Abstract
Although gliomatosis cerebri (GC) has been removed as an independent tumor type from the WHO classification, its extensive infiltrative pattern may harbor a unique biological behavior. However, the clinical implication of GC in the context of the 2021 WHO classification is yet to be unveiled. This study investigated the incidence, clinicopathologic and imaging correlations, and prognostic implications of GC in adult-type diffuse glioma patients. Retrospective chart and imaging review of 1,211 adult-type diffuse glioma patients from a single institution between 2005 and 2021 was performed. Among 1,211 adult-type diffuse glioma patients, there were 99 (8.2%) patients with GC. The proportion of molecular types significantly differed between patients with and without GC (P = 0.017); IDH-wildtype glioblastoma was more common (77.8% vs. 66.5%), while IDH-mutant astrocytoma (16.2% vs. 16.9%) and oligodendroglioma (6.1% vs. 16.5%) were less common in patients with GC than in those without GC. The presence of contrast enhancement, necrosis, cystic change, hemorrhage, and GC type 2 were independent risk factors for predicting IDH mutation status in GC patients. GC remained as an independent prognostic factor (HR = 1.25, P = 0.031) in IDH-wildtype glioblastoma patients on multivariable analysis, along with clinical, molecular, and surgical factors. Overall, our data suggests that although no longer included as a distinct pathological entity in the WHO classification, recognition of GC may be crucial considering its clinical significance. There is a relatively high incidence of GC in adult-type diffuse gliomas, with different proportion according to molecular types between patients with and without GC. Imaging may preoperatively predict the molecular type in GC patients and may assist clinical decision-making. The prognostic role of GC promotes its recognition in clinical settings.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Gliomatosis cerebri (GC) is defined as glioma showing a diffusely infiltrating growth pattern with the involvement of multiple contiguous lobes of the brain [27]. Although historically defined as an independent tumor entity in the 2007 World Health Organization (WHO) classification [27], subsequent studies showed that GC is a phenotypic growth pattern found in various types of diffuse gliomas rather than a separate entity [3, 8]. Thus, GC was excluded as a distinct tumor type in the 2016 WHO classification, as well as in the subsequent 2021 WHO classification [15, 16]. However, extensive infiltration of the brain with preservation of the local parenchymal architecture is a unique characteristic of GC that is different from the destructive and necrotic infiltrative pattern usually observed in high-grade gliomas [27, 28], and its clinical behavior is frequently neglected. However, due to its extremely invasive phenotype, GC is known to have poor prognosis within gliomas [7].
We have anecdotally noted in routine clinical practice that imaging patterns of GC seem to be relatively frequently encountered in adult-type diffuse gliomas. However, as previous studies have mostly focused on the subpopulation of patients with GC, its incidence within the entire population of adult-type diffuse glioma patients is unknown [8, 12, 25]. Moreover, the distribution of GC among the molecular types according to the recent 2021 WHO classification has not been reported; thus, whether a specific molecular type is prone to manifest as GC remains to be revealed. Due to the diffuse infiltrative growth pattern of GC, biopsy is often preferred over gross surgical removal; however, it frequently leads to nondiagnostic results due to cellular insufficiency [32]. Thus, the discovery of preoperative imaging phenotypes to predict the molecular type of GC may be crucial. Furthermore, whether GC is an important prognostic marker for more aggressive treatment planning also needs to be revealed.
We retrospectively collected data from pathologically confirmed adult-type diffuse glioma patients over a 17-year period at our institution and investigated the presence of GC. The aim of this study was to investigate the incidence, clinicopathologic and imaging correlates, and prognosis of GC in adult-type glioma patients according to the 2021 WHO classification.
Materials and methods
The requirement for patient consent was waived owing to the retrospective study design from our institutional review board (Approval number: 4-2023-0045). A total of 1,473 consecutive patients with diffuse gliomas from our institution were included in this study. The inclusion criteria were as follows: (1) WHO grade 2 to 4 diffuse gliomas confirmed by histopathology, (2) known isocitrate dehydrogenase (IDH) mutation, 1p/19q codeletion, and O6-methylguanine-methyltransferase (MGMT) promoter methylation status, and (3) aged > 18 years. The exclusion criteria were as follows: (1) histological grade 2 or 3 IDH-wildtype diffuse gliomas that did not undergo testing for three genetic parameters (telomerase reverse transcriptase promoter [TERTp], epidermal growth factor receptor [EGFR] amplification, or combined gain of entire chromosome 7 and loss of entire chromosome 10 [+ 7/-10]), thereby diagnosed as IDH-wildtype diffuse glioma, not otherwise specified [17] (n = 112); (2) histological grade 2 or 3 IDH-wildtype diffuse gliomas that were negative for all three genetic parameters (TERTp, EGFR, and + 7/-10), thereby diagnosed as IDH-wildtype diffuse glioma, not elsewhere classified [17] (n = 21); (3) follow-up loss within 3 months (n = 93); and (4) presence of H3 K27M alteration, leading to a diagnosis of diffuse midline glioma, H3 K27-altered (n = 36). A total of 1,211 adult diffuse glioma patients were analyzed (Fig. 1A).
Patient characteristics of the study cohort of adult diffuse glioma patients of our institution. (A) Flow chart of patient inclusion. (B) Representative imaging and histologic findings in a patient with IDH-wildtype glioblastoma showing GC. On MRI, a diffuse infiltrative glioma involving bilateral cerebral hemispheres is seen on FLAIR image. Faint enhancement is seen in some areas on postcontrast T1-weighted image. On low-power view (H&E; x1.25), glioma cells are diffusely infiltrated into the cerebral parenchyma, suggesting GC. (C) Pie charts summarizing the distribution of molecular types of the adult-type diffuse glioma in patients with and without GC. (D) Summary plot of the clinical, molecular and imaging findings of patients with GC. GC = gliomatosis cerebri; IDH = isocitrate dehydrogenase; MGMT = O6-methylguanine-methyltransferase, NOS = not otherwise specified, NEC = not elsewhere classified, CE = contrast-enhancing, TERTp = telomerase reverse transcriptase promoter, = epidermal growth factor receptor
Molecular classification
Patients were diagnosed according to the 2021 WHO classification [16]. All patients underwent IDH1/2 mutation, 1p/19q codeletion, and MGMT promoter methylation status testing. ATRX loss, p53 expression and TERTp mutation were also assessed. Since 2017, targeted next-generation sequencing (NGS) has been performed using the Illumina TruSight Tumor Panel. Apart from the traditional definition of IDH-wildtype glioblastoma, which is diagnosed based on the characteristic histological presence of microvascular proliferation or necrosis (“histological glioblastoma”), in the recent 2021 WHO classification, IDH-wildtype diffuse gliomas previously assigned to histological grade 2 or 3 can also be defined as IDH-wildtype glioblastoma in the presence of qualifying molecular markers (including TERTp mutation, EGFR gene amplification, and + 7/-10 (“molecular glioblastoma”). A total of 40 patients with histological grade 2 or 3 IDH-wildtype gliomas with either TERTp mutation, EGFR amplification, or + 7/-10 were classified as having IDH-wildtype glioblastoma, namely, ‘molecular glioblastoma’, according to the 2021 WHO classification [17]. ATRX loss, p53 protein expression, TERTp mutation, EGFR amplification, + 7/-10, and TP53 information was available for 1,026 (84.7%), 838 (69.2%), 868 (71.7%), 873 (72.1%), 469 (38.7%) and 870 (71.8%) patients, respectively. Details of the molecular classification can be found in Supplementary Material S1.
MRI (magnetic resonance imaging) protocol
Brain MR images, including T1-weighted, T2-weighted, fluid-attenuated inversion recovery (FLAIR), postcontrast 3D T1-weighted, and diffusion-weighted images were acquired. The detailed parameters for the MRI protocols are listed in Supplementary Material S2.
Image analysis
GC was diagnosed according to the following criteria: (1) T2-weighted or FLAIR imaging showing a diffuse process of infiltration involving at least three contiguous lobes and relative preservation of the anatomical architecture [8], and/or (2) pathological analysis confirming glial cell proliferation consistent with an infiltrative glioma. IDH-wildtype glioblastomas which have the dominant feature of a heterogeneous contrast-enhancing mass with mass effect and peritumoral edema were not diagnosed as GC if there was no underlying infiltrative non-enhancing tumor involving at least three contiguous lobes. Fig. 1B shows representative imaging and histological findings of GC.
All MRIs were reviewed and classified as either type 1 or type 2 GCs, according to the previous criteria [6]. Type 1 GCs are gliomas showing diffuse neoplastic growth and enlargement of the existing structure involved, without the formation of a discrete tumor mass at the initial clinical presentation. Type 2 GCs are gliomas with an obvious neoplastic mass, in addition to a diffuse infiltrative lesion involving more than three different lobes at the time of diagnosis (Supplementary Fig. 1) [19].
The location, presence of contrast enhancement, presence of necrosis, and presence of leptomeningeal metastases were identified [20]. Within GC patients, the presence of contrast enhancement, proportion of contrast-enhancing tumors > 5%, presence of diffusion restriction, cystic change, and hemorrhage were additionally labeled.
Bidimensional perpendicular measurement of the entire tumor was performed via preoperative and immediate postoperative imaging taken within 48-72 hour to evaluate the extent of resection (EOR) [10, 31]. The EOR was categorized as total (gross tumor removal, 100%), subtotal (≥ 75% but < 100%), partial (< 75%), or biopsy [10]. All imaging findings were reviewed by two neuroradiologists (Y.W.P. and S.S.A., with 11 and 18 years of experience, respectively) in consensus.
Statistical analysis
Comparison of patient characteristics according to GC status
Patient characteristics were compared according to GC status in the entire adult-type diffuse glioma cohort using the chi-square test for categorical variables and the t-test or Mann‒Whitney U test for continuous variables, according to normality. Identical analysis were performed within subgroups of IDH-wildtype glioblastoma patients.
Prediction of IDH mutation status within GC
Logistic regression analyses were performed to predict IDH mutation status in GC patients. Variables of interest in the univariable analysis (P < 0.05) were included in the multivariable models using backward elimination according to the likelihood ratio with a variable selection criterion of P < 0.05. The area under the curve, accuracy, sensitivity, and specificity of the multivariable model were calculated.
Survival analysis of the entire adult-type diffuse glioma cohort and subgroup of IDH-wildtype glioblastoma patients
Survival rates were determined using the Kaplan‒Meier method, and curves were compared using the log-rank test for the entire cohort. The potential associations between the parameters and overall survival (OS) were evaluated by constructing univariable Cox proportional hazards regression models for each parameter. To assess whether GC remains an independent prognostic factor, multivariable Cox proportional hazards regression modeling for OS was performed. Identical analysis was performed within the subgroup of IDH-wildtype glioblastoma patients.
Results
Patient characteristics in the entire cohort according to GC status
This study included 1,211 adult diffuse glioma patients (age range: 18–90 years, median age: 56.4 years), comprising 509 females and 702 males, with a median follow-up period of 50.5 months (95% CI: 45.4–55.7). Among the 1,211 patients, 190 (15.7%) had oligodendroglioma, 204 (16.8%) had IDH-mutant astrocytoma, and 817 (67.5%) had IDH-wildtype glioblastoma. A total of 623 (51.4%) patients had MGMT promoter methylation.
There were 99 (8.2%) patients with GC among 1,211 adult-type diffuse glioma patients, six (3.2%) among the 190 oligodendroglioma patients, 16 (7.8%) among the 204 IDH-mutant astrocytoma patients, and 77 (9.4%) among the 817 IDH-wildtype glioblastoma patients. The proportion of molecular types was significantly different between patients with and without GC (P = 0.017) (Fig. 1C). A greater proportion of gliomas with GC than without GC were IDH-wildtype glioblastomas (77.8% vs. 66.5%), while oligodendrogliomas were observed in a smaller percentage of gliomas with GC than without GC (6.1% vs. 16.5%) (Fig. 1C). The proportion of patients with MGMT promoter methylation was lower (41.4% vs. 52.3%, P = 0.037) in patients with GC than in those without GC. Among the 1,026 (84.7%) patients in which data were available, the proportion of patients with ATRX loss was greater (26.1% vs. 16.3%, P = 0.019) among those with GC than among those without GC. According to the MRI findings, the proportion of patients with necrosis (70.7% vs. 48.5%, P < 0.001) was greater in patients with GC than in patients without GC. Gross total removal was not achieved in any patients with GC compared with those without GC (0% vs. 34.1%, P < 0.001). However, gross total resection of contrast-enhancing tumor was performed in 36 (36.4%) patients with GC, while biopsy was performed in 19 (19.2%) GC patients. The characteristics of the entire cohort and the patients stratified by the presence of GC are summarized in Table 1. Fig. 1D shows a summary plot of the clinical, molecular, and imaging findings of patients with GC.
Patient characteristics in the subgroup of IDH-wildtype glioblastoma patients according to GC status
Among the 817 IDH-wildtype glioblastoma patients, 77 (9.4%) had GC. The proportion of histological grade 2 or 3 (molecular glioblastoma) patients was greater (15.6% vs. 3.8%, P < 0.001) in patients with GC than in those without GC. Among the 748 (91.6%) patients for whom data were available, the proportion of patients with ATRX loss was greater (18.9% vs. 9.9%, P = 0.018) among those with GC than among those without GC. Contrast enhancement was less frequent (89.6% vs. 96.2%, P = 0.001), while necrosis was more frequent (80.5% vs. 67.8%, P = 0.022) in patients with GC than in those without GC. The characteristics of the IDH-wildtype glioblastoma patients stratified by the presence of GC are summarized in Table 2.
Risk factors for predicting IDH mutation status in patients with GC
Only 22 (22.2%) patients with GC had IDH mutation (6 with oligodendroglioma and 16 with IDH-mutant astrocytoma). The characteristics of the GC patients according to IDH mutation status are summarized in Supplementary Table 1. Compared with IDH-wildtype glioblastoma patients with GC, IDH-mutant patients with GC were significantly younger, had a greater proportion of females, less frequent contrast enhancement, a lower proportion of contrast-enhancing tumors (> 5%), less necrosis, less diffusion restriction, less hemorrhage, less frequent manifestation of GC type 2, and a greater proportion of cystic changes.
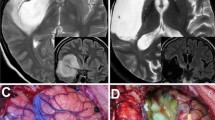
On multivariable analyses of clinical and imaging characteristics among GC patients, several imaging factors remained independent risk factors for predicting IDH mutation status, including the presence of contrast enhancement (odds ratio [OR] = 0.01, P < 0.001), necrosis (OR = 0.13, P < 0.001), cystic change (OR = 18.23, P < 0.001), hemorrhage (OR = 0.02, P < 0.001), and GC type 2 (OR = 0.08, P < 0.001) (Supplementary Table 2). The area under the curve, accuracy, sensitivity, and specificity of the multivariable model were 0.97 (95% CI 0.93-1.00), 87.9%, 86.4%, and 88.3%, respectively. Representative GC patients whose IDH mutation status were correctly predicted according to this model are shown in Fig. 2A and B. Among the 12 patients in which the multivariable model could not be used for accurate prediction, the MRI findings of all patients showed GC without contrast enhancement, necrosis, cystic, change, hemorrhage, or type 2 GC; 1 (8.3%) patient had grade 3 oligodendroglioma, and 3 (25%) patients had grade 2 IDH-mutant astrocytomas, while the remaining 8 (66.7%) patients had IDH-wildtype glioblastomas, which were histologically grade 2 or 3 (molecular glioblastoma). Representative cases of GC that were not correctly classified according to IDH mutation status are shown in Fig. 2C and D.
Representative imaging cases of GC cases with correctly (A, B) and incorrectly (C, D) predicted IDH mutation status according to multivariable model. (A) A 59-year-old male with IDH-mutant astrocytoma, CNS WHO grade 3. MRI shows a non-enhancing diffuse infiltrative tumor involving bilateral frontal lobes, left basal ganglia, and left thalamus. There is no discrete tumor mass, indicating type 1 GC. Cystic changes are seen at the left frontal lobe (arrows) on T2-weighted and FLAIR images. There is no hemorrhage on gradient recalled echo (GRE)-weighted image and no cellularity increase on apparent diffusion coefficient (ADC) map. (B) A 60-year-old female with IDH-wildtype glioblastoma, CNS WHO grade 4. MRI shows a non-enhancing diffuse infiltrative tumor involving the bilateral parietotemporooccipital lobes. There are obvious contrast-enhancing tumor masses, indicating type 2 GC. Contrast-enhancing necrotic tumor portions are seen at the right temporal and left parietotemporal lobes. There is a focal cellularity increase of solid enhancing tumor portions on ADC map. (C) A 65-year-old female with IDH-mutant astrocytoma, CNS WHO grade 2 showing a non-enhancing diffuse infiltrative tumor without necrosis, cystic change, nor hemorrhage. (D) A 32-year-old male with IDH-wildtype glioblastoma, CNS WHO grade 4. This patient was histologically grade 2, but was classified as IDH-wildtype glioblastoma due to presence of TERTp mutation (molecular glioblastoma). This case alsoshows imaging finding of a non-enhancing diffuse infiltrative tumor without necrosis, cystic change, nor hemorrhage
Prognostic factors in the entire cohort according to GC status
On multivariable analysis, age, sex, Karnofsky Performance Scale (KPS), IDH mutation, 1p/19q codeletion, MGMT promoter methylation status, EOR, and leptomeningeal metastases were found to be independent predictors of OS. GC did not remain an independent predictor of OS (HR = 1.28, P = 0.083). The univariable and multivariable Cox analysis results are shown in Supplementary Table 3. The Kaplan–Meier curve showed that GC was a predictor of poor OS (log-rank test, P < 0.001; Fig. 3A). The median OS in patients with GC was 16.7 months (95% CI: 12.2–21.3), while the median OS in patients without GC was 35.3 months (95% CI: 30.4–40.3).
Prognostic factors in subgroup of IDH-wildtype glioblastoma patients according to GC
According to multivariable GC analysis, GC status was an independent predictor of OS (HR = 1.25, P = 0.031), as were age, sex, KPS, MGMT promoter methylation status, presence of contrast enhancement, EOR, and leptomeningeal metastasis. The univariable and multivariable Cox analyses results are shown in Table 3. The Kaplan–Meier curve showed a significant difference in OS according to GC status (log-rank test, P = 0.002; Fig. 3B). The median OS in IDH-wildtype glioblastoma patients with GC was 14.2 months (95% CI: 11.9–16.4), while the median OS in IDH-wildtype glioblastoma patients without GC was 18.6 months (95% CI: 17.3–20.0).
Discussion
This retrospective single-center study comprehensively examined the incidence, clinicopathologic and imaging correlates, and prognostic implications of GCs in adult-type diffuse gliomas. The estimated overall incidence of GC was 8.2% at our institution, which suggests that GC is relatively common in patients with adult-type diffuse gliomas. There was a greater proportion of IDH-wildtype glioblastomas and a lower proportion of oligodendrogliomas in gliomas with GC than in those without GC, suggesting that the manifestation of GC can help predict molecular markers. Moreover, imaging phenotypes reflect the underlying IDH mutation status in GC patients and thus can aid in the preoperative prediction of molecular markers. GC was a poor prognostic marker in the entire cohort suggesting that the preoperative identification of GC can aid in planning treatment for these patients. Overall, our results suggest that although GC is not a separate tumor entity, the relatively high incidence of GC in adult-type diffuse gliomas and its prognostic impact promote its recognition in clinical settings.
A recent study based on the SEER database reported that GC may represent 1/400 of glial tumors, and suggested its rare manifestation [7]. However, the results from population-based databases should be interpreted with caution since databases prevent direct access to imaging and recording of the data, which may include inconsistent labeling of GCs. Furthermore, this study did not exclusively examine the incidence of GC in patients with adult-type diffuse gliomas. Our data were labeled for the presence of GC by qualified neuroradiologists experienced in neuro-oncology with central review of imaging and showed that the incidence of GC was greater than expected, accounting for 8.2% of adult-type diffuse gliomas. Considering that one GC patient may appear among every twelve adult-type diffuse glioma patients, we propose that GC should not be neglected or missed but should be actively acknowledged on imaging.
Our results show that the proportion of GC is different among molecular types; IDH-wildtype glioblastomas manifest as GC more frequently, while oligodendrogliomas rarely manifest as GC. As IDH-wildtype glioblastomas are known to display high tumorigenicity and infiltrative migration [2], there may be a greater proportion of gliomas manifesting as GC. Notably, in our study, there was a significantly greater proportion of patients with IDH-wildtype gliomas with a histological grade of 2 or 3 (molecular glioblastoma) (15.6% vs. 3.8%, P < 0.001) among those with GC than among those without GC. Several previous studies have shown that IDH-wildtype glioblastoma patients with histological grade 2 or 3 (molecular glioblastoma) frequently have GC, which may support our findings [9, 13, 26]. The significantly lower proportion of MGMT promoter methylation in GC patients warrants further investigation, and the possibility of lower tumor purity in GC patients contributing to a false negative result in MGMT promoter methylation should be considered [14, 23]. However, as 36 (36.4%) GC patients underwent gross total resection of the contrast-enhancing tumor in case of presence of contrast-enhancing tumor portion, we speculate that the proportion of lower tumor purity should not be exceptionally high. A significantly higher frequency of ATRX loss was also observed in GC compared with patients without GC, both in IDH-mutant astrocytomas (P = 0.020, not shown) and IDH-wildtype glioblastomas (P = 0.018, Table 2), suggesting that ATRX loss may also play a unique role in the manifestation of GC. ATRX loss is reported to be associated with genomic instability and DNA damage [29], with increased cellular motility and invasion [5, 18]; however, the underlying molecular pathway of this association with GC should be explored in future studies.
Our results also showed that imaging phenotypes reflect the underlying IDH mutation status and can aid in the preoperative prediction of the IDH mutation status in patients with GC. Imaging features that predict the IDH mutation status in GC are in line with imaging features that generally predict IDH mutation status in glioma patients without GC; contrast enhancement, necrosis, absence of cystic change, and hemorrhage are all well-known imaging phenotypes for the differentiation of IDH-mutant gliomas from IDH-wildtype glioblastomas [22, 33]. Preoperative prediction of molecular features in GC patients may assist in planning treatment strategies and predicting the clinical course in patients with tissue insufficiency. The IDH mutation status in the majority of GC patients could be correctly classified according to imaging phenotypes, but some IDH-wildtype glioblastomas with histological grade 2 or 3 (molecular glioblastomas) tended to exhibit imaging features indistinguishable from those of IDH-mutant astrocytomas. It should be taken note of that in GC patients showing a non-enhancing diffuse infiltrative tumor without necrosis, cystic change, nor hemorrhage, there is a high probability of IDH-wildtype glioblastomas with a histological grade of 2 or 3 (molecular glioblastoma) (66.7%). As patients with molecular glioblastomas may consequently have identical biological behavior and prognosis as histological grade 4 IDH-wildtype glioblastomas this imaging manifestation should not be overlooked [1, 24]. Because the diagnosis of IDH-wildtype glioblastomas with histological grade 2 or 3 (molecular glioblastoma) is only possible after the post-NGS era, we speculate that the true proportion of IDH-wildtype glioblastomas with histological grade 2 or 3 within these non-enhancing GCs without any additional aggressive imaging phenotype may be even greater in future studies.
GC is known to have a dismal prognosis [4, 7, 25]; however, whether it is an independent prognostic factor along with other well-known clinical and molecular prognostic factors [11] in adult-type diffuse gliomas has not been evaluated. Our database had complete critical molecular information and meticulously labeled NGS results, imaging findings, EOR status, and the presence of leptomeningeal metastases in adult-type diffuse gliomas over the following period [11, 22, 34]. Although GC was not a significant prognostic factor in the multivariable analysis of the entire adult-type diffuse glioma cohort, it remained an independent prognostic factor in IDH-wildtype glioblastoma patients. Thus, special attention should be given to IDH-wildtype glioblastoma with GC, especially when the optimal treatment strategy is yet to be revealed [35].
There are several limitations in our study. First, our study analyzed a single center, retrospectively collected dataset. Second, data on EGFR amplification, TERTp mutation, and + 7/-10 status were available only at a particular period [21]. Thus, only a small portion of patients with histological grade 2 or 3 IDH-wildtype gliomas with molecular features of glioblastomas were enrolled. Third, all GC lesions cannot be evaluated via histopathological examination because gross total removal cannot be achieved in GC patients, possibly resulting in intratumoral heterogeneity. However, in routine practice, neurosurgeons target the area with most aggressive imaging findings on surgery, which may decrease the possibility of histological downgrading of GC patients. Lastly, post-surgical treatments were not included in the analysis. However, all patients received standard adjuvant therapy in accordance with the recommended EANO guidelines, tailored to each patient’s molecular type of tumor, WHO grade, age, and performance [30].
Conclusion
The incidence of GC is 8.2% in patients with adult-type diffuse gliomas, with a greater proportion of patients with IDH-wildtype gliomas than patients without GC. Preoperative imaging features may predict IDH mutation status in GC patients. GC is an independent marker of poor prognosis in IDH-wildtype glioblastomas. Thus, it becomes important to reorganize and discuss GCs in imaging reports as well as in multidisciplinary tumor boards.
Data availability
Data generated or analyzed during the study are available from the corresponding author by request.
Abbreviations
- GC:
-
Gliomatosis cerebri
- WHO:
-
World Health Organization
- IDH:
-
Isocitrate dehydrogenase
- MGMT :
-
O6-methylguanine-methyltransferase
- TERTp:
-
Telomerase reverse transcriptase promoter
- EGFR :
-
Epidermal growth factor receptor
- NGS:
-
Next-generation sequencing
- MRI:
-
Magnetic resonance imaging
- FLAIR:
-
Fluid-attenuated inversion recovery
- EOR:
-
Extent of resection
- OS:
-
Overall survival
- KPS:
-
Karnofsky performance status
References
Aibaidula A, Chan AK, Shi Z, Li Y, Zhang R, Yang R, Li KK, Chung NY, Yao Y, Zhou L al (2017) Adult IDH wild-type lower-grade gliomas should be further stratified. Neuro Oncol 19:1327–1337. https://doi.org/10.1093/neuonc/nox078
Bergès R, Tchoghandjian A, Honoré S, Estève MA, Figarella-Branger D, Bachmann F, Lane HA, Braguer D (2016) The Novel tubulin-binding checkpoint activator BAL101553 inhibits EB1-Dependent Migration and Invasion and promotes differentiation of Glioblastoma Stem-like cells. Mol Cancer Ther 15:2740–2749. https://doi.org/10.1158/1535-7163.Mct-16-0252
Broniscer A, Chamdine O, Hwang S, Lin T, Pounds S, Onar-Thomas A, Shurtleff S, Allen S, Gajjar A, Northcott Pet al et al (2016) Gliomatosis cerebri in children shares molecular characteristics with other pediatric gliomas. Acta Neuropathol 131:299–307. https://doi.org/10.1007/s00401-015-1532-y
Carroll KT, Hirshman B, Ali MA, Alattar AA, Brandel MG, Lochte B, Lanman T, Carter B, Chen CC (2017) Management and survival patterns of patients with Gliomatosis Cerebri: a SEER-Based analysis. World Neurosurg 103:186–193. https://doi.org/10.1016/j.wneu.2017.03.103
Danussi C, Bose P, Parthasarathy PT, Silberman PC, Van Arnam JS, Vitucci M, Tang OY, Heguy A, Wang Y, Chan TA al (2018) Atrx inactivation drives disease-defining phenotypes in glioma cells of origin through global epigenomic remodeling. Nat Commun 9:1057. https://doi.org/10.1038/s41467-018-03476-6
Fuller GNKJ (2007) Gliomatosis cerebri. WHO classification of Tumours of the Central Nervous System. IARC, City
Georgakis MK, Spinos D, Pourtsidis A, Psyrri A, Panourias IG, Sgouros S, Petridou ET (2018) Incidence and survival of gliomatosis cerebri: a population-based cancer registration study. J Neurooncol 138:341–349. https://doi.org/10.1007/s11060-018-2802-z
Herrlinger U, Jones DTW, Glas M, Hattingen E, Gramatzki D, Stuplich M, Felsberg J, Bähr O, Gielen GH, Simon Met al et al (2016) Gliomatosis cerebri: no evidence for a separate brain tumor entity. Acta Neuropathol 131:309–319. https://doi.org/10.1007/s00401-015-1495-z
Izquierdo C, Barritault M, Poncet D, Cartalat S, Joubert B, Bruna J, Jouanneau E, Guyotat J, Vasiljevic A, Fenouil Tet al et al (2019) Radiological characteristics and natural history of adult IDH-Wildtype astrocytomas with TERT promoter mutations. Neurosurgery 85:E448–e456. https://doi.org/10.1093/neuros/nyy513
Karschnia P, Vogelbaum MA, van den Bent M, Cahill DP, Bello L, Narita Y, Berger MS, Weller M, Tonn JC (2021) Evidence-based recommendations on categories for extent of resection in diffuse glioma. Eur J Cancer 149:23–33. https://doi.org/10.1016/j.ejca.2021.03.002
Kim M, Kim S, Park YW, Han K, Ahn SS, Moon JH, Kim EH, Kim J, Kang SG, Chang JH al (2022) Sex as a prognostic factor in adult-type diffuse gliomas: an integrated clinical and molecular analysis according to the 2021 WHO classification. J Neurooncol 159:695–703. https://doi.org/10.1007/s11060-022-04114-4
Kwon MJ, Kang SY, Cho H, Lee JI, Kim ST, Suh YL (2020) Clinical relevance of molecular subgrouping of gliomatosis cerebri per 2016 WHO classification: a clinicopathological study of 89 cases. Brain Pathol 30:235–245. https://doi.org/10.1111/bpa.12782
Lee D, Riestenberg RA, Haskell-Mendoza A, Bloch O (2021) Diffuse astrocytic glioma, IDH-Wildtype, with molecular features of glioblastoma, WHO grade IV: a single-institution case series and review. J Neurooncol 152:89–98. https://doi.org/10.1007/s11060-020-03677-4
Lou S, Zhang J, Yin X, Zhang Y, Fang T, Wang Y, Xue Y (2021) Comprehensive Characterization of Tumor Purity and its clinical implications in gastric Cancer. Front Cell Dev Biol 9:782529. https://doi.org/10.3389/fcell.2021.782529
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM, Reifenberger Get al et al (2021) The 2021 WHO classification of tumors of the Central Nervous System: a summary. Neuro Oncol 23:1231–1251. https://doi.org/10.1093/neuonc/noab106
Louis DN, Wesseling P, Paulus W, Giannini C, Batchelor TT, Cairncross JG, Capper D, Figarella-Branger D, Lopes MB Wick W (2018) cIMPACT-NOW update 1: not otherwise specified (NOS) and not elsewhere classified (NEC). Acta Neuropathol 135: 481–484 https://doi.org/10.1007/s00401-018-1808-0
Malgulwar PB, Danussi C, Dharmaiah S, Johnson W, Singh A, Rai K, Rao A, Huse JT (2024) Sirtuin 2 inhibition modulates chromatin landscapes genome-wide to induce senescence in ATRX-deficient malignant glioma. Neuro Oncol 26:55–67. https://doi.org/10.1093/neuonc/noad155
Park S, Suh YL, Nam DH, Kim ST (2009) Gliomatosis cerebri: clinicopathologic study of 33 cases and comparison of mass forming and diffuse types. Clin Neuropathol 28:73–82. https://doi.org/10.5414/npp28073
Park YW, Han K, Ahn SS, Bae S, Choi YS, Chang JH, Kim SH, Kang SG, Lee SK (2018) Prediction of IDH1-Mutation and 1p/19q-Codeletion status using preoperative MR Imaging Phenotypes in Lower Grade Gliomas. AJNR Am J Neuroradiol 39:37–42. https://doi.org/10.3174/ajnr.A5421
Park YW, Park JE, Ahn SS, Kim EH, Kang SG, Chang JH, Kim SH, Choi SH, Kim HS, Lee SK (2021) Magnetic Resonance Imaging Parameters for Noninvasive Prediction of Epidermal Growth Factor Receptor Amplification in Isocitrate dehydrogenase-wild-type Lower-Grade gliomas: a Multicenter Study. Neurosurgery 89:257–265. https://doi.org/10.1093/neuros/nyab136
Park YW, Han K, Park JE, Ahn SS, Kim EH, Kim J, Kang SG, Chang JH, Kim SH, Lee SK (2022) Leptomeningeal metastases in glioma revisited: incidence and molecular predictors based on postcontrast fluid-attenuated inversion recovery imaging. J Neurosurg 1–11. https://doi.org/10.3171/2022.9.Jns221659
Schulze Heuling E, Knab F, Radke J, Eskilsson E, Martinez-Ledesma E, Koch A, Czabanka M, Dieterich C, Verhaak RG, Harms Cet al et al (2017) Prognostic relevance of Tumor Purity and Interaction with MGMT methylation in Glioblastoma. Mol Cancer Res 15:532–540. https://doi.org/10.1158/1541-7786.Mcr-16-0322
Stichel D, Ebrahimi A, Reuss D, Schrimpf D, Ono T, Shirahata M, Reifenberger G, Weller M, Hänggi D, Wick W et al (2018) Distribution of EGFR amplification, combined chromosome 7 gain and chromosome 10 loss, and TERT promoter mutation in brain tumors and their potential for the reclassification of IDHwt astrocytoma to glioblastoma. Acta Neuropathol 136: 793–803 https://doi.org/10.1007/s00401-018-1905-0
Taillibert S, Chodkiewicz C, Laigle-Donadey F, Napolitano M, Cartalat-Carel S, Sanson M (2006) Gliomatosis cerebri: a review of 296 cases from the ANOCEF database and the literature. J Neurooncol 76:201–205. https://doi.org/10.1007/s11060-005-5263-0
Tesileanu CMS, Dirven L, Wijnenga MMJ, Koekkoek JAF, Vincent A, Dubbink HJ, Atmodimedjo PN, Kros JM, van Duinen SG, Smits Met al et al (2020) Survival of diffuse astrocytic glioma, IDH1/2 wildtype, with molecular features of glioblastoma, WHO grade IV: a confirmation of the cIMPACT-NOW criteria. Neuro Oncol 22:515–523. https://doi.org/10.1093/neuonc/noz200
Thurnher MM (2009) 2007 World Health Organization classification of tumours of the central nervous system. Cancer Imaging 9 Spec No A: S1-3. https://doi.org/10.1102/1470-7330.2009.9001
Vates GE, Chang S, Lamborn KR, Prados M, Berger MS (2003) Gliomatosis cerebri: a review of 22 cases. Neurosurgery 53:261–271 discussion 271. https://doi.org/10.1227/01.neu.0000073527.20655.e6
Wang Y, Yang J, Wild AT, Wu WH, Shah R, Danussi C, Riggins GJ, Kannan K, Sulman EP, Chan TA al (2019) G-quadruplex DNA drives genomic instability and represents a targetable molecular abnormality in ATRX-deficient malignant glioma. Nat Commun 10:943. https://doi.org/10.1038/s41467-019-08905-8
Weller M, van den Bent M, Preusser M, Le Rhun E, Tonn JC, Minniti G, Bendszus M, Balana C, Chinot O, Dirven Let al et al (2021) EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol 18:170–186. https://doi.org/10.1038/s41571-020-00447-z
Wen PY, Chang SM, Van den Bent MJ, Vogelbaum MA, Macdonald DR, Lee EQ (2017) Response Assessment in Neuro-Oncology clinical trials. J Clin Oncol 35:2439–2449. https://doi.org/10.1200/jco.2017.72.7511
Woodworth GF, McGirt MJ, Samdani A, Garonzik I, Olivi A, Weingart JD (2006) Frameless image-guided stereotactic brain biopsy procedure: diagnostic yield, surgical morbidity, and comparison with the frame-based technique. J Neurosurg 104:233–237. https://doi.org/10.3171/jns.2006.104.2.233
Zhou H, Vallières M, Bai HX, Su C, Tang H, Oldridge D, Zhang Z, Xiao B, Liao W, Tao Y et al (2017) MRI features predict survival and molecular markers in diffuse lower-grade gliomas. Neuro Oncol 19: 862–870. https://doi.org/10.1093/neuonc/now256
Park YW, Jang G, Kim SB, Choi K, Han K, Shin NY, ... Jain R (2024) Leptomeningeal metastases in IDH-wildtypeglioblastomas revisited: comprehensive analysis of incidence, risk factors, and prognosis based on post-contrast flair.Neuro-Oncology noae091
Shin I, Sim Y, Choi SH, Park YW, Lee N, Ahn SS, ... Lee SK (2024) Revisiting prognostic factors of gliomatosis cerebri in adult-type diffuse gliomas. J Neuro-Oncol 168(2):239–247
Acknowledgements
We would like to thank Yerim Moon for her graphical support.
Funding
This research was supported by the "Team Science Award" of Yonsei University College of Medicine (6-2021-0009).
Author information
Authors and Affiliations
Contributions
Conception and design: Yae Won Park. Collection and assembly of data: Yae Won Park, Yongsik Sim, Seo Hee Choi, Sung Soo Ahn, Jong Hee Chang, Se Hoon Kim, Seung-Koo Lee. Data analysis and interpretation: Ilah Shin, Yae Won Park, Yongsik Sim. Statistical analysis: Yae Won Park, Kyunghwa Han. Manuscript writing: Ilah Shin, Yae Won Park, Rajan Jain. Final approval of the manuscript: Ilah Shin, Yae Won Park, Yongsik Sim, Seo Hee Choi, Sung Soo Ahn, Jong Hee Chang, Se Hoon Kim, Seung-Koo Lee, Rajan Jain.
Corresponding author
Ethics declarations
Ethics approval and consult to participate
Patient consent was waived owing to the retrospective study design from the institutional review board or Yonsei university (Approval number: 4-2023-0045).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shin, I., Park, Y.W., Sim, Y. et al. Revisiting gliomatosis cerebri in adult-type diffuse gliomas: a comprehensive imaging, genomic and clinical analysis. acta neuropathol commun 12, 128 (2024). https://doi.org/10.1186/s40478-024-01832-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-024-01832-w