Abstract
High mortality and morbidity rates associated with severe infections in the critically ill continue to be a significant issue for the healthcare system. In view of the diverse and unique pharmacokinetic profile of drugs in this patient population, there is increasing use of therapeutic drug monitoring (TDM) in attempt to optimize the exposure of antibiotics, improve clinical outcome and minimize the emergence of antibiotic resistance. Despite this, a beneficial clinical outcome for TDM of antibiotics has only been demonstrated for aminoglycosides in a general hospital patient population. Clinical outcome studies for other antibiotics remain elusive. Further, there is significant variability among institutions with respect to the practice of TDM including the selection of patients, sampling time for concentration monitoring, methodologies of antibiotic assay, selection of PK/PD targets as well as dose optimisation strategies. The aim of this paper is to review the available evidence relating to practices of antibiotic TDM, and describe how TDM can be applied to potentially improve outcomes from severe infections in the critically ill.
Similar content being viewed by others
Review
Introduction
Despite advances in contemporary medicine, severe infections and sepsis-related mortality in critically ill patients remain a global problem [1–4]. An important consideration of antimicrobial treatment failure in the critically ill is inadequate drug exposure from use of dosing regimens derived in non-critically ill patients [5]. There is extensive evidence of sub-therapeutic exposure from standard doses across different antibiotic classes including beta-lactams [6, 7], aminoglycosides [8], glycopeptides [9], fluoroquinolones [10], and oxazolidinones [11]. This can be a direct consequence of pharmacokinetic alterations emanating from the complex pathophysiologic processes associated with severe infection. Multi-drug resistant organisms more frequently encountered in the critically ill also alter the dosing requirements for these patients [12–14]. Appropriate, timely antibiotic therapy given at an adequate dose is thought to be of paramount importance in improving clinical outcome of severe sepsis [15]. To further increase the likelihood of achieving a good patient outcome from infection, optimizing antibiotic dosing is crucial. Therapeutic drug monitoring (TDM), a tool traditionally used primarily to minimize toxicity in drugs with narrow therapeutic window or drugs with complex pharmacokinetics, is being increasingly used for antibiotic dose optimization in the attempt to improve attainment of pharmacokinetic/pharmacodynamic (PK/PD) targets and outcomes of severe infections in the critically ill [16–19].
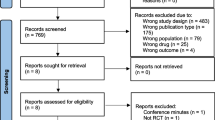
Despite a growth in practice of antibiotic TDM globally, clinical outcome studies on TDM-based interventions are limited. To date, definitive benefit is only demonstrated for aminoglycosides [20, 21]. Further, there is significant variability among institutions with respect to the practice of TDM including the selection of patients, sampling time for concentration monitoring, methodologies of antibiotic assay, selection of PK/PD target as well as dose optimisation strategies [22]. The aim of this paper is therefore to critically review the available evidence of the practices of antibiotic TDM, and describe how TDM can be utilised to potentially improve critically ill patient outcomes from severe infections.
Pharmacokinetic changes in the critically ill
Altered pharmacokinetics of antibiotics in ICU patients with severe infections secondary to dynamic disease processes and medical interventions has been widely described [10, 11, 23, 24]. Altered drug exposure may also be observed in patients with severe sepsis outside the ICU. Specifically, changes in volume of distribution (Vd) and drug clearance (Cl) may lead to sub-therapeutic or toxic exposures of antibiotics when standard doses are used. Table 1 describes common factors that may alter pharmacokinetics of antibiotics in critically ill patients. Fluid resuscitation, capillary leakage and third space losses could substantially increase Vd of hydrophilic antibiotics such as beta-lactams and aminoglycosides, the Vd of which approximates the extracellular fluid volume. The Cl of antibiotics is dependent on patient organ function, drug clearance mechanisms and extracorporeal interventions given to the patient. Renal hypoperfusion, acute kidney injury and end-organ failure decrease Cl of antibiotics. On the contrary, augmented renal clearance (ARC) has been described in critically ill patients, where increased elimination of antibiotics lead to sub-therapeutic concentrations [25, 26]. The impact of interventions such as renal replacement therapy (RRT) and extracorporeal membrane oxygenation (ECMO) on antibiotic pharmacokinetics is multifactorial, variable and complex and have been discussed in detail elsewhere [27–30].
Main pharmacokinetic/pharmacodynamic indices associated with antibiotic efficacy
The three main PK/PD indices that describe antibiotic exposure required for bacterial stasis or killing are summarised in Tables 2 and 3. The PK/PD targets for individual groups of antibiotics proven or proposed to be associated with clinical advantage based on animal and clinical studies are also listed. Of note, all PK/PD targets are expressed in relation to the minimal inhibitory concentration (MIC) of the pathogen, highlighting that beyond measurement of antibiotics concentrations, accurate and timely determination of MIC also should be considered a cornerstone of antibiotic TDM. MICs for TDM can be defined by various strategies, including Etest, disc method, micro-dilution broth method and automated microbiology system (e.g. Phoenix, Vitek 2), or adoption of local antibiograms, EUCAST and CLSI breakpoints. Clinicians utilising TDM in treating severe infections, especially those that involve resistant organisms, need to be aware of the limitations of each method. These limitations have been discussed in detail elsewhere [31–35].
How TDM could be utilised to optimize PK/PD in treating severe infections – clinical evidence and practical issues
Beta-lactams
Given the excellent safety profile of beta-lactams, the main aim of TDM with these antibiotics is to maximise efficacy through achievement of therapeutic exposures [36]. Targets required to achieve a favourable clinical outcome in the critically ill have been described to be higher than that supported by studies in animal models or in non-ICU patients (Table 2). A PK/PD target of 100% fT>MIC as against fT>MIC lower than 100% was associated with significantly greater clinical cure and bacteriological eradication in septic critically ill patients with bacteremia, lower respiratory tract or complicated urinary tract infection treated with cefepime and ceftazidime [18]. Tam et al. found similar associations against gram-negative infections, although proposed an even higher PK/PD target with cefepime (on concurrent aminoglycosides) [37]. Unfortunately, achievement of these higher drug concentrations in ICU patients is infrequent, especially in the early phase of sepsis [6, 38]. Other dosing strategies have been proposed for optimizing beta-lactams exposure, these include dose adjustments made specific to interventions, continuous infusion and dosing monograms. However, individual reports still demonstrate the extreme difficulties in achieving appropriate drug concentrations in some severely ill patients [30, 39–42]. TDM appeared to be a feasible strategy to adapt beta-lactam dosing and may complement these other measures [12, 43]. The potential benefit of beta-lactam TDM probably warrants evaluation of its value for treating severe infections in the critically ill, despite the fact that the optimal PK/PD target remains unclear.
Beta-lactams have a low likelihood of toxicity. However, given the high drug concentration requirement in some severely ill patients for difficult to treat infections, toxicity becomes an issue that could be minimize with TDM. No threshold of toxicity has been defined currently, however TDM could aid early recognition of potential drug-related toxicities (especially neurological toxicity) in susceptible patients [44–46].
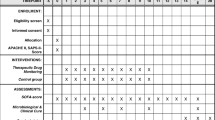
Selection of patients
Patients with sepsis or septic shock, who potentially would benefit from TDM, are those with labile blood pressure (ie septic shock), dynamic renal function, burns injury, receiving RRT or ECMO, infected with resistant organisms, and where neurological toxicity is clinically suspected [22, 47, 48].
Sampling time
Trough concentrations sampled at steady state (generally after 3–4 doses given) are appropriate for determining whether PK/PD targets have been achieved. Additional sampling (e.g. at mid-dosing interval) is appropriate for a more accurate calculation of pharmacokinetic parameters and would be useful for a Bayesian-driven dose adaptation using appropriate computer software.
Assay
Liquid chromatography is the most widely used assaying method for beta-lactam TDM [49–53]. A variety of published protocols are available to suit clinical and laboratory needs in different institutes [22]. The high equipment and personnel costs as well as the relatively prolonged processing time (between 6–24 hours) are disadvantages of the method that might hinder the wider application of beta-lactam TDM. Direct measurement of unbound drug concentrations is also recommended in critically ill patients with hypoalbuminaemia receiving highly protein-bound antibiotics [54].
Dose adjustment strategies
Generalized but non-specific dose adjustment methods including changing dose amount or frequency, utilization of extended or continuous infusion have been used in most units practising TDM routinely [22]. New dosages can be determined more accurately by calculating the individual patient’s drug clearance from measured beta-lactam concentrations. Dosing nomograms and PK softwares for dose adjustment are available but have not been widely tested nor validated [39, 55].
Aminoglycosides
With activity against gram-negative bacteria, aminoglycosides are an inexpensive group of antibiotics frequently used in the ICU for treatment of severe infections. Once-daily administration to maximize its concentration-dependent effect and post-antibiotic effect is widely accepted as the standard regimen in general ward patients, and in ICU patients as well. For gentamicin, the regimen itself has been proven to provide small improvement in efficacy and/or reduced nephrotoxicity, and the benefit is augmented with active TDM [19, 56–59]. Gentamicin, tobramycin and amikacin are the three antibiotics mostly subjected to TDM. In non-critically ill patients, the aim of TDM for extended interval aminoglycoside dosing is mainly to reduce toxicity, as arguably the single high dose would provide an adequate Cmax (maximum concentration in dosing interval) in most cases [60]. However, these doses in critically ill patients are associated with a decreased rate of achievement of peak and AUC (area under the concentration-time curve) targets [8, 61–64]. Although minimizing the likelihood of toxicity using TDM is important in critically ill patients, dose adaptation to avoid under-dosing and maximize efficacy is also valuable. Given the high mortality rate of severe infections in the critically ill, high variability in aminoglycoside PK, and the proven benefit of aminoglycoside TDM in general patient populations, TDM practice tailored to the critically ill population is advised.
Selection of patients
Measurement of Cmax concentrations is advisable in patients with conditions associated with an increased Vd (eg. burns, septic shock). Those with unstable hemodynamic and/or renal function, undergoing RRT, infected with resistant pathogens would also benefit from routine TDM. AUC based monitoring is preferred, but where not possible, trough concentration monitoring to minimize toxicity is suggested especially for patients receiving regimens exceeding 48 hours [65–68].
Sampling time
Traditionally, measuring one random concentration between 6–14 hours after commencement of antibiotic infusion with interpretation using a nomogram has been used for aminoglycosides. Given these nomograms are more commonly developed in non-critically ill patients, use of this approach in the critically ill is not recommended [57, 69]. TDM with two samples drawn at 1 (30-mins post completion of drug infusion) and 6–22 hours post administration [70, 71] allows description of peak concentrations and AUC using linear regression or Bayesian approaches and a more accurate prediction of future dosing requirements.
Assay
Commercially available immunoassays are the most frequently used method for aminoglycoside TDM. Although other methods such as capillary zone electrophoresis and chromatography offer higher precision, the inexpensive immunoassays have been validated and are appropriate for routine daily clinical practice [72, 73].
Dose adjustment strategies
The PK/PD targets conventionally used for aminoglycoside TDM are described in Table 3. To the best of our knowledge, no other targets have been established especially for the critically ill population. Calculation of the AUC for an individual patient and subsequent dosage adjustment using dosing software should be considered the ideal approach. Although clinical advantages of using software based dosing methods have not been demonstrated, they should be considered preferred for critically ill patients with severe infections [74–76].
Vancomycin
The benefit of vancomycin TDM both for avoidance of toxicity as well as improving clinical outcome remains controversial. Conflicting evidence exists in regards to correlation of nephrotoxicity with high serum vancomycin concentrations [77–84]. A recent meta-analysis [85] concluded that the collective literature favours the association. However it is still debatable whether the high concentration or kidney damage is the preceding event. Similarly controversy exists with respect to ototoxicity [86, 87] as well as benefit in clinical outcome [17, 84, 88–90]. A meta-analysis by Ye et al.[91] suggested TDM significantly increases the likelihood of clinical efficacy and decreases the rate of nephrotoxicity. There is also a good agreement in the benefit of TDM to prevent the emergence of vancomycin resistant organisms with trough concentration above 10 mg/L [90, 92, 93].
Selection of patients
TDM is warranted to avoid toxicity in patients receiving high doses; during concomitant therapy with other nephrotoxic or ototoxic agents, in patients with unstable renal function, those receiving prolonged therapy (>3 to 5 days), during RRT and in hemodynamically unstable critically ill septic patients [16, 94].
Sampling time
Trough concentrations are modestly correlated with AUC enabling prediction of the target AUC/MIC [95, 96]. Based on available techniques, samples should be taken at pharmacokinetic steady state, which would usually be after about four doses (assuming 12-hourly dosing) [97]. In patients with renal dysfunction where half life is prolonged, steady state may not be achieved at the fourth dosing and therefore a trough concentration at this time may underestimate steady-state antibiotic exposure [97, 98]. This should be taken into consideration when making any dose adjustment.
Assay
Immunoassay is the most widely used commercial assay [99]. Currently there is no data indicating the superiority of any of the immunoassay methods over the others [100]. However, bias due to lack of between-method standardisation and high variability of measurement between methods is likely [101, 102]. Immunoassays remain appropriate for daily clinical TDM.
Dose adjustment strategies
Dose adjustments can be made by proportionally increasing or decreasing the dose relative to the ratio of the measured and the target concentration. The target concentrations commonly used for intermittent (15–20 mg/L) and continuous dosing (20–25 mg/L) are not the same with a higher continuous infusion target required to ensure the achievement of the same AUC as the intermittent dosing. Methodologies for dose individualization based on calculation of individual pharmacokinetic parameters and PK/PD targets (AUC/MIC) are available but not widely adopted in clinical practice [103]. Real time Bayesian forecasting coupled with TDM is thought to be most accurate for dose adaptation [104, 105].
No conclusive evidence supports the benefit of CI as a dose optimization strategy. It is not superior to intermittent dosing in terms of microbiological and clinical outcomes [106–111]. It may be considered though as a faster means to achieve consistent therapeutic concentrations given an adequate loading dose is used to avoid initial sub-therapeutic exposure [9, 112–114]. A recent meta- analysis [115] suggested a potential benefit of CI in reducing risk of nephrotoxicity.
Linezolid
The variability in linezolid pharmacokinetics was traditionally regarded less significant than with other antibiotics and consequently dose adjustments were considered unnecessary even in patients with renal and hepatic impairments [116]. However, accumulation of linezolid in renal insufficiency has been shown to be likely and results in toxicities such as pancytopenia, thrombocytopenia and liver dysfunction [117–120]. Reduced clearance has also been suggested in moderate hepatic insufficiency [121]. Contrasting reports exist on the possibility of disease related pharmacokinetic alterations. Consequently standard doses may result in a variable pharmacodynamic exposure [122], and are reported in the critically ill population with burns injuries [123, 124]. Elevated plasma concentration and associated risk of toxicity have also been reported [125–127]. In general, data to date indicates that TDM may be required in about 30 to 40% of patients to avoid dose-dependent toxicity as well as therapeutic failure [24, 122]. The impact of linezolid TDM on clinical outcome is yet to be demonstrated.
Selection of patients
A universal TDM program for linezolid is not supported based on current clinical data. Critically ill patients with sepsis, burns, pleural and peritoneal effusions, organ failure; patients infected with multidrug resistant bacteria; those receiving concomitant therapy with drugs that alter linezolid concentrations as well as those receiving long term linezolid therapy may benefit from TDM [121, 127, 128].
Sampling time
Trough concentrations are well correlated with AUC and are sufficient for linezolid TDM and estimation of an AUC/MIC ratio [122, 129]. The initial TDM sample should be taken just after pharmacokinetic steady state is achieved (usually considered on the third day of therapy).
Assay
HPLC methods have been published for linezolid TDM in plasma [128, 130], dried plasma spots [131, 132] and oral fluid [133] with good correlations between methods.
Dose adjustment strategies
Dose adjustments can be made by proportionally increasing or decreasing the dose in reference to the target concentration range (Table 3). CI may be a valuable strategy to provide a stable therapeutic exposure.
Fluoroquinolones
Difficult-to-predict pharmacokinetics of fluoroquinolones, particularly ciprofloxacin, can occur in critically ill patients as well as other patient groups. TDM may be beneficial given this pharmacokinetic variability to avoid treatment failure as well as minimise the emergence of resistance, particularly in the presence of less susceptible pathogens such as Pseudomonas aeruginosa which may have MICs of >0.5 mg/l [21, 134, 135].
Ciprofloxacin accumulation necessitating dose reduction has been reported in non-critically ill patients with renal impairment [136], although Van Zanten et al.[10] argued that dose reduction is unnecessary in critically ill patients despite their observation of increased AUCs. Other authors [137–139] also do not support dose reduction since accumulation is generally rare. It is likely that in patients with renal and gastrointestinal failure, dose reduction will be required as both clearance mechanisms will be affected. However, factors such as significant extracorporeal clearance due to RRT could influence variability of concentration in the critically ill [140, 141]. TDM may thus be an advantage for ciprofloxacin, although has yet to be described for levofloxacin or moxifloxacin.
Selection of patients
Universal TDM is not recommended and no specific patient groups have been shown to benefit most from TDM. Patients with infections caused by organisms with a high MIC (>0.5 mg/L) may benefit most, as traditional dosing is likely to result in sub-optimal exposure in high proportion of these patients.
Sampling time
At least two samples (peak and trough) should be taken to estimate the AUC. Both of these samples should be measured at steady state. The peak should be sampled in the post distribution phase, i.e. at least 30 min from the end of bolus infusion [137].
Assay
HPLC is the predominant method for measuring fluoroquinolones in plasma [142, 143] with dried blood spots [144] also used for TDM. A method using capillary electrophoresis has also been described [145] and immunoassay may be a more convenient future alternative [146].
Dose adjustment strategies
A wide range of targets has been proposed, however AUC/MIC of 125 or a Cmax/MIC of 8–10 is mostly accepted for treatment of Gram negative pathogens. A validated approach for dose adjustment is not currently available. Generally, to increase the AUC0–24, increasing the dose (e.g. IV 400 mg to 600 mg) or the frequency of dose (12-hourly to 8-hourly) are the more common methods for dose adaptation.
Daptomycin
TDM data on daptomycin is limited. The high protein binding and variable renal clearance make daptomycin a plausible candidate for TDM to increase the likelihood of achieving PK/PD targets [147–149]. TDM might also be useful in reducing the risk of musculoskeletal toxicity where it is highly associated with a trough concentration (Cmin) of >24.3 mg/L [150], especially when higher than standard doses are used. Current data is probably not sufficient to support a systematic TDM program for daptomycin. In vivo and small patient cohort studies reported efficacy cutoffs of AUC/MIC of 666 and Cmax/MIC of 59–94, the optimal PK/PD target for clinical application is yet to be elucidated [151, 152]. However, critically ill patients with sepsis, thermal burn injuries, profound hypoalbuminaemia, those infected by less susceptable bacteria, and those receiving RRT could potentially benefit from TDM-guided therapy as a means of ensuring achievement of PK/PD targets. Validated chomatographic assay methods are available for quantification of daptomycin [153], but given the high protein-binding of daptomycin and prevelance of hypoalbuminaemia in the critically ill, direct measurement of unbound drug concentrations might be preferred for clinical practice.
Conclusion
TDM has traditionally served as a mechanism to minimize the toxicity of drugs. However, the approach to use TDM to maximize the therapeutic effects of less toxic compounds is becoming increasingly common. In the context of critical illness, there is strong data demonstrating that standard dosing regimens for many antibiotics frequently fail to provide optimal PK/PD exposure in critically ill patients. Given that pharmacokinetic exposures can be very difficult-to-predict in some patients, TDM is valuable to identify these patients and guide dose optimization. TDM can ensure attainment of PK/PD surrogate indicators of antibiotic efficacy, and therefore potentially improve patient outcome. A conservative approach to development of TDM programs is suggested because for many antibiotics, the personnel and resource costs are moderate and studies demonstrating conclusive clinical outcome advantages remain elusive. Based on the available data, a well-designed randomized controlled trial to determine the effect of TDM-guided dosing is supported.
Abbreviations
- AUC:
-
Area under the concentration-time curve
- f AUC/MIC:
-
Ratio of area under the concentration–time curve of the unbound drug and the minimal inhibitory concentration of the pathogen
- Cmax :
-
Peak concentration during a dosing interval
- Cmin :
-
Trough concentration during a dosing interval
- CLSI:
-
Clinical and Laboratory Standards Institute
- ECMO:
-
Extracorporeal membrane oxygenation
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- HPLC:
-
High-performance liquid chromatography
- ICU:
-
Intensive care unit
- MIC:
-
Minimal inhibitory concentration
- PK/PD:
-
Pharmacokinetics/pharmacodynamics
- RRT:
-
Renal replacement therapy
- TDM:
-
Therapeutic drug monitoring.
References
Bellomo R: Mortality in severe sepsis: an inconvenient truth. Crit Care Resusc. 2010, 12 (1): 6-8.
Boussekey N, Cantrel J, Dorchin Debrabant L, Langlois J, Devos P, Meybeck A, Chiche A, Georges H, Leroy O: Epidemiology, prognosis, and evolution of management of septic shock in a French intensive care unit: a five years survey. Crit Care Res Pract. 2010, 2010: 436427-
Melamed A, Sorvillo FJ: The burden of sepsis-associated mortality in the United States from 1999 to 2005: an analysis of multiple-cause-of-death data. Crit Care. 2009, 13 (1): R28-
Vincent J-L, Rello J, Marchall JC, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall CD, Sakr Y, Reinhart K: International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009, 302 (21): 2323-2329.
Roberts J, Abdul Aziz M, Lipman J, Mouton J, Vinks A, Felton T, Hope W, Farkas A, Neely M, Schentag J, Drusano G, Frey OR, Theuretzbacher U, Kuti JL, on behalf of The International Society of Anti-Infective Pharmacology and the Pharmacokinetics and Pharmacodynamics Study Group of the European Society of Clinical Microbiology and Infectious Diseases: Individualised antibiotic dosing for patients who are critically ill challenges and potential solutions. Lancet Inf Dis. 2014, 14 (6): 498-509.
Taccone FS, Laterre P-F, Dugernier T, Spapen H, Delattre IK, Wittebole X, De Backer D, Layeux B, Wallemacq P, Vincent J-L, Jacobs F: Insufficient beta-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care. 2010, 14 (4): R126-
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, Kaukonen KM, Koulenti D, Martin C, Montravers P, Rello J, Rhodes A, Starr T, Wallis SC, Lipman J, DALI Study: DALI: defining antibiotic levels in intensive care unit patients: are current beta-lactam antibiotic doses sufficient for critically ill patients?. Clin Infect Dis. 2014, 58 (8): 1072-1083.
Rea RS, Capitano B, Bies R, Bigos KL, Smith R, Lee H: Suboptimal aminoglycoside dosing in critically ill patients. Ther Drug Monit. 2008, 30 (6): 674-681.
Roberts JA, Taccone FS, Udy AA, Vincent JL, Jacobs F, Lipman J: Vancomycin dosing in critically ill patients: robust methods for improved continuous-infusion regimens. Antimicrob Agents Chemother. 2011, 55 (6): 2704-2709.
van Zanten AR, Polderman KH, van Geijlswijk IM, van der Meer GY, Schouten MA, Girbes AR: Ciprofloxacin pharmacokinetics in critically ill patients: a prospective cohort study. J Crit Care. 2008, 23 (3): 422-430.
Swoboda S, Ober MC, Lichtenstern C, Saleh S, Schwenger V, Sonntag HG, Haefeli WE, Hempel G, Hoppe-Tichy T, Weigand MA: Pharmacokinetics of linezolid in septic patients with and without extended dialysis. Eur J Clin Pharmacol. 2010, 66 (3): 291-298.
Taccone FS, Cotton F, Roisin S, Vincent J-L, Jacobs F: Optimal meropenem concentrations to treat multidrug-resistant pseudomonas aeruginosa septic shock. Antimicrob Agents Chemother. 2012, 56 (4): 2129-2131.
Tam VH, Rogers CA, Chang KT, Weston JS, Caeiro JP, Garey KW: Impact of multidrug-resistant Pseudomonas aeruginosa bacteremia on patient outcomes. Antimicrob Agents Chemother. 2010, 54 (9): 3717-3722.
Wegner C, Hubner NO, Gleich S, Thalmaier U, Kruger CM, Kramer A: One-day point prevalence of emerging bacterial pathogens in a nationwide sample of 62 German hospitals in 2012 and comparison with the results of the one-day point prevalence of 2010. GMS Hyg Infect Control. 2013, 8 (1): Doc12-
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L: Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006, 34 (6): 1589-1596.
Rybak MJ, Lomaestro BM, Rotschafer JC, Moellering RC, Craig WA, Billeter M, Dalovisio JR, Levine DP: Vancomycin therapeutic guidelines: a summary of consensus recommendations from the infectious diseases Society of America, the American Society of Health-System Pharmacists, and the Society of Infectious Diseases Pharmacists. Clin Infect Dis. 2009, 49 (3): 325-327.
Kullar R, Davis SL, Levine DP, Rybak MJ: Impact of vancomycin exposure on outcomes in patients with methicillin-resistant Staphylococcus aureus bacteremia: support for consensus guidelines suggested targets. Clin Infect Dis. 2011, 52 (8): 975-981.
McKinnon PS, Paladino JA, Schentag JJ: Evaluation of Area Under the Inhibitory Curve (AUIC) and Time Above the Minimum Inhibitory Concentration (T > MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008, 31 (4): 345-351.
van Lent-Evers NA, Mathôt RA, Geus WP, van Hout BA, Vinks AA: Impact of goal-oriented and model-based clinical pharmacokinetic dosing of aminoglycosides on clinical outcome: a cost-effectiveness analysis. Ther Drug Monit. 1999, 21 (1): 63-73.
Lacy MK, Nicolau DP, Nightingale CH, Quintiliani R: The pharmacodynamics of aminoglycosides. Clin Infect Dis. 1998, 27 (1): 23-27.
Forrest A, Nix DE, Ballow CH, Goss TF, Birmingham MC, Schentag JJ: Pharmacodynamics of intravenous ciprofloxacin in seriously Ill patients. Antimicrob Agents Chemother. 1993, 37 (5): 1073-1081.
Wong G, Brinkman A, Benefield RJ, Carlier M, De Waele JJ, El Helali N, Frey O, Harbarth S, Huttner A, McWhinney B, Misset B, Pea F, Preisenberger J, Roberts MS, Robertson TA, Roehr A, Sime FB, Taccone FS, Ungerer JP, Lipman J, Roberts JA: An international, multicentre survey of beta-lactam antibiotic therapeutic drug monitoring practice in intensive care units. J Antimicrob Chemother. 2014, 69 (5): 1416-1423.
Roberts JA, Norris R, Paterson DL, Martin JH: Therapeutic drug monitoring of antimicrobials. Br J Clin Pharmacol. 2012, 73 (1): 27-36.
Dong H, Wang X, Dong Y, Lei J, Li H, You H, Wang M, Xing J, Sun J, Zhu H: Clinical pharmacokinetic/pharmacodynamic profile of linezolid in severely ill intensive care unit patients. Int J Antimicrob Agents. 2011, 38 (4): 296-300.
Udy AA, Roberts JA, De Waele JJ, Paterson DL, Lipman J: What’s behind the failure of emerging antibiotics in the critically ill? Understanding the impact of altered pharmacokinetics and augmented renal clearance. Int J Antimicrob Agents. 2012, 39 (6): 455-457.
Udy AA, Varghese JM, Altukroni M, Briscoe S, McWhinney B, Ungerer J, Lipman J, Roberts JA: Sub-therapeutic initial β-lactam concentrations in select critically ill patients. Chest. 2012, 142 (1): 30-39.
Kielstein JT, Burkhardt O: Dosing of antibiotics in critically ill patients undergoing renal replacement therapy. Curr Pharm Biotechnol. 2011, 12 (12): 2015-2019.
Jamal J-A, Economou CJP, Lipman J, Roberts JA: Improving antibiotic dosing in special situations in the ICU: burns, renal replacement therapy and extracorporeal membrane oxygenation. Curr Opin Crit Care. 2012, 18 (5): 460-471.
Shekar K, Fraser JF, Smith MT, Roberts JA: Pharmacokinetic changes in patients receiving extracorporeal membrane oxygenation. J Crit Care. 2012, 27: 741-e749–e718
Choi GYS, Gomersall CD, Tian Q, Joynt GM, Freebairn R, Lipman J: Principles of antibacterial dosing in continuous renal replacement therapy. Crit Care Med. 2009, 37: 2268-2282.
Tam VH, Gamez EA, Weston JS, Gerard LN, Larocco MT, Caeiro JP, Gentry LO, Garey KW: Outcomes of bacteremia due to Pseudomonas aeruginosa with reduced susceptibility to piperacillin-tazobactam: implications on the appropriateness of the resistance breakpoint. Clin Infect Dis. 2008, 46 (6): 862-867.
Weisenberg SA, Morgan DJ, Espinal-Witter R, Larone DH: Clinical outcomes of patients with Klebsiella pneumoniae carbapenemase-producing K. pneumoniae after treatment with imipenem or meropenem. Diagn Microbiol Infect Dis. 2009, 64 (2): 233-235.
Bhat SV, Peleg AY, Lodise TPJ, Shutt KA, Capitano B, Potoski BA, Paterson DL: Failure of current cefepime breakpoints to predict clinical outcomes of bacteremia caused by gram-negative organisms. Antimicrob Agents Chemother. 2007, 51 (12): 4390-4395.
Vading M, Samuelsen O, Haldorsen B, Sundsfjord AS, Giske CG: Comparison of disk diffusion, Etest and VITEK2 for detection of carbapenemase-producing Klebsiella pneumoniae with the EUCAST and CLSI breakpoint systems. Clin Microbiol Infect. 2011, 17 (5): 668-674.
Kitzis M: Antibiotic assay. Antibiogram. Edited by: Courvalin P, Leclercq R, Rice LB. 2010, Portland, Oregon: ESKA Publishing, ASM Press, 75-88. 3
Sime FB, Roberts MS, Peake SL, Lipman J, Roberts JA: Does beta-lactam pharmacokinetic variability in critically ill patients justify therapeutic drug monitoring? A systematic review. Ann Intensive Care. 2012, 2 (1): 35-
Tam VH, McKinnon PS, Akins RL, Rybak MJ, Drusano GL: Pharmacodynamics of cefepime in patients with Gram-negative infections. J Antimicrob Chemother. 2002, 50 (3): 425-428.
Roberts JA, Ulldemolins M, Roberts MS, McWhinney B, Ungerer J, Paterson DL, Lipman J: Therapeutic drug monitoring of beta-lactams in critically ill patients: proof of concept. Int J Antimicrob Agents. 2010, 36: 332-339.
Pea F, Viale P, Cojutti P, Furlanut M: Dosing nomograms for attaining optimum concentrations of meropenem by continuous infusion in critically ill patients with severe gram-negative infections: a pharmacokinetics/pharmacodynamics-based approach. Antimicrob Agents Chemother. 2012, 56 (12): 6343-6348.
Roberts JA, Kirkpatrick CMJ, Roberts MS, Dalley AJ, Lipman J: First-dose and steady-state population pharmacokinetics and pharmacodynamics of piperacillin by continuous or intermittent dosing in critically ill patients with sepsis. Int J Antimicrob Agents. 2010, 35 (2): 156-163.
Lee GC, Liou H, Yee R, Quan CF, Neldner K: Outcomes of extended-infusion piperacillin-tazobactam: a retrospective analysis of critically ill patients. Clin Ther. 2012, 34 (12): 2297-2300.
Dulhunty JM, Roberts JA, Davis JS, Webb SA, Bellomo R, Gomersall C, Shirwadkar C, Eastwood GM, Myburgh J, Paterson DL, Starr T, Udy AA, Paul SK, Lipman J, Australian and New Zealand Intensive Care Society Clinical Trials Group: A protocol for a multicentre randomised controlled trial of continuous beta-lactam infusion compared with intermittent beta-lactam dosing in critically ill patients with severe sepsis: the BLING II study. Crit Care Resusc. 2013, 15 (3): 179-185.
Pea F, Cojutti P, Sbrojavacca R, Cadeo B, Cristini F, Bulfoni A, Furlanut M: TDM-guided therapy with daptomycin and meropenem in a morbidly obese. Critically ill patient. Ann Pharmacother. 2011, 45: e37-
Lamoth F, Buclin T, Pascual A, Vora S, Bolay S, Decosterd LA, Calandra T, Marchetti O: High cefepime plasma concentrations and neurological toxicity in febrile neutropenic patients with mild impairment of renal function. Antimicrob Agents Chemother. 2010, 54 (10): 4360-4367.
Lonsdale DO, Udy AA, Roberts JA, Lipman J: Antibacterial therapeutic drug monitoring in cerebrospinal fluid: difficulty in achieving adequate drug concentrations. J Neurosurg. 2013, 118 (2): 297-301.
Chapuis TM, Giannoni E, Majcherczyk PA, Chiolero R, Schaller M-D, Berger MM, Bolay S, Decosterd LA, Bugnon D, Moreillon P: Prospective monitoring of cefepime in intensive care unit adult patients. Crit Care. 2010, 14 (2): R51-
Simon N, Dussol B, Sampol E, Purgus R, Brunet P, Lacarelle B, Berland Y, Bruguerolle B, Urien S: Population pharmacokinetics of ceftriaxone and pharmacodynamic considerations in haemodialysed patients. Clin Pharmacokinet. 2006, 45 (5): 493-501.
Seyler L, Cotton F, Taccone FS, De Backer D, Macours P, Vincent J-L, Jacobs F: Recommended beta-lactam regimens are inadequate in septic patients treated with continuous renal replacement therapy. Crit Care. 2011, 15: R137-
Carlier M, Stove V, Roberts JA, Van de Velde E, De Waele JJ, Verstraete AG: Quantification of seven beta-lactam antibiotics and two beta-lactamase inhibitors in human plasma using a validated UPLC-MS/MS method. Int J Antimicrob Agents. 2012, 40 (5): 416-422.
Ohmori T, Suzuki A, Niwa T, Ushikoshi H, Shirai K, Yoshida S, Ogura S, Itoh Y: Simultaneous determination of eight beta-lactam antibiotics in human serum by liquid chromatography–tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2011, 879: 1038-1042.
Mendez AS, Steppe M, Schapoval EE: Validation of HPLC and UV spectrophotometric methods for the determination of meropenem in pharmaceutical dosage form. J Chromatogr B Analyt Technol Biomed Life Sci. 2003, 33: 947-954.
McWhinney B, Wallis SC, Hillister T, Roberts JA, Lipman J, Ungerer J: Analysis of 12 beta-lactam antibiotics in human plasma by HPLC with ultraviolet detection. J Chromatogr B Analyt Technol Biomed Life Sci. 2010, 878: 2036-2043.
Briscoe S, McWhinney B, Lipman J, Roberts JA, Ungerer JP: A method for determining the free (unbound) concentration of ten beta-lactam antibiotics in human plasma using high performance liquid chromatography with ultraviolet detection. J Chromatogr B Analyt Technol Biomed Life Sci. 2012, 907: 178-184.
Wong G, Briscoe S, Adnan S, McWhinney B, Ungerer J, Lipman J, Roberts JA: Protein binding of beta-lactam antibiotics in critically ill patients: can we successfully predict unbound concentrations?. Antimicrob Agents Chemother. 2013, 57 (12): 6165-6170.
Farkas A, Daroczi G: Individually Designed Optimum Dosing Strategies (ID-ODS): A Multi-Model Based Online Application to Individualize Antibiotic Dosing in Critically Ill Patients. Proceedings of NewYork-Presbyterian Healthcare System Quality Symposium. Edited by: Osten WM, Lazar EJ, Regan BK. 2013, New York: The NewYork-Presbyterian, 240-
Barclay ML, Kirkpatrick CM, Begg EJ: Once daily aminoglycoside therapy. Is it less toxic than multiple daily doses and how should it be monitored?. Clin Pharmacokinet. 1999, 36 (2): 89-98.
Nicolau DP, Freeman CD, Belliveau PP, Nightingale CH, Ross JW, Quintiliani R: Experience with a once-daily aminoglycoside program administered to 2,184 adult patients. Antimicrob Agents Chemother. 1995, 39 (3): 650-655.
Bartal C, Danon A, Schlaeffer F, Reisenberg K, Alkan M, Smoliakov R, Sidi A, Almog Y: Pharmacokinetic dosing of aminoglycosides: a controlled trial. Am J Med. 2003, 114 (3): 194-198.
Streetman DS, Nafziger AN, Destache CJ, Bertino AS: Individualized pharmacokinetic monitoring results in less aminoglycoside-associated nephrotoxicity and fewer associated costs. Pharmacotherapy. 2001, 21 (4): 443-451.
Sanchez-Alcaraz A, Vargas A, Quintana MB, Rocher A, Querol JM, Poveda JL, Hermenegildo M: Therapeutic drug monitoring of tobramycin: once-daily versus twice-daily dosage schedules. J Clin Pharm Ther. 1998, 23 (5): 367-373.
Conil JM, Georges B, Ruiz S, Rival T, Seguin T, Cougot P, Fourcade O, Pharmd GH, Saivin S: Tobramycin disposition in ICU patients receiving a once daily regimen: population approach and dosage simulations. Br J Clin Pharmacol. 2011, 71 (1): 61-71.
Taccone FS, Laterre PF, Spapen H, Dugernier T, Delattre I, Layeux B, De Backer D, Wittebole X, Wallemacq P, Vincent JL, Jacobs F: Revisiting the loading dose of amikacin for patients with severe sepsis and septic shock. Crit Care. 2010, 14 (2): R53-
Conil JM, Georges B, Breden A, Segonds C, Lavit M, Seguin T, Coley N, Samii K, Chabanon G, Houin G, Saivin S: Increased amikacin dosage requirements in burn patients receiving a once-daily regimen. Int J Antimicrob Agents. 2006, 28 (3): 226-230.
Bracco D, Landry C, Dubois MJ, Eggimann P: Pharmacokinetic variability of extended interval tobramycin in burn patients. Burns. 2008, 34 (6): 791-796.
Petejova N, Zahalkova J, Duricova J, Kacirova I, Brozmanova H, Urbanek K, Grundmann M, Martinek A: Gentamicin pharmacokinetics during continuous venovenous hemofiltration in critically ill septic patients. J Chemother. 2012, 24 (2): 107-112.
Boyer A, Gruson D, Bouchet S, Clouzeau B, Hoang-Nam B, Vargas F, Gilles H, Molimard M, Rogues AM, Moore N: Aminoglycosides in septic shock: an overview, with specific consideration given to their nephrotoxic risk. Drug Saf. 2013, 36 (4): 217-230.
Mueller EW, Boucher BA: The use of extended-interval aminoglycoside dosing strategies for the treatment of moderate-to-severe infections encountered in critically ill surgical patients. Surg Infect (Larchmt). 2009, 10 (6): 563-570.
Prins JM, Weverling GJ, de Blok K, van Ketel RJ, Speelman P: Validation and nephrotoxicity of a simplified once-daily aminoglycoside dosing schedule and guidelines for monitoring therapy. Antimicrob Agents Chemother. 1996, 40 (11): 2494-2499.
Wallace AW, Jones M, Bertino JS: Evaluation of four once-daily aminoglycoside dosing nomograms. Pharmacotherapy. 2002, 22 (9): 1077-1083.
Botha FJ, van der Bijl P, Seifart HI, Parkin DP: Fluctuation of the volume of distribution of amikacin and its effect on once-daily dosage and clearance in a seriously ill patient. Intensive Care Med. 1996, 22 (5): 443-446.
Begg EJ, Barclay ML, Duffull SB: A suggested approach to once-daily aminoglycoside dosing. Br J Clin Pharmacol. 1995, 39 (6): 605-609.
Fonge H, Kaale E, Govaerts C, Desmet K, Van Schepdael A, Hoogmartens J: Bioanalysis of tobramycin for therapeutic drug monitoring by solid-phase extraction and capillary zone electrophoresis. J Chromatogr B Analyt Technol Biomed Life Sci. 2004, 810 (2): 313-318.
Dasgupta A: Advances in antibiotic measurement. Adv Clin Chem. 2012, 56: 75-104.
Avent ML, Teoh J, Lees J, Eckert KA, Kirkpatrick CM: Comparing 3 methods of monitoring gentamicin concentrations in patients with febrile neutropenia. Ther Drug Monit. 2011, 33 (5): 592-601.
Delattre IK, Musuamba FT, Nyberg J, Taccone FS, Laterre PF, Verbeeck RK, Jacobs F, Wallemacq PE: Population pharmacokinetic modeling and optimal sampling strategy for Bayesian estimation of amikacin exposure in critically ill septic patients. Ther Drug Monit. 2010, 32 (6): 749-756.
Turnidge J: Pharmacodynamics and dosing of aminoglycosides. Infect Dis Clin. 2003, 17 (3): 503-528.
Minejima E, Choi J, Beringer P, Lou M, Tse E, Wong-Beringer A: Applying new diagnostic criteria for acute kidney injury to facilitate early identification of nephrotoxicity in vancomycin-treated patients. Antimicrob Agents Chemother. 2011, 55 (7): 3278-3283.
Prabaker KK, Tran TP, Pratummas T, Goetz MB, Graber CJ: Elevated vancomycin trough is not associated with nephrotoxicity among inpatient veterans. J Hosp Med. 2012, 7 (2): 91-97.
Hidayat LK, Hsu DI, Quist R, Shriner KA, Wong-Beringer A: High-dose vancomycin therapy for methicillin-resistant Staphylococcus aureus infections: efficacy and toxicity. Arch Intern Med. 2006, 166 (19): 2138-2144.
Jeffres MN, Isakow W, Doherty JA, Micek ST, Kollef MH: A retrospective analysis of possible renal toxicity associated with vancomycin in patients with health care-associated methicillin-resistant Staphylococcus aureus pneumonia. Clin Ther. 2007, 29 (6): 1107-1115.
Lodise TP, Lomaestro B, Graves J, Drusano GL: Larger vancomycin doses (at least four grams per day) are associated with an increased incidence of nephrotoxicity. Antimicrob Agents Chemother. 2008, 52 (4): 1330-1336.
Bosso JA, Nappi J, Rudisill C, Wellein M, Bookstaver PB, Swindler J, Mauldin PD: Relationship between vancomycin trough concentrations and nephrotoxicity: a prospective multicenter trial. Antimicrob Agents Chemother. 2011, 55 (12): 5475-5479.
Pritchard L, Baker C, Leggett J, Sehdev P, Brown A, Bayley KB: Increasing vancomycin serum trough concentrations and incidence of nephrotoxicity. Am J Med. 2010, 123 (12): 1143-1149.
Hermsen ED, Hanson M, Sankaranarayanan J, Stoner JA, Florescu MC, Rupp ME: Clinical outcomes and nephrotoxicity associated with vancomycin trough concentrations during treatment of deep-seated infections. Expert Opin Drug Saf. 2010, 9 (1): 9-14.
van Hal SJ, Paterson DL, Lodise TP: Systematic review and meta-analysis of vancomycin-induced nephrotoxicity associated with dosing schedules that maintain troughs between 15 and 20 milligrams per liter. Antimicrob Agents Chemother. 2013, 57 (2): 734-744.
Forouzesh A, Moise PA, Sakoulas G: Vancomycin ototoxicity: a reevaluation in an era of increasing doses. Antimicrob Agents Chemother. 2009, 53 (2): 483-486.
Shields RK, Martello JL, Potoski BA: Is vancomycin ototoxicity a significant risk?. Antimicrob Agents Chemother. 2009, 53 (10): 4572-author reply 4572–4573
Jeffres MN, Isakow W, Doherty JA, McKinnon PS, Ritchie DJ, Micek ST, Kollef MH: Predictors of mortality for methicillin-resistant Staphylococcus aureus health-care-associated pneumonia: specific evaluation of vancomycin pharmacokinetic indices. Chest. 2006, 130 (4): 947-955.
Iwamoto T, Kagawa Y, Kojima M: Clinical efficacy of therapeutic drug monitoring in patients receiving vancomycin. Biol Pharm Bull. 2003, 26 (6): 876-879.
Cheong JY, Makmor-Bakry M, Lau CL, Abdul Rahman R: The relationship between trough concentration of vancomycin and effect on methicillin-resistant Staphylococcus aureus in critically ill patients. S Afr Med J. 2012, 102 (7): 616-619.
Ye ZK, Tang HL, Zhai SD: Benefits of therapeutic drug monitoring of vancomycin: a systematic review and meta-analysis. PLoS One. 2013, 8 (10): e77169-
Sakoulas G, Gold HS, Cohen RA, Venkataraman L, Moellering RC, Eliopoulos GM: Effects of prolonged vancomycin administration on methicillin-resistant Staphylococcus aureus (MRSA) in a patient with recurrent bacteraemia. J Antimicrob Chemother. 2006, 57 (4): 699-704.
Howden BP, Ward PB, Charles PG, Korman TM, Fuller A, du Cros P, Grabsch EA, Roberts SA, Robson J, Read K, Bak N, Hurley J, Johnson PD, Morris AJ, Mayall BC, Grayson ML: Treatment outcomes for serious infections caused by methicillin-resistant Staphylococcus aureus with reduced vancomycin susceptibility. Clin Infect Dis. 2004, 38 (4): 521-528.
Moellering RC: Monitoring serum vancomycin levels: climbing the mountain because it is there?. Clin Infect Dis. 1994, 18 (4): 544-546.
Rybak M, Lomaestro B, Rotschafer JC, Moellering R, Craig W, Billeter M, Dalovisio JR, Levine DP: Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2009, 66 (1): 82-98.
Potoski BA, Paterson DL: Appropriate pharmacokinetic index for outcome in Staphylococcus aureus pneumonia. Chest. 2007, 132 (3): 1101-1102. author reply 1102–1103
Morrison AP, Melanson SE, Carty MG, Bates DW, Szumita PM, Tanasijevic MJ: What proportion of vancomycin trough levels are drawn too early? Frequency and impact on clinical actions. Am J Clin Pathol. 2012, 137 (3): 472-478.
Takahashi Y, Takesue Y, Takubo S, Ishihara M, Nakajima K, Tsuchida T, Ikeuchi H, Uchino M: Preferable timing of therapeutic drug monitoring in patients with impaired renal function treated with once-daily administration of vancomycin. J Infect Chemother. 2013, 19 (4): 709-716.
Tobin CM, Darville JM, Thomson AH, Sweeney G, Wilson JF, MacGowan AP, White LO: Vancomycin therapeutic drug monitoring: is there a consensus view? The results of a UK National External Quality Assessment Scheme (UK NEQAS) for antibiotic assays questionnaire. J Antimicrob Chemother. 2002, 50 (5): 713-718.
Matsumoto K, Takesue Y, Ohmagari N, Mochizuki T, Mikamo H, Seki M, Takakura S, Tokimatsu I, Takahashi Y, Kasahara K, Okada K, Igarashi M, Kobayashi M, Hamada Y, Kimura M, Nishi Y, Tanigawara Y, Kimura T: Practice guidelines for therapeutic drug monitoring of vancomycin: a consensus review of the Japanese Society of Chemotherapy and the Japanese Society of Therapeutic Drug Monitoring. J Infect Chemother. 2013, 19 (3): 365-380.
Wilson JF, Davis AC, Tobin CM: Evaluation of commercial assays for vancomycin and aminoglycosides in serum: a comparison of accuracy and precision based on external quality assessment. J Antimicrob Chemother. 2003, 52 (1): 78-82.
Murphy JE, Gillespie DE, Bateman CV: Predictability of vancomycin trough concentrations using seven approaches for estimating pharmacokinetic parameters. Am J Health Syst Pharm. 2006, 63 (23): 2365-2370.
DeRyke CA, Alexander DP: Optimizing vancomycin dosing through pharmacodynamic assessment targeting area under the concentration-time curve/minimum inhibitory concentration. Hosp Pharm. 2009, 44 (9): 751-765.
Pea F, Bertolissi M, Di Silvestre A, Poz D, Giordano F, Furlanut M: TDM coupled with Bayesian forecasting should be considered an invaluable tool for optimizing vancomycin daily exposure in unstable critically ill patients. Int J Antimicrob Agents. 2002, 20 (5): 326-332.
Avent ML, Vaska VL, Rogers BA, Cheng AC, van Hal SJ, Holmes NE, Howden BP, Paterson DL: Vancomycin therapeutics and monitoring: a contemporary approach. Intern Med J. 2013, 43 (2): 110-119.
Man SS, Carr RR, Ensom MH: Comparison of continuous and intermittent IV infusion of vancomycin: systematic review. Can J Hosp Pharm. 2010, 63 (5): 373-381.
James JK, Palmer SM, Levine DP, Rybak MJ: Comparison of conventional dosing versus continuous-infusion vancomycin therapy for patients with suspected or documented gram-positive infections. Antimicrob Agents Chemother. 1996, 40 (3): 696-700.
Wysocki M, Delatour F, Faurisson F, Rauss A, Pean Y, Misset B, Thomas F, Timsit JF, Similowski T, Mentec H, Mier L, Dreyfuss D: Continuous versus intermittent infusion of vancomycin in severe Staphylococcal infections: prospective multicenter randomized study. Antimicrob Agents Chemother. 2001, 45 (9): 2460-2467.
DiMondi VP, Rafferty K: Review of continuous-infusion vancomycin. Ann Pharmacother. 2013, 47 (2): 219-227.
Panday PN, Sturkenboom M: Continuous infusion of vancomycin less effective and safe than intermittent infusion, based on pharmacodynamic and pharmacokinetic principles. Clin Infect Dis. 2009, 49 (12): 1964-1965. author reply 1965
Jeurissen A, Sluyts I, Rutsaert R: A higher dose of vancomycin in continuous infusion is needed in critically ill patients. Int J Antimicrob Agents. 2011, 37 (1): 75-77.
De Waele JJ, Danneels I, Depuydt P, Decruyenaere J, Bourgeois M, Hoste E: Factors associated with inadequate early vancomycin levels in critically ill patients treated with continuous infusion. Int J Antimicrob Agents. 2013, 41 (5): 434-438.
Saugel B, Nowack MC, Hapfelmeier A, Umgelter A, Schultheiss C, Thies P, Phillip V, Eyer F, Schmid RM, Huber W: Continuous intravenous administration of vancomycin in medical intensive care unit patients. J Crit Care. 2013, 28 (1): 9-13.
Ampe E, Delaere B, Hecq JD, Tulkens PM, Glupczynski Y: Implementation of a protocol for administration of vancomycin by continuous infusion: pharmacokinetic, pharmacodynamic and toxicological aspects. Int J Antimicrob Agents. 2013, 41 (5): 439-446.
Cataldo MA, Tacconelli E, Grilli E, Pea F, Petrosillo N: Continuous versus intermittent infusion of vancomycin for the treatment of Gram-positive infections: systematic review and meta-analysis. J Antimicrob Chemother. 2012, 67 (1): 17-24.
Stalker DJ, Jungbluth GL: Clinical pharmacokinetics of linezolid, a novel oxazolidinone antibacterial. Clin Pharmacokinet. 2003, 42 (13): 1129-1140.
Tsuji Y, Hiraki Y, Mizoguchi A, Hayashi W, Kamohara R, Kamimura H, Karube Y: Pharmacokinetics of repeated dosing of linezolid in a hemodialysis patient with chronic renal failure. J Infect Chemother. 2008, 14 (2): 156-160.
Tsuji Y, Hiraki Y, Matsumoto K, Mizoguchi A, Kobayashi T, Sadoh S, Morita K, Kamimura H, Karube Y: Thrombocytopenia and anemia caused by a persistent high linezolid concentration in patients with renal dysfunction. J Infect Chemother. 2011, 17 (1): 70-75.
Matsumoto K, Takeshita A, Ikawa K, Shigemi A, Yaji K, Shimodozono Y, Morikawa N, Takeda Y, Yamada K: Higher linezolid exposure and higher frequency of thrombocytopenia in patients with renal dysfunction. Int J Antimicrob Agents. 2010, 36 (2): 179-181.
Nukui Y, Hatakeyama S, Okamoto K, Yamamoto T, Hisaka A, Suzuki H, Yata N, Yotsuyanagi H, Moriya K: High plasma linezolid concentration and impaired renal function affect development of linezolid-induced thrombocytopenia. J Antimicrob Chemother. 2013, 68 (9): 2128-2133.
Sousa R, Lopez R, Martinez-Pastor JC, Cervera C, Bori G, Garcia-Ramiro S, Mensa J, Soriano A: Usefulness of monitoring linezolid trough serum concentration in prolonged treatments. Rev Esp Quimioter. 2011, 24 (3): 151-153.
Pea F, Furlanut M, Cojutti P, Cristini F, Zamparini E, Franceschi L, Viale P: Therapeutic drug monitoring of linezolid: a retrospective monocentric analysis. Antimicrob Agents Chemother. 2010, 54 (11): 4605-4610.
Hallam MJ, Allen JM, James SE, Donaldson PM, Davies JG, Hanlon GW, Dheansa BS: Potential subtherapeutic linezolid and meropenem antibiotic concentrations in a patient with severe burns and sepsis. J Burn Care Res. 2010, 31 (1): 207-209.
Lovering AM, Le Floch R, Hovsepian L, Stephanazzi J, Bret P, Birraux G, Vinsonneau C: Pharmacokinetic evaluation of linezolid in patients with major thermal injuries. J Antimicrob Chemother. 2009, 63 (3): 553-559.
Pea F, Scudeller L, Lugano M, Baccarani U, Pavan F, Tavio M, Furlanut M, Rocca GD, Bresadola F, Viale P: Hyperlactacidemia potentially due to linezolid overexposure in a liver transplant recipient. Clin Infect Dis. 2006, 42 (3): 434-435.
Pea F, Viale P, Lugano M, Pavan F, Scudeller L, Della Rocca G, Furlanut M: Linezolid disposition after standard dosages in critically ill patients undergoing continuous venovenous hemofiltration: a report of 2 cases. Am J Kidney Dis. 2004, 44 (6): 1097-1102.
Pea F, Cojutti P, Pagotto A, Cristini F, Furlanut M, Viale P: Successful long-term treatment of cerebral nocardiosis with unexpectedly low doses of linezolid in an immunocompromised patient receiving complex polytherapy. Antimicrob Agents Chemother. 2012, 56 (6): 3438-3440.
Polillo M, Tascini C, Lastella M, Malacarne P, Ciofi L, Viaggi B, Bocci G, Menichetti F, Danesi R, Del Tacca M, Di Paolo A: A rapid high-performance liquid chromatography method to measure linezolid and daptomycin concentrations in human plasma. Ther Drug Monit. 2010, 32 (2): 200-205.
Alffenaar JW, Kosterink JG, van Altena R, van der Werf TS, Uges DR, Proost JH: Limited sampling strategies for therapeutic drug monitoring of linezolid in patients with multidrug-resistant tuberculosis. Ther Drug Monit. 2010, 32 (1): 97-101.
Cattaneo D, Baldelli S, Conti F, Cozzi V, Clementi E: Determination of linezolid in human plasma by high-performance liquid chromatography with ultraviolet detection. Ther Drug Monit. 2010, 32 (4): 520-524.
Baietto L, D’Avolio A, Ariaudo A, Corcione S, Simiele M, Cusato J, Urbino R, Di Perri G, Ranieri VM, De Rosa FG: Development and validation of a new UPLC-PDA method to quantify linezolid in plasma and in dried plasma spots. J Chromatogr B Analyt Technol Biomed Life Sci. 2013, 936: 42-47.
Vu DH, Bolhuis MS, Koster RA, Greijdanus B, de Lange WC, van Altena R, Brouwers JR, Uges DR, Alffenaar JW: Dried blood spot analysis for therapeutic drug monitoring of linezolid in patients with multidrug-resistant tuberculosis. Antimicrob Agents Chemother. 2012, 56 (11): 5758-5763.
Bolhuis MS, van Altena R, van Hateren K, de Lange WC, Greijdanus B, Uges DR, Kosterink JG, van der Werf TS, Alffenaar JW: Clinical validation of the analysis of linezolid and clarithromycin in oral fluid of patients with multidrug-resistant tuberculosis. Antimicrob Agents Chemother. 2013, 57 (8): 3676-3680.
Kontou P, Chatzika K, Pitsiou G, Stanopoulos I, Argyropoulou-Pataka P, Kioumis I: Pharmacokinetics of ciprofloxacin and its penetration into bronchial secretions of mechanically ventilated patients with chronic obstructive pulmonary disease. Antimicrob Agents Chemother. 2011, 55 (9): 4149-4153.
Fish DN, Piscitelli SC, Danziger LH: Development of resistance during antimicrobial therapy: a review of antibiotic classes and patient characteristics in 173 studies. Pharmacotherapy. 1995, 15 (3): 279-291.
Gasser TC, Ebert SC, Graversen PH, Madsen PO: Ciprofloxacin pharmacokinetics in patients with normal and impaired renal function. Antimicrob Agents Chemother. 1987, 31 (5): 709-712.
Pea F, Poz D, Viale P, Pavan F, Furlanut M: Which reliable pharmacodynamic breakpoint should be advised for ciprofloxacin monotherapy in the hospital setting? A TDM-based retrospective perspective. J Antimicrob Chemother. 2006, 58 (2): 380-386.
Jones EM, McMullin CM, Hedges AJ, Lovering AM, White LO, Reeves DS, MacGowan AP: The pharmacokinetics of intravenous ciprofloxacin 400 mg 12 hourly in patients with severe sepsis: the effect of renal function and intra-abdominal disease. J Antimicrob Chemother. 1997, 40 (1): 121-124.
Gous A, Lipman J, Scribante J, Tshukutsoane S, Hon H, Pinder M, Mathivha R, Verhoef L, Stass H: Fluid shifts have no influence on ciprofloxacin pharmacokinetics in intensive care patients with intra-abdominal sepsis. Int J Antimicrob Agents. 2005, 26 (1): 50-55.
Fish DN, Bainbridge JL, Peloquin CA: Variable disposition of ciprofloxacin in critically ill patients undergoing continuous arteriovenous hemodiafiltration. Pharmacotherapy. 1995, 15 (2): 236-245.
Roberts DM, Roberts JA, Roberts MS, Liu X, Nair P, Cole L, Lipman J, Bellomo R, RENAL Replacement Therapy Study Investigators: Variability of antibiotic concentrations in critically ill patients receiving continuous renal replacement therapy: a multicentre pharmacokinetic study. Crit Care Med. 2012, 40 (5): 1523-1528.
van Geijlswijk IM, van Zanten AR, van der Meer YG: Reliable new high-performance liquid chromatographic method for the determination of ciprofloxacin in human serum. Ther Drug Monit. 2006, 28 (2): 278-281.
Sousa J, Alves G, Campos G, Fortuna A, Falcao A: First liquid chromatography method for the simultaneous determination of levofloxacin, pazufloxacin, gatifloxacin, moxifloxacin and trovafloxacin in human plasma. J Chromatogr B Analyt Technol Biomed Life Sci. 2013, 930: 104-111.
Al-Ghazawi M, AbuRuz S: Determination of ciprofloxacin in dried blood spots for therapeutic drug monitoring. Chromatographia. 2010, 71 (11/12): 999-1005.
Sun HW, He P, Lv YK, Liang SX: Effective separation and simultaneous determination of seven fluoroquinolones by capillary electrophoresis with diode-array detector. J Chromatogr B Analyt Technol Biomed Life Sci. 2007, 852 (1–2): 145-151.
Zeng H-J, Yang R, Liu B, Lei L-F, Li J-J, Qu L-B: Simple and sensitive determination of sparfloxacin in pharmaceuticals and biological samples by immunoassay. J Pharmaceutical Analysis. 2012, 2 (3): 214-219.
Wenisch JM, Meyer B, Fuhrmann V, Saria K, Zuba C, Dittrich P, Thalhammer F: Multiple-dose pharmacokinetics of daptomycin during continuous venovenous haemodiafiltration. J Antimicrob Chemother. 2012, 67 (4): 977-983.
Falcone M, Russo A, Venditti M, Novelli A, Pai MP: Considerations for higher doses of daptomycin in critically ill patients with methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2013, 57 (11): 1568-1576.
Pea F, Crapis M, Cojutti P, Bassetti M: Daptomycin underexposure in a young intravenous drug user who was affected by life-threatening Staphylococcus aureus-complicated skin and soft tissue infection associated with bacteraemia. Infection. 2014, 42 (1): 207-210.
Bhavnani SM, Rubino CM, Ambrose PG, Drusano GL: Daptomycin exposure and the probability of elevations in the creatine phosphokinase level: data from a randomized trial of patients with bacteremia and endocarditis. Clin Infect Dis. 2010, 50 (12): 1568-1574.
Falcone M, Russo A, Cassetta MI, Lappa A, Tritapepe L, d’Ettorre G, Fallani S, Novelli A, Venditti M: Variability of pharmacokinetic parameters in patients receiving different dosages of daptomycin: is therapeutic drug monitoring necessary?. J Infect Chemother. 2013, 19 (4): 732-739.
Safdar N, Andes D, Craig WA: In vivo pharmacodynamic activity of daptomycin. Antimicrob Agents Chemother. 2004, 48 (1): 63-68.
Bazoti FN, Gikas E, Skoutelis A, Tsarbopoulos A: Development and validation of an ultra performance liquid chromatography-tandem mass spectrometry method for the quantification of daptomycin in human plasma. J Pharm Biomed Anal. 2011, 56 (1): 78-85.
Craig WA: Interrelationship between pharmacokinetics and pharmacodynamics in determining dosage regimens for broad-spectrum cephalosporins. Diagn Microbiol Infect Dis. 1995, 22 (1–2): 89-96.
Li C, Du X, Kuti JL, Nicolau DP: Clinical pharmacodynamics of meropenem in patients with lower respiratory tract infections. Antimicrob Agents Chemother. 2007, 51 (5): 1725-1730.
Rayner CR, Forrest A, Meagher AK, Birmingham MC, Schentag JJ: Clinical pharmacodynamics of linezolid in seriously ill patients treated in a compassionate use programme. Clinical Pharmacokinet. 2003, 42 (15): 1411-1423.
Cattaneo D, Orlando G, Cozzi V, Cordier L, Baldelli S, Merli S, Fucile S, Gulisano C, Rizzardini G, Clementi E: Linezolid plasma concentrations and occurrence of drug-related haematological toxicity in patients with gram-positive infections. Int J Antimicrob Agents. 2013, 41 (6): 586-589.
Pea F, Viale P, Cojutti P, Del Pin B, Zamparini E, Furlanut M: Therapeutic drug monitoring may improve safety outcomes of long-term treatment with linezolid in adult patients. J Antimicrob Chemother. 2012, 67 (8): 2034-2042.
Schentag JJ: Antimicrobial action and pharmacokinetics/pharmacodynamics: the use of AUIC to improve efficacy and avoid resistance. J Chemother. 1999, 11 (6): 426-439.
Zelenitsky SA, Ariano RE: Support for higher ciprofloxacin AUC 24/MIC targets in treating Enterobacteriaceae bloodstream infection. J Antimicrob Chemother. 2010, 65 (8): 1725-1732.
Scaglione F: Can PK/PD be used in everyday clinical practice. Int J Antimicrob Agents. 2002, 19 (4): 349-353.
Rodvold KA, Neuhauser M: Pharmacokinetics and pharmacodynamics of fluoroquinolones. Pharmacotherapy. 2001, 21 (10 Pt 2): 233S-252S.
Moore RD, Lietman PS, Smith CR: Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis. 1987, 155 (1): 93-99.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/14/288/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GW and FS are proposed to be joint first authors and contributed equally to the drafting of the manuscript. All authors read and approved the final manuscript.
Gloria Wong, Fekade Bruck Sime contributed equally to this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wong, G., Sime, F.B., Lipman, J. et al. How do we use therapeutic drug monitoring to improve outcomes from severe infections in critically ill patients?. BMC Infect Dis 14, 288 (2014). https://doi.org/10.1186/1471-2334-14-288
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-14-288