Abstract
Despite the increasing demographic diversity of the United States’ aging population, there remain significant gaps in post-mortem research investigating the ethnoracial heterogeneity in the neuropathological landscape of Alzheimer Disease (AD). Most autopsy-based studies have focused on cohorts of non-Hispanic White decedents (NHWD), with few studies including Hispanic decedents (HD). We aimed to characterize the neuropathologic landscape of AD in NHWD (n = 185) and HD (n = 92) evaluated in research programs across three institutions: University of California San Diego, University of California Davis, and Columbia University. Only persons with a neuropathologic diagnosis of intermediate/high AD determined by NIA Reagan and/or NIA-AA criteria were included. A frequency-balanced random sample without replacement was drawn from the NHWD group using a 2:1 age and sex matching scheme with HD. Four brain areas were evaluated: posterior hippocampus, frontal, temporal, and parietal cortices. Sections were stained with antibodies against Aβ (4G8) and phosphorylated tau (AT8). We compared the distribution and semi-quantitative densities for neurofibrillary tangles (NFTs), neuropil threads, core, diffuse, and neuritic plaques. All evaluations were conducted by an expert blinded to demographics and group status. Wilcoxon’s two-sample test revealed higher levels of neuritic plaques in the frontal cortex (p = 0.02) and neuropil threads (p = 0.02) in HD, and higher levels of cored plaques in the temporal cortex in NHWD (p = 0.02). Results from ordinal logistic regression controlling for age, sex, and site of origin were similar. In other evaluated brain regions, semi-quantitative scores of plaques, tangles, and threads did not differ statistically between groups. Our results demonstrate HD may be disproportionately burdened by AD-related pathologies in select anatomic regions, particularly tau deposits. Further research is warranted to understand the contributions of demographic, genetic, and environmental factors to heterogeneous pathological presentations.
Similar content being viewed by others
Introduction
Alzheimer Disease (AD) is the most prevalent neurodegenerative brain disease and the leading cause of dementia globally [18, 40]. AD is often associated with other pathological changes and can cause irreversible damage to neurons, cell death, and brain atrophy, resulting in progressive cognitive deterioration [40]. The number of individuals in the United States aged 65 years and older is more than 55 million (16.8% of the total population), and around one out of eight Americans in this group is afflicted by AD. This number is projected to double by 2050 [9, 17]. Moreover, socioeconomic disparities within the United States population significantly impact the access to diagnosis, care, and treatment for demented persons, especially since AD and related disorders (ADRDs) disproportionally affect individuals from historically excluded ethnic groups. [6, 12, 26, 35, 46, 73]. Considering this exponential growth, ADRDs are emerging as the most significant challenge for healthcare systems worldwide. Since 2012, the World Health Organization has declared dementia a public health priority in an effort to raise awareness and mobilize collective international action from governments and policy-makers [60]. Further, in the same year, the National Alzheimer's Project Act was published in the United States with the objective of reducing dementia disparities and developing effective strategies for prevention and care for all individuals [23, 41].
When discussing AD disparities, there is a need to expand the current knowledge especially in post-mortem studies on underrepresented persons of certain race and/or ethnic groups [57]. Race and ethnicity are terms ubiquitously used in the medical literature, often interchangeably, despite their fundamentally differing definitions. Historically, race has been used to define persons with a common ancestral background and/or similar phenotypic traits, while ethnicity refers to an individual’s cultural identity and traditions. It is important to note these terms are social constructs, with many aspects influencing differences reported in literature, including but not limited to access to care, education, poverty, living conditions, culture, stress, and systemic, institutional, and individual racism [11, 78, 79]. The Hispanic population is the largest and fastest-growing ethnic group in the US, reaching 62.1 million in 2020 and accounting for 19% of the nation's total population [17]. There is evidence demographic, genetic, and/or environmental differences can result in distinct risks and manifestations of AD among different ethnic groups [19, 28, 30, 34]. Epidemiological studies have shown persons self-identifying as Hispanic are 1 to 1.5 times more likely to be diagnosed with AD and may also exhibit the onset of dementia symptoms earlier in life when compared to non-Hispanic White individuals [9, 62, 70, 73]. According to the Alzheimer’s Association Facts and Figures report in 2023, approximately 12 to 14% of Hispanic individuals who are 65 or older have been diagnosed with ADRDs in the United States, although the cause for the increased prevalence remain poorly elucidated [9, 44, 62]. Therefore, a comprehensive understanding of the ethnoracial determinants of health, particularly those hypothesized to influence the pathogenesis of ADRDs, is instrumental to mitigate risk factors and aid in early recognition of the disease process.
The definitive diagnosis of the underlying causes of AD can only be established through histopathological evaluation of the brain at autopsy [21, 67]. The neuropathological hallmarks of AD feature extracellular aggregated amyloid β (Aβ) protein in the form of Aβ plaques and intraneuronal aggregated hyperphosphorylated tau protein in the form of neurofibrillary tangles (NFTs) and neuropil threads [21]. Despite the increasing demographic diversity of the United States population, there remain significant gaps in postmortem research investigating the ethnoracial heterogeneity in the neuropathological landscape of ADRDs [9, 16, 31, 38, 57]. Most autopsy-based studies, including the frequently used neuropathologic scales (BrainNet Europe, Thal, Braak, CERAD), have been conducted almost exclusively on brains of individuals of White European ancestries, with very few studies involving individuals from other ethnic groups, particularly Hispanic decedents [4, 15, 26, 31, 38, 50, 57, 64, 69, 72, 76]. Here, our objective was to characterize the neuropathologic landscape of AD, denoting the distribution and densities of hallmark AD pathologies – NFTs, neuropil threads (NT’s) and plaques (diffuse, cored, and neuritic) in persons of Hispanic descent. To accomplish this, we utilized brain tissues from Hispanic and non-Hispanic White decedents across three research programs that encompassed Alzheimer’s Disease Research Centers at Columbia University, University of California San Diego, and University of California Davis.
Material and methods
Cohort selection
In our study, autopsy brain tissue free of personal identifiers (as determined by the Health Insurance Portability and Accountability Act—HIPAA) was obtained from three different institutions that encompassed Alzheimer’s Disease Research Centers (ADRCs) at University of California Davis, Columbia University, and University of California San Diego (Fig. 1 – Study Flowchart). Autopsies reflected persons who were denoted to have evaluations for cognitive concerns prior to death and had a recorded pathological diagnosis of AD, of which was defined as having NIA Reagan criteria of intermediate/ high and/or NIA-AA criteria of Intermediate/High AD neuropathologic change [1, 37]. Individuals of two ethnic groups were included: Hispanic and non-Hispanic White decedents, defined based on the participant’s self-reported identification utilizing forms from the National Alzheimer’s Coordinating Center (NACC) [51], genetic determinations were not made. We followed JAMA guidelines on terminology to report race and ethnicity [27]. As this was a retrospective study, data were historical, spanning multiple decades, hence NIA Reagan and NIA-AA criteria were both used.
After evaluating each site, there were 102 decedents who records identified them as having Hispanic ethnicity with available samples. A 2–1 comparison group stratified by site (UCD, UCSD, Columbia) of non-Hispanic White decedents was selected as a random sample from 843 eligible cases. The comparison sample was frequency balanced by sex and by 5-year age group (10 years for the oldest and youngest decades, 50–59 and 100–109, due to small numbers of non-Hispanic White decedents in those groups). Two non-Hispanic White decedents were chosen at random from each cell, or all available in smaller cells. After final definition of the study cohort, the dataset was re-assessed, and cases subsequently found not to meet inclusion criteria were excluded (5 cases reporting an ethnicity other than Hispanic or non-Hispanic White, and 13 cases having no available pathology data) (see Fig. 1 for flowchart). During life, research participants were enrolled in IRB-approved studies at each institution, and at death autopsies were performed after legal consent for autopsy was provided by appropriate family members.
Clinical comorbidity data
Available information regarding the presence of clinical comorbidities was recorded based on data retrieved from NACC’s Uniform Dataset (UDS) and/or similar forms, which were collected by each institution [51]. Diabetes, hypertension, and/or hyperlipidemia were present if there was history of diagnosis (recorded within the UDS as active and/or inactive) and/or if the participant was mentioned to be taking medication to treat these conditions. Presence of depression was recorded if there was history of diagnosis (active and/or inactive) of depression and/or if the participant was ever-taking antidepressant medication. Presence of stroke and/or trans ischemic attack was recorded if there was mention of history of diagnosis (active and/or inactive).
Histology and assessments
Brain areas were selected based on availability as well as having consistent sampling across all 3 institutions; here we evaluate the hippocampus, frontal, parietal, and temporal cortices. Prior to processing and assessment, twelve batch numbers were assigned using permuted block randomization within center, gender, and ethnicity stratum. As a measure to minimize potential staining differences across the three sites and due to changes in pathological criteria and antibody staining over time, 5 µm formalin fixed paraffin-embedded (FFPE) sections were cut from the designated anatomic areas available in each institution and stained in the randomized twelve batches at one location (UCD).
All sections were deparaffinized through a graded series of alcohols; unstained slides were placed into two changes of 3 min each into Xylene (HistoPrep™—Fisher Scientific, Pittsburgh, PA, USA), and placed into 2 changes of 100% alcohol (StatLab Medical Products, McKinney, TX, USA) for 2 min each, followed by 2 changes of 95% alcohol for 2 min each. After the deparaffinization was complete, the slides were placed into distilled water. For assessment of Aβ deposits, slides were submitted to pretreatment prior to staining including 10 min in 87% formic acid, endogenous peroxidases were block with 3% Hydrogen Peroxide with subsequent applications of primary and secondary antibodies. The immunohistochemistry staining was performed using the 4G8 monoclonal antibody against Aβ (1:1600; Covance Labs, Madison, WI, USA).
For assessment of tau pathology, the pretreatment used for the AT8 antibody is Heat-Induced-Epitope-Retrieval (HIER). The deparaffinized slides were placed into a plastic coplin jar filled with a Target Retrieval Solution (Citrate Buffer, pH 6.1) and posteriorly placed into a pressure cooker for HIER. Then, slides were stained using a specific antibody for phosphorylated tau, AT8 (1:1000, Thermo Scientific, Waltham, MA, USA). All antibody staining was conducted following standard procedures on automated machines (i.e. autostainers; DAKO AutostainerLink48, Agilent, Santa Clara, CA, USA) utilizing proper positive and negative control for each specific antibody. All staining and immunohistochemistry procedures were performed at the UC Davis Histology Core, a Clinical Laboratory Improvement Amendments (CLIA) and College of American Pathologists (CAP) accredited laboratory operating under the best laboratory practices standards and meets all Federal, State of California, and UC Davis guidelines and regulations.
All immunohistochemistry-stained slides were digitized to obtain whole slide imaging (WSI) using the Zeiss Axio Scan Z.1 scanner at 40 × magnification (0.11 µm/pixel) and files were saved in the proprietary czi format at a 60% compression rate. Semi-quantitative histopathological assessments of each area/stain were conducted by an expert (BD) who was blinded to the demographic, clinical, and genetic information of all cases and their ADRC origin, adapting CERAD and BrainNet Europe semi-quantitative assessments and following guidelines put forth by the NACC Neuropathology form version 10 [4, 14, 15, 48].
The CERAD scoring system was adapted to provide a semi-quantitative assessment of NFTs, cored, diffuse, and neuritic plaques in the densest mm2 of tissue area on the slide (none = no pathology denoted as 0, sparse (0–5) denoted as 1, moderate (6–20) denoted as 2, or frequent (greater than 20) denoted as 3); the final score represents the densest area evaluated within the stated subregion for the specific pathology [48].
The Thal amyloid phase scoring system was utilized to denote the anatomic distribution of amyloid plaques in the neocortex, hippocampus, basal ganglia, substantia nigra, and cerebellum, as well as to analyze the neuroanatomical hierarchical course of the disease [72]. The maximum Thal phase was assigned if plaques were observed in: Phase 1: neocortex; Phase 2: hippocampus and entorhinal cortex; Phase 3: putamen; Phase 4: substantia nigra; and Phase 5: cerebellum. Summary of data previously collected by each site are in Table 1.
Neuropil threads semi-quantitative densities were defined as 0 (0), + (1), + + (2) or + + + (3) according to BrainNET Europe Criteria [4]. Because our study was based on evaluation of tissue and data collected retrospectively, differences in sampling protocols among centers were present. We did not receive and evaluate tissue from the occipital cortex, hence we did not uniformly evaluate Braak NFT stage [15] in these cases. Available data from previous evaluations, albeit done by different experts/neuropathologists over time at the respective centers is included and is present in select Tables to aid with the cohort description.
Statistical analysis
Demographic, clinical, and neuropathologic characteristics were summarized separately for Hispanic and non-Hispanic White decedents, overall and by site (Table 1). Quantitative variables were summarized by means and standard deviation, and the means for both groups were compared by Student’s two-sample T test. For semi-quantitative or non-normally distributed variables, medians and ranges were provided as summary statistics, and Wilcoxon’s two-sample nonparametric test, using average scores for ties. Analyses of individual variables were restricted to decedents with non-missing data, with no attempt at imputation. To reduce the potential impact of heterogeneity due to the wide range of ages in the sample, we further compared neuropathologic summaries of the two groups by regression analyses, adjusted for age and sex as well as for site (Additional file 1: Table S3). We used linear regression for quantitative variables and ordinal logistic regression for semi-quantitative variables with small numbers of categories. Secondary analyses further compared demographic, clinical, and neuropathologic characteristics across three groups based on Hispanic heritage (Caribbean, Mexican, and Others) and non-Hispanic White decedents, using Kruskal–Wallis nonparametric tests for ordinal categorical variables as an omnibus test of equality across all groups. To assess pairwise differences in neuropathologic characteristics across the four groups, an ordinal logistic regression model was used. The model was adjusted by age and sex, but not site since all Caribbean decedents were from one site. The false discovery rate (FDR) was used for multiple comparisons. All statistical analyses were performed using SAS software (version 9.4, SAS institute, Inc.; Cary, NC, USA). Figures were created using Lucidchart (Lucidchart.com), Biorender (Biorender.com), and R Studio package ggplot2.
Results
Demographics
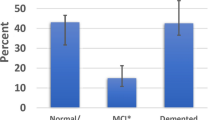
A total of 277 deceased individuals were screened across the three institutes and included in our analyses. As we had a 2:1 matching schema, 33.2% (n = 92) were persons self-identified as Hispanic decedents and 66.8% (n = 185) as Non-Hispanic White decedents. Table 1 summarizes the demographics, neuropathologic, and clinical characteristics of the participants and the groups. Age and gender distributions were nearly identical for Hispanic and non-Hispanic White decedents, reflecting the sampling design (Table 1). The largest Hispanic heritage-based group was of Caribbean heritage (36/92 [39.1%]), predominantly from Puerto Rico (22/92 [23.9%]), followed by Dominican Republic (9/92 [9.8%]), and then Cuba (5/92 [5.4%]). Mexican decedents were the second largest subset of our study cohort (31/92 [33.7%]); fewer Hispanic decedents were of other origins (4/92 [4.3%]), South American descent (3/92 [3.3%]), or of unknown origin (no data available) (18/92 [19.6%]).
Non-Hispanic White decedents averaged five more years of formal education attainment when compared to Hispanic decedents (P < 0.01). The groups were similar in having just over 50% having at least one APOE e4 allele. Some differences were apparent among those with data available on clinical comorbidities, with Hispanic decedents having almost three times higher rates of diabetes (P = 0.01) and two times higher rates of stroke (P = 0.05), but lower proportions of high cholesterol (P = 0.02). Hypertension was present in over half of each group, with higher levels in Hispanic decedents (P = 0.04). Depression was reported in about a quarter of each group, and transient ischemic attack in about 1 in 7 decedents in each group. The proportions with missing data on clinical comorbidities were similar in each group (Table 1).
Neuropathology
Although all cases had a pathological diagnosis of AD, a primary pathological diagnosis of AD with no secondary pathology present was found in 36.8% of the overall cohort; similar percentages were found for Hispanic (37%) and non-Hispanic White decedents (36.8%) (P = 0.97). The second most frequent diagnosis was cerebral vascular disease (CVD) concomitant with AD, with similar results between groups (Hispanic decedents (34.8%) and non-Hispanic decedents (37.8%) P = 0.62). A third frequent diagnosis of mixed pathologies, Lewy body disease concurrent with AD, was significantly more prevalent among Hispanic individuals (29.3%) than among non-Hispanic White (18.4%) individuals (P = 0.04) (Table 1).
Neuropathologic findings for the posterior hippocampus were similar for both groups, with median levels of 1 (sparse) for core plaques, 2 (moderate) for neuritic plaques, and 3 (frequent) for diffuse plaques, neuropil threads, and NFTs (Table 2). Adjustment via ordinal logistic regression did not alter this finding. Findings in the frontal cortex showed greater levels of neuritic plaques (median 2 vs. 1, p = 0.02) and neuropil threads (median 3 vs. 2, p = 0.02) for Hispanic decedents than for non-Hispanic White decedents. The groups had similar levels of core plaques, NFTs, and diffuse plaques. Ordinal logistic regression did not modify these findings (Additional File 1: Table S1). In the parietal cortex, levels of core plaques, neuritic plaques, and NFTs were similar in Hispanic and non-Hispanic White decedents with medians of 2, while diffuse plaques had medians of 3 in each group. The median for neuropil threads was 2 in non-Hispanic White and 3 in Hispanic decedents, approaching statistical significance (p = 0.06), with some of the difference further accounted for in ordinal logistic regression models (Additional file 1: Table S2). The temporal cortex showed similar findings for both groups for neuritic plaques (medians of 3 for Hispanic decedents and 2 for non-Hispanic White decedents; p = 0.56), as well as diffuse plaques, neuropil threads, and NFTs (median of 3 for both groups for all pathologies.) However, even though the median was 1 for both groups, a longer upper tail was observed in the non-Hispanic White decedents for core plaques (p = 0.02) (Fig. 2). Additional analyses were carried out adjusting for Braak NFT Stage, Thal phase, and CERAD score, and results did not change substantially, although there was sparse numbers for lower scores of Braak NFT stage, Thal phase, and CERAD score.
A visualization comprising of a combination of violin and box plots was used to depict the distribution of various pathologies (cored plaques: CPs, diffuse plaques: DPs, neuritic plaques: NPs, neuropil threads: NTs, and neurofibrillary tangles: NFTs) in three specific brain areas-frontal, temporal, and parietal cortices. The violin plots were used to display the distribution of the data, while the boxes indicate the range between the first and third quartiles. The bold horizontal line inside the boxes represents the median value. Additionally, the whiskers extend beyond the upper and lower limits of the box and indicate the range of data within 1.5 times the length of the box
In secondary exploratory analyses, comparisons further divided the Hispanic participants into three groups based on Hispanic heritage: Caribbean decedents (N = 36), Mexican decedents (N = 31), and other decedents (N = 25) (Additional file 1: Table S2). In the posterior hippocampus, the Caribbean heritage group had higher levels of neuritic plaques and neuropil threads than non-Hispanic White, and the Mexican heritage group (Additional file 1: Tables S2 and S3). Caribbean decedents also had higher levels of neuritic plaques and neuropil threads than Non-Hispanic White decedents in the frontal, parietal, cortices, and NFTs in the frontal cortices (Fig. 3).
Examples of the histopathologic densities of tau-deposits and corresponding overall regional density scores (for neuropil threads: NTs, and neurofibrillary tangles: NFTs- lower left corner in each image) in three brain regions (frontal, temporal, and parietal cortices). Cases were selected based on heritage group within Hispanic decedents and non-Hispanic White decedents, having similar age at death, gender, and AD likelihood (ADNC = Alzheimer disease neuropathologic change). Scale bar = 50 μm
Discussion
We report the neuropathological findings and the frequency distribution of select clinical comorbidities in a research-based autopsy cohort of 277 decedents of Hispanic and non-Hispanic White heritage with AD. Our analysis of semi-quantitative scores using established standardized scales demonstrates Hispanic decedents had greater densities of neuritic plaques and neuropil threads in the frontal cortex, whereas non-Hispanic White decedents had a greater amount of core plaques in the temporal cortex. We also observed a higher range in the score of neuropil threads in the parietal cortex of Hispanic decedents, although it was not significantly different when compared to non-Hispanic White decedents. Interestingly, there were no differences in the pathological findings of the posterior hippocampus between groups. Due to our inclusion criteria and analytic methodology, we had a certain level of homogeneity in terms of age, gender, APOE e4 allele frequency, and final clinicopathological diagnoses (Table 1). There were notable differences in educational attainment and select clinical comorbidities between the groups, with Hispanic decedents having significantly lower educational levels and greater rates of diabetes, hypertension, and stroke, as well as CVD, which are underlying risk factors of AD and may have contributed to the heterogeneous pathological presentation. Our data, provide evidence Hispanic decedents with AD are disproportionately burdened by AD-related pathology, particularly tau deposits, in comparison to non-Hispanic White decedents, based on differences in their pathological profile and severity.
To date, limited neuropathological studies have been conducted to explore disparities in the manifestation of AD in underrepresented populations, particularly in Hispanic persons [26, 31, 57, 64, 69, 76]. In a previous neuropathological study on demented persons, our group reported Hispanic decedents to have a higher incidence of mixed pathologies concurrent with AD, compared to non-Hispanic White decedents who have a significantly higher rate of non-mixed AD (43% vs. 14%) [26]. It is worth noting Hispanic participants in the present study focused on AD also had lower levels of educational attainment and higher rates of co-existing health conditions, which partially align with our previous findings. The lower levels of education in individuals of Hispanic descent might contribute to substantial disparities in their susceptibility to dementia, as it has been shown even a minimal increase in formal education can result in improved cognitive reserve could compensate the neurodegeneration [24, 45]. Interestingly, in the current study we observed a lower percentage of cerebrovascular disease (CVD) in this Hispanic cohort, and this was not different from the non-Hispanic White cohort, in contrast to what we previously reported in the dementia cohort [26]. This discrepancy could be attributed to variations in cohort inclusion/exclusion criteria, the recruitment practices of participants across the three centers, as well as the diversity within the Hispanic cohort. For instance, UC Davis and Columbia include participants regardless of their prior or current cardiovascular risk factors or disease, while UCSD excludes persons having insulin dependent diabetes and major stroke or neurological illness [69] (see Additional file 1: Table S4). There could also be site/temporal differences in the way co-morbidities, such as concomitant pathological diagnoses, are reported. Furthermore, our study included Hispanic individuals from different heritage groups, while prior works focus on select groups [64, 69, 76]. Additional studies delving further into these data are warranted to understand underlying causes of the discrepancies.
Due to the retrospective nature of the study, we utilized the term Hispanic decedents to encompass persons from many different origins; the Hispanic community should not be viewed as one monolithic group [49, 73]. This population has intrinsically diverse genetic, socioeconomic, and cultural characteristics that may help to address the disparities previously reported in AD's clinical presentation [8, 61, 62, 70, 73]. Therefore, to account for this diversity, we performed additional exploratory analyses, although underpowered, to examine potential differences within the Hispanic cohort by creating three groups based on the individuals' self-reported Hispanic heritage: Caribbean, Mexican, and others (including individuals from South America). We also found pathological heterogeneity within Hispanic decedents, with Caribbean decedents having a higher presence of plaques, threads, and NFTs in all four evaluated brain areas, as well as lower levels of education and higher rates of diabetes, hypertension, stroke, and depression compared to the two other Hispanic decedent subgroups, albeit cohort numbers were low having insufficient power and effect size. We also observed in the brains of persons of Mexican descent lower levels of neuropil threads in both the hippocampus and the temporal cortex, even lower than non-Hispanic White decedents (Additional file 1: Table S3). This may aid in explanations of increased AD prevalence in Caribbean individuals [7, 42, 58, 73]. Additionally, with respect to dementia incidence rates Caribbean had higher average frequencies than Mexican persons [10, 25, 58, 71]. Although these results are intriguing, they are underpowered and may well not be representative of the population given the high selectivity of autopsy cohorts. Our data, however, support further study of the role this intrinsic diversity plays in the development of AD [73]. The geographical distribution of the Hispanic population also varies across the United States [2, 22, 57]. Mexican decedents are the largest group and are primarily concentrated in the southwest and south of the country, while Caribbean decedents are more heavily concentrated on the east coast [2, 22]. California and New York are the states with high Hispanic population, ranking first and fourth, respectively [63], which also reflects the origin of our study participants: all evaluated Caribbean participants came from Columbia, and the Mexican participants were mainly from UCSD and UCD.
Generally, the accumulation of tau deposits, in the form of NTs and NFTs, is hypothesized to start in the entorhinal cortex and hippocampus and then spreads to the neocortex. Nonetheless, there are also subtypes of AD with atypical presentation of pathological features, such as sparing the hippocampus [53]. Tau is a microtubule associated protein widely expressed in neurons of the human brain and plays important physiological roles on microtubule assembly and stabilization, as well as promotion of axonal outgrowth [75]. In non-pathological conditions, tau has a naturally unfolded structure, showing a low tendency to aggregation [52]. The correlation between tau pathology and cognitive decline has been well established [20, 32, 43, 55, 56]. Our results did not reveal a significant difference in NFT scoring between groups, although most cases had scores of 2 (moderate) or 3 (frequent) and more finer grain quantitative analyses may aid in providing insight, as has been done with identifying AD subgroups [53]. That stated, our findings did reveal a more pronounced presence of neuropil threads in the frontal and parietal cortices of Hispanic decedents, but no differences within temporal cortices. Typically, neuropil threads are more predominant in comparison to NFTs in immunohistochemically stained sections, which implies that evaluating the presence and density of neuropil threads instead of NFTs may provide more optimal insights into neurodegenerative disease progression, as has been done with the BrainNet Europe Criteria; however, better interrater agreement has been achieved evaluating more severe stages of neuropil threads (Stage V and VI) [4]. To aid in unlocking the secrets of these devastating deposits, more quantitative analysis is needed to aid in understanding potential disease subtypes based on tau pathologies. This variability in severity may arise from several factors including genetic predisposition, concurrent neuropathologies, and/or environmental factors.
Establishing criteria for assessing pathological hallmarks of AD has been a major milestone in the dementia research field, providing a standard procedure for routine diagnostic settings such as NIA Reagan criteria and NIA-AA guidelines (Intermediate or High) [1, 37]. The field has historically used semi-quantitative (CERAD neuritic plaque density) [48] and regional distributions (Thal and Braak) [15, 72] for AD assessment. These disease scales were primarily derived based on the evaluation of the brain tissue of non-Hispanic White individuals, with limited numbers and highly variable methods for sample collection and processing. Specifically, the initial paper on Braak NFT stage was based on a cohort of 83 brains of White individuals of European descent [15]. Furthermore, in our study, we were unable to perform a stage of the tau-related pathology in our study cohort using Braak or BrainNet Europe criteria, as the occipital cortex was not included in the evaluation; available retrospective data collected at each site (UCD, UCSD, Columbia) were included. Further, these criteria employ semi-quantitative scoring methods, which can have interrater variability [5, 33, 36, 47, 54]. Quantitative measurement of pathological features through methods in digital pathology and/or machine learning are a novel and rapidly growing field, particularly promising for providing scalable deeper phenotyping of ADRDs [3, 39, 59, 65, 67, 68, 77]. However, these innovative computer-based evaluation methods require training and validation on large quantities of digitalized and annotated pathology data, which can pose a significant hurdle. To date, many machine learning algorithms have yet to be tested/validated on multiple brain areas to understand generalizability.
Our results should be interpreted with consideration of certain constraints related to data collection and cohort characteristics. Despite applying robust sample selection methods, variation in procedures among centers may contribute to potential bias [26, 31, 74]. The autopsy studies and clinical recruitment within the three institutes are based on a volunteer sample of convenience. Our analyses controlled for the participants' age, gender, and center of origin, providing an increased confidence in our results. However, our results may not be representative of the general Hispanic population affected by AD dementia. Our study utilized case materials collected over a 30-year period. There can be variability in the time intervals between the last clinical evaluation and death, in addition evaluates for specific disorders have evolved over time as well as persons conducting have changed at each of the institutions. Even with careful quality control and data cleaning, there still may be discrepancies, especially within large datasets. This highlights the complexities of retrospective data analyses. Furthermore, the brain tissue evaluated during our study was collected over time, and variations in sampling protocols, preparation methods (e.g., sectioning and/or fixation), and preservation of paraffin-embedded tissue can influence staining quality [13, 29, 66, 74]. To mitigate possible center bias on our results, we centralized slide staining at a single CLIA and CAP certified laboratory with extensive experience conducting pathological staining protocols and choose anatomic areas with similar sample procedures although rostro/caudal medio/lateral and superior/inferior variations can exist. We also only evaluated one 5 µm section per stain and this may not be representative of an entire region. We used randomized block sequences for processing and assessment to further reduce bias. The selected stains (AT8, 4G8) used in this study have previously been used within numerous centers and in published scales [74]. Hence given these limitations, we focused analyses on the neuropathology variables collected in a standardized fashion through this study and to highlight the heterogeneity of the pathological changes.
Despite the limitations, this study has numerous strengths. To our knowledge, this is the largest autopsy-based study focused on Hispanic decedents with AD. We have measured the hallmark pathologies of AD using validated semi-quantitative measurements, providing an unbiased evaluation across multiple brain regions. The participants of the two groups had systematic pathological assessments performed by a single individual blind to all information pertaining to the cases, reducing potential interrater variability and evaluation bias. This innovative multi-center autopsy-based study presents a foundation of novel information about the neuropathological landscape heterogeneity of AD among a cohort of Hispanic and non-Hispanic White decedents matched on demographic features.
In summary, our results indicate adjusting for age, sex, and center of origin, Hispanic decedents with a pathological diagnosis of AD prior to death have greater levels of tau pathology in select brain regions when compared to non-Hispanic White decedents, demonstrating differences of the neuroanatomical distribution and severity of AD-related pathology. Although the focus of this work was to characterize the differences in the hallmark pathology of AD, further research is needed to elucidate the role of other common dementia-related pathologies (such as CVD and Lewy body disease) and how their interaction influences disease onset and progression in persons of Hispanic descent. It is vital to note these historic categories are social constructs and cultural and social associations may underlie differences. Additional studies using innovative quantitative methods can aid in broadening these findings, providing detailed brain tissue phenotyping in more ethnically diverse groups. Overall, the results we present here emphasize the importance of more thorough deeper phenotyping of the AD neuropathological landscape among diverse ethnic cohorts for enhanced clinical correlations and precision medicine advancement [67]. We hope to contribute to filling the historical knowledge gap about how ethnicity may interplay with genetic, sociocultural, and environmental factors affecting the prevalence and trajectory of ADRDs among underrepresented populations, ultimately aiming for better preventive measures, treatments, and prognoses for all individuals.
Availability of data and materials
If accepted for publication and after journal release of the formal formatted manuscript, associated data will be available through Dryad (https://datadryad.org/stash). Dryad, is a tool for researchers to describe, upload, and share their research data. Datasets published in Dryad receive a citation and can be versioned at any time.
References
Consensus recommendations for the postmortem diagnosis of Alzheimer's disease. (1997) The National Institute on Aging, and Reagan Institute Working Group on Diagnostic Criteria for the Neuropathological Assessment of Alzheimer's Disease. Neurobiol Aging 18: S1-2
Hispanic Population and Origin in Select U.S. (2014) Metropolitan Areas https://www.pewresearch.org/hispanic/interactives/hispanic-population-in-select-u-s-metropolitan-areas/
(FDA) FaDA (2017) FDA allows marketing of first whole slide imaging system for digital pathology https://www.fda.gov/news-events/press-announcements/fda-allows-marketing-first-whole-slide-imaging-system-digital-pathology. Accessed 08/31/2022 2022
Alafuzoff I, Arzberger T, Al-Sarraj S, Bodi I, Bogdanovic N, Braak H et al (2008) Staging of neurofibrillary pathology in Alzheimer’s disease: a study of the BrainNet Europe Consortium. Brain Pathol 18:484–496. https://doi.org/10.1111/j.1750-3639.2008.00147.x
Alafuzoff I, Pikkarainen M, Al-Sarraj S, Arzberger T, Bell J, Bodi I et al (2006) Interlaboratory comparison of assessments of Alzheimer disease-related lesions: a study of the BrainNet Europe Consortium. J Neuropathol Exp Neurol 65:740–757. https://doi.org/10.1097/01.jnen.0000229986.17548.27
Aranda MP, Kremer IN, Hinton L, Zissimopoulos J, Whitmer RA, Hummel CH et al (2021) Impact of dementia: health disparities, population trends, care interventions, and economic costs. J Am Geriatr Soc 69:1774–1783. https://doi.org/10.1111/jgs.17345
Arnold SE, Vega IE, Karlawish JH, Wolk DA, Nunez J, Negron M et al (2013) Frequency and clinicopathological characteristics of presenilin 1 Gly206Ala mutation in Puerto Rican Hispanics with dementia. J Alzheimers Dis 33:1089–1095. https://doi.org/10.3233/JAD-2012-121570
Association As (2022) 2022 Alzheimer's disease facts and figures https://www.alz.org/alzheimers-dementia/facts-figures. Accessed 18 Aug 2022
Association As (2023) 2023 Alzheimer's disease facts and figures https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf. Accessed 17 Apr 2023
Athan ES, Williamson J, Ciappa A, Santana V, Romas SN, Lee JH et al (2001) A founder mutation in presenilin 1 causing early-onset Alzheimer disease in unrelated Caribbean Hispanic families. JAMA 286:2257–2263. https://doi.org/10.1001/jama.286.18.2257
Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT (2017) Structural racism and health inequities in the USA: evidence and interventions. Lancet 389:1453–1463. https://doi.org/10.1016/S0140-6736(17)30569-X
Balls-Berry JJE, Babulal GM (2022) Health disparities in Dementia. Continuum (Minneap Minn) 28:872–884. https://doi.org/10.1212/CON.0000000000001088
Baxi V, Edwards R, Montalto M, Saha S (2022) Digital pathology and artificial intelligence in translational medicine and clinical practice. Mod Pathol 35:23–32. https://doi.org/10.1038/s41379-021-00919-2
Besser LM et al (2018) The revised National Alzheimer's Coordinating Center's neuropathology form-available data and new analyses. J Neuropathol Exp Neurol 77(8):717–726. https://doi.org/10.1093/jnen/nly049
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82(4):239–259. https://doi.org/10.1007/bf00308809
Breitkopf CR (2009) Attitudes, beliefs and behaviors surrounding organ donation among Hispanic women. Curr Opin Organ Trans. 14:191–195
Bureau USC (2021) Race and Ethnicity in the United States: 2010 Census and 2020 Census https://www.census.gov/library/visualizations/interactive/race-and-ethnicity-in-the-united-state-2010-and-2020-census.html. Accessed 11/21/2022
Burns A, Iliffe S (2009) Dementia. BMJ 338: 75 Doi https://doi.org/10.1136/bmj.b75
Chin AL, Negash S, Hamilton R (2011) Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer disease. Alzheimer Dis Assoc Disord 25:187–195. https://doi.org/10.1097/WAD.0b013e318211c6c9
Cicognola C, Brinkmalm G, Wahlgren J, Portelius E, Gobom J, Cullen NC et al (2019) Novel tau fragments in cerebrospinal fluid: relation to tangle pathology and cognitive decline in Alzheimer’s disease. Acta Neuropathol 137:279–296. https://doi.org/10.1007/s00401-018-1948-2
Dugger BN, Dickson DW (2017) Pathology of neurodegenerative diseases. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a028035
Ennis SR, Ríos-Vargas M, Albert NG (2011) The hispanic population: 2010. US Department of Commerce, Economics and Statistics Administration, US Census Bureau
Epstein-Lubow G (2013) The national Alzheimer’s project act and the national plan to address Alzheimer’s disease: an update and future directions. Am J Geriatr Psychiatry 21:S36–S37. https://doi.org/10.1016/j.jagp.2012.12.075
Farfel JM, Nitrini R, Suemoto CK, Grinberg LT, Ferretti RE, Leite RE et al (2013) Very low levels of education and cognitive reserve: a clinicopathologic study. Neurology 81:650–657. https://doi.org/10.1212/WNL.0b013e3182a08f1b
Figueroa R, Steenland K, MacNeil JR, Levey AI, Vega IE (2008) Geographical differences in the occurrence of Alzheimer’s disease mortality: United States versus Puerto Rico. Am J Alzheimers Dis Other Demen 23:462–469. https://doi.org/10.1177/1533317508321909
Filshtein TJ, Dugger BN, Jin LW, Olichney JM, Farias ST, Carvajal-Carmona L et al (2019) Neuropathological diagnoses of demented Hispanic, black, and non-Hispanic white decedents seen at an Alzheimer’s disease Center. J Alzheimers Dis 68:145–158. https://doi.org/10.3233/JAD-180992
Flanagin A, Frey T, Christiansen SL, Committee AMAMoS (2021) Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA 326:621–627. https://doi.org/10.1001/jama.2021.13304
Gavett BE, Fletcher E, Harvey D, Farias ST, Olichney J, Beckett L et al (2018) Ethnoracial differences in brain structure change and cognitive change. Neuropsychology 32:529–540. https://doi.org/10.1037/neu0000452
Gavrielides MA, Ronnett BM, Vang R, Barak S, Lee E, Staats PN et al (2021) Pathologist concordance for ovarian carcinoma subtype classification and identification of relevant histologic features using microscope and whole slide imaging. Arch Pathol Lab Med 145:1516–1525. https://doi.org/10.5858/arpa.2020-0579-OA
Glymour MM, Manly JJ (2008) Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychol Rev 18:223–254. https://doi.org/10.1007/s11065-008-9064-z
Graff-Radford NR, Besser LM, Crook JE, Kukull WA, Dickson DW (2016) Neuropathologic differences by race from the national Alzheimer’s coordinating center. Alzheimers Dement 12:669–677. https://doi.org/10.1016/j.jalz.2016.03.004
Guillozet AL, Weintraub S, Mash DC, Mesulam MM (2003) Neurofibrillary tangles, amyloid, and memory in aging and mild cognitive impairment. Arch Neurol 60:729–736. https://doi.org/10.1001/archneur.60.5.729
Halliday G, Ng T, Rodriguez M, Harding A, Blumbergs P, Evans W et al (2002) Consensus neuropathological diagnosis of common dementia syndromes: testing and standardising the use of multiple diagnostic criteria. Acta Neuropathol 104:72–78. https://doi.org/10.1007/s00401-002-0529-5
Hayes-Larson E, Mobley TM, Gilmore-Bykovskyi A, Shaw C, Karlamangla A, Manly JJ et al (2021) Racial/Ethnic differences in health-related quality of life in persons with and without dementia. J Am Geriatr Soc 69:629–636. https://doi.org/10.1111/jgs.16908
Hill CV, Perez-Stable EJ, Anderson NA, Bernard MA (2015) The national institute on aging health disparities research framework. Ethn Dis 25:245–254. https://doi.org/10.18865/ed.25.3.245
Hogervorst E, Barnetson L, Jobst KA, Nagy Z, Combrinck M, Smith AD (2000) Diagnosing dementia: interrater reliability assessment and accuracy of the NINCDS/ADRDA criteria versus CERAD histopathological criteria for Alzheimer’s disease. Dement Geriatr Cogn Disord 11:107–113. https://doi.org/10.1159/000017222
Hyman BT, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Carrillo MC et al (2012) National institute on aging-Alzheimer’s association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement 8:1–13. https://doi.org/10.1016/j.jalz.2011.10.007
Ighodaro ET, Nelson PT, Kukull WA, Schmitt FA, Abner EL, Caban-Holt A et al (2017) Challenges and considerations related to studying dementia in blacks/African Americans. J Alzheimers Dis 60:1–10. https://doi.org/10.3233/JAD-170242
Jo T, Nho K, Saykin AJ (2019) Deep learning in alzheimer’s disease: diagnostic classification and prognostic prediction using neuroimaging data. Front Aging Neurosci 11:220. https://doi.org/10.3389/fnagi.2019.00220
Kapasi A, DeCarli C, Schneider JA (2017) Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol 134:171–186. https://doi.org/10.1007/s00401-017-1717-7
Khachaturian ZS, Khachaturian AS, Thies W (2012) The draft “National Plan” to address Alzheimer’s disease - National Alzheimer’s Project Act (NAPA). Alzheimers Dement 8:234–236. https://doi.org/10.1016/j.jalz.2012.04.004
Livney MG, Clark CM, Karlawish JH, Cartmell S, Negron M, Nunez J et al (2011) Ethnoracial differences in the clinical characteristics of Alzheimer’s disease at initial presentation at an urban Alzheimer’s disease center. Am J Geriatr Psychiatry 19:430–439. https://doi.org/10.1097/JGP.0b013e3181f7d881
Malpetti M, Kievit RA, Passamonti L, Jones PS, Tsvetanov KA, Rittman T et al (2020) Microglial activation and tau burden predict cognitive decline in Alzheimer’s disease. Brain 143:1588–1602. https://doi.org/10.1093/brain/awaa088
Matthews KA, Xu W, Gaglioti AH, Holt JB, Croft JB, Mack D et al (2019) Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged >/=65 years. Alzheimers Dement 15:17–24. https://doi.org/10.1016/j.jalz.2018.06.3063
Mehta KM, Simonsick EM, Rooks R, Newman AB, Pope SK, Rubin SM et al (2004) Black and white differences in cognitive function test scores: what explains the difference? J Am Geriatr Soc 52:2120–2127. https://doi.org/10.1111/j.1532-5415.2004.52575.x
Mehta KM, Yeo GW (2017) Systematic review of dementia prevalence and incidence in United States race/ethnic populations. Alzheimers Dement 13:72–83. https://doi.org/10.1016/j.jalz.2016.06.2360
Mirra SS, Gearing M, McKeel DW Jr, Crain BJ, Hughes JP, van Belle G et al (1994) Interlaboratory comparison of neuropathology assessments in Alzheimer’s disease: a study of the Consortium to establish a registry for Alzheimer’s Disease (CERAD). J Neuropathol Exp Neurol 53:303–315
Mirra SS, Heyman A, McKeel D, Sumi S, Crain BJ, Brownlee L et al (1991) The consortium to establish a registry for Alzheimer’s Disease (CERAD): Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41:479–479
Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ (2002) Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved 13:477–503. https://doi.org/10.1177/104920802237532
Morlett Paredes A, Guarena LA, Stickel AM, Schairer CE, Gonzalez HM (2022) To donate, or not to donate, that is the question: Latino insights into brain donation. Alzheimers Dement. https://doi.org/10.1002/alz.12755
Morris JC, Weintraub S, Chui HC, Cummings J, Decarli C, Ferris S et al (2006) The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer Disease Centers. Alzheimer Dis Assoc Disord 20:210–216. https://doi.org/10.1097/01.wad.0000213865.09806.92
Murray ME, Cannon A, Graff-Radford NR, Liesinger AM, Rutherford NJ, Ross OA et al (2014) Differential clinicopathologic and genetic features of late-onset amnestic dementias. Acta Neuropathol 128:411–421. https://doi.org/10.1007/s00401-014-1302-2
Murray ME, Graff-Radford NR, Ross OA, Petersen RC, Duara R, Dickson DW (2011) Neuropathologically defined subtypes of Alzheimer’s disease with distinct clinical characteristics: a retrospective study. Lancet Neurol 10:785–796. https://doi.org/10.1016/S1474-4422(11)70156-9
Nagy Z, Vatter-Bittner B, Braak H, Braak E, Yilmazer DM, Schultz C et al (1997) Staging of Alzheimer-type pathology: an interrater-intrarater study. Dement Geriatr Cogn Disord 8:248–251. https://doi.org/10.1159/000106639
Nelson PT, Alafuzoff I, Bigio EH, Bouras C, Braak H, Cairns NJ et al (2012) Correlation of Alzheimer disease neuropathologic changes with cognitive status: a review of the literature. J Neuropathol Exp Neurol 71:362–381. https://doi.org/10.1097/NEN.0b013e31825018f7
Nelson PT, Braak H, Markesbery WR (2009) Neuropathology and cognitive impairment in Alzheimer disease: a complex but coherent relationship. J Neuropathol Exp Neurol 68:1–14. https://doi.org/10.1097/NEN.0b013e3181919a48
Nguyen ML, Huie EZ, Whitmer RA, George KM, Dugger BN (2022) Neuropathology studies of Dementia in US persons other than Non-Hispanic whites. Free Neuropathol. https://doi.org/10.17879/freeneuropathology-2022-3795
Olarte L, Schupf N, Lee JH, Tang MX, Santana V, Williamson J et al (2006) Apolipoprotein E epsilon4 and age at onset of sporadic and familial Alzheimer disease in Caribbean Hispanics. Arch Neurol 63:1586–1590. https://doi.org/10.1001/archneur.63.11.1586
Oliveira LC, Lai Z, Harvey D, Nzenkue K, Jin LW, Decarli C et al (2023) Preanalytic variable effects on segmentation and quantification machine learning algorithms for amyloid-beta analyses on digitized human brain slides. J Neuropathol Exp Neurol. https://doi.org/10.1093/jnen/nlac132
Organization W-WH (2022) Global action plan on the public health response to dementia 2017–2025. WHO, City
Proctor BD, Semega JL, Kollar MA (2016) Income and poverty in the United States: 2015. US census bureau, current population reports 14:
Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA (2021) Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimers Dement 17:1966–1975. https://doi.org/10.1002/alz.12362
Review WP (2023) Hispanic Population by State https://worldpopulationreview.com/state-rankings/hispanic-population-by-state. Accessed 01/27/2023
Santos OA, Pedraza O, Lucas JA, Duara R, Greig-Custo MT, Hanna Al-Shaikh FS et al (2019) Ethnoracial differences in Alzheimer’s disease from the FLorida Autopsied Multi-Ethnic (FLAME) cohort. Alzheimers Dement 15:635–643. https://doi.org/10.1016/j.jalz.2018.12.013
Scalco R, Hamsafar Y, White CL, Schneider JA, Reichard RR, Prokop S et al (2023) The status of digital pathology and associated infrastructure within Alzheimer’s disease Centers. J Neuropathol Exp Neurol. https://doi.org/10.1093/jnen/nlac127
Schmitt M, Maron RC, Hekler A, Stenzinger A, Hauschild A, Weichenthal M et al (2021) Hidden variables in deep learning digital pathology and their potential to cause batch effects: prediction model study. J Med Internet Res 23:e23436. https://doi.org/10.2196/23436
Shakir MN, Dugger BN (2022) Advances in deep neuropathological phenotyping of Alzheimer disease: past, present, and future. J Neuropathol Exp Neurol 81:2–15. https://doi.org/10.1093/jnen/nlab122
Signaevsky M, Prastawa M, Farrell K, Tabish N, Baldwin E, Han N et al (2019) Artificial intelligence in neuropathology: deep learning-based assessment of Tauopathy. Lab Invest 99:1019–1029. https://doi.org/10.1038/s41374-019-0202-4
Soria JA, Huisa BN, Edland SD, Litvan I, Peavy GM, Salmon DP et al (2018) Clinical-neuropathological correlations of Alzheimer’s disease and related dementias in latino volunteers. J Alzheimers Dis 66:1539–1548. https://doi.org/10.3233/JAD-180789
Steenland K, Goldstein FC, Levey A, Wharton W (2016) A meta-analysis of Alzheimer’s disease incidence and prevalence comparing African-Americans and Caucasians. J Alzheimers Dis 50:71–76. https://doi.org/10.3233/JAD-150778
Tang MX, Cross P, Andrews H, Jacobs DM, Small S, Bell K et al (2001) Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology 56:49–56. https://doi.org/10.1212/wnl.56.1.49
Thal DR, Rub U, Orantes M, Braak H (2002) Phases of A beta-deposition in the human brain and its relevance for the development of AD. Neurology 58:1791–1800
Vega IE, Cabrera LY, Wygant CM, Velez-Ortiz D, Counts SE (2017) Alzheimer’s disease in the latino community: intersection of genetics and social determinants of health. J Alzheimers Dis 58:979–992. https://doi.org/10.3233/JAD-161261
Vizcarra JC, Teich A, Dugger B, Gutman D (2023) Survey of neuroanatomic sampling and staining procedures in Alzheimer disease research center brain banks. Free Neuropathol 4:6–6
Wang Y, Mandelkow E (2016) Tau in physiology and pathology. Nat Rev Neurosci 17:5–21. https://doi.org/10.1038/nrn.2015.1
Weissberger GH, Gollan TH, Bondi MW, Nation DA, Hansen LA, Galasko D et al (2019) Neuropsychological deficit profiles, vascular risk factors, and neuropathological findings in Hispanic older adults with autopsy-confirmed Alzheimer’s disease. J Alzheimers Dis 67:291–302. https://doi.org/10.3233/JAD-180351
Wong DR, Tang Z, Mew NC, Das S, Athey J, McAleese KE et al (2022) Deep learning from multiple experts improves identification of amyloid neuropathologies. Acta Neuropathol Commun 10:66. https://doi.org/10.1186/s40478-022-01365-0
Yearby R (2020) Structural racism and health disparities: reconfiguring the social determinants of health framework to include the root cause. J Law Med Ethics 48:518–526. https://doi.org/10.1177/1073110520958876
Yearby R, Clark B, Figueroa JF (2022) Structural racism in historical and modern US health care policy. Health Aff (Millwood) 41:187–194. https://doi.org/10.1377/hlthaff.2021.01466
Acknowledgements
The authors thank the families and participants of the University of California Davis, University of California San Diego, and Columbia University Alzheimer’s Disease Research Centers (ADRC) for their generous donations as well as ADRC staff and faculty for their contributions. This project was made possible by grants from the National Institute on Aging (NIA) of the National Institutes of Health (NIH) under Award Numbers R01AG062517, P30AG072972, P30AG062429, P50AG008702, P30AG066462. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any public health agency or of the US government.
Funding
This project was primarily made possible by grants from the National Institute on Aging (NIA) of the National Institutes of Health (NIH) under Award Numbers R01AG062517, P30AG072972, P30AG062429, P50AG008702, P30AG066462.
Author information
Authors and Affiliations
Contributions
All authors provided critical review of the manuscript. RS: Writing, original draft and figure preparation; BD, LB: Study conceptualization and methodology design/development; EH, MN, HW, DF, LH: data curation and quality control; NS and LB: statistical analyses and write up, and table creation; AT, RR, CD, LH, LJ: provided data; BD: neuropathology analyses and obtaining primary project funding. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
This project was primarily made possible by grants from the National Institute on Aging (NIA) of the National Institutes of Health (NIH) under Award Numbers R01AG062517, P30AG072972, P30AG062429, P50AG008702, P30AG066462. BND: receives funding by grants from the National Institute on Aging (NIA) of the National Institutes of Health (NIH) under Award Numbers P30AG072972, U01AG061357-S1, R01AG052132, R01AG056519, and R01AG062517. She serves on the external advisory board for the Alzheimer’s Disease Center at USC, and as a committee member for the ADRC neuropathology committee and the College of American Pathologists Neuropathology committee. She has no conflicts of interest to declare related to this project. LB: has received support over the last 48 months from payments to her institution from U01AG024904 (Dr. Weiner, UCSF/NCIRE), R01AG062517 (Dr. Dugger), B639943 (Dr. Coleman), and the National Institute of Justice 2014-R2-CX-0012 (Dr. Wintemute). She has served on the external advisory boards for Alzheimer’s Disease Centers at UCSD, Washington University, University of Pittsburgh, and Data and Safety Monitoring Boards for NIH-funded clinical trials (UCSF), and as an external advisory board member for the LEADS study, all paid directly to her. She has no other support or conflicts of interest to declare. RR has received support from AG058252, AG073979, AG051848 to RAR and biomarker. Other authors report no conflicts of interest relevant to this project.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Tables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Scalco, R., Saito, N., Beckett, L. et al. The neuropathological landscape of Hispanic and non-Hispanic White decedents with Alzheimer disease. acta neuropathol commun 11, 105 (2023). https://doi.org/10.1186/s40478-023-01574-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-023-01574-1