 28-day mortality, in-hospital mortality, clinical cure, target attainment at day 1 and day 3, and length of stay in the ICU when compared with standard protocols. Further RCTs in which outcomes are clearly defined, include disease severity, and focus on sepsis patients are warranted to verify the true efficacy of TDM.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- TDM:
-
Therapeutic drug monitoring
- ICU:
-
Intensive care unit
- PK/PD:
-
Pharmacokinetics/pharmacodynamics
- RCT:
-
Randomized control trial
- GRADE:
-
Grading of Recommendations Assessment, Development, and Evaluation
- RR:
-
Risk ratios
- CI:
-
Confidence intervals
- SD:
-
Standard deviation
- IQR:
-
Interquartile
- AUC:
-
Area under the curve
- MIC:
-
Minimum inhibitory concentration
- ITT:
-
Intention to treat
References
Kollef MH, Sherman G, Ward S, Fraser VJ. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999;115(2):462–74.
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118(1):146–55.
Shorr AF, Micek ST, Welch EC, Doherty JA, Reichley RM, Kollef MH. Inappropriate antibiotic therapy in Gram-negative sepsis increases hospital length of stay. Crit Care Med. 2011;39(1):46–51.
Roberts JA, Abdul-Aziz MH, Lipman J, Mouton JW, Vinks AA, Felton TW, et al. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14(6):498–509.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–143.
Baptista JP, Udy AA, Sousa E, Pimentel J, Wang L, Roberts JA, et al. A comparison of estimates of glomerular filtration in critically ill patients with augmented renal clearance. Crit Care. 2011;15(3):R139.
Martin JH, Fay MF, Udy A, Roberts J, Kirkpatrick C, Ungerer J, et al. Pitfalls of using estimations of glomerular filtration rate in an intensive care population. Intern Med J. 2011;41(7):537–43.
Udy AA, Varghese JM, Altukroni M, Briscoe S, McWhinney BC, Ungerer JP, et al. Subtherapeutic initial β-lactam concentrations in select critically ill patients: association between augmented renal clearance and low trough drug concentrations. Chest. 2012;142(1):30–9.
Udy AA, Roberts JA, Lipman J. Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med. 2013;39(12):2070–82.
De Waele JJ, Lipman J, Akova M, Bassetti M, Dimopoulos G, Kaukonen M, et al. Risk factors for target non-attainment during empirical treatment with β-lactam antibiotics in critically ill patients. Intensive Care Med. 2014;40(9):1340–51.
Sime FB, Roberts MS, Roberts JA. Optimization of dosing regimens and dosing in special populations. Clin Microbiol Infect. 2015;21(10):886–93.
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, et al. DALI: defining antibiotic levels in intensive care unit patients: are current β-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis. 2014;58(8):1072–83.
Hanrahan TP, Harlow G, Hutchinson J, Dulhunty JM, Lipman J, Whitehouse T, et al. Vancomycin-associated nephrotoxicity in the critically ill: a retrospective multivariate regression analysis. Crit Care Med. 2014;42(12):2527–36.
Beumier M, Casu GS, Hites M, Wolff F, Cotton F, Vincent JL, et al. Elevated β-lactam concentrations associated with neurological deterioration in ICU septic patients. Minerva Anestesiol. 2015;81(5):497–506.
Sime FB, Roberts MS, Tiong IS, Gardner JH, Lehman S, Peake SL, et al. Can therapeutic drug monitoring optimize exposure to piperacillin in febrile neutropenic patients with haematological malignancies? A randomized controlled trial. J Antimicrob Chemother. 2015;70(8):2369–75.
Muller AE, Huttner B, Huttner A. Therapeutic drug monitoring of beta-lactams and other antibiotics in the intensive care unit: which agents, which patients and which infections? Drugs. 2018;78(4):439–51.
Cusumano JA, Klinker KP, Huttner A, Luther MK, Roberts JA, LaPlante KL. Towards precision medicine: Therapeutic drug monitoring-guided dosing of vancomycin and β-lactam antibiotics to maximize effectiveness and minimize toxicity. Am J Health Syst Pharm. 2020;77(14):1104–12.
Pai Mangalore R, Ashok A, Lee SJ, Romero L, Peel TN, Udy AA, et al. Beta-lactam antibiotic therapeutic drug monitoring in critically ill patients: a systematic review and meta-analysis. Clin Infect Dis. 2022;75(10):1848–60.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343: d4002.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Bartal C, Danon A, Schlaeffer F, Reisenberg K, Alkan M, Smoliakov R, et al. Pharmacokinetic dosing of aminoglycosides: a controlled trial. Am J Med. 2003;114(3):194–8.
De Waele JJ, Carrette S, Carlier M, Stove V, Boelens J, Claeys G, et al. Therapeutic drug monitoring-based dose optimisation of piperacillin and meropenem: a randomised controlled trial. Intensive Care Med. 2014;40(3):380–7.
Hagel S, Bach F, Brenner T, Bracht H, Brinkmann A, Annecke T, et al. Effect of therapeutic drug monitoring-based dose optimization of piperacillin/tazobactam on sepsis-related organ dysfunction in patients with sepsis: a randomized controlled trial. Intensive Care Med. 2022;48(3):311–21.
Roggeveen LF, Guo T, Fleuren LM, Driessen R, Thoral P, van Hest RM, et al. Right dose, right now: bedside, real-time, data-driven, and personalised antibiotic dosing in critically ill patients with sepsis or septic shock-a two-centre randomised clinical trial. Crit Care. 2022;26(1):265.
Ewoldt TMJ, Abdulla A, Rietdijk WJR, Muller AE, de Winter BCM, Hunfeld NGM, et al. Model-informed precision dosing of beta-lactam antibiotics and ciprofloxacin in critically ill patients: a multicentre randomised clinical trial. Intensive Care Med. 2022;48(12):1760–71.
Ye ZK, Tang HL, Zhai SD. Benefits of therapeutic drug monitoring of vancomycin: a systematic review and meta-analysis. PLoS ONE. 2013;8(10): e77169.
Luxton TN, King N, Wälti C, Jeuken LJC, Sandoe JAT. A systematic review of the effect of therapeutic drug monitoring on patient health outcomes during treatment with carbapenems. Antibiotics (Basel). 2022. https://doi.org/10.3390/antibiotics11101311.
Roberts JA, Ulldemolins M, Roberts MS, McWhinney B, Ungerer J, Paterson DL, et al. Therapeutic drug monitoring of beta-lactams in critically ill patients: proof of concept. Int J Antimicrob Agents. 2010;36(4):332–9.
Cojutti PG, Lazzarotto D, Candoni A, Dubbini MV, Zannier ME, Fanin R, et al. Real-time TDM-based optimization of continuous-infusion meropenem for improving treatment outcome of febrile neutropenia in oncohaematological patients: results from a prospective, monocentric, interventional study. J Antimicrob Chemother. 2020;75(10):3029.
Wong G, Briscoe S, McWhinney B, Ally M, Ungerer J, Lipman J, et al. Therapeutic drug monitoring of β-lactam antibiotics in the critically ill: direct measurement of unbound drug concentrations to achieve appropriate drug exposures. J Antimicrob Chemother. 2018;73(11):3087–94.
Berry AV, Kuti JL. Pharmacodynamic thresholds for beta-lactam antibiotics: a story of mouse versus man. Front Pharmacol. 2022;13: 833189.
Scharf C, Liebchen U, Paal M, Taubert M, Vogeser M, Irlbeck M, et al. The higher the better? Defining the optimal beta-lactam target for critically ill patients to reach infection resolution and improve outcome. J Intensive Care. 2020;8(1):86.
Dalton BR, Rajakumar I, Langevin A, Ondro C, Sabuda D, Griener TP, et al. Vancomycin area under the curve to minimum inhibitory concentration ratio predicting clinical outcome: a systematic review and meta-analysis with pooled sensitivity and specificity. Clin Microbiol Infect. 2020;26(4):436–46.
Acknowledgements
The authors thank the committees of Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock 2024 (J-SSCG 2024) for this publication.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
NT, YK, KKu, ME, KiK, YO, TN contributed to the conception and study design, and NT, YO contributed to acquisition of data. NT performed statistical analysis and drafting the manuscript, and NT and YK contributed to the interpretation of data. All authors contributed to subsequent drafts and approved manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Literature search strategy for each database. Figure S1. Forest plot of TDM and control group in beta-lactam antibiotics. Figure S2. Funnel plot for the publication bias assessment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Takahashi, N., Kondo, Y., Kubo, K. et al. Efficacy of therapeutic drug monitoring-based antibiotic regimen in critically ill patients: a systematic review and meta-analysis of randomized controlled trials. j intensive care 11, 48 (2023). https://doi.org/10.1186/s40560-023-00699-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-023-00699-8