Abstract
Background
The International Society on Thrombosis and Haemostasis (ISTH) released overt disseminated intravascular coagulation (DIC) diagnostic criteria in 2001. Since then, DIC has been understood as the end-stage consumptive coagulopathy and not the therapeutic target. However, DIC is not merely a decompensated coagulation disorder, but also includes early stages with systemic activation in coagulation. Thus, the ISTH has recently released sepsis-induced coagulopathy (SIC) criteria that can diagnose compensated-phase of coagulopathy with readily available biomarkers.
Main body
DIC is a laboratory-based diagnosis due to various critical conditions, although sepsis is the most common underlying disease. The pathophysiology of sepsis-associated DIC is multifactorial, and in addition to coagulation activation with suppressed fibrinolysis, multiple inflammatory responses are initiated by activated leukocytes, platelets, and vascular endothelial cells as part of thromboinflammation. Although overt DIC diagnostic criteria were established by ISTH to diagnose the advanced stage of DIC, additional criteria that can detect an earlier stage of DIC were needed for potential therapeutic considerations. Accordingly, the ISTH introduced SIC criteria in 2019 that are easy to use and require only platelet count, prothrombin time-international normalized ratio, and Sequential Organ Failure Assessment Score. SIC score can be used to evaluate disease severity and determine the timing of potential therapeutic interventions. One of the major disadvantages in treating sepsis-associated DIC is the lack of availability of specific therapeutic approaches beyond treating the underlying infection. Clinical trials to date have failed because included patients who were not coagulopathic. Nevertheless, in addition to infection control, anticoagulant therapy will be the choice for sepsis-associated DIC. Therefore, the efficacy of heparin, antithrombin, and recombinant thrombomodulin has to be proven in future clinical studies.
Conclusion
It is necessary to develop a novel therapeutic strategy against sepsis-associated DIC and improve the outcomes. Consequently, we recommend screening and monitoring DIC using SIC scoring system.
Similar content being viewed by others
Introduction
Hemostasis, a fundamental host defense mechanism against various pathophysiologic insults, clinically presents as macro- and microthrombosis in acute injury and critically ill patients. Although the hemostatic response is beneficial in some conditions, excess thromboinflammation also induces tissue malcirculation and causes subsequent organ dysfunction [1]. Systemic hypercoagulation with or without consumptive coagulopathy frequently occurs following major tissue injury, and based on laboratory-based disseminated intravascular coagulation (DIC) diagnostic criteria, patients are clinically diagnosed as having DIC [2]. The pathophysiology, phenotypic expression, and treatments of DIC vary considerably based on the underlying causative diseases [3, 4]. However, sepsis is the most frequent and life-threatening cause of DIC and commonly presents as a thrombotic type DIC [5, 6]. This type of DIC is often complicated by organ dysfunction, with hemorrhagic events occurring less commonly [7]. Coagulation status changes dynamically based on the progression of the underlying disease. Sepsis-associated DIC is a dynamic condition that starts from coagulation disorder, can advance to sepsis-induced coagulopathy (SIC), and finally to decompensated coagulation disorder (overt DIC) (Fig. 1). Anticoagulation is expected for the compensated DIC, and the decompensated stage may require additional therapeutic modalities with supplementation therapy [8, 9]. Recent advances in sepsis-associated DIC management include the development of early diagnostic criteria based on readily available clinical information and the administration of potentially effective anticoagulants [4, 10]. This review will focus on advances in sepsis-associated DIC diagnosis, management, and future perspectives.
The initiation and progression of thromboinflammation in sepsis. The inflammation and host responses to infection induce coagulation disorder in sepsis. Although coagulation disorder is a part of host defense, excess coagulation disorder can be harmful to the host. Disseminated intravascular coagulation (DIC) is a systemic coagulation disorder that can cause the disturbance of tissue malcirculation and subsequent organ dysfunction. Sepsis-induced coagulopathy (SIC) is an early phase of DIC and a potential target of anticoagulant therapy. The advanced stage of DIC is defined as overt DIC and potentially the target of supplementation therapy
Pathophysiology of sepsis-associated DIC
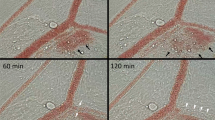
Monocytes/macrophages are the first-line responders to the invaded pathogens and phagocyte pathogens that detect bacteria by sensing specific molecular patterns and elicit proinflammatory and procoagulant reactions to entrap and localize them [11]. As pattern-recognizing receptors, monocytes/macrophages express Toll-like receptors (TLRs), Fcγ-receptors, and G-protein-coupled receptors that detect the pathogen-associated molecular patterns (PAMPs), subsequently integrating the innate immune system as well as the coagulation system [12]. TLRs not only react to PAMPs, but also transduce the binding signals of host-derived stress molecules, namely damage-associated molecular patterns (DAMPs), thereby initiating a vicious cycle of inflammation and coagulation [13]. After the subsequent multi-step signal transduction, monocytes/macrophages produce proinflammatory cytokines and chemokines that activate neutrophils and upregulate the expression of tissue factor (TF) and phosphatidylserine (PS) on the cellar membrane [14]. TF and PS initiate extrinsic and intrinsic coagulation cascades and facilitate prothrombotic reactions. Activated neutrophils kill pathogens by using proteases, reactive oxygen species, releasing neutrophil extracellular traps (NETs), and further propagating inflammation by cell death mechanisms [15]. Pyroptosis, necroptosis, NETosis, and necrosis are the representative cell death styles that increase inflammation and coagulation by releasing DAMPs and other cytotoxic substances [16]. Platelets also participate in the host defense by developing thrombus formation via expressing adhesion molecules, releasing granule components such as platelet factor 4 (PF4), von Willebrand factor (VWF) [17], and procoagulant microvesicles [18]. These responses lead to intravascular microthrombus formation (immunothrombosis) to protect the host against infection (Fig. 2). Among the coagulation factors, thrombin is a critical mediator that regulates inflammation and coagulation [19]. Monocyte, neutrophil, platelet, and endothelial cells also express protease-activated receptor-1 (PAR-1), and thrombin upregulates proinflammatory and procoagulant reactions by binding to PAR-1 [19, 20]. Following sepsis-induced acute inflammatory responses, vascular endothelial cells lose their antithrombotic properties by factors that include decreased nitric oxide/prostaglandin I2 production, and disruption of the glycocalyx. Thrombomodulin is proteolytically cleaved and released from the endothelial surface. In addition, the production of plasminogen activator inhibitor 1 (PAI-1) is upregulated, and fibrinolytic suppression becomes evident. This suppression in fibrinolysis is the critical feature of coagulation disorder in sepsis (fibrinolytic shutdown). Damaged endothelial cells release thrombogenic molecules, including VWF and adhesion molecules, and stimulate platelet adhesion and aggregation [21]. Furthermore, physiological anticoagulant factors such as antithrombin and protein C are extravasated with increased vascular permeability [22]. These events facilitate widespread microthrombus formation during sepsis (Fig. 3).
Microthrombosis in the microcirculation in sepsis model of rat. Rat mesenteric microcirculation was observed under the intravital microscope after lipopolysaccharide injection. Round stiff leukocytes adhered to the unsmooth and swelled endothelial cells. Some leukocytes transmigrated to the extravascular space. Aggregated platelets stick to the leukocytes and endothelium and form leukocyte–platelet aggregation. Along with these changes, the blood flow gradually decreased
Pathophysiology of sepsis-associated coagulation disorder. Monocytes, neutrophils, and platelets express various receptors such as Toll-like receptors (TLRs), Fcγ receptor (FcγR), and protease-activated receptor (PAR)-1, and induce inflammatory and procoagulant responses in these cells. Activated monocytes express tissue factor (TF) and phosphatidylserine (PS) on the surface, which initiate coagulation cascades. At the same time, monocytes release proinflammatory cytokines and stimulate neutrophils. Activated neutrophils release damage-associated molecular patterns (DAMPs) after cell death, and expel extracellular traps (NETs) that facilitate inflammation through binding to TLRs. Platelets release procoagulant microvesicles and prothrombotic substances such as von Willebrand factor (VWF) and platelet factor 4 (PF4). VWF helps platelet aggregation, and PF4 neutralizes heparan sulfate of the glycocalyx. Vascular endothelial cells lose anti-thrombogenicity by decreasing the production of nitric oxide (NO) and prostaglandin I2 (PG I2), and by increasing the production of plasminogen activator inhibitor 1 (PAI-1). Thrombomodulin which converts protein C (PC) to its activated form activated protein C (APC) is released from endothelial cells, and antithrombin is extravasated with increased vascular permeability. LPS lipopolysaccharide, Ig G immunoglobulin G, GP glycoprotein
Diagnosis of sepsis-associated DIC
DIC is defined as the systemic activation of coagulation and not the consumptive coagulopathy [23], but many physicians consider DIC as a decompensated coagulation disorder, potentially due to the 2001 definition of overt DIC criteria by the International Society on Thrombosis and Haemostasis (ISTH) that is defined as thrombocytopenia, significant prolongation of prothrombin time (PT), moderate or strong increase of fibrin related markers, and/or decreased fibrinogen level. It has not been well-known, but the ISTH has also defined non-overt DIC diagnostic criteria determined by sensitive and specific molecular markers that include antithrombin, protein C, or thrombin–antithrombin (TAT) complexes [23]. However, many patients developed overt DIC independently of non-overt DIC. In addition, since the molecular markers were not commonly used clinically, they were not suitable to use for diagnosing non-overt DIC.
Despite the presence of these classical definitions and criteria, the establishment of new DIC diagnostic criteria was demanded to identify the potential therapeutic target. Consequently, the Japanese Society for Acute Medicine (JAAM) released its compensated DIC criteria by using readily available laboratory tests and clinical data in 2006 [24]. However, after the update of the sepsis definition to Sepsis-3 [25, 26], the JAAM DIC criteria became outdated because the JAAM DIC criteria included the systemic inflammatory response syndrome (SIRS) score. SIC criteria were then introduced in 2017 to diagnose the early onset DIC in sepsis [27]. SIC criteria are defined by the presence of sepsis (infection with organ failure [increased Sequential Organ Failure Assessment (SOFA) score]) and coagulation disorder (decreased platelet count and prolonged PT-international normalized ratio [INR]) [27] (Table 1). The measurement of the platelet count and PT-INR are routine clinical tests, and the SOFA score is an easily calculated clinical score used to evaluate the severity of sepsis [28]. Screening for DIC in septic patients is important based on a large Japanese study reporting efficacy of anticoagulant therapy for coagulopathic septic patients with a high risk of death [29]. After additional clinical reports [30, 31], SIC diagnostic criteria were approved by ISTH DIC Scientific Standardization Committee (SSC) [32, 33]. The clinically relevant importance of the SIC criteria is its simplicity and ability to facilitate the timing of anticoagulant therapy [34]. The JAAM DIC criteria are used popularly for the diagnosis of sepsis-associated DIC in Japan. To mention the superiority of SIC scoring over JAAM DIC scoring, we have to show a better treatment effect based on the SIC diagnosis than that based on the JAAM DIC diagnosis. However, such a study has not been done yet. But, SIC criteria are simpler than JAAM DIC criteria, less costly, and therefore, more suitable for monitoring. In addition, SIC has been shown to directly continue to overt DIC with disease progression.
SIC criteria were specifically designed for sepsis-associated DIC. Likewise, establishing underlying disease-specific considerations may allow us to develop simple and better criteria; we think this approach should be expanded to other areas of DIC, i.e., hematologic DIC and cancer-induced DIC.
The prevalence and mortality of sepsis-associated DIC
In sepsis, the prevalence of DIC varies depending on the target cohorts and diagnostic criteria, but the mortality is always higher in DIC patients compared to non-DIC patients. Gando et al. [35] examined the incidence and the mortality of overt DIC and JAAM DIC in septic patients (Sepsis-1) and reported that they were 18.1% vs. 46.8%, and 38.1% vs. 38.4%, respectively. Another retrospective cohort study examined the prevalence and the mortality of overt DIC, JAAM DIC, and SIC in 1892 patients with sepsis (Sepsis-1) and reported that they were 29.3% and 38.4%, 61.4% and 33.9%, and 60.8% and 32.5%, respectively [36]. Data from a Sepsis-3 cohort of 296 subjects reported the prevalence of overt DIC, modified-JAAM DIC (SIRS score was replaced with antithrombin activity), and SIC were 22.6%, 43.2%, and 56.1%, and 28-day mortalities were 55.2%, 47.7%, and 44.0%, respectively [37]. These data suggest that the prevalence of DIC differs based on definitions, but the mortality of sepsis-associated DIC exceeded 30% regardless of the diagnostic criteria. The primary objective of diagnosing DIC is not to predict outcomes but to decide the timing of initiating intervention because DIC patients have higher mortality compared to non-DIC patients [38]. Of note, recent studies support the idea that anticoagulant therapy is more effective for patients with coagulopathy/DIC and high disease severity [38, 39]. Further, the JAAM DIC and SIC scores reflect disease severity, and the relationship between the scores and mortality was reported [24, 27]. Lu et al. [40] evaluated performance of SIC scoring in 9432 sepsis patients and reported that 28-day mortality was 34% in SIC patients compared to 25% in non-SIC patients. They also reported that the presence of SIC was an independent risk factor for 28-day mortality with an adjusted odds ratio of 1.52 (95% confidence interval [CI]: 1.39 to 1.67).
The performance of SIC scoring system
The usefulness of diagnostic criteria has been examined by evaluating their performance to discriminate the patients with a high risk of death. Wang et al. [37] compared the performance of various DIC diagnostic criteria including SIC, modified-JAAM DIC, simplified Japanese Society on Thrombosis and Hemostasis DIC, and overt DIC criteria in predicting 28-day mortality and reported that the area under the curves (AUC) did not differ among the diagnostic criteria (AUC: between 0.730 and 0.763); nevertheless, it is impactful that SIC is the simplest criterion among them and the odds ratio to death was highest and 5.218 (95% CI: 2.878 to 9.459, P < 0.001). As a screening test like SIC scoring, the expected performance is the capability to deny death when SIC is negative. In this sense, the negative predictive value for 28-day mortality was also highest in SIC and 86.9%. Similar results were confirmed in multiple studies, and the SIC score was reported to be associated with the severity of diseases [40,41,42,43,44,45,46,47,48,49].
The primary objective of diagnosing DIC was not to identify septic patients with a high risk of death but to identify patients who may benefit from anticoagulant therapy. Zou et al. [47] evaluated 6646 septic patients retrospectively and reported the association between heparin administration and lower mortality only in patients with SIC (hazard ratio [HR]: 0.74, 95% CI: 0.65 to 0.85). In contrast, the association was not observed in patients without SIC (HR: 0.95, 95% CI: 0.64 to 1.40). Peng et al. [48] also examined the effect of heparin on septic patients in their retrospective study and concluded that patients with SIC could be good candidates for heparin therapy. In their study, most of the overt DIC patients were diagnosed with SIC, and most overt DIC patients had received a prior diagnosis of SIC [30]. Therefore, SIC precedes overt DIC, and patients progress from SIC to overt DIC with disease progression.
One limitation of SIC criteria is the risk of misdiagnosing diseases that mimic DIC, which may not be small as only two coagulation biomarkers are included. For example, it is not easy to differentiate the thrombotic microangiopathic (TMA) disorders such as thrombotic thrombocytopenic purpura (TTP) [49] and atypical hemolytic uremic syndrome (aHUS) [50], and heparin-induced thrombocytopenia (HIT) from SIC [51]. To support the accurate diagnosis, the ISTH DIC SSC provides a flow chart that aids with systematic differential diagnosis [52]. Although the prolongation of PT-INR is mild, TMA disorders commonly have significant thrombocytopenia and achieve sufficient scores. The decrease in platelet count is more prominent, and the changes in PT are milder in TTP, aHUS, and HIT, and the balance of platelet count and PT can be useful for differentiation. In addition, antithrombin activity, a biomarker of endothelial damage, is significantly decreased in SIC and DIC [53, 54], but it is usually maintained in the TMA and can be helpful for discrimination [55, 56]. Antithrombin level is known to decrease in the early phase of DIC. Jackson Chornenki et al. [57] reported that platelet count and PT-INR in combination with antithrombin activity could identify early-phase DIC in septic patients. Although the incidences are not high, the differential diagnosis of these DIC-mimicking diseases is critical because the mortality is considerably high if treated inappropriately.
How should we treat sepsis-associated DIC?
The treatment of underlying disease is essential in DIC, but for sepsis-associated DIC, additional treatment for ongoing tissue poor perfusion is critical in clinical management. However, little evidence supports the efficacy of anticoagulant therapy in addition to antibiotics and source control. Despite studies of several anticoagulants in large-scale randomized controlled trials (RCTs), no current anticoagulant has yet demonstrated efficacy [61, 63]. Potential reasons include the variability of clinical presentation in sepsis [61], but as previously described, anticoagulant therapy should be considered only for patients with a coagulation disorder, as best noted the optimal target is sepsis-associated DIC with high disease severity [38, 39] (Fig. 4).
The therapeutic target of anticoagulant. The most popular anticoagulants worldwide are heparins, meanwhile, antithrombin and recombinant thrombomodulin are popularly used for disseminated intravascular coagulation (DIC) in Japan. For more than a decade, it has been reported that anticoagulant therapy is effective only for patients with coagulation disorder, and recent studies have shown that sepsis-associated DIC with high disease severity is the optimal target
Heparin
Heparin is commonly used in septic patients for multiple reasons. However, no large randomized controlled study has examined heparin alone for sepsis-associated DIC. A recent meta-analysis reported that unfractionated heparin could reduce the mortality of sepsis, especially in patients with high severity [62]. However, the study population was not restricted to patients with coagulopathy/DIC. Another systematic review of heparin in DIC [63] was limited by including studies in which three out of eight studies used heparin as the control. Although heparin is strongly recommended for COVID-19 [64], its efficacy for sepsis-associated DIC is still unclear. A Japanese RCT compared the efficacy and safety of recombinant thrombomodulin to heparin in DIC-associated with hematologic malignancy or infection. In subgroup analysis, 80 patients with sepsis-associated DIC were subjected to the analyses. The results showed DIC resolution rates in recombinant thrombomodulin group and heparin group were 67.5% and 55.6%, and 28-day mortality rates were 21.4% and 31.6%, respectively [65].
Recombinant thrombomodulin
Recombinant thrombomodulin was developed and approved for clinical use in Japan in 2008 for the treatment of DIC [66]. As described before, Aikawa et al. [65] performed a subgroup analysis on 80 sepsis-associated DIC patients from a Phase 3 trial [67] and reported better performance of recombinant thrombomodulin. The subsequent SCARLET trial reported in 2019 enrolled septic patients with coagulopathy and organ dysfunction (cardiovascular and/or respiratory failure, platelet count 30 to 150 × 109/L or > 30%-decrease within 24 h, and PT-INR > 1.4 [SIC score > 4]) [68]. Although the difference was not statistically significant in the intention-to-treat population, a trend of better 28-day survival was observed in the subgroup that fulfilled the entry criteria at baseline (difference: 5.40%, 95% CI: -1.68% to 12.48%). In this trial, a significant inter-nations difference was noted, and a post hoc analysis revealed absolute risk reductions of 8.3% in the French population in contrast to 1.1% in the rest of the world; the greater effect in the French cohort was thought to be due to a higher rate of sustained coagulopathy and a lower rate of heparin use [69]. It is noteworthy that all the RCTs showed trends toward better outcomes in the treatment group, and a meta-analysis of RCTs showed a significant improvement in mortality [70]. Consequently, recombinant thrombomodulin is recommended for sepsis-associated DIC in Japanese sepsis guidelines [71].
Antithrombin
The largest RCT that examined the effect of antithrombin was performed in severe sepsis but not in sepsis-associated DIC patients [58]. However, Kienast et al. [72] performed a post hoc analysis in 563 patients (antithrombin group: n = 286, and placebo group: n = 277) who had DIC and did not receive concomitant heparin, and reported an absolute reduction of 14.6% in 28-day mortality in the antithrombin group (P = 0.02), whereas no such effect was seen in patients without DIC. Antithrombin is used for the treatment of DIC in Japan, and that is the recommendation of Japanese sepsis guidelines [71]. Japanese recommendations are based on data by Tagami et al. [73], who performed propensity score-matched analysis using a nationwide administrative database consisting of 9075 pneumonia patients with sepsis-associated DIC (antithrombin: n = 2663 and control: n = 6412) and created a matched cohort of 2194 pairs. The result reported a mortality difference between the groups (antithrombin: 40.6% vs. control: 44.2%, P = 0.02). Furthermore, multiple logistic regression analyses showed an association between antithrombin use and 28-day mortality (odds ratio [OR] 0.85, 95% CI: 0.75 to 0.97). In addition to the plasma-derived product, recombinant antithrombin (antithrombin-γ) was approved in Japan in 2015, and better performance in terms of improvements in DIC and SOFA scores was reported in small studies [74, 75]. Consistent with these reports, Japanese Sepsis guidelines recommend the use of antithrombin and recombinant thrombomodulin for sepsis-associated DIC [71].
Recently, a potentially beneficial effect of the combination therapy of antithrombin with recombinant thrombomodulin has been reported, especially in severe cases [76]. The effect of this combination therapy should be examined in a future trial.
Future perspectives
The mortality associated with sepsis as well as sepsis-associated DIC remains high and exceeds 30%. Accumulated evidence suggests that anticoagulant therapy is effective for critically ill patients with coagulation disorders. Sepsis is a systemic response that acutely causes multiorgan dysfunction, and is treatable with antibiotics and source control in its early phase. However, the condition gets worse once it is complicated by coagulation disorder. Therefore, it is important to screen and monitor coagulation changes in septic patients routinely with readily available methods. This review focuses on sepsis-associated DIC rather than covering all types of DIC. The SIC scoring system is specifically designed for diagnosing sepsis-associated DIC in its early phase and is simple and easy to calculate, making it useful for DIC screening and monitoring purposes in the sepsis population. Such screening and monitoring have been performed in Japan using the JAAM DIC criteria. However, since the calculation of the SIRS score was no longer used in the diagnosis of sepsis, an update is necessary. SIC was introduced to Japan by the Japanese Sepsis Guideline Working Group in 2019 as alternative diagnostic criteria [77], and it will be included in the next version of the Japanese sepsis guidelines.
As for the treatment of SIC, heparins, antithrombin, and recombinant thrombomodulin are the current choices for sepsis-associated DIC. So far, none of them has robust evidence for efficacy. There are some obstacles to designing clinical trials that prove the effectiveness of these anticoagulants. First, the endpoint has been set as mortality difference; however, there are many factors that affect the patient’s outcome, and a more sophisticated endpoint that reflects the treatment effect of anticoagulation is warranted. Second, determining the optimal dose, duration, and termination is not easy. Since activation in coagulation is a part of host defense mechanisms, the selection of targets and the choice of agents are also important. Since anticoagulation has increasingly attracted attention [4, 8, 10], it is necessary to set up international collaborative studies that adopt proper endpoints.
Conclusion
DIC is a common complication in sepsis. Although the mortality of sepsis-associated DIC is high, early detection and timely intervention are important to improve outcomes. DIC is a laboratory-based diagnosis, and the ISTH DIC SSC introduced SIC criteria which are simple, easy to calculate, and suitable for repeated evaluation to identify septic patients with a risk of progressing to overt DIC and death. Despite the advances in research on the pathophysiology, therapeutic agents for improving sepsis outcomes beyond antimicrobial treatment have never been recommended in most countries. Although recombinant thrombomodulin and antithrombin are approved by Japanese guidelines, further prospective international collaborative studies are needed.
Availability of data and materials
Not applicable.
Abbreviations
- DIC:
-
Disseminated intravascular coagulation
- ISTH:
-
International Society on Thrombosis and Haemostasis
- SIC:
-
Sepsis-induced coagulopathy
- TLRs:
-
Toll-like receptors
- PAMPs:
-
Pathogen-associated molecular patterns
- DAMPs:
-
Damage-associated molecular patterns
- TF:
-
Tissue factor
- PS:
-
Phosphatidylserine
- NETs:
-
Neutrophil extracellular traps
- PF4:
-
Platelet factor 4
- VWF:
-
Von Willebrand factor
- PAR-1:
-
Protease-activated receptor-1
- PAI-1:
-
Plasminogen activator inhibitor 1
- JAAM:
-
Japanese Society for Acute Medicine
- SIRS:
-
Systemic inflammatory response syndrome
- PT:
-
Prothrombin time
- INR:
-
International normalization ratio
- SOFA:
-
Sequential Organ Failure Assessment
- SSC:
-
Scientific Standardization Committee
- AUC:
-
Area under the curves
- HR:
-
Hazard ratio
- TTP:
-
Thrombocytopenic purpura
- aHUS:
-
Atypical hemolytic uremic syndrome
- HIT:
-
Heparin-induced thrombocytopenia
- RCT:
-
Randomized controlled trials
- OR:
-
Odds ratio
References
Lelubre C, Vincent JL. Mechanisms and treatment of organ failure in sepsis. Nat Rev Nephrol. 2018;14(7):417–27.
Squizzato A, Gallo A, Levi M, Iba T, Levy JH, Erez O, Ten Cate H, Solh Z, Gando S, Vicente V, Di Nisio M. Underlying disorders of disseminated intravascular coagulation: communication from the ISTH SSC Subcommittees on Disseminated Intravascular Coagulation and Perioperative and Critical Care Thrombosis and Hemostasis. J Thromb Haemost. 2020;18(9):2400–7.
Levi M, Sivapalaratnam S. Disseminated intravascular coagulation: an update on pathogenesis and diagnosis. Expert Rev Hematol. 2018;11(8):663–72.
Iba T, Levi M, Thachil J, Levy JH. Disseminated intravascular coagulation: the past, present, and future considerations. Semin Thromb Hemost. 2022;48(8):978–87.
Yamakawa K, Ohbe H, Taniguchi K, Matsui H, Fushimi K, Yasunaga H. Time trends of the outcomes and treatment options for disseminated intravascular coagulation: a nationwide observational study in Japan. JMA J. 2020;3(4):313–20.
Adelborg K, Larsen JB, Hvas AM. Disseminated intravascular coagulation: epidemiology, biomarkers, and management. Br J Haematol. 2021;192(5):803–18.
Chang JC. Disseminated intravascular coagulation: new identity as endotheliopathy-associated vascular microthrombotic disease based on in vivo hemostasis and endothelial molecular pathogenesis. Thromb J. 2020;18:25.
Helms J, Iba T, Connors JM, Gando S, Levi M, Meziani F, Levy JH. How to manage coagulopathies in critically ill patients? Int Care Med. 2023;49(3):273–90.
Scully M, Levi M. How we manage haemostasis during sepsis. Br J Haematol. 2019;185(2):209–18.
Iba T, Connors JM, Nagaoka I, Levy JH. Recent advances in the research and management of sepsis-associated DIC. Int J Hematol. 2021;113(1):24–33.
Futosi K, Fodor S, Mócsai A. Neutrophil cell surface receptors and their intracellular signal transduction pathways. Int Immunopharmacol. 2013;17(3):638–50.
Iba T, Levi M, Levy JH. Intracellular communication and immunothrombosis in sepsis. J Thromb Haemost. 2022;20(11):2475–84.
Salomão R, Martins PS, Brunialti MK, Fernandes Mda L, Martos LS, Mendes ME, Gomes NE, Rigato O. TLR signaling pathway in patients with sepsis. Shock. 2008;30(Suppl 1):73–7.
Gould TJ, Lysov Z, Swystun LL, Dwivedi DJ, Zarychanski R, Fox-Robichaud AE, Liaw PC, Canadian Critical Care Translational Biology Group. Extracellular histones increase tissue factor activity and enhance thrombin generation by human blood monocytes. Shock. 2016;46(6):655–62.
Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13(3):159–75.
Pérez-Figueroa E, Álvarez-Carrasco P, Ortega E, Maldonado-Bernal C. Neutrophils: many ways to die. Front Immunol. 2021;12: 631821.
Assinger A, Schrottmaier WC, Salzmann M, Rayes J. Platelets in sepsis: an update on experimental models and clinical data. Front Immunol. 2019;10:1687.
Reid VL, Webster NR. Role of microparticles in sepsis. Br J Anaesth. 2012;109(4):503–13.
Ma L, Dorling A. The roles of thrombin and protease-activated receptors in inflammation. Semin Immunopathol. 2012;34(1):63–72.
José RJ, Williams AE, Mercer PF, Sulikowski MG, Brown JS, Chambers RC. Regulation of neutrophilic inflammation by proteinase-activated receptor 1 during bacterial pulmonary infection. J Immunol. 2015;194(12):6024–34.
Joffre J, Hellman J, Ince C, Ait-Oufella H. Endothelial responses in sepsis. Am J Respir Crit Care Med. 2020;202(3):361–70.
Ito T, Kakuuchi M, Maruyama I. Endotheliopathy in septic conditions: mechanistic insight into intravascular coagulation. Crit Care. 2021;25(1):95.
Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M, Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86(5):1327–30.
Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, Mayumi T, Murata A, Ikeda T, Ishikura H, Ueyama M, Ogura H, Kushimoto S, Saitoh D, Endo S, Shimazaki S, Japanese Association for Acute Medicine Disseminated Intravascular Coagulation (JAAM DIC) Study Group. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006;34(3):625–31.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Members of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference Committee: American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Definition for sepsis and organ failure and guidelines for the use innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
Iba T, Nisio MD, Levy JH, Kitamura N, Thachil J. New criteria for sepsis-induced coagulopathy (SIC) following the revised sepsis definition: a retrospective analysis of a nationwide survey. BMJ Open. 2017;7(9): e017046.
Zhang Y, Khalid S, Jiang L. Diagnostic and predictive performance of biomarkers in patients with sepsis in an intensive care unit. J Int Med Res. 2019;47(1):44–58.
Hayakawa M, Ono K. A summary of the Japan septic disseminated intravascular coagulation study. Acute Med Surg. 2018;5(2):123–8.
Iba T, Arakawa M, Di Nisio M, Gando S, Anan H, Sato K, Ueki Y, Levy JH, Thachil J. Newly proposed sepsis-induced coagulopathy precedes international society on thrombosis and haemostasis overt-disseminated intravascular coagulation and predicts high mortality. J Intensive Care Med. 2020;35(7):643–9.
Iba T, Arakawa M, Levy JH, Yamakawa K, Koami H, Hifumi T, Sato K. Sepsis-induced coagulopathy and Japanese Association for Acute Medicine DIC in coagulopathic patients with decreased antithrombin and treated by antithrombin. Clin Appl Thromb Hemost. 2018;24(7):1020–6.
Iba T, Levy JH, Yamakawa K, Thachil J, Warkentin TE, Levi M, Scientific and Standardization Committee on DIC of the International Society on Thrombosis and Haemostasis. Proposal of a two-step process for the diagnosis of sepsis-induced disseminated intravascular coagulation. J Thromb Haemost. 2019;17(8):1265–8.
Iba T, Levy JH, Warkentin TE, Thachil J, van der Poll T, Levi M, Scientific and Standardization Committee on DIC, and the Scientific and Standardization Committee on Perioperative and Critical Care of the International Society on Thrombosis and Haemostasis. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019;17(11):1989–94.
Iba T, Levi M, Thachil J, Helms J, Scarlatescu E, Levy JH. Communication from the SSC of the ISTH on sepsis-induced coagulopathy (SIC) in the management of sepsis. J Thromb Haemost. 2022. https://doi.org/10.1016/j.jtha.2022.10.022.
Gando S, Saitoh D, Ogura H, Fujishima S, Mayumi T, Araki T, Ikeda H, Kotani J, Kushimoto S, Miki Y, Shiraishi S, Suzuki K, Suzuki Y, Takeyama N, Takuma K, Tsuruta R, Yamaguchi Y, Yamashita N, Aikawa N, Japanese Association for Acute Medicine Sepsis Registry (JAAMSR) Study Group. A multicenter, prospective validation study of the Japanese Association for Acute Medicine disseminated intravascular coagulation scoring system in patients with severe sepsis. Crit Care. 2013;17:R111.
Yamakawa K, Yoshimura J, Ito T, Hayakawa M, Hamasaki T, Fujimi S. External validation of the two newly proposed criteria for assessing coagulopathy in sepsis. Thromb Haemost. 2019;119(2):203–12.
Wang B, Zhang B, Shen Y, Li J, Yuan X, Tang N. Validation of two revised, simplified criteria for assessing sepsis-associated disseminated intravascular coagulation in ICU patients with sepsis-3: a retrospective study. Lab Med. 2022. https://doi.org/10.1093/labmed/lmac112.
Umemura Y, Yamakawa K. Optimal patient selection for anticoagulant therapy in sepsis: an evidence-based proposal from Japan. J Thromb Haemost. 2018;16(3):462–4.
Yamakawa K, Gando S, Ogura H, Umemura Y, Kabata D, Shintani A, Shiraishi A, Saitoh D, Fujishima S, Mayumi T, Kushimoto S, Abe T, Shiino Y, Nakada TA, Tarui T, Hifumi T, Otomo Y, Okamoto K, Kotani J, Sakamoto Y, Sasaki J, Shiraishi SI, Takuma K, Tsuruta R, Hagiwara A, Masuno T, Takeyama N, Yamashita N, Ikeda H, Ueyama M, Fujimi S, Japanese Association for Acute Medicine (JAAM) Focused Outcomes Research in Emergency Care in Acute Respiratory Distress Syndrome, Sepsis Trauma (FORECAST) Study Group. Identifying sepsis populations benefitting from anticoagulant therapy: a prospective cohort study incorporating a restricted cubic spline regression model. Thromb Haemost. 2019;119(11):1740–51.
Lu Z, Zhang J, Hong J, Wu J, Liu Y, Xiao W, Hua T, Yang M. Development of a nomogram to predict 28-day mortality of patients with sepsis-induced coagulopathy: an analysis of the MIMIC-III database. Front Med. 2021;8: 661710.
Fang Y, Lin S, Dou Q, Gui J, Li W, Tan H, Wang Y, Zeng J, Khan A, Wei DQ. Network pharmacology- and molecular simulation-based exploration of therapeutic targets and mechanisms of heparin for the treatment of sepsis/COVID-19. J Biomol Struct Dyn. 2023;20:1–13.
Tanaka C, Tagami T, Kudo S, Takehara A, Fukuda R, Nakayama F, Kaneko J, Ishiki Y, Sato S, Kuno M, Unemoto K. Validation of sepsis-induced coagulopathy score in critically ill patients with septic shock: post hoc analysis of a nationwide multicenter observational study in Japan. Int J Hematol. 2021;114(2):164–71.
Xiang L, Ren H, Wang Y, Zhang J, Qian J, Li B, An K, Fu L. Clinical value of pediatric sepsis-induced coagulopathy score in diagnosis of sepsis-induced coagulopathy and prognosis in children. J Thromb Haemost. 2021;19(12):2930–7.
Hosseini SF, Behnam-Roudsari S, Alavinia G, Emami A, Toghyani A, Moradi S, Zadeh MM, Mohseni S, Shafiee MA. Diagnostic and prognostic value of sepsis-induced coagulopathy and International Society on Thrombosis and Hemostasis scoring systems in COVID-19-associated disseminated intravascular coagulopathy. J Res Med Sci. 2021;26:102.
Kapoor M, Panda PK, Saini LK, Bahurupi Y. Disseminated intravascular coagulation score and sepsis-induced coagulopathy score in prediction of COVID-19 severity: a retrospective analysis. Indian J Crit Care Med. 2021;25(12):1357–63.
Shinada K, Miike T, Matsuoka A, Miyazaki M, Goto T, Sasaki A, Yamazaki H, Mori K, Nakayama K, Sakurai R, Asahi M, Yoshitake K, Narumi S, Koba M, Koami H, Sakamoto Y. Coagulation influencing liberation from respiratory support in patients with coronavirus disease 2019: a retrospective, observational study. J Nippon Med Sch. 2022. https://doi.org/10.1272/jnms.JNMS.2022_89-506.
Zou ZY, Huang JJ, Luan YY, Yang ZJ, Zhou ZP, Zhang JJ, Yao YM, Wu M. Early prophylactic anticoagulation with heparin alleviates mortality in critically ill patients with sepsis: a retrospective analysis from the MIMIC-IV database. Burns Trauma. 2022;10:tkac029.
Peng JC, Nie F, Li YJ, Xu QY, Xing SP, Li W, Gao Y. Favorable outcomes of anticoagulation with unfractioned heparin in sepsis-induced coagulopathy: a retrospective analysis of MIMIC-III database. Front Med. 2022;8: 773339.
Habe K, Wada H, Ito-Habe N, Hatada T, Matsumoto T, Ohishi K, Maruyama K, Imai H, Mizutani H, Nobori T. Plasma ADAMTS13, von Willebrand factor (VWF) and VWF propeptide profiles in patients with DIC and related diseases. Thromb Res. 2012;129(5):598–602.
Laurence J, Haller H, Mannucci PM, Nangaku M, Praga M, Rodriguez de Cordoba S. Atypical hemolytic uremic syndrome (aHUS): essential aspects of an accurate diagnosis. Clin Adv Hematol Oncol. 2016;14(Suppl 11):2–15.
Greinacher A, Selleng K, Warkentin TE. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15(11):2099–114.
Iba T, Levy JH, Wada H, Thachil J, Warkentin TE, Levi M, Subcommittee on Disseminated Intravascular Coagulation. Differential diagnoses for sepsis-induced disseminated intravascular coagulation: communication from the SSC of the ISTH. J Thromb Haemost. 2019;17(2):415–9.
Iba T, Levy JH, Thachil J, Susen S, Levi M, Scarlatescu E. Communication from the SSC of the ISTH on vascular endothelium-related biomarkers in DIC. J Thromb Haemost. 2022 in press.
Matsubara T, Yamakawa K, Umemura Y, Gando S, Ogura H, Shiraishi A, Kushimoto S, Abe T, Tarui T, Hagiwara A, Otomo Y, Fujimi S, Japanese Association for Acute Medicine (JAAM) Focused Outcomes Research in Emergency Care in Acute Respiratory Distress Syndrome, Sepsis and Trauma (FORECAST) Group. Significance of plasma fibrinogen level and antithrombin activity in sepsis: a multicenter cohort study using a cubic spline model. Thromb Res. 2019;181:17–23.
Sakai K, Wada H, Nakatsuka Y, Kubo M, Hayakawa M, Matsumoto M. Characteristics behaviors of coagulation and fibrinolysis markers in acquired thrombotic thrombocytopenic purpura. J Intensive Care Med. 2021;36(4):436–42.
Sakurai S, Kato H, Yoshida Y, Sugawara Y, Fujisawa M, Yasumoto A, Matsumoto M, Fujimura Y, Yatomi Y, Nangaku M. Profiles of coagulation and fibrinolysis activation-associated molecular markers of atypical hemolytic uremic syndrome in the acute phase. J Atheroscler Thromb. 2020;27(4):353–62.
Jackson Chornenki NL, Dwivedi DJ, Kwong AC, Zamir N, Fox-Robichaud AE, Liaw PC, Canadian Critical Care Translational Biology Group. Identification of hemostatic markers that define the pre-DIC state: a multi-center observational study. J Thromb Haemost. 2020;18(10):2524–31.
Warren BL, Eid A, Singer P, Pillay SS, Carl P, Novak I, Chalupa P, Atherstone A, Pénzes I, Kübler A, Knaub S, Keinecke HO, Heinrichs H, Schindel F, Juers M, Bone RC, Opal SM, KyberSept Trial Study Group. Caring for the critically ill patient High-dose antithrombin III in severe sepsis: a randomized controlled trial (Erratum in: JAMA 2002;287(2):192.). JAMA. 2001;286(15):1869–78. https://doi.org/10.1001/jama.286.15.1869.
Ranieri VM, Thompson BT, Barie PS, Dhainaut JF, Douglas IS, Finfer S, Gårdlund B, Marshall JC, Rhodes A, Artigas A, Payen D, Tenhunen J, Al-Khalidi HR, Thompson V, Janes J, Macias WL, Vangerow B, Williams MD, PROWESS-SHOCK Study Group. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366(22):2055–64.
Abraham E, Reinhart K, Opal S, Demeyer I, Doig C, Rodriguez AL, Beale R, Svoboda P, Laterre PF, Simon S, Light B, Spapen H, Stone J, Seibert A, Peckelsen C, De Deyne C, Postier R, Pettilä V, Sprung CL, Artigas A, Percell SR, Shu V, Zwingelstein C, Tobias J, Poole L, Stolzenbach JC, Creasey AA, OPTIMIST Trial Study Group. Efficacy and safety of tifacogin (recombinant tissue factor pathway inhibitor) in severe sepsis: a randomized controlled trial. JAMA. 2003;290(2):238–47.
Seymour CW, Kennedy JN, Wang S, Chang CH, Elliott CF, Xu Z, et al. Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA. 2019;321:2003–17.
Fu S, Yu S, Wang L, Ma X, Li X. Unfractionated heparin improves the clinical efficacy in adult sepsis patients: a systematic review and meta-analysis. BMC Anesthesiol. 2022;22(1):28.
Omidkhoda N, Abedi F, Ghavami V, Rahimi H, Samadi S, Arasteh O, Mohammadpour AH. The effect of heparin and its preparations on disseminated intravascular coagulation mortality and hospitalization: a systematic review. Int J Clin Pract. 2022;2022:2226761.
Schulman S, Sholzberg M, Spyropoulos AC, Zarychanski R, Resnick HE, Bradbury CA, Broxmeyer L, Connors JM, Falanga A, Iba T, Kaatz S, Levy JH, Middeldorp S, Minichiello T, Ramacciotti E, Samama CM, Thachil J, International Society on Thrombosis and Haemostasis. ISTH guidelines for antithrombotic treatment in COVID-19. J Thromb Haemost. 2022;20(10):2214–25.
Aikawa N, Shimazaki S, Yamamoto Y, Saito H, Maruyama I, Ohno R, Hirayama A, Aoki Y, Aoki N. Thrombomodulin alfa in the treatment of infectious patients complicated by disseminated intravascular coagulation: subanalysis from the phase 3 trial. Shock. 2011;35(4):349–54.
Murata A, Okamoto K, Mayumi T, Muramatsu K, Matsuda S. Recent change in treatment of disseminated intravascular coagulation in Japan: an epidemiological study based on a National Administrative Database. Clin Appl Thromb Hemost. 2016;22(1):21–7.
Saito H, Maruyama I, Shimazaki S, Yamamoto Y, Aikawa N, Ohno R, Hirayama A, Matsuda T, Asakura H, Nakashima M, Aoki N. Efficacy and safety of recombinant human soluble thrombomodulin (ART-123) in disseminated intravascular coagulation: results of a phase III, randomized, double-blind clinical trial. J Thromb Haemost. 2007;5(1):31–41.
Vincent JL, Francois B, Zabolotskikh I, Daga MK, Lascarrou JB, Kirov MY, Pettilä V, Wittebole X, Meziani F, Mercier E, Lobo SM, Barie PS, Crowther M, Esmon CT, Fareed J, Gando S, Gorelick KJ, Levi M, Mira JP, Opal SM, Parrillo J, Russell JA, Saito H, Tsuruta K, Sakai T, Fineberg D, SCARLET Trial Group. Effect of a recombinant human soluble thrombomodulin on mortality in patients with sepsis-associated coagulopathy: the SCARLET Randomized Clinical Trial. JAMA. 2019;321(20):1993–2002.
François B, Fiancette M, Helms J, Mercier E, Lascarrou JB, Kayanoki T, Tanaka K, Fineberg D, Vincent JL, Wittebole X. Efficacy and safety of human soluble thrombomodulin (ART-123) for treatment of patients in France with sepsis-associated coagulopathy: post hoc analysis of SCARLET. Ann Intensive Care. 2021;11(1):53.
Yamakawa K, Levy JH, Iba T. Recombinant human soluble thrombomodulin in patients with sepsis-associated coagulopathy (SCARLET): an updated meta-analysis. Crit Care. 2019;23(1):302.
Egi M, Ogura H, Yatabe T, Atagi K, Inoue S, Iba T, Kakihana Y, Kawasaki T, Kushimoto S, Kuroda Y, Kotani J, Shime N, Taniguchi T, Tsuruta R, Doi K, Doi M, Nakada TA, Nakane M, Fujishima S, Hosokawa N, Masuda Y, Matsushima A, Matsuda N, Yamakawa K, Hara Y, Sakuraya M, Ohshimo S, Aoki Y, Inada M, Umemura Y, Kawai Y, Kondo Y, Saito H, Taito S, Takeda C, Terayama T, Tohira H, Hashimoto H, Hayashida K, Hifumi T, Hirose T, Fukuda T, Fujii T, Miura S, Yasuda H, Abe T, Andoh K, Iida Y, Ishihara T, Ide K, Ito K, Ito Y, Inata Y, Utsunomiya A, Unoki T, Endo K, Ouchi A, Ozaki M, Ono S, Katsura M, Kawaguchi A, Kawamura Y, Kudo D, Kubo K, Kurahashi K, Sakuramoto H, Shimoyama A, Suzuki T, Sekine S, Sekino M, Takahashi N, Takahashi S, Takahashi H, Tagami T, Tajima G, Tatsumi H, Tani M, Tsuchiya A, Tsutsumi Y, Naito T, Nagae M, Nagasawa I, Nakamura K, Nishimura T, Nunomiya S, Norisue Y, Hashimoto S, Hasegawa D, Hatakeyama J, Hara N, Higashibeppu N, Furushima N, Furusono H, Matsuishi Y, Matsuyama T, Minematsu Y, Miyashita R, Miyatake Y, Moriyasu M, Yamada T, Yamada H, Yamamoto R, Yoshida T, Yoshida Y, Yoshimura J, Yotsumoto R, Yonekura H, Wada T, Watanabe E, Aoki M, Asai H, Abe T, Igarashi Y, Iguchi N, Ishikawa M, Ishimaru G, Isokawa S, Itakura R, Imahase H, Imura H, Irinoda T, Uehara K, Ushio N, Umegaki T, Egawa Y, Enomoto Y, Ota K, Ohchi Y, Ohno T, Ohbe H, Oka K, Okada N, Okada Y, Okano H, Okamoto J, Okuda H, Ogura T, Onodera Y, Oyama Y, Kainuma M, Kako E, Kashiura M, Kato H, Kanaya A, Kaneko T, Kanehata K, Kano KI, Kawano H, Kikutani K, Kikuchi H, Kido T, Kimura S, Koami H, Kobashi D, Saiki I, Sakai M, Sakamoto A, Sato T, Shiga Y, Shimoto M, Shimoyama S, Shoko T, Sugawara Y, Sugita A, Suzuki S, Suzuki Y, Suhara T, Sonota K, Takauji S, Takashima K, Takahashi S, Takahashi Y, Takeshita J, Tanaka Y, Tampo A, Tsunoyama T, Tetsuhara K, Tokunaga K, Tomioka Y, Tomita K, Tominaga N, Toyosaki M, Toyoda Y, Naito H, Nagata I, Nagato T, Nakamura Y, Nakamori Y, Nahara I, Naraba H, Narita C, Nishioka N, Nishimura T, Nishiyama K, Nomura T, Haga T, Hagiwara Y, Hashimoto K, Hatachi T, Hamasaki T, Hayashi T, Hayashi M, Hayamizu A, Haraguchi G, Hirano Y, Fujii R, Fujita M, Fujimura N, Funakoshi H, Horiguchi M, Maki J, Masunaga N, Matsumura Y, Mayumi T, Minami K, Miyazaki Y, Miyamoto K, Murata T, Yanai M, Yano T, Yamada K, Yamada N, Yamamoto T, Yoshihiro S, Tanaka H, Nishida O. The Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock 2020 (J-SSCG 2020). Acute Med Surg. 2021;8(1): e659.
Kienast J, Juers M, Wiedermann CJ, Hoffmann JN, Ostermann H, Strauss R, Keinecke HO, Warren BL, Opal SM, KyberSept investigators. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J Thromb Haemost. 2006;4(1):90–7.
Tagami T. Antithrombin concentrate use in sepsis-associated disseminated intravascular coagulation: re-evaluation of a “pendulum effect” drug using a nationwide database. J Thromb Haemost. 2018;16(3):458–61.
Kuroda H, Masuda Y. Comparison of protective effects of recombinant antithrombin gamma and plasma-derived antithrombin on sepsis-induced disseminated intravascular coagulation and multiple organ failure. Clin Appl Thromb Hemost. 2020. https://doi.org/10.1177/1076029620981630.
Endo S, Shimazaki R, Antithrombin Gamma Study Group. An open-label, randomized, phase 3 study of the efficacy and safety of antithrombin gamma in patients with sepsis-induced disseminated intravascular coagulation syndrome. J Intensive Care. 2018;6:75.
Murao A, Kato T, Yamane T, Honda G, Eguchi Y. Benefit profile of thrombomodulin alfa combined with antithrombin concentrate in patients with sepsis-induced disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2022;28:10760296221077096.
Iba T, Umemura Y, Watanabe E, Wada T, Hayashida K, Kushimoto S, Japanese Surviving Sepsis Campaign Guideline Working Group for disseminated intravascular coagulation. Diagnosis of sepsis-induced disseminated intravascular coagulation and coagulopathy. Acute Med Surg. 2019;6(3):223–32.
Acknowledgements
Not applicable.
Funding
This work was supported in part by a Grant-in-Aid for Special Research in Subsidies for ordinary expenses of private schools from The Promotion and Mutual Aid Corporation for Private Schools of Japan.
Author information
Authors and Affiliations
Contributions
All authors met authorship criteria and participated significantly in the study. TI and JHL wrote the draft. JH, and JC reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
TI has participated in advisory boards of Japan Blood Products Organization, Toray Medical, and Asahi Kasei Pharmaceuticals and received a research grant from JIMRO. JH has received honoraria from Diagnostica Stago, Pfizer PFE France and Sanofi Aventis France, MSD, Shionogi, and Inotrem. JMC has participated in scientific advisory boards and consulting from Abbott, Anthos, Alnylam, Bristol Myers Squibb, Five Prime Therapeutics, Pfizer, Takeda, and research funding from CSL Behring. JHL serves on the Steering Committees for Merck, Octapharma, and Werfen.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Iba, T., Helms, J., Connors, J.M. et al. The pathophysiology, diagnosis, and management of sepsis-associated disseminated intravascular coagulation. j intensive care 11, 24 (2023). https://doi.org/10.1186/s40560-023-00672-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-023-00672-5