Abstract
Background
Continuous positive airway pressure (CPAP) therapy is the first-line treatment for obstructive sleep apnea (OSA). However, the low acceptance rate of CPAP remains a challenging clinical issue. This study aimed to determine the factors that influence the acceptance rate of CPAP.
Methods
This retrospective cohort study was conducted at the sleep center of Shuang-Ho Hospital. Initially, 1186 OSA patients who received CPAP therapy between December 2013 and December 2017 were selected, and finally, 1016 patients were analyzed. All patients with OSA received CPAP therapy for at least 1 week, and their acceptance to treatment was subsequently recorded. Outcome measures included patients’ demographic and clinical characteristics (sex, age, BMI, comorbidities, history of smoking, and the medical specialist who prescribed CPAP treatment), polysomnography (PSG) results, and OSA surgical records.
Results
Patients with a lower CPAP acceptance rate were referred from otolaryngologists (acceptance rate of otolaryngology vs. others: 49.6% vs. 56.6%, p = .015), in addition to having a lower apnea–hypopnea index (AHI) (acceptance vs. non-acceptance: 55.83 vs. 40.79, p = .003), rapid eye movement AHI (REM-AHI) (acceptance vs. non-acceptance: 51.21 vs. 44.92, p = .014), and arousal index (acceptance vs. non-acceptance: 36.80 vs. 28.75, p = .011). The multiple logistic regression model showed that patients referred from otolaryngology had a lower CPAP acceptance rate (odds ratio 0.707, p = .0216) even after adjusting for age, sex, BMI, AHI, REM-AHI, arousal index, comorbidities, and smoking status.
Conclusions
Before their initial consultation, patients may already have their preferred treatment of choice, which is strongly linked to the type of medical specialists they visit, and consequently, affects their rate of acceptance to CPAP therapy. Therefore, physicians should provide personalized care to patients by exploring and abiding by their preferred treatment choices.
Similar content being viewed by others
Background
Obstructive sleep apnea (OSA) is a chronic condition caused by the episodic collapse and obstruction of the upper airway during sleep. The prevalence of OSA syndrome ranges from 3 to 7% among adult men and 2–5% among adult women in the general population [1]. Among OSA patients in the United States, 17% of men and 9% of women are 50‒70 years of age [2]. OSA patients have a higher risk of daytime sleepiness; cardiovascular, neurovascular, and metabolic disturbances; motor vehicle accidents; and decreased psychomotor speed [3,4,5,6,7,8]; however, many of them remain undiagnosed [9].
Several treatment options are available, including lifestyle changes [10, 11], oral appliance [12], pharmacological treatment [13], surgical treatment [14, 15], and continuous positive airway pressure (CPAP) therapy. CPAP therapy can prevent upper airway collapse and is the first-line treatment for OSA owing to its immediate effects and relatively lower complication rates [16,17,18]. CPAP reduces daytime sleepiness [19,20,21,22], has beneficial effects in cardiovascular and metabolic diseases [23,24,25,26,27,28], and improves health-related quality of life, mood, and neurocognitive function, especially in subgroups with higher treatment adherence [19, 29].
The efficacy of CPAP therapy is correlated with patients’ adherence [30, 31]. Nevertheless, low acceptance and adherence to CPAP therapy remain challenging issues in clinical practice. According to Yang et al. and Simon-Tuval et al., the acceptance rate of CPAP is approximately 40% [32, 33]. CPAP adherence is often defined as using the therapy for an average of 4 h per night for at least 70% of the nights monitored [34]. Studies have shown that 46–83% of patients are non-adherent to treatment [35, 36]. Further, a systematic review of 82 studies found that CPAP non-adherence affects at least one-third of treated patients and showed that CPAP adherence did not significantly improve in the past 20 years despite efforts in behavioral intervention and patient coaching [37].
Many studies have focused on CPAP adherence and its correlated factors, and have shown inconsistent results with factors including age, sex, race, severity of OSA, severity of symptoms, smoking status, and socioeconomic status [38,39,40,41,42,43,44,45,46]. However, only a few studies have mentioned factors related to CPAP acceptance [32, 33, 47], and the specialties of doctors who prescribe CPAP treatment are rarely discussed. Achieving shared decision-making depends on building good relationships in clinical encounters, so it is important for physicians to understand patients and share information. Therefore, we aimed to investigate and analyze the factors that cause a lower acceptance rate of CPAP in patients with OSA.
Methods
Data collection and sample
This retrospective cohort study initially included 1186 OSA patients treated with CPAP at least 1 week at Shuang-Ho Hospital (New Taipei City, Taiwan) between December 2013 and December 2017. Patients with symptoms of OSA underwent polysomnography (PSG) at Shuang-Ho Hospital, and those diagnosed with OSA were referred to the hospital’s sleep center for CPAP treatment. Apart from otolaryngology, other outpatient departments, including pulmonology, cardiology, neurology, and psychiatry, also referred patients with OSA to the sleep center, and each patient received CPAP treatment for at least 1 week. In addition, patients were instructed on how to use the CPAP device correctly and followed up continuously for at least 3 months via telephone or mobile communication software by the sleep case manager of the sleep center to ensure adherence to the treatment regimen was achieved.
Eligibility criteria included patients aged 20 years or older, a record of CPAP use, and a diagnosis of OSA, which is defined as having an apnea–hypopnea index (AHI) of at least 5, based on the PSG records. Patients were excluded from the study if they were younger than 20 years of age, had an AHI of less than 5, had missing data on PSG records, or were referred from departments with fewer than 10 patient referrals to the sleep center.
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Taipei Medical University (IRB Number: N202201092, 2022/4/14 of approval).
Assessment of baseline demographic and clinical characteristics
Patients’ medical history and clinical characteristics were comprehensively reviewed through their admission, outpatient, and surgical records, including their demographic characteristics (age, sex, and BMI), specialties of their referral doctors, smoking status, and presence of baseline comorbidities, including hypertension (HTN), diabetes mellitus (DM), cardiovascular disease (CVD), chronic kidney disease (CKD), hyperlipidemia (HLD), and chronic obstructive pulmonary disease (COPD). Cardiovascular disease was defined as a coronary artery disease or cerebrovascular accident. For patients who did not receive CPAP therapy, we tracked whether they had undergone OSA-related surgeries. OSA-related surgery was defined as uvulopalatopharyngoplasty (UPPP), uvulopalatal flap surgery (UPF), laser-assisted uvulopalatoplasty (LAUP), pharyngoplasty, tonsillectomy, adenoidectomy, septoplasty, submucosal resection of the nose, and submucosal turbinectomy.
Assessment of polysomnography results
PSG was conducted by certified respiratory therapists with at least 1 year of clinical experience. Standard monitoring devices included electroencephalography (EEG), electrooculography (EOG), electrocardiography (ECG), and electromyography (EMG) placed on the chin and bilateral anterior tibialis; position sensors, snore sensors, pulse oximetry, and thermistors to sense nasal and oral airflow; and plethysmography to sense thoracoabdominal movements.
PSG reports included the Epworth Sleepiness Scale (ESS) score, Pittsburgh Sleep Quality Index (PSQI), apnea–hypopnea index (AHI), rapid eye movement AHI (REM-AHI), non-rapid eye movement apnea–hypopnea index (NREM-AHI), sleep efficiency, mean oxygen saturation (mean SAT), mean heart rate (mean HR), arousal index, periodic limb movement index (PLMI), and pressure settings of the CPAP machine (90% pressure).
AHI was calculated as the number of apnea and hypopnea events per hour during sleep. REM-AHI was defined as the AHI during the rapid eye movement period. Sleep efficiency was defined as the ratio of the total sleep time to the total recording time. The 90% pressure was adjusted to eliminate 95% of apneas, hypopneas, and snoring to achieve an oxygen saturation of > 90% and AHI < 5 events/h in patients during REM sleep in a supine position.
Acceptance and non-acceptance
All enrolled patients commenced CPAP therapy for at least 1 week as a test trial. Patients who purchased the CPAP machine were defined as the acceptance group, and those who did not were placed in the non-acceptance group. For those who accepted CPAP, we further documented the date of purchase and for those who did not accept, we recorded the date they returned the CPAP device.
Statistical analyses
Continuous data were presented as mean ± standard deviation (SD) and tested by independent t test. Categorical data were presented as N (%) and tested by Chi-square test or Fisher's exact test. We further performed multivariate logistic regression to evaluate associations between factors chosen by this study and CPAP acceptance. Odds ratio (OR) and 95% confidence intervals (CI) were also calculated. Three models were established. Model 1 was adjusted by age, gender, and BMI. Model 2 was adjusted by covariates in Model 1, plus AHI, REM-AHI, and Arousal Index. Model 3 was adjusted by covariates in Model 2, plus HTN, DM, CVD, HLD, CKD, COPD, and smoking status. P value lower than 0.05 was regarded as statistically significant. Data were analyzed using SAS version 9.4 software (SAS Inc., Cary, NC, USA).
Results
Characteristics of the participants
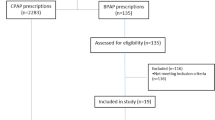
A total of 1016 patients consisting of 825 men (81.2%) and 191 women (18.8%), mean age of 50.7 years, were enrolled for analysis (Fig. 1). A total of 546 (53.7%) patients accepted CPAP, and the baseline demographic and clinical characteristics of the acceptance group versus the non-acceptance group are shown in Table 1. We found that patients in the non-acceptance group were older (51.62 vs. 49.84, p = 0.031) and had lower body mass index (BMI) (28.54 vs. 29.33, p = 0.011). However, there were no significant differences in the baseline comorbidities between the two groups. Notably, the acceptance rate of CPAP therapy in patients referred by otolaryngologists was 49.6%, which was the lowest among all medical specialties who referred patients for CPAP treatment.
The overnight PSG results of the acceptance and non-acceptance groups are shown in Table 2. Multivariable analysis revealed that the non-acceptance group had a lower AHI (40.79 vs. 55.83, p = 0.003), REM-AHI (44.92 vs. 51.21, p = 0.014), and arousal index (28.75 vs. 36.80, p = 0.011).
Based on our results, the acceptance rate of CPAP therapy seemed to strongly correlate with the medical specialty that referred the patients for treatment. Hence, we performed a logistic model analysis to calculate the OR of otolaryngology patients who accepted CPAP (Table 3). In Model one, we adjusted the variables for baseline characteristics (sex, age, BMI). Model two was adjusted based on model one with the addition of PSG-related variables that significantly correlated with CPAP acceptance (AHI, REM-AHI, and arousal index). Model three was adjusted according to model two plus smoking status and presence of comorbidities (HTN, DM, CVD, HLD, CKD, and COPD). The OR was 0.707 (p = 0.0216, CI 0.526–0.950), which indicated that the odds of otolaryngology patients accepting CPAP treatment were significantly lower than those of non-otolaryngology patients, even after adjusting for all the factors above.
Analysis of otolaryngology versus other departments
Since patients referred from otolaryngology had a lower CPAP acceptance rate, we aimed to further analyze the differences between these patients and those referred from other medical specialties. The baseline demographic and clinical characteristics are shown in Table 4. We found that patients from the otolaryngology department were younger (46.97 vs. 53.22, p < 0.001), had lower BMI (28.49 vs. 29.29, p = 0.012), were more likely to be male (84.6% vs. 78.9%, p = 0.022), and had fewer smokers (24.8% vs. 35.4%, p < 0.001). Compared with other medical specialties, patients referred from otolaryngology also had significantly less comorbidities such as hypertension (30.4 vs. 55.6%, p < 0.001), diabetes mellitus (12.3% vs. 20.5%, p < 0.001), cardiovascular diseases (11.8% vs. 28.1%, p < 0.001), hyperlipidemia (21.9% vs. 34.4%, p < 0.001), and chronic obstructive pulmonary disease (1.2% vs. 10.1%, p < 0.001).
The overnight PSG results of patients referred from otolaryngology versus patients referred from other specialties are shown in Table 5. We observed that patients referred from otolaryngology exhibited no significant difference in OSA severity compared to patients referred by other specialties, including variables that determine CPAP acceptance, such as AHI (p = 0.299), REM-AHI (p = 0.855), and arousal index (p = 0.080).
From the analysis of the population accepting CPAP, it was found that patients referred by the otolaryngology department had a higher proportion of seeking surgical intervention compared to other departments. This difference is statistically significant, with percentages of 19.2% versus 7.5%, respectively (p < 0.001).
We further analyzed whether patients underwent OSA surgery after refusing CPAP therapy and discovered that a higher ratio of patients from otolaryngology underwent OSA surgery (20.6% vs. 6.5%, p < 0.001, Fig. 2). Subsequently, we combined the data of patients who underwent CPAP or OSA surgery as receiving treatment for OSA and found no significant difference between the two groups (Fig. 2).
According to the baseline demographic characteristics and PSG results of the patients who underwent OSA surgery, there was no significant difference between the groups (Table 6).
Discussion
The present study showed that OSA patients with lower CPAP acceptance tend to be referred to the sleep center by otolaryngologists and had milder OSA severity (specifically lower AHI, REM-AHI, and arousal index), lower BMI, and older age. After excluding patients who initially visited the otolaryngology department, we found that patients from other specialties exhibited similar trends to the original data (Additional file 1: Table S1 and Table S2).
A total of 53.7% (546/1016) of patients accepted CPAP in the present study, which was substantially higher compared to the 40.1% in Simon et al. (n = 162, mean age 54.9 y/o) and 39.7% in Yang et al. (n = 315, mean age 56.7 y/o). This may be attributed to the younger age (50.7 y/o) of our cohort. Furthermore, instructions and assistance were provided to patients by the case manager of the sleep center via a mobile communication software on the correct use of the device in order to maximize their acceptance of CPAP treatment.
Previous studies have consistently demonstrated that greater OSA severity is associated with higher CPAP adherence [33, 38, 39, 42,43,44, 46, 48]. However, demographic characteristics, including sex, age, BMI, comorbidities, and smoking, showed inconsistent results [45]. In addition, we found that BMI and age significantly influenced acceptance of CPAP. Several studies have shown that higher ESS scores and more severe OSA symptoms are associated with higher CPAP adherence [33, 39,40,41, 44, 46]. Our results displayed similar trends but without statistical significance. Moreover, it is noteworthy that comorbidities and PLMI, which have not been discussed in previous studies, did not appear to be significant predictors of acceptance of CPAP.
We further compared the demographic and clinical characteristics of patients referred by otolaryngologists with those of patients referred from other specialties. Patients referred from otolaryngology had a lower BMI, fewer comorbidities, fewer smokers, and more young men; however, the PSG results were similar between the two groups (Tables 4, 5). According to previous studies, OSA severity is highly correlated with CPAP acceptance [33, 38, 39, 42,43,44, 46, 48]. Nevertheless, our study showed that otolaryngology patients had a lower acceptance of CPAP but demonstrated the same OSA severity as patients from other specialties (Table 5).
Similar to our results, Salas et al. showed that patients referred from otolaryngology had fewer comorbidities, lower BMI, and younger age, except for having the same OSA severity as other specialties [49]. Furthermore, after adjusting for multiple variables that may affect the CPAP acceptance rate, such as age, BMI, AHI, REM-AHI, and arousal index, the OR of CPAP acceptance in patients from otolaryngology was still significantly lower than that in patients from other departments (OR = 0.707, p = 0.0216, Table 3).
Three possible reasons may explain the disparity in patients’ choice of medical specialties for the treatment of OSA: the intention for surgery, surgical risks involved, and knowledge about the treatment.
First, our study showed that patients from otolaryngology who did not accept CPAP showed higher incidences of undergoing surgery afterwards than non-otolaryngology OSA patients (20.6% vs. 6.5%, p < 0.001, Fig. 2). Furthermore, we analyzed the ratio of OSA-related treatments, including CPAP or OSA surgery, and found no significant difference between patients from otolaryngology and those from other departments (p = 0.848, Fig. 2). This may indicate that both groups shared a similar intent for treatment, and a substantial portion of otolaryngology patients who refused CPAP treatment may have undergone surgery. In addition, we analyzed the AHI of the patients who underwent surgery and found no significant difference between the groups (p = 0.308, Table 6). This demonstrates that the two groups had similar indications for OSA surgery. In summary, patients’ intention to undergo surgery may contribute to their preference for otolaryngology clinics when seeking treatment for OSA. Second, our results were consistent with those of Salas et al., which showed that patients from otolaryngology had a lower risk of general anesthesia and surgical treatment [49]. Hence, we infer that patients’ surgical risks may affect their preference for specialties when they seek treatment. Third, previous studies showed that patients’ knowledge and beliefs about the disease affected their adherence to treatment [36, 50, 51]. Gulati et al. [52] pointed out that patients receiving surgery for OSA, compared to those who did not, had a higher ratio of independently doing research for OSA treatment prior to their consultation with the surgeon. This would explain why patients’ knowledge about the variety of treatment options plays a crucial role in their adherence and decision-making, which may also determine their choice of medical specialties.
Patients who visit different departments may have different treatment preferences for OSA. According to the principle of shared decision making [53, 54], increasing patient participation in discussions on treatment options may provide a better therapeutic effect.
Our study has several advantages. First, to the best of our knowledge, this is the first study to investigate the rate of acceptance of CPAP in patients referred by different specialties. Second, our sample size was relatively large (n = 1016) compared to previous studies. Third, we selected a more stringent definition of CPAP acceptance in our study, where “Acceptance” was defined as patients who purchased CPAP machines after their test trial, which is also the same definition adopted by Yang and Simon-Tuval [32, 33]. Compared to Rauscher et al., which only had a 3-day CPAP test trial [47], our definition of CPAP acceptance may better reflect the patients’ actual intent.
This study has several limitations. First, this was a retrospective cohort study; therefore, potential participants were excluded because of missing data, and the baseline data of the otolaryngology versus non-otolaryngology groups may be different. Second, few patients were referred from certain medical specialties. For example, patients from the Department of Psychiatry had a higher acceptance of CPAP compared to other specialties; however, no statistical significance was noted. Lastly, some patients in the non-acceptance group may purchase CPAP via alternative routes; as a result, this may have caused a selection bias. In order to minimize this bias, the medical records of the non-acceptance group were carefully examined during their subsequent visits to the hospital to ensure that no CPAP treatment had been initiated. Moreover, patients from the non-acceptance group were constantly followed up by the case manager of the sleep center regarding their subsequent treatment for OSA, and whether they received treatment elsewhere or if they were using other respiratory devices.
Conclusions
Shared decision making is crucial for achieving therapeutic success in clinical practice. In the sleep center, patients with OSA who initially visited otolaryngology clinics had a lower acceptance rate for CPAP. Therefore, besides adhering to clinical guidelines, physicians should provide individualized care through shared decision-making and identifying patients’ preferred treatment.
Availability of data and materials
The datasets analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AHI:
-
Apnea–hypopnea index
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- CKD:
-
Chronic kidney disease
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- ECG:
-
Electrocardiography
- EEG:
-
Electroencephalography
- EMG:
-
Electromyography
- EOG:
-
Electrooculography
- ESS:
-
Epworth sleepiness scale
- HLD:
-
Hyperlipidemia
- HR:
-
Heart rate
- HTN:
-
Hypertension
- IRB:
-
Institutional Review Board
- LAUP:
-
Laser-assisted uvulopalatoplasty
- NREM-AHI:
-
Non-rapid eye movement apnea–hypopnea index
- OR:
-
Odds ratio
- OSA:
-
Obstructive sleep apnea
- PLMI:
-
Periodic limb movement index
- PSG:
-
Polysomnography
- PSQI:
-
Pittsburgh Sleep Quality Index
- REM-AHI:
-
Rapid eye movement AHI
- SAT:
-
Saturation
- SD:
-
Standard deviation
- UPF:
-
Uvulopalatal flap surgery
- UPPP:
-
Uvulopalatopharyngoplasty
References
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–43.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–14.
Veasey SC, Rosen IM. Obstructive sleep apnea in adults. N Engl J Med. 2019;380(15):1442–9.
Engleman HM, Kingshott RN, Martin SE, Douglas NJ. Cognitive function in the sleep apnea/hypopnea syndrome (SAHS). Sleep. 2000;23(Suppl 4):S102–8.
Jean-Louis G, Zizi F, Clark LT, Brown CD, McFarlane SI. Obstructive sleep apnea and cardiovascular disease: role of the metabolic syndrome and its components. J Clin Sleep Med. 2008;4(3):261–72.
King S, Cuellar N. Obstructive sleep apnea as an independent stroke risk factor: a review of the evidence, stroke prevention guidelines, and implications for neuroscience nursing practice. J Neurosci Nurs. 2016;48(3):133–42.
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–41.
Connor J, Whitlock G, Norton R, Jackson R. The role of driver sleepiness in car crashes: a systematic review of epidemiological studies. Accid Anal Prev. 2001;33(1):31–41.
Lindberg E, Gislason T. Epidemiology of sleep-related obstructive breathing. Sleep Med Rev. 2000;4(5):411–33.
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–21.
Penzel T, Möller M, Becker HF, Knaack L, Peter JH. Effect of sleep position and sleep stage on the collapsibility of the upper airways in patients with sleep apnea. Sleep. 2001;24(1):90–5.
Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F, Kushida CA, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10(2):215–27.
Hedner J, Zou D. Drug therapy in obstructive sleep apnea. Sleep Med Clin. 2018;13(2):203–17.
Kent D, Stanley J, Aurora RN, Levine C, Gottlieb DJ, Spann MD, et al. Referral of adults with obstructive sleep apnea for surgical consultation: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021;17(12):2499–505.
Carvalho B, Hsia J, Capasso R. Surgical therapy of obstructive sleep apnea: a review. Neurotherapeutics. 2012;9(4):710–6.
Qaseem A, Holty JE, Owens DK, Dallas P, Starkey M, Shekelle P. Management of obstructive sleep apnea in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2013;159(7):471–83.
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2019;15(2):301–34.
Genta PR, Kaminska M, Edwards BA, Ebben MR, Krieger AC, Tamisier R, et al. The importance of mask selection on continuous positive airway pressure outcomes for obstructive sleep apnea. An Official American Thoracic Society workshop report. Ann Am Thorac Soc. 2020;17(10):1177–85.
Labarca G, Saavedra D, Dreyse J, Jorquera J, Barbe F. Efficacy of CPAP for improvements in sleepiness, cognition, mood, and quality of life in elderly patients with OSA: Systematic review and meta-analysis of randomized controlled trials. Chest. 2020;158(2):751–64.
Engleman HM, Martin SE, Kingshott RN, Mackay TW, Deary IJ, Douglas NJ. Randomised placebo controlled trial of daytime function after continuous positive airway pressure (CPAP) therapy for the sleep apnoea/hypopnoea syndrome. Thorax. 1998;53(5):341–5.
Montserrat JM, Ferrer M, Hernandez L, Farré R, Vilagut G, Navajas D, et al. Effectiveness of CPAP treatment in daytime function in sleep apnea syndrome: a randomized controlled study with an optimized placebo. Am J Respir Crit Care Med. 2001;164(4):608–13.
Monasterio C, Vidal S, Duran J, Ferrer M, Carmona C, Barbé F, et al. Effectiveness of continuous positive airway pressure in mild sleep apnea-hypopnea syndrome. Am J Respir Crit Care Med. 2001;164(6):939–43.
Durán-Cantolla J, Aizpuru F, Martínez-Null C, Barbé-Illa F. Obstructive sleep apnea/hypopnea and systemic hypertension. Sleep Med Rev. 2009;13(5):323–31.
Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, Mullins R, Jenkinson C, Stradling JR, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet. 2002;359(9302):204–10.
Becker HF, Jerrentrup A, Ploch T, Grote L, Penzel T, Sullivan CE, et al. Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation. 2003;107(1):68–73.
Cuhadaroğlu C, Utkusavaş A, Oztürk L, Salman S, Ece T. Effects of nasal CPAP treatment on insulin resistance, lipid profile, and plasma leptin in sleep apnea. Lung. 2009;187(2):75–81.
Comondore VR, Cheema R, Fox J, Butt A, John Mancini GB, Fleetham JA, et al. The impact of CPAP on cardiovascular biomarkers in minimally symptomatic patients with obstructive sleep apnea: a pilot feasibility randomized crossover trial. Lung. 2009;187(1):17–22.
Labarca G, Reyes T, Jorquera J, Dreyse J, Drake L. CPAP in patients with obstructive sleep apnea and type 2 diabetes mellitus: systematic review and meta-analysis. Clin Respir J. 2018;12(8):2361–8.
Giles TL, Lasserson TJ, Smith BJ, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006(1):Cd001106.
Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30(6):711–9.
Bratton DJ, Gaisl T, Wons AM, Kohler M. CPAP vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea: a systematic review and meta-analysis. JAMA. 2015;314(21):2280–93.
Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32(4):545–52.
Yang MC, Lin CY, Lan CC, Huang CY, Huang YC, Lim CS, et al. Factors affecting CPAP acceptance in elderly patients with obstructive sleep apnea in Taiwan. Respir Care. 2013;58(9):1504–13.
Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147(4):887–95.
Cistulli PA, Armitstead J, Pepin JL, Woehrle H, Nunez CM, Benjafield A, et al. Short-term CPAP adherence in obstructive sleep apnea: a big data analysis using real world data. Sleep Med. 2019;59:114–6.
Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–8.
Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45(1):43.
Krieger J, Kurtz D, Petiau C, Sforza E, Trautmann D. Long-term compliance with CPAP therapy in obstructive sleep apnea patients and in snorers. Sleep. 1996;19(9 Suppl):S136–43.
McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999;159(4 Pt 1):1108–14.
Pelletier-Fleury N, Rakotonanahary D, Fleury B. The age and other factors in the evaluation of compliance with nasal continuous positive airway pressure for obstructive sleep apnea syndrome. A Cox’s proportional hazard analysis. Sleep Med. 2001;2(3):225–32.
Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430–5.
Kohler M, Smith D, Tippett V, Stradling JR. Predictors of long-term compliance with continuous positive airway pressure. Thorax. 2010;65(9):829–32.
Campos-Rodriguez F, Martinez-Alonso M, Sanchez-de-la-Torre M, Barbe F. Long-term adherence to continuous positive airway pressure therapy in non-sleepy sleep apnea patients. Sleep Med. 2016;17:1–6.
Jacobsen AR, Eriksen F, Hansen RW, Erlandsen M, Thorup L, Damgård MB, et al. Determinants for adherence to continuous positive airway pressure therapy in obstructive sleep apnea. PLoS ONE. 2017;12(12): e0189614.
Mehrtash M, Bakker JP, Ayas N. Predictors of continuous positive airway pressure adherence in patients with obstructive sleep apnea. Lung. 2019;197(2):115–21.
Van Ryswyk E, Anderson CS, Antic NA, Barbe F, Bittencourt L, Freed R, et al. Predictors of long-term adherence to continuous positive airway pressure in patients with obstructive sleep apnea and cardiovascular disease. Sleep. 2019;42(10):zsz152.
Rauscher H, Popp W, Wanke T, Zwick H. Acceptance of CPAP therapy for sleep apnea. Chest. 1991;100(4):1019–23.
Florés M, Martinez-Alonso M, Sánchezde-la-Torre A, Aldomà A, Galera E, Barbé F, et al. Predictors of long-term adherence to continuous positive airway pressure in patients with obstructive sleep apnoea and acute coronary syndrome. J Thorac Dis. 2018;10(Suppl 1):S124–34.
Salas C, Dreyse J, Contreras A, Nazar G, Astorquiza C, Cabezon R, et al. Differences in patients derived from otolaryngology and other specialties with sleep apnea. J Otolaryngol Head Neck Surg. 2019;48(1):53.
Olsen S, Smith S, Oei T, Douglas J. Health belief model predicts adherence to CPAP before experience with CPAP. Eur Respir J. 2008;32(3):710–7.
Wild MR, Engleman HM, Douglas NJ, Espie CA. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004;24(3):461–5.
Gulati A, Stephens EM, Cai Y, Chang JL. Characterizing decisional conflict in patients presenting to sleep surgery clinic and an exploration of resource limitations. Laryngoscope. 2021;131(10):2384–90.
Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):Cd001431.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Drs. Lin and Wu had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. CSW: concept and design, statistical analysis, drafting of the manuscript. DHKC: drafting of the manuscript. YK: drafting of the manuscript. CHB: statistical analysis. PYC: administrative, technical, and material support. WTL: administrative, technical, and material support. YCL: concept and design, statistical analysis, acquisition, analysis, or interpretation of data, drafting of the manuscript, administrative, technical, and material support. All authors approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Taipei Medical University (IRB Number: N202201092, 2022/4/14 of approval).
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Baseline Data for Study Participants Referred by Non-Surgeons.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, CS., Chen, D.HK., Ko, YC. et al. The firstly visited department affects the acceptance of CPAP in patients with obstructive sleep apnea: a cohort study. J of Otolaryngol - Head & Neck Surg 52, 71 (2023). https://doi.org/10.1186/s40463-023-00676-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40463-023-00676-z