Abstract
Purpose
To determine the predictive factors of initial and long-term adherence to positive airway pressure (PAP) therapy and factors leading to an unfavorable shift of PAP compliance.
Methods
This follow-up study was comprised of newly diagnosed patients with obstructive sleep apnea (OSA) amenable to PAP therapy from January 2017 to April 2019. Information on basic demographics, comorbidities, and sleep-related symptoms were collected. PAP adherence data were collected at the end of the first week and the third month.
Results
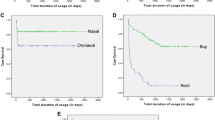
Of 166 patients enrolled, data from 142 (86%) were in the final analysis. Overall PAP usage was worse at 3 months declining from the first week. After adjusting for age and gender, multinomial logistic regression analysis showed that a small number of sleep-related symptoms (OR, 0.69; 95% CI, 0.52–0.91) and low arousal threshold (ArTH) (OR, 4.44; 95% CI, 1.52–12.98) were associated with higher odds of noncompliance. Low ArTH (OR, 2.87; 95% CI, 1.09–7.57) and lower body mass index (BMI) (OR, 0.88; 95% CI, 0.78–0.99) increased the risk of compliance-to-noncompliance shift. Sixty-two patients with polysomnography were analyzed separately. After adjustment for age and gender, poor sleep efficiency (OR, 0.80; 95% CI, 0.68–0.94) was associated with higher odds of consistent noncompliance. Low ArTH (OR, 15.36; 95% CI, 1.44–164.24) increased the risk of compliance-to-noncompliance shift in this subgroup.
Conclusions
Lower BMI and low ArTH were associated with an unfavorable shift of PAP compliance over time in patients with OSA, which was different from the predictors of consistent PAP noncompliance of patients with OSA.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip M, Morrell MJ et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7:687–698
Gottlieb DJ, Punjabi NM (2020) Diagnosis and management of obstructive sleep apnea: a review. JAMA. 323:1389–1400
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med 15:335–343
Streatfeild J, Hillman D, Adams R, Mitchell S, Pezzullo L (2019) Cost-effectiveness of continuous positive airway pressure therapy for obstructive sleep apnea: health care system and societal perspectives. SLEEP. 42
Nilius G, Schroeder M, Domanski U, Tietze A, Schafer T, Franke KJ. Telemedicine improves continuous positive airway pressure adherence in stroke patients with obstructive sleep apnea in a randomized trial. Respiration. 20191-11.
Ishak A, Ramsay M, Hart N, Steier J (2019) BPAP is an effective second-line therapy for obese patients with OSA failing regular CPAP: a prospective observational cohort study. Respirology.
Boyer L, Philippe C, Covali-Noroc A, Dalloz MA, Rouvel-Tallec A, Maillard D, Stoica M, d'Ortho MP (2019) OSA treatment with CPAP: randomized crossover study comparing tolerance and efficacy with and without humidification by ThermoSmart. Clin Respir J 13:384–390
Li Y, Huang X, Su J (2019) Wang Y. Mindfulness may be a novel factor associated with CPAP adherence in OSAHS patients, SLEEP BREATH
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 15:335–343
Kushida CA, Nichols DA, Holmes TH, Quan SF, Walsh JK, Gottlieb DJ, Simon RD Jr, Guilleminault C, White DP, Goodwin JL, Schweitzer PK, Leary EB, Hyde PR, Hirshkowitz M, Green S, McEvoy LK, Chan C, Gevins A, Kay GG, Bloch DA, Crabtree T, Dement WC (2012) Effects of continuous positive airway pressure on neurocognitive function in obstructive sleep apnea patients: the apnea positive pressure long-term efficacy Study (APPLES). SLEEP. 35:1593–1602
Mehrtash M, Bakker JP, Ayas N (2019) Predictors of continuous positive airway pressure adherence in patients with obstructive sleep apnea. LUNG. 197:115–121
Crawford MR, Espie CA, Bartlett DJ, Grunstein RR (2014) Integrating psychology and medicine in CPAP adherence--new concepts? Sleep Med Rev 18:123–139
Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea - new pathways for targeted therapy. Sleep Med Rev 37:45–59
Edwards BA, Eckert DJ, McSharry DG, Sands SA, Desai A, Kehlmann G et al (2014) Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am J Respir Crit Care Med 190:1293–1300
Zinchuk A, Edwards BA, Jeon S, Koo BB, Concato J, Sands S, Wellman A, Yaggi HK (2018) Prevalence, associated clinical features, and impact on continuous positive airway pressure use of a low respiratory arousal threshold among male United States veterans with obstructive sleep apnea. J Clin Sleep Med 14:809–817
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guidelin. J Clin Sleep Med 13:479–504
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 15:301–334
Flores M, Martinez-Alonso M, Sanchezde-la-Torre A, Aldoma A, Galera E, Barbe F et al (2018) Predictors of long-term adherence to continuous positive airway pressure in patients with obstructive sleep apnoea and acute coronary syndrome. J Thorac Dis 10:S124–S134
Campos-Rodriguez F, Martinez-Alonso M, Sanchez-de-la-Torre M, Barbe F (2016) Long-term adherence to continuous positive airway pressure therapy in non-sleepy sleep apnea patients. Sleep Med 17:1–6
Gagnadoux F, Le Vaillant M, Paris A, Pigeanne T, Chollet S, Masson P et al (2013) Adherence to positive airway pressure in non-sleepy patients with obstructive sleep apnoea. Eur Respir J 42:863–866
Van Ryswyk E, Anderson CS, Antic NA, Barbe F, Bittencourt L, Freed R et al (2019) Predictors of long-term adherence to continuous positive airway pressure in patients with obstructive sleep apnea and cardiovascular disease. SLEEP. 42
Gentina T, Bailly S, Jounieaux F, Verkindre C, Broussier PM, Guffroy D, Prigent A, Gres JJ, Kabbani J, Kedziora L, Tamisier R, Gentina E, Pépin JL (2019) Marital quality, partner’s engagement and continuous positive airway pressure adherence in obstructive sleep apnea. Sleep Med 55:56–61
Eckert DJ, Younes MK (2014) Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol (1985) 116:302–313
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014
Gray EL, McKenzie DK, Eckert DJ (2017) Obstructive sleep apnea without obesity is common and difficult to treat: evidence for a distinct pathophysiological phenotype. J Clin Sleep Med 13:81–88
Panossian LA, Veasey SC (2012) Daytime sleepiness in obesity: mechanisms beyond obstructive sleep apnea--a review. SLEEP. 35:605–615
Somiah M, Taxin Z, Keating J, Mooney AM, Norman RG, Rapoport DM, Ayappa I (2012) Sleep quality, short-term and long-term CPAP adherence. J Clin Sleep Med 8:489–500
Drake CL, Day R, Hudgel D, Stefadu Y, Parks M, Syron ML, Roth T (2003) Sleep during titration predicts continuous positive airway pressure compliance. SLEEP. 26:308–311
Lettieri CJ, Collen JF, Eliasson AH, Quast TM (2009) Sedative use during continuous positive airway pressure titration improves subsequent compliance: a randomized, double-blind, placebo-controlled trial. CHEST. 136:1263–1268
Stepnowsky CJ, Dimsdale JE (2002) Dose-response relationship between CPAP compliance and measures of sleep apnea severity. Sleep Med 3:329–334
Lettieri CJ, Shah AA, Holley AB, Kelly WF, Chang AS, Roop SA (2009) Effects of a short course of eszopiclone on continuous positive airway pressure adherence: a randomized trial. Ann Intern Med 151:696–702
Acknowledgements
We thank Dr. Q. Chen and C.Y. Ma for subject follow-up work. Stanley Yung-Chuan Liu, M.D., from the division of Sleep Surgery, Dept. of Otolaryngology-Head & Neck Surgery, at Stanford University School of Medicine, provided useful comments.
Funding
This study was financially supported by NSFC (Project 81870335) and Capital’s Funds for Health Improvement and Research (CFH-2020-4-1055).
Author information
Authors and Affiliations
Contributions
WH and WY performed the study design and experiment operation, and were major contributors in writing the manuscript. WC and ZX performed the study design and data collection. FF analyzed and interpreted the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of Beijing An Zhen Hospital and was registered in the Chinese Clinical Trial Register (ChiCTR-ROC-17011027).
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 23 kb)
Rights and permissions
About this article
Cite this article
Wu, H., Fang, F., Wu, C. et al. Low arousal threshold is associated with unfavorable shift of PAP compliance over time in patients with OSA . Sleep Breath 25, 887–895 (2021). https://doi.org/10.1007/s11325-020-02197-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02197-9