Abstract
Background
The development of disseminated intravascular coagulation (DIC) in patients with sepsis has been repeatedly confirmed as a factor associated with poor prognosis. Anticoagulant therapy has been expected to improve sepsis patient outcomes, whereas no randomized controlled trials have demonstrated the survival benefit of anticoagulant therapies in non-specific overall sepsis. Patient selection based on the component of “high disease severity” in addition to “sepsis with DIC” has recently proved important in identifying appropriate targets for anticoagulant therapy. The aims of this study were to characterize “severe” sepsis DIC patients and to identify the patient population benefiting from anticoagulant therapy.
Methods
This retrospective sub-analysis of a prospective multicenter study included 1,178 adult patients with severe sepsis from 59 intensive care units in Japan from January 2016 to March 2017. We examined the association of patient outcomes, including organ dysfunction and in-hospital mortality, with the DIC score and prothrombin time-international normalized ratio (PT-INR), one of the components of the DIC score, using multivariable regression models including the cross-product term between these indicators. Multivariate Cox proportional hazard regression analysis with non-linear restricted cubic spline including a three-way interaction term (anticoagulant therapy × the DIC score × PT-INR) was also performed. Anticoagulant therapy was defined as the administration of antithrombin, recombinant human thrombomodulin, or their combination.
Results
In total, we analyzed 1013 patients. The regression model showed that organ dysfunction and in-hospital mortality deteriorated with higher PT-INR values in the range of < 1.5 and that this trend was more pronounced with higher DIC scores. Three-way interaction analysis demonstrated that anticoagulant therapy was associated with better survival outcome in patients with a high DIC score and high PT-INR. Furthermore, we identified a DIC score ≥ 5 and PT-INR ≥ 1.5 as the clinical threshold for identification of optimal targets for anticoagulant therapy.
Conclusions
The combined use of the DIC score and PT-INR helps in selecting the optimal patient population for anticoagulant therapy in sepsis-induced DIC. The results obtained from this study will provide valuable information regarding the study design of randomized controlled trials examining the effects of anticoagulant therapy for sepsis.
Trial registration: UMIN-CTR, UMIN000019742. Registered on November 16, 2015.
Similar content being viewed by others
Background
The Analysis for the Global Burden of Disease demonstrated the incidence of sepsis to be 48.9 million and the number of sepsis-related deaths to be 11 million worldwide in 2017 [1]. Thus, 20% of worldwide deaths resulted from sepsis, which is greater than the proportion of deaths from cancer. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) define sepsis as “life-threatening organ dysfunction caused by a dysregulated host response to infection” [2], and disseminated intravascular coagulation (DIC) is one of the most common causes of organ dysfunction associated with sepsis [3]. DIC is characterized by systemic hypercoagulation followed by microcirculatory endothelial dysfunction, leading to the development of organ dysfunction and adversely affecting patient outcomes [3,4,5,6]. Two large-scale observational studies have clearly reported significantly higher mortality rate among sepsis patients with DIC than among those without DIC [7, 8]. In addition, a nationwide multicenter observational study suggested that the screening and diagnosis of DIC were associated with a survival benefit in patients with sepsis [9], implying that some interventions for coagulation disorders associated with sepsis may contribute to improved patient outcomes.
However, no large-scale randomized controlled trials (RCTs) have demonstrated the survival benefit of anticoagulant therapies for patients with sepsis. However, a meta-analysis has indicated the important concept regarding anticoagulant therapy for sepsis; the optimal population benefiting from anticoagulant therapy consists of patients with sepsis and DIC, rather than those with sepsis only [10]. In addition, a recent study proposed that patient selection for anticoagulant therapy should be based on disease severity as indicated by the Sequential Organ Failure Assessment (SOFA) or Acute Physiology and Chronic Health Evaluation (APACHE) II scores, in addition to “sepsis with DIC” [11].
The Japanese Association for Acute Medicine (JAAM) DIC diagnostic criteria [12] (see Additional file 1: Table S1) as well as the International Society on Thrombosis and Haemostasis (ISTH) overt DIC diagnostic criteria [4] account for the most widely used diagnostic criteria [13]. The JAAM scoring system has been repeatedly validated as a highly sensitive and simple diagnostic method [7, 13, 14], consisting of systemic inflammatory response syndrome (SIRS) criteria and global coagulation markers including prothrombin time (PT) ratio, platelet counts, and fibrin/fibrinogen degradation products [12]. The aforementioned SOFA score has also been found to be useful in identifying the optimal patient population benefiting from anticoagulant therapy in patients with sepsis. However, the limitations of this score, including discrepancies with current clinical practices, such as the effect of dopamine in scoring circulatory system, lack of positive end-expiratory pressure in scoring respiratory system, and determination of cut-off values based on expert opinion rather than statistical methods, have been noted [15]. Previous studies have demonstrated that PT values are strongly correlated with SOFA scores [16] and that mortality in patients with sepsis increases with an increase in the PT value [17], further indicating that PT values could serve as an alternative to the SOFA score.
From this perspective, this study aimed to characterize severely septic DIC patients using the DIC score and PT value and to identify the patient population that would best benefit from anticoagulant therapy based on these two indicators.
Methods
Study design, setting, and ethical approval
This study was a retrospective sub-analysis of a cohort of patients with sepsis in the JAAM Focused Outcomes Research in Emergency Care in Acute Respiratory Distress Syndrome, Sepsis, and Trauma (FORECAST) database. The main investigation in this cohort had evaluated the characteristics, management, and outcomes among patients with severe sepsis in Japan [18]. The JAAM FORECAST study was a multicenter prospective study of acutely ill patients, including those with acute respiratory distress syndrome, sepsis, and trauma, that collected consecutive samples from 59 intensive care units in Japan from January 2016 to March 2017. This manuscript was written in accordance with the STROBE reporting guidelines (https://www.strobe-statement.org/).
This study was approved by the JAAM and the Ethics Committee of all participating hospitals, waiving written informed consent (JAAM, 2014-01, Hokkaido University Graduate School of Medicine, Head institute of the FORECAST group, 014-0307) since these were already previously obtained from each patient or their next of kin. Furthermore, the study was performed in accordance with the tenets underlying the Declaration of Helsinki.
Participants
The sepsis sub-cohort of the JAAM FORECAST study included adult patients aged ≥ 16 years with severe sepsis and septic shock according to the Sepsis-2 criteria [19] who had been admitted to the intensive care unit. The exclusion criteria were as follows: end-of-life care or resuscitated status after cardiac arrest at the time of sepsis diagnosis. The current study also excluded patients with substantial missing data, such as DIC scores at study enrollment. The size of the study population was dependent on the study period. All patients were followed up until discharge.
Participants were divided into four groups according to a PT-international normalized ratio (INR) ≤ 1.2, 1.2 < PT-INR ≤ 1.4, 1.4 < PT-INR ≤ 1.6, and 1.6 < PT-INR, based on existing diagnostic scoring systems of sepsis-related coagulopathies [12, 17, 20].
Definitions
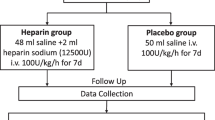
SIRS, sepsis, severe sepsis, and septic shock were defined according to the American College of Chest Physicians/Society of Critical Care Medicine consensus conference (Sepsis-1) [21] and its revised version (Sepsis-2) [19]. Moreover, disease severity was assessed based on the APACHE II score [22], and organ dysfunction was evaluated based on the SOFA score [23]. Multiple organ dysfunction syndrome (MODS) was defined as a SOFA score of ≥ 12 based on a previous study [23]. Baseline comorbidities were assessed by the Charlson Comorbidity Index (CCI) [24]. Additionally, DIC was diagnosed based on the JAAM DIC scoring system using PT-INR as a substitute for the PT ratio [12]. Anticoagulant therapy was defined as the administration of antithrombin, rhTM, or their combination based on the J-SSCG 2020 [25]. Serine protease inhibitors mentioned in this guideline were not included in anticoagulant therapy based on the results of a previous study reporting that their administration as treatment for sepsis-induced DIC had decreased over the years in Japan [26]. Heparin was also excluded from the anticoagulant therapy since no corresponding data for sepsis were present in the JAAM FORECAST sepsis database. There were no pre-determined, definitive indications for anticoagulant therapy, and anticoagulants were administered at the discretion of the attending physicians based on the treatment policies of each hospital. The standard dosage and administration of antithrombin for sepsis-induced DIC in Japan is 1500 U/day or 30 U/kg/day for 3–5 days, whereas that of rhTM is 380 U/kg for 6 days.
Data collection
Data were collected from the electronic data capture system, which was compiled by the FORECAST investigators. Patient information included baseline characteristics, various comorbidities, activity of daily living (ADL), suspected sites of infection, indicators of severity associated with sepsis, and therapeutic interventions. The primary outcome was in-hospital all-cause mortality. The SOFA scores and MODS prevalence at 72 h after admission were recorded as secondary outcomes.
Statistical analyses
Descriptive statistics used numbers for categorical variables and median values (interquartile range) for continuous variables. Categorical variables were compared using Chi-squared tests or Fisher’s exact test, as appropriate. The Mann–Whitney U and Chi-squared tests were used to determine the differences between two groups. To compare results among multiple groups, Kruskal–Wallis one-way analysis was adopted. We examined the association of prognosis with the DIC score and PT-INR value, which were assessed at the time of admission, using multivariable regression models including the cross-product term between the DIC score and PT-INR value.
To estimate the occurrence of MODS at 72 h after admission, we used multivariable logistic regression models with adjustment for age, sex, CCI, and ADL at the time of admission. We allowed the non-linear association of PT-INR with the outcome variable through a restricted-cubic-spline with knot three. Furthermore, we estimated the correlation of the SOFA score at 72 h after admission with the time to in-hospital mortality within 90 days of admission using a multivariable non-linear regression model and multivariable Cox proportional hazard regression model, respectively. In these models, the consideration of the non-linear association of PT-INR values and adjustment for the covariates were conducted similarly to the logistic regression model described above. Furthermore, to illustrate the effect of the anticoagulant therapy according to the DIC score and PT-INR value, we performed similar analyses as described above, including three- and two-way cross-product terms between the presence or absence of anticoagulant therapy, DIC scores, and PT-INR values. In the regression models, all missing values were imputed using multiple imputation methods with the predictive mean matching approach with five repetitions. We compared disease severity using the SOFA score at 0 h and APACHE II score, as well as in-hospital mortality between the groups with and without anticoagulant therapy using several DIC score and PT-INR value combinations as a sensitive analysis.
All statistical hypothesis tests were performed with a two-sided 5% significance level using SPSS version 26 (IBM Japan, Tokyo, Japan) and R version 4.1.1 (https://cran.r-project.org/).
Results
Patient demographics and baseline characteristics
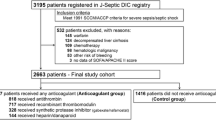
A total of 1,184 consecutive patients with severe sepsis fulfilling the inclusion criteria were included in the JAAM FORECAST sepsis study. As shown in Additional file 2: Fig. S1, six patients with missing values exceeding the threshold (> 170) detected by a one-sample robust regression with M estimator were excluded. In addition, 165 patients were excluded as shown in Table 1 and Additional file 1: Tables S2 and S3 due to missing information regarding the DIC score or PT-INR value at day 0. In total, 1013 patients were analyzed in this study. Table 1 shows baseline clinical and demographic characteristics of the patients divided into four groups according to the PT-INR value. No significant differences were observed in patient characteristics, including age, sex, and preexisting conditions such as CCI and ADL, among the groups. The SOFA and DIC scores at 0 h increased with higher PT-INR values, then plateaued at PT-INR values > 1.4. The most common site of infection was the lungs (31.3%), followed by the abdomen (26.8%), urinary tract (18.6%), and skin/soft tissues (9.7%). In addition, the proportion of patients receiving various therapeutic interventions generally tended to increase with increasing PT-INR values up to 1.6. The proportion of patients with PT-INR values > 1.6 receiving AT or rhTM was lower than that of patients with PT-INR values between 1.4 and 1.6. A comparison of platelet counts, global markers of coagulation and fibrinolysis, and clinical outcomes are shown in Additional file 1: Tables S2 and S3.
Figure 1a shows the results of a multivariable Cox proportional hazard regression model including the cross-product term between the DIC score and PT-INR. For PT-INR values approximately < 1.5, the hazard of in-hospital mortality markedly increased with increasing PT-INR values, and the changes were more pronounced with higher DIC scores. In addition, similar results were found regarding the development of MODS in patients with DIC (DIC score ≥ 4) according to a multivariate logistic regression analysis (Fig. 1b). A multivariable non-linear regression model indicated that the SOFA scores at 72 h after admission increased with higher PT-INR values, and this trend was more prominent with higher DIC scores within the range of less than approximately 1.5 (Fig. 1c).
In-hospital mortality within 90 days after admission and organ dysfunction within 72 h after admission. a Regression lines of in-hospital mortality estimated by multivariable Cox proportional hazard regression model including the cross-product term between the DIC score and PT-INR value. In-hospital mortality increased with higher values of PT-INR, and this trend was more prominent with higher DIC scores. b Regression lines of the development of MODS estimated by multivariate logistic regression analysis. The odds of the development of MODS in patients with DIC increased with higher PT-INR values and DIC scores. c Regression lines of the SOFA scores at 72 h after admission estimated by a multivariable linear regression model. The SOFA score was higher with higher PT-INR values, and this trend was more prominent with higher DIC scores. Solid and dashed lines indicate the estimated log-transformed hazard, and shaded areas represent 95% confidence intervals. DIC, disseminated intravascular coagulation; PT-INR, prothrombin time-international normalized ratio; MODS, multiple organ dysfunction syndrome; SOFA, Sequential Organ Failure Assessment
Efficacy of anticoagulant therapy according to the DIC score and PT-INR value
The median doses within 24 and 72 h after admission for patients who received AT were 1500 U (interquartile range, 1500–1500) and 4500 U (interquartile range, 1500–4500), respectively, whereas those of patients who received rhTM were 12,800 U (interquartile range, 6400–19,200) and 30,720 U (interquartile range, 17,160–55,680), respectively. Regardless of the DIC score within the range of ≥ 4, the hazard of in-hospital mortality was equivalent in patients with and without anticoagulant therapy at a PT-INR value of 1.4 (Fig. 2a). A survival benefit from anticoagulant therapy was confirmed in patients with a higher DIC score and PT-INR value (Fig. 2b) (a 3D digital figure that can trace the coordinates and be rotated is shown in Additional file 2: Fig. S2). Notably, anticoagulant therapy in patients with both lower DIC scores and PT-INR values increased the hazard of in-hospital mortality. Based on this result, we compared the disease severity according to the SOFA and APACHE II scores at hospital admission, as well as the in-hospital mortality between patients with and without anticoagulant therapy, to determine the clinical threshold for this treatment. Patients with a DIC score ≥ 5 and PT-INR ≥ 1.5 showed similar disease severity regardless of anticoagulant therapy, while in-hospital mortality was 30.6% and 46.9% (P = 0.067) in those with and without anticoagulant therapy, respectively. For factors associated with severe coagulation disorder, such as DIC score ≥ 6 and PT ≥ 1.5 or DIC score ≥ 6 and PT ≥ 1.6, anticoagulant therapy was significantly associated with better survival outcomes (P = 0.010 and P = 0.014, respectively) (Table 2).
The hazard of in-hospital mortality by PT-INR value and DIC score. a When the DIC score is ≥ 4, the hazard of in-hospital mortality is equivalent in patients with and without anticoagulant therapy when the PT-INR value = 1.4. b The survival benefit of anticoagulant therapy was confirmed in the patient population with higher DIC scores and PT-INR values. a, b Are originally similar, shown at different viewing angles to demonstrate the results. The plates represent the estimated log-transformed relative hazard. The blue plate indicates patients who received anticoagulant therapy, and the red plate indicates those who did not. DIC, disseminated intravascular coagulation; PT-INR, prothrombin time-international normalized ratio
We then performed the same abovementioned analysis for the cohort of patients with PT-INR values ≤ 2.2 to exclude the effect of an extremely high PT-INR, which could have been due to the prescribed anticoagulants. The survival benefit of anticoagulant therapy was found to be more strongly associated with increased DIC scores and PT-INR values (Fig. 3; Additional file 2: Fig. S3: 3D digital figure).
The hazard of in-hospital mortality by PT-INR value and DIC score in patients with PT-INR ≤ 2.2. The survival benefit of anticoagulant therapy was found to be more pronounced with increasing DIC score and PT-INR value. The plates represent the estimated log-transformed relative hazard. The blue plate indicates patients who received anticoagulant therapies, and the red plate indicates those who did not. DIC, disseminated intravascular coagulation; PT-INR, prothrombin time-international normalized ratio
Discussion
Our previous study found that anticoagulant therapy was associated with better outcomes according to both DIC and disease severity. Based on these findings, this study assessed the association of in-hospital mortality and organ dysfunction with JAAM DIC score, which is sensitive, simple, and available worldwide, and the PT-INR, a specific surrogate marker of disease severity. We then evaluated the interaction between these two indicators and the impact of anticoagulant therapy on in-hospital mortality. Then, we established a threshold to identify the patient population that would best benefit from this therapy. The degree of organ dysfunction became more severe and in-hospital mortality increased with increasing PT-INR. This trend was more prominent with higher DIC scores. Although patients with anticoagulant therapy in the lower range of DIC scores and PT-INR values had a higher risk of in-hospital mortality, anticoagulant therapy was associated with better survival outcomes in patients with higher DIC scores and PT-INR values. Among those with a DIC score ≥ 5 and PT-INR ≥ 1.5, patients receiving anticoagulant therapy had a lower risk of in-hospital mortality compared with those without anticoagulant therapy.
Recent studies have shown that anticoagulant therapy should be given to patients with a combination of sepsis, DIC, and high disease severity, rather than to those with sepsis only, which has been the target population in most previous large-scale RCTs [27,28,29,30,31,32]. The SCARLET trial [33], the most recent RCT that evaluated the efficacy of rhTM, adopted sepsis-associated coagulopathy characterized by PT-INR > 1.4, platelet count of 30–150 × 109/L, or a decrease in platelet count > 30% within 24 h, as inclusion criteria. The disease severity in the patient population defined by sepsis-associated coagulopathy was likely to be milder than that defined by DIC, and it was suggested that the enrollment criteria should be modified [34]. In fact, post hoc, sub-analysis of the SCARLET trial showed that patients receiving rhTM with higher levels of thrombin generation biomarkers, including prothrombin fragment 1 + 2 and thrombin antithrombin complex, had lower mortality rates compared with those receiving a placebo [35]. Importantly, this study demonstrated the harmful effects of anticoagulant therapy on sepsis patients without DIC or with lower PT-INR values. This result is supported by the concept of immunothrombosis, a physiological process characterized by the coagulofibrinolytic responses against sepsis, which is not an indication for targets of anticoagulant therapy [3, 36].
Our previous study indicated that anticoagulant therapy can be more effective when based on the level of aggravation of DIC and disease severity as evaluated by the ISTH overt DIC diagnostic criteria and APACHE II score, respectively [37]. As shown in Fig. 2, the issues investigated in the previous study can be evaluated using the DIC score and PT-INR value. Based on these results, we have identified a DIC score ≥ 5 and PT-INR value ≥ 1.5 as the threshold for identifying the optimal target population for anticoagulant therapy. It is important to note that the proportion of patients with PT-INR values > 1.6 receiving AT or rhTM was lower than that of patients with PT-INR values between 1.4 and 1.6, which may be owing to hesitation regarding anticoagulant therapy with AT or rhTM because of concerns about bleeding complications. This study supports a major purpose of diagnostic criteria: to diagnose diseases to improve patient outcomes by intervening with specific treatments [38].
This study had some limitations. First, although the data set was prospectively collected, we were unable to define causal relationships due to the retrospective study design. Second, this study did not assess the efficacy of individual anticoagulant drugs or concomitant therapy because we defined anticoagulant therapy as the administration of rhTM, antithrombin, or their combination. In addition, this study was unable to evaluate the duration and dosage of anticoagulant agents. Third, the efficacy of anticoagulant therapy might not have been evaluated correctly because we did not exclude patients with prescribed anticoagulants as with our previous studies [8, 37, 39]. However, sensitivity analysis of a cohort of patients with a PT-INR value ≤ 2.2 to exclude the effect of patients with an extremely high PT-INR (possibly due to the prescribed anticoagulants) confirmed the robustness of the results regarding the interaction between anticoagulant therapy and in-hospital mortality. Fourth, the data set used in this study did not include several important variables, such as adverse events associated with anticoagulant therapies, including bleeding complications, or the administration of heparin, which is widely used for the prevention of venous thromboembolism, and the administration of coagulation factors corrected prior to ICU admission. Fifth, we estimated regression curves using restricted-cubic-splines, a reasonable choice for assessing the non-linear association between a predictor and an outcome. However, restricted-cubic-spline linearly fits for both ends of the distribution, which do not always provide well-fitted estimates of the actual observations on these regions. Therefore, we should carefully interpret the estimates among the end of the distributions of the predictors. Sixth, data required to control potential confounders might have resulted in biased estimates of the effects. Finally, the study being conducted in a single country may limit the generalizability of the obtained results.
Conclusion
Organ dysfunction associated with sepsis and in-hospital mortality worsened with higher PT-INR values, and this trend was more prominent with higher DIC scores. Anticoagulant therapy was associated with better survival outcomes based on increases in the DIC scores and PT-INR values, while it should be noted that anticoagulant therapy would be harmful to patients with extremely high PT-INR values, probably caused by the prescribed anticoagulants. Moreover, among patients with a DIC score ≥ 5 and PT-INR value ≥ 1.5, those receiving anticoagulant therapy had lower in-hospital mortality compared with those without anticoagulant therapy. The effects of anticoagulant drugs must be properly assessed in RCTs with robust study designs to further benefit more patients with sepsis. The current results will provide important evidence for designing future RCTs evaluating the effects of anticoagulant therapies for sepsis.
Availability of data and materials
The data that support the findings of this study are available from the authors upon reasonable request.
Abbreviations
- ADL:
-
Activities of daily living
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CCI:
-
Charlson Comorbidity Index
- DIC:
-
Disseminated Intravascular Coagulation
- FDP:
-
Fibrin/fibrinogen degradation products
- FORECAST:
-
Focused Outcomes Research in Emergency Care in Acute Respiratory Distress Syndrome, Sepsis, and Trauma
- ICUs:
-
Intensive care units
- ISTH:
-
International Society on Thrombosis and Haemostasis
- JAAM:
-
Japanese Association for Acute Medicine
- J-SSCG 2020:
-
Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock 2020
- MODS:
-
Multiple organ dysfunction syndrome
- PT:
-
Prothrombin time
- PT-INR:
-
Prothrombin time-international normalized ratio
- qSOFA:
-
Quick Sequential Organ Failure Assessment
- RCTs:
-
Randomized controlled trials
- rhTM:
-
Recombinant human thrombomodulin
- SIRS:
-
Systemic inflammatory response syndrome
- SOFA:
-
Sequential Organ Failure Assessment
- SSCG:
-
Survival Sepsis Campaign Guidelines for Management of Sepsis and Septic Shock
References
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395:200–11.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Gando S, Levi M, Toh CH. Disseminated intravascular coagulation. Nat Rev Dis Primers. 2016;2:16037.
Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86:1327–30.
Bone RC. The pathogenesis of sepsis. Ann Intern Med. 1991;115:457–69.
Levi M, van der Poll T. A short contemporary history of disseminated intravascular coagulation. Semin Thromb Hemost. 2014;40(8):874–80.
Gando S, Saitoh D, Ogura H, Fujishima S, Mayumi T, Araki T, et al. A multicenter, prospective validation study of the Japanese Association for Acute Medicine disseminated intravascular coagulation scoring system in patients with severe sepsis. Crit Care. 2013;17:R111.
Gando S, Shiraishi A, Yamakawa K, Ogura H, Saitoh D, Fujishima S, et al. Role of disseminated intravascular coagulation in severe sepsis. Thromb Res. 2019;178:182–8.
Umemura Y, Yamakawa K, Hayakawa M, Hamasaki T, Fujimi S. Screening itself for disseminated intravascular coagulation may reduce mortality in sepsis: a nationwide multicenter registry in Japan. Thromb Res. 2018;161:60–6.
Umemura Y, Yamakawa K, Ogura H, Yuhara H, Fujimi S. Efficacy and safety of anticoagulant therapy in three specific populations with sepsis: a meta-analysis of randomized controlled trials. J Thromb Haemost. 2016;14:518–30.
Umemura Y, Yamakawa K. Optimal patient selection for anticoagulant therapy in sepsis: an evidence-based proposal from Japan. J Thromb Haemost. 2018;16:462–4.
Gando S, Saitoh D, Ogura H, Mayumi T, Koseki K, Ikeda T, et al. Natural history of disseminated intravascular coagulation diagnosed based on the newly established diagnostic criteria for critically ill patients: results of a multicenter, prospective survey. Crit Care Med. 2008;36:145–50.
Iba T, Umemura Y, Watanabe E, Wada T, Hayashida K, Kushimoto S. Diagnosis of sepsis-induced disseminated intravascular coagulation and coagulopathy. Acute Med Surg. 2019;6:223–32.
Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, et al. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006;34:625–31.
Vacheron CH, Friggeri A, Iwaz J, Allaouchiche B, Bohe J, Monneret G, et al. A new simplified and accurate sa-SOFA score. J Crit Care. 2020;57:240–5.
Zhang J, Du HM, Cheng MX, He FM, Niu BL. Role of international normalized ratio in nonpulmonary sepsis screening: an observational study. World J Clin Cases. 2021;9:7405–16.
Iba T, Nisio MD, Levy JH, Kitamura N, Thachil J. New criteria for sepsis-induced coagulopathy (SIC) following the revised sepsis definition: a retrospective analysis of a nationwide survey. BMJ Open. 2017;7: e017046.
Abe T, Ogura H, Shiraishi A, Kushimoto S, Saitoh D, Fujishima S, et al. Characteristics, management, and in-hospital mortality among patients with severe sepsis in intensive care units in Japan: the FORECAST study. Crit Care. 2018;22:322.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003;29:530–8.
Lyons PG, Micek ST, Hampton N, Kollef MH. Sepsis-associated coagulopathy severity predicts hospital mortality. Crit Care Med. 2018;46:736–42.
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–8.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Egi M, Ogura H, Yatabe T, Atagi K, Inoue S, Iba T, et al. The Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock 2020 (J-SSCG 2020). J Intensive Care. 2021;9:53.
Yamakawa K, Ohbe H, Taniguchi K, Matsui H, Fushimi K, Yasunaga H. Time trends of the outcomes and treatment options for disseminated intravascular coagulation: a nationwide observational study in Japan. JMA J. 2020;3:313–20.
Warren BL, Eid A, Singer P, Pillay SS, Carl P, Novak I, et al. Caring for the critically ill patient. High-dose antithrombin III in severe sepsis: a randomized controlled trial. JAMA. 2001;286:1869–78.
Ranieri VM, Thompson BT, Barie PS, Dhainaut JF, Douglas IS, Finfer S, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055–64.
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344:699–709.
Abraham E, Reinhart K, Opal S, Demeyer I, Doig C, Rodriguez AL, et al. Efficacy and safety of tifacogin (recombinant tissue factor pathway inhibitor) in severe sepsis: a randomized controlled trial. JAMA. 2003;290:238–47.
Abraham E, Laterre PF, Garg R, Levy H, Talwar D, Trzaskoma BL, et al. Drotrecogin alfa (activated) for adults with severe sepsis and a low risk of death. N Engl J Med. 2005;353:1332–41.
Wunderink RG, Laterre PF, Francois B, Perrotin D, Artigas A, Vidal LO, et al. Recombinant tissue factor pathway inhibitor in severe community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med. 2011;183:1561–8.
Vincent JL, Francois B, Zabolotskikh I, Daga MK, Lascarrou JB, Kirov MY, et al. Effect of a recombinant human soluble thrombomodulin on mortality in patients with sepsis-associated coagulopathy: the SCARLET randomized clinical trial. JAMA. 2019;321:1993–2002.
van der Poll T. Recombinant human soluble thrombomodulin in patients with sepsis-associated coagulopathy: another negative sepsis trial? JAMA. 2019;321:1978–80.
Levi M, Vincent JL, Tanaka K, Radford AH, Kayanoki T, Fineberg DA, et al. Effect of a recombinant human soluble thrombomodulin on baseline coagulation biomarker levels and mortality outcome in patients with sepsis-associated coagulopathy. Crit Care Med. 2020;48:1140–7.
Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol. 2013;13:34–45.
Yamakawa K, Gando S, Ogura H, Umemura Y, Kabata D, Shintani A, et al. Identifying sepsis populations benefitting from anticoagulant therapy: a prospective cohort study incorporating a restricted cubic spline regression model. Thromb Haemost. 2019;119:1740–51.
Gando S, Meziani F, Levi M. What’s new in the diagnostic criteria of disseminated intravascular coagulation? Intensive Care Med. 2016;42:1062–4.
Wada T, Yamakawa K, Kabata D, Abe T, Ogura H, Shiraishi A, et al. Age-related differences in the survival benefit of the administration of antithrombin, recombinant human thrombomodulin, or their combination in sepsis. Sci Rep. 2022;12:9304.
Acknowledgements
The JAAM FORECST Study Group thanks Shuta Fukuda for his special assistance in completing the study. We would also like to thank Editage (www.editage.com) for English language editing. Moreover, we wish to express our gratitude to the JAAM FORECAST Study group, Keio University School of Medicine (Junichi Sasaki), Kobe University Graduate School of Medicine (Joji Kotani), Aichi Medical University Hospital (Naoshi Takeyama), Yamaguchi University Hospital (Ryosuke Tsuruta), Kawasaki Municipal Hospital (Kiyotsugu Takuma), Kurume University (Norio Yamashita), Aizu Chuo Hospital (Shin-ichiro Shiraishi), Teikyo University School of Medicine (Hiroto Ikeda), Kawasaki Medical School (Yasukazu Shiino), Kyorin University School of Medicine (Takehiko Tarui), Chiba University Graduate School of Medicine (Takaaki Nakada), St. Luke’s International Hospital (Toru Hifumi), Kitakyushu City Yahata Hospital (Kohji Okamoto), Saga University Hospital (Yuichiro Sakamoto), Center Hospital of the National Center for Global Health and Medicine (Akiyoshi Hagiwara), Nippon Medical School (Tomohiko Masuno), Community Healthcare Organization, Chukyo Hospital (Masashi Ueyama), Osaka General Medical Center (Satoshi Fujimi, Yutaka Umemura), and the JAAM FORECAST Sepsis investigators, Osaka City University Hospital (Yasumitsu Mizobata), National Hospital Organization Sendai Medical Center (Yasuo Yamada), Saitama Medical University Saitama Medical Center (Satoru Sugiyama), Fukui Prefectural Hospital (Hiroshi Ishida), Sapporo Medical University (Eichi Narimatsu), Fukuyama City Hospital (Koji Miyasho), Hiratsuka City Hospital (Toshio Kanai), Saiseikai Utsunomiya Hospital (Satoru Miyatake), Japanese Red Cross Society Kyoto Daini Hospital (Ryouji Iiduka), Shinsyu University School of Medicine (Hiroshi Imamura), Rinku General Medical Center (Yasuaki Mizushima), Subaru Health Insurance Society Ota Memorial Hospital (Yoshitake Sato), Saitama Medical University International Medical Center (Manabu Nemoto), Aomori Prefectural Central Hospital (Hiroyuki Hanada), National Hospital Organization Hokkaido Medical Center (Yasuo Shichinohe), Saga-ken Medical Centre Koseikan (Kenji Hirahara), Hachinohe City Hospital (Akihide Kon), Juntendo University Nerima Hospital (Manabu Sugita), Kawaguchi Municipal Medical Center (Yasutaka Naoe), Kakogawa West City Hospital (Manabu Kirita), Osaka National Hospital (Daikai Sadamitsu), and Kouseiren Takaoka Hospital (Masahiro Yoshida).
Funding
This study was supported by the Japanese Association for Acute Medicine (JAAM, 2014-01).
Author information
Authors and Affiliations
Consortia
Contributions
TW conceived and designed this study; contributed to the analysis and interpretation of the data; and was responsible for drafting, editing, and submitting the manuscript. KY contributed to the acquisition of data, interpreted the data, and revised the manuscript for important intellectual content. DK played a significant role in data analysis and helped in drafting the manuscript. TA, SF, SK, TM, HO, DS, AS, and YO contributed to the design of the study, organization of data collection, drafting of database charts, and scientific discussion of all processes of the study as well as reviewed the manuscript and registered the patients. SG had a significant influence on data interpretation and the critical appraisal of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the JAAM and the Ethics Committee of all participating hospitals waiving written informed consent (JAAM, 2014-01, Hokkaido University Graduate School of Medicine, Head institute of the FORECAST group, 014-0307) since these were already previously obtained from each patient or their next of kin.
Consent for publication
Not applicable.
Competing interests
None of the authors declare any conflicts of interests in connection with the submitted article. TW reported receiving research funding from Takeda Science Foundation and personal fees from Asahi Kasei Pharma America Inc. and Asahi Kasei Pharma Japan Inc. outside the submitted work. AS reported receiving personal fees from CSL Behring outside the submitted work. All other authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Scoring system for DIC according to the JAAM. Table S2. Platelet counts, global markers of coagulation, and fibrinolysis at hospital arrival in sepsis patients according to PT-INR value. Table S3. Clinical outcomes and PT-INR at hospital arrival.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wada, T., Yamakawa, K., Kabata, D. et al. Sepsis-related coagulopathy treatment based on the disseminated intravascular coagulation diagnostic criteria: a post-hoc analysis of a prospective multicenter observational study. j intensive care 11, 8 (2023). https://doi.org/10.1186/s40560-023-00656-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-023-00656-5