Abstract
Background
Lithium has long been considered the gold-standard pharmacological treatment for the maintenance treatment of bipolar disorders (BD) which is supported by a wide body of evidence. Prior research has shown a steady decline in lithium prescriptions during the last two decades. We aim to identify potential factors explaining this decline across the world with an anonymous worldwide survey developed by the International Society for Bipolar Disorders (ISBD) Task Force “Role of Lithium in Bipolar Disorders” and distributed by diverse academic and professional international channels.
Results
A total of 886 responses were received of which 606 completed the entire questionnaire while 206 completed it partially. Respondents were from 43 different countries comprising all continents. Lithium was the most preferred treatment option for the maintenance of BD patients (59%). The most relevant clinical circumstances in which lithium was the preferred option were in patients with BD I (53%), a family history of response (18%), and a prior response during acute treatment (17%). In contrast, Lithium was not the preferred option in case of patients´ negative beliefs and/or attitudes towards lithium (13%), acute side-effects or tolerability problems (10%) and intoxication risk (8%). Clinicians were less likely to prefer lithium as a first option in BD maintenance phase when practising in developing economy countries [X2 (1, N = 430) = 9465, p = 0.002) ] and private sectors [X2 (1, N = 434) = 8191, p = 0.004)].
Conclusions
Clinicians’ preferences and attitudes towards the use of lithium in the maintenance treatment of bipolar disorders appear to be affected by both the patients’ beliefs and the professional contexts where clinicians provide their services. More research involving patients is needed for identifying their attitudes toward lithium and factors affecting its use, particularly in developing economies.
Similar content being viewed by others
Background
Lithium has long been considered a key and gold-standard pharmacological treatment for mood disorders. Its cost-effectiveness in the long-term treatment of mood disorders, and especially in bipolar disorders (BD), has been supported by numerous randomized clinical trials, observational studies and meta-analyses (Burgess et al. 2001; Smith and Cipriani 2017). Its use as a first-line treatment option during maintenance phase of BD is widely supported by most international guidelines (Kessing 2019a; Malhi et al. 2017). A renewed interest in the academic field has also highlighted lithium as the only pharmacological compound in mood disorders with antisuicidal properties in recent decades (Smith and Cipriani 2017). More recently, even potential neuroprotective as well as antiviral effects were proposed when used in lower doses than those recommended in BD maintenance treatment (i.e., 0.60–0.80 mmol/L) (Dell’Osso et al. 2016; Murru et al. 2020; Nolen et al. 2019; Won and Kim 2017).
Despite lithium’s obvious advantages and the long experience of clinicians prescribing it, it is generally assumed it requires more initial and regular assessments and tests (i.e. ECG, blood plasma levels, renal and thyroid-parathyroid function tests) compared to other mood stabilizers (Nolen et al. 2019). In addition, there is still conflicting evidence regarding the long-term effects of its use on the kidneys (Nielsen et al. 2018; Schoretsanitis et al. 2022). Nevertheless, it is not clear whether the aforementioned reasons have contributed to the steady decline in lithium prescriptions in mood disorders in several countries and regions during the last two decades (Karanti et al. 2016; Rhee et al. 2020; Young and Hammond 2007). Given its many benefits in comparison to its inconveniences, this reduction in the use of lithium is especially worrisome considering the current lack of better pharmacological with similar properties in BD (Fountoulakis et al. 2022; Nestsiarovich et al. 2022; Young and Hammond 2007).
Considering this context, the Lithium Task Force (TF) of the International Society of Bipolar Disorders (ISBD) in collaboration with the International Group for the Study of Lithium-Treated Patients (IGSLI)-has launched a series of initiatives to explore the reasons and potential problems that could be influencing the prescription of lithium around the world while also work on recommendations about its appropriate use and monitoring (Grillault Laroche et al. 2020; Nolen et al. 2019; Shulman et al. 2019). Among these initiatives, it was decided that an anonymous worldwide survey collecting clinicians’ lithium prescription patterns and preferences could provide useful data regarding potential obstacles concerning the use of lithium in the maintenance treatment of bipolar disorders according to its scientific evidence. Identifying factors will allow the TF to plan more specific initiatives and actions to address potential issues influencing lithium prescription worldwide.
Methodology
In order to accomplish our aim, a first set of initial questions based on theliterature and previous studies (Pérez de Mendiola et al. 2021; Strejilevich et al. 2011) were outlined (DHM, TM, AY). This first draft was distributed to international members of the TF (WN, MB, ES,AG, EV) to incorporate all potential local and general preferences, issues, alongside limitations in Lithium prescription. After three iterative rounds, a final version of the questionnaire with 29 items was agreed upon (Additional file 1), which was subsequently formatted and uploaded to the Hospital Clínic of Barcelona survey platform (https://enquesta.clinic.cat/). Following a one-week internal technical and consistency check, the link to the survey was distributed among the mailing list of the ISBD and IGSLI members as well as several other professional organizations around the world involved in the care of people with BD and further distributed by diverse academic and professional international channels. The mail also requested colleagues and members to re-distribute the invitation within their local institutions as well as regional and national professional associations. The link to the survey was also announced in strictly closed professional groups on social networks (i.e., Facebook and LinkedIn). After accessing the survey, a protective CAPTCHA challenge-response test was set to prevent automatic responses followed by a brief introduction about the survey’s aims and specific questions used conditional logic to avoid redundant questions (e.g., If lithium was not available to prescribe in the country where the clinician provided services, further questions about lithium prescription were omitted). Data collected was stored in encrypted servers only accessible to the researchers at Hospital Clínic of Barcelona. No direct (e.g. name, ID, date or place of birth, exact age, etc.) or indirect (e.g. IP address, cookies tracking) personally identifiable information was collected by the website to ensure a fully anonymous survey.
Initial access to the survey was planned for 1 year, starting in August 2020. However, an additional 3-month extension to November 2021 was agreed upon among the TF due to the circumstances arising from the COVID-19 pandemic during the survey distribution period.
We conducted descriptive analyses to depict the respondents’ sociodemographic and professional characteristics. As no mandatory response to any specific question was requested, this resulted in a variable number of responses for each item. Hence, each question was analyzed independently to characterize the sample. Within groups´ percentages were computed to make associations and inferences between variables of interest. Chi-square tests were conducted to determine specific differences (i.e., sex, age, years practising, sector, context and country providing services) of those respondents preferring to use lithium as a first treatment option. Countries´ economic category were determined by the last edition (April 2022) of International Monetary Fund (IMF) (International Monetary Fund IMF 2022). Lithium monitoring standards were adopted from the last recommendations of the ISBD/IGSLI Lithium Task Force (Nolen et al. 2019). Statistical significance was established at p < .05. The data collected were analyzed using SPSS version 28 (SPSS Inc., Chicago, IL). For reporting purposes, we rounded up percentages if the next decimal was six or above, and down if it was five or less.
Results
A total of 886 responses were received of which 606 completed the whole questionnaire while 206 completed it partially (below 50% of all questions). There were no mandatory questions, but surveys completing less than 20% of the questions were omitted from the analyses for comparative reasons (N = 68). Respondents were from 43 different countries from 5 continents, with most responses received from Argentina (14%), France (12%), Netherlands (11%), Italy (10%), Germany (9%), Spain (8%), United States (6%), Chile (5%), Brazil (4%), Canada (3%), Australia (2%), United Kingdom (2%), Mexico (1%) and Denmark (1%). Thirty per cent of the responses corresponded to clinicians from 20 different developing economies with most respondents from SouthAmerica (35%), Asia (30%) and Africa (15%). Seventy-five per cent of the clinicians were not affiliated with major mood disorders international societies distributing directly or indirectly the survey [i.e., ISBD, IGSLI, International Society for Affective Disorders (ISAD)].
The majority of the respondents were male (55%) with a large predominance of psychiatrists among them (83%) while 11% were trainees and 5% were general practitioners. There was an equivalent distribution of age range with most respondents between 25 and 35 (25%), 36–45 (26%), 46–55 (21%) and 56–65 (18%) years old. Most of them had between 6 and 15 years of practice (30%) followed by those between 16 and 34 years (28%). The setting where they provided their services was mostly public (72%) and to a lesser extent the private sector (27%). 37% of the clinicians reported having between 11 and 25% of bipolar patients in their caseload while 23% had between 26% and 50% and twenty% less than 10%. Other sociodemographic and professional characteristics are detailed in Table 1.
Regarding the prescription of lithium, half of the respondents reported using lithium in more than 50% of their bipolar patients as maintenance treatment while 16% to over 75% of them. 44% prescribe it with a frequency of administration of twice a day for immediate-release and 57% with a frequency of once per day for extended-release formulas.
Lithium salts were the most preferred first treatment option for the maintenance treatment of BD patients (74%), followed by antipsychotics (12%) and valproate (7%). Figure 1 shows first and second treatment choice percentage distributions. Table 2 details group percentage differences among variables of interest in which lithium was the preferred first option. Most of the respondents started lithium right afterthe first manic or hypomanic episode (46%) with a lesser extent prescribing it after the second episode regardless of if it is manic or depressive (13%). The 5 most relevant clinical circumstances in which lithiumwas the preferred option during the maintenance phase were in patients with bipolar I disorder (53%), a family history of response to lithium (18%), a response to lithium during the acute treatment (17%), there were current or previous suicidal thoughts or attempts (15%) and when there was a specific predominant polarity (9%).
First and second choice of pharmacological treatment in the maintenance phase of BD. The bar chart shows the percentage distribution of first and second choice of pharmacological treatments in the maintenance phase of BD according to participants´ responses. In each bar section, actual number of responses for each option are displayed
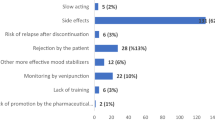
In contrast, the most common reasons in which lithium was not the preferred option were patients’ negative beliefs and/or attitudes towards lithium (13%), acute side-effects or tolerability problems (10%), intoxication risk (8%), medical comorbidities (6%) and long-term side-effects or safety issues (metabolic, thyroid or renal dysfunction) (6%). Figure 2 shows further reasons answered by respondents in which lithium was a preferred or not preferred option for the maintenance treatment of BD. In this context, professionals prescribing lithium were more concerned with the following long-term side effects: renal function alteration (55%), hypothyroidism (29%) and weight-gain (18%).
With regard to lithium levels tests and assessments during maintenance treatment, most of the respondents ordered them routinely between 2 and 4 times per year (73%), with most of them targeting plasma levels between 0.6 and 0.8 mmol/L (52%), 0.8–1 mmol/L (14.4%) or any level between 0.6 and 1.2 mmol/L (5%). The most common additional laboratory tests routinely performed in these controls alongside lithium plasma levels were renal (78%) and thyroid (78%) functions, and electrolytes (59%), with serum calcium tests requested only by 38% of the respondents. A minority also ordered an ECG (6%) and a thyroid gland ultrasound (3%). Importantly, weight and Body mass index (BMI) were assessed frequently during routine controls by 52% of the participants. Overall, 73% of the participants responded that they included all recommended tests (i.e. BMI, lithium plasma levels, electrolytes, renal and thyroid function and calcium). About half of the surveyed responded that they followed a guideline or protocol for systematically monitoring levels, but only a quarter of them used a standardized instrument to evaluate response to the treatment.
Considering variables of interest, a Chi-square test was conducted to explore whether professionals’ characteristics were related to the preference to use lithium as the first option in the maintenance treatment of BD. Two variables of interest showed a statistically significant relationship between those preferring lithium as a first option: clinicians were less likely to prefer lithium as a first option in BD maintenance phase when practising in developing economy countries [X2 (1, N = 430) = 9465, p = 0.002) and private sectors (X2 (1, N = 434) = 8191, p = 0.004)]. Considering these differences, we further conducted analyses to explore if differences in these variables were also translated to recommended lithium monitoring frequency (i.e. 2 or more per year) and lithium plasma levels (i.e. 0.4–1 mmol/L) during maintenance phases. No statistically significant differences were found in these parameters between developing economies or practising in the private sector.
Discussion
With this survey, we aimed to capture attitudes toward the use of lithium in the maintenance treatment of BD, and we involved a significant sample of diverse mental health professionals from different regions around the world. Respondents´ personal and professional characteristics reflected in the survey results confirm this diversity. This allows us to extract some generalizable conclusions while also identifying some specific patterns influencing the preference to prescribe lithium upon which actions can be taken.
In general, our results indicating that clinicians use lithium in more than 50% of their BD patients as maintenance treatment are in line with previous reports and registries from diverse countries (Lin et al. 2022; Mandal et al. 2019; Pacciardi et al. 2017; Pérez de Mendiola et al. 2021; Sköld et al. 2021). However, there is a striking diversity of prescriptions patterns among different countries (Kessing 2019b), with some countries and regions having lithium prescription patterns below 50% (Grover et al. 2021; Heeren et al. 2011; Karanti et al. 2016; Lyall et al. 2019) or above (Bohlken et al. 2020; Pérez de Mendiola et al. 2021). Based on our results and due to the lack of similar precedent worldwide survey, it is difficult to confirm or not a general decline in lithium prescriptions as it has been previously reported by studies based on data from national registries. However, recently Reed et al. analyzed 20-yeard prescriptions trends in the treatment of BD from systematic national surveys to clinicians in United Stated and found a decrease in use of lithium from 30.4% to 1997 to 17.6% in 2016 (Rhee et al. 2020). The much higher percentage of lithium prescription in our sample in comparison to the results by Rhee et al. might be explained by the specific regional and health system particularities of where the survey was conducted (i.e., United States) as well as the systematic random sampling of the surveyed clinicians in comparison to our anonymous convenience sample from professional associations. Nonetheless, it can be inferred from our results that clinicians around the world have a common preference, training, and monitoring standards for lithium, including trainees, but external factors might play a role in their decision to prescribe it.
Despite the participants’ heterogeneity, it can be assumed from the general preferences and attitudes reported in the survey, that lithium use and monitoring levels generally adhere to international guidelines. Though it is one of the oldest psychopharmacological compounds, the lack of a uniform consensus among health professionals regarding its use and monitoring is still concerning (Malhi et al. 2017). Disparities in the most appropriate maintenance plasma levels and monitoring frequencies, as well as needed tests, have been continuously reported within institutions and countries around the world (Janet A Butler 2009; Nederlof et al. 2018; Nikolova et al. 2018; Paton et al. 2010; Sköld et al. 2021).
The lower preference for lithium among developing nations and the private sector is noteworthy. In the case of lithium underutilization in developing countries, there is a lack of previous studies to compare with. Moreover, there in our sample there is imbalance between developing and developed economies in which the former has significant underrepresented regions (i.e. Caribbean, Central America). Even though clinicians’ false beliefs, misconceptions and lack of training might play a role, it is also reasonable to suggest that the lack of resources allowing appropriate monitoring makes lithium a less attractive choice in comparison to those not requiring periodic monitoring and testing. Other factors that may play a role are geographical and transportation barriers to access periodic controls due to unequal distribution of health care centers and sociocultural and religious beliefs and stigma held by local communities (Muhorakeye and Biracyaza 2021; Rathod et al. 2017). Aside from the lack of infrastructure, even if they are available, test costs might also play a role in the decision to prescribe lithium in countries with limited universal healthcare (Andrade et al. 2014). The same costs-associated reasons could explain the lower preference for lithium prescription among mental health professionals from private sectors where patients need to pay the price of required tests out-of-pocket. In both cases, the lack of systematic registries and data about the actual use of lithium represents a barrier difficult to overcome in order to extract firm conclusions (Williams and Boren 2008). Nonetheless, it must be emphasized that despite the involved test costs in the use of lithium its final cost-effectiveness in both developed and developing countries is still superior to valproic acid and antipsychotics (Chisholm et al. 2005). In addition, the mhGAP Intervention Guide of the World Health Organization (WHO) reinforces this recommendation (World Health Organization, WHO 2016).
In contrast with previous surveys, we found that the most common reason for not prescribing lithium was based on the patient’s perspective, instead of the mental health care professional’s concerns about side effects. These results may reflect a growing number of negative beliefs or attitudes about lithium salts in the general population and the rapid dissemination of the misconceptions through social media (Kessing 2019a; Malhi et al. 2020). This is not a specific issue about either lithium or psychiatry as a discipline, but a new extended problem throughout the health care sector (Chou et al. 2018; Khullar 2022). In the case of lithium, these misconceptions might be also prompted in part by false beliefs about the availability of more modern, effective, and tolerable compounds such as second-generation antipsychotics (SGA) which are also approved for the maintenance of BD (Jauhar and Young 2019; Malhi et al. 2020). SGAs are generally supported by a robust marketing plan from pharmaceutical companies (Malhi et al. 2009; Young and Hammond 2007). However, no SGA has performed as well as lithium in so many crucial long-term prognosis factors of BD as lithium (Lindström et al. 2017; Selle et al. 2014). While SGAs do not require so much baseline or therapeutic monitoring, metabolic syndrome, drowsiness, sexual dysfunction, and extrapyramidal effects are much more frequent in comparison to lithium (Miura et al. 2014).
Hence, our results stress the increasing need for mental health institutions and scientific societies to counter these false beliefs with more educational and promotional campaigns about lithium targeting the general population (Bauer 2022; Chou et al. 2018; Rybakowski 2022). Likewise, closer collaboration with patients´ associations could help further explore and understand their perspectives and beliefs about lithium (Gomes et al. 2022; Jørgensen and Rendtorff 2018). The move toward a more shared-decision-making (SDM) psychiatry could also represent another interesting approach to mitigate this belief as it allows time and space to build a structuredand informed decision-making process where doubts, fears and facts can be openly discussed between patients and clinicians. It has been proposed an SDM approach can improve patient satisfaction and medication adherence in recurrent mood disorders (Samalin et al. 2018a) with several studies still ongoing to confirm this hypothesis in BD (Samalin et al. 2018b).
This research has several limitations that must be taken into account to interpret these results. First, as in all anonymous survey-based studies, the information provided by respondents is a subjective, partial and non-quantitative perspective of the topics explored. Anonymous responses make it possible to obtain more honest answers without respondents feeling judged or tested. However, most of the results at least concerning lithium prescription are in line with studies using national registries. Secondly, the possibility of a sampling bias was compensated by using all possible survey distribution channels to reach colleagues around the world the TF members, including social networks. This was reflected in the diverse, although imbalanced, representation of almost all regions around the world of the respondents. However, given the limited sample size and some underrepresented regions, results cannot be generalizable across all countries. A further frequent issue is that online surveys distributed by national and international scientific associations and academic institutions do not reach sectors such as private practices. Colleagues associated with these associations are frequently more exposed to training programs, conferences and guidelines which constantly update them on the use of lithium (Pérez de Mendiola et al. 2021). Nonetheless, 75% of colleagues were not affiliated at all with major international mood disorder societies, and almost 28% provided their services in the private sector. Thus, we consider the survey distribution strategy was successful at reaching a representative sample of real-world clinicians, most of them not affiliated to the mood disorders societies. Finally, it is important to stress that as a survey primarily designed and announced with the aim of exploring the use of lithium in the maintenance of BD. Hence, clinicians who don’t see a substantial role for lithium for this indication might be less inclined to take part in the survey in comparison to those who feel strongly positively about it.
Conclusion
Overall, this study highlights the heterogeneous patterns of lithium prescription around the world. These patterns appear to be affected by both the patients’ beliefs and the professional context and region in which the clinicians operate, despite the strength of the evidence-base in favor of lithium and its safety (Carvalho et al. 2021; Gomes-da-Costa et al. 2022). More research involving patients is needed for identifying their attitudes toward lithium. There is also a need for more objective data in developing economies to determine and sort out factors influencing the use of lithium.
Availability of data and materials
The dataset used in this study is available upon reasonable request from researchers of academic institutions to the ISBD/IGSLI Task Force on treatment with lithium.
Abbreviations
- BD:
-
Bipolar disorder
- BMI:
-
Body mass index
- ISBD:
-
International society of bipolar disorders
- IGSLI:
-
International group for the study of lithium-treated patients
- TF:
-
Task force
References
Andrade LH, Alonso J, Mneimneh Z, Wells JE, Al-Hamzawi A, Borges G, et al. Barriers to mental health treatment: results from the WHO World Mental Health surveys. Psychol Med. 2014;44(6):1303–17.
Bauer M. Lithium: What can we do to overcome the discrepancies between evidence,guideline recommendations and clinical practice? Eur Neuropsychopharmacol. 2022;60:1–3.
Bohlken J, Bauer M, Kostev K. Drug treatment for patients with bipolar disorders in psychiatric practices in Germany in 2009 and 2018. Psychiatry Res. 2020;289:112965.
Burgess SS, Geddes J, Hawton KK, Taylor MJ, Townsend E, Jamison K, et al. Lithium for maintenance treatment of mood disorders. Cochrane Database Syst Rev. 2001. https://doi.org/10.1002/14651858.CD003013.
Carvalho AF, Solmi M, Husain MI, Berk M, Vieta E. The rebirth of lithium as the archetypal mood stabilizer. Bipolar Disord. 2021;23(2):211–2.
Chisholm D, Van Ommeren M, Ayuso-Mateos JL, Saxena S. Cost-effectiveness of clinical interventions for reducing the global burden of bipolar disorder. Br J Psychiatry. z2005;187(6):559–67.
Chou WYS, Oh A, Klein WMP. Addressing health-related misinformation on social media. JAMA. 2018;320(23):2417–8.
de Pérez X, Hidalgo-Mazzei D, Vieta E, González-Pinto A. Overview of lithium’s use: a nationwide survey. Int J Bipolar Disord. 2021;9(1):1–8.
Dell’Osso L, del Grande C, Gesi C, Carmassi C, Musetti L. A new look at an old drug: neuroprotective effects and therapeutic potentials of lithium salts. Neuropsychiatr Dis Treat. 2016;12:1687.
Fountoulakis KN, Tohen M, Zarate CA. Lithium treatment of Bipolar disorder in adults: a systematic review of randomized trials and meta-analyses. Eur Neuropsychopharmacol. 2022;54:100.
Gomes FA, Brietzke E, Bauer M, Post RM. A call for improving lithium literacy among clinicians and patients. Int J Bipolar Disord. 2022;10(1):1–2.
Gomes-da-Costa S, Marx W, Corponi F, Anmella G, Murru A, Pons-Cabrera MT, et al. Lithium therapy and weight change in people with bipolar disorder: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2022;134:104266.
Grillault Laroche D, Etain B, Severus E, Scott J, Bellivier F. Socio-demographic and clinical predictors of outcome to long-term treatment with lithium in bipolar disorders: a systematic review of the contemporary literature and recommendations from the ISBD/IGSLI task force on treatment with lithium. Int J Bipolar Disord. 2020;8(1):1–13.
Grover S, Avasthi A, Chakravarty R, Dan A, Chakraborty K, Neogi R, et al. Prescription patterns in clinically stable patients with bipolar disorder: findings from the bipolar disorder course and outcome from India (BiD-CoIN) study. Asian J Psychiatr. 2021;57:102549.
Heeren O, Sánchez De Carmona M, Vásquez G, Córdoba R, Forero J, Madrid L, et al. Psychopharmacological treatment of bipolar disorder in Latin American. Revista de Psiquiatría y Salud Mental. 2011. https://doi.org/10.1016/j.rpsmen.2011.08.001.
International Monetary Fund (IMF). World economic and financial surveys world economic outlook database—WEO groups and aggregates information. 2022.
Janet A, Butler DT. A survey of lithium monitoring and prescribing patterns. Int J Psychiatry Clin Pract. 2009;4(2):135–8.
Jauhar S, Young AH. Controversies in bipolar disorder; role of second-generation antipsychotic for maintenance therapy. Int J Bipolar Disord. 2019;7(1):10.
Jørgensen K, Rendtorff JD. Patient participation in mental health care–perspectives of healthcare professionals: an integrative review. Scand J Caring Sci. 2018;32(2):490–501.
Karanti A, Kardell M, Lundberg U, Landén M. Changes in mood stabilizer prescription patterns in bipolar disorder. J Affect Disord. 2016;195:50–6.
Kessing LV. Lithium as the drug of choice for maintenance treatment in bipolar disorder. Acta Psychiatr Scand. 2019;140(2):91–3.
Kessing LV. Lithium as the drug of choice for maintenance treatment in bipolar disorder. Acta Psychiatr Scand. 2019;140(2):91–3.
Khullar D. Social media and medical misinformation. JAMA. 2022;328(14):1393–4.
Lin SK, Yang SY, Park SC, Jang OJ, Zhu X, Xiang YT, et al. Prescription patterns for bipolar disorder in Asian Countries: findings from research on asian prescription pattern-bipolar disorder. Clin Psychopharmacol Neurosci. 2022;28(1):61–9.
Lindström L, Lindström E, Nilsson M, Höistad M. Maintenance therapy with second generation antipsychotics for bipolar disorder—a systematic review and meta-analysis. J Affect Disord. 2017;213:138–50.
Lyall LM, Penades N, Smith DJ. Changes in prescribing for bipolar disorder between 2009 and 2016: national-level data linkage study in Scotland. Br J Psychiatry. 2019;215(1):415–21.
Malhi GS, Adams D, Berk M. Is lithium in a class of its own? A Brief Profile of Its Clinical Use. 2009. https://doi.org/10.3109/00048670903279937.
Malhi GS, Bell E, Boyce P, Hazell P, Murray G, Bassett D, et al. Make lithium great again! Bipolar Disord. 2020;22(4):325–7.
Malhi GS, Gessler D, Outhred T. The use of lithium for the treatment of bipolar disorder: recommendations from clinical practice guidelines. J Affect Disord. 2017;217:266–80.
Mandal S, Mamidipalli S, Mukherjee B, Hara S. Perspectives, attitude, and practice of lithium prescription among psychiatrists in India. Indian J Psychiatry. 2019;61(5):451.
Miura T, Noma H, Furukawa TA, Mitsuyasu H, Tanaka S, Stockton S, et al. Comparative efficacy and tolerability of pharmacological treatments in the maintenance treatment of bipolar disorder: a systematic review and network meta-analysis. Lancet Psychiatry. 2014;1(1):351–9.
Muhorakeye O, Biracyaza E. Exploring barriers to mental health services utilization at kabutare district hospital of Rwanda: perspectives from patients. Front Psychol. 2021;12:638377.
Murru A, Manchia M, Hajek T, Nielsen RE, Rybakowski JK, Sani G, et al. Lithium’s antiviral effects: a potential drug for CoViD-19 disease? Int J Bipolar Disord. 2020;8(1):19.
Nederlof M, Heerdink ER, Egberts ACG, Wilting I, Stoker LJ, Hoekstra R, et al.Monitoring of patients treated with lithium for bipolar disorder: an international survey. Int J Bipolar Disord. 2018;6(1):1–9.
Nestsiarovich A, Gaudiot CES, Baldessarini RJ, Vieta E, Zhu Y, Tohen M. Preventing new episodes of bipolar disorder in adults: systematic review and meta-analysis of randomized controlled trials. Eur Neuropsychopharmacol. 2022;54:75–89.
Nielsen R, Kessing L, Nolen W, Licht R. Lithium and renal impairment: a review on a still hot topic. Pharmacopsychiatry. 2018;51(05):200–5.
Nikolova VL, Pattanaseri K, Hidalgo-Mazzei D, Taylor D, Young AH. Is lithium monitoring NICE? Lithium monit UK secondary care sett. 2018. https://doi.org/10.1177/0269881118760663.
Nolen WA, Licht RW, Young AH, Malhi GS, Tohen M, Vieta E, et al. What is the optimal serum level for lithium in the maintenance treatment of bipolar disorder? A systematic review and recommendations from the ISBD/IGSLI task force on treatment with lithium. Bipolar Disord. 2019;21(5):394–409.
Pacciardi B, Palagini L, Mainardi C, Cotugno B, Cargioli C, Perugi G, et al. Attitude toward prescription and clinical monitoring of lithium salts in a sample of Italian psychiatrists: preliminary data. Off J Ital Soc Psychopathol. 2017;23:172–9.
Paton C, Barnes TRE, Shingleton-Smith A, McAllister-Williams HR, Kirkbride J, Jones PB, et al. Lithium in bipolar and other affective disorders: prescribing practice in the UK. J Psychopharmacol. 2010;24(12):1739–46.
Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low- and middle-income countries. Health Serv Insights. 2017. https://doi.org/10.1177/1178632917694350.
Rhee TG, Olfson M, Nierenberg AA, Wilkinson ST. 20-years Trends in the pharmacologic treatment of bipolar disorder by psychiatrists in outpatient care settings. Am J Psychiatry. 2020;177(8):706.
Rybakowski JK. Lithium. Eur Neuropsychopharmacol. 2022;57:86–7.
Samalin L, Genty JB, Boyer L, Lopez-Castroman J, Abbar M, Llorca PM. Shared decision-making: a systematic review focusing on mood disorders. Curr Psychiatry Rep. 2018;20:1–1.
Samalin L, Honciuc M, Boyer L, de Chazeron I, Blanc O, Abbar M, et al. Efficacy of shared decision-making on treatment adherence of patients with bipolar disorder: a cluster randomized trial (ShareD-BD). BMC Psychiatry. 2018;18(1):1.
Schoretsanitis G, de Filippis R, Brady BM, Homan P, Suppes T, Kane JM. Prevalence of impaired kidney function in patients with long-term lithium treatment: a systematic review and meta-analysis. Bipolar Disord. 2022;24(3):264–74.
Selle V, Schalkwijk S, Vázquez GH, Baldessarini RJ. Treatments for acute bipolar depression: meta-analyses of placebo-controlled, monotherapy trials of anticonvulsants, lithium and antipsychotics. Pharmacopsychiatry. 2014;47(2):43–52.
Shulman KI, Almeida OP, Herrmann N, Schaffer A, Strejilevich SA, Paternoster C, et al. Delphi survey of maintenance lithium treatment in older adults with bipolar disorder: an ISBD task force report. Bipolar Disord. 2019;21(2):117–23.
Sköld M, Rolstad S, Joas E, Kardell M, Pålsson E, Goodwin GM, et al. Regional lithium prescription rates and recurrence in bipolar disorder. Int J Bipolar Disord. 2021;9(1):1–9.
Smith KA, Cipriani A. Lithium and suicide in mood disorders: updated meta-review of the scientific literature. Bipolar Disord. 2017;19(7):575–86.
Strejilevich SA, Urtueta-Baamonde M, Teitelbaum J, Martino DJ, Marengo E, Igoa A, et al. Clinical concepts associated with lithium underutilization in the treatment of bipolar disorder. Vertex. 2011;22:3–20.
Williams F, Boren SA. The role of the electronic medical record (EMR) in care delivery development in developing countries: a systematic review. Inf Prim Care. 2008;16(2):139–45.
Won E, Kim YK. An oldie but goodie: lithium in the treatment of bipolar disorder through neuroprotective and neurotrophic mechanisms. Int J Mol Sci. 2017;18(12):2679.
World Health Organization (WHO). mhGAP intervention guide for mental, neurological and substance use disorders in nonspecialized health settings: mental health gap action programme (mhGAP). 2016.
Young AH, Hammond JM. Lithium in mood disorders: increasing evidence base, declining use?. Br J Psychiatry. 2007;191(6):474–6.
Acknowledgements
The authors would like to thank all participants who completed the survey for this study. We want to express our gratitude for their help in the distribution of the link survey to Mary Miller and Chad Daversa from the International Society for Bipolar Disorders (ISBD) as well as to all representatives of local, regional, national and international professional associations. Allan H. Young’s independent research is funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. Eduard Vieta thanks the support of the Spanish Ministry of Science, Innovation and Universities (PI15/00283, PI18/00805, PI19/00394, PI21/00787, CPII19/00009) integrated into the Plan Nacional de I + D + I and co-financed by the Instituto de Salud Carlos III (ISCIII)-Subdirección General de Evaluación and the Fondo Europeo de Desarrollo Regional (FEDER); the ISCIII; the CIBER of Mental Health (CIBERSAM); the Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2017 SGR 1365), and the CERCA Programme / Generalitat de Catalunya. We would like to thank the Departament de Salut de la Generalitat de Catalunya for the PERIS Grant SLT006/17/00357. Diego Hidalgo-Mazzei´s research is supported by a Juan Rodés JR18/00021 granted by the Instituto de Salud Carlos III (ISCIII). Juan Undurraga is supported by ANID-PIA-ACT192064, and ANID-FONDECYT 1180358, 1200601.
Funding
This study was supported and conducted by resources already available of the Institutions involved as well as the International Society for Bipolar Disorders (ISBD).
Author information
Authors and Affiliations
Contributions
DHM, TM, XP, AG, AY and SS developed the initial surveys which were subsequently merged to generate the first draft of the survey circulated among TF members. WN, MB, ES, SS, AG, AY and EV reviewed and improved this first initial version in an iterative process which led to the final version of the survey. LS, JU and SS actively collaborated in distributing the survey in their countries and regions. DHM administered the survey platform, analyzed the data collected and drafted the first version of this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided electronic approval to participate in the study prior to completing the anonymous survey. Ethical review and approval were waived for this study as it did not involve any patients or animals but just medical professionals responding an anonymized survey.
Consent for publication
All authors contributed to and approved the final manuscript giving their consent for publication.
Competing interests
Diego Hidalgo-Mazzei has received CME-related honoraria and served as consultant for Abbott, Angelini, Ethypharm Digital Therapy and Janssen-Cilag with no financial or other relationship relevant to the subject of this article. Ludovic Samalin has received CME-related honoraria and served as consultant for Janssen-Cilag, Lundbeck, Otsuka, Sanofi-Aventis with no financial or other relationship relevant to the subject of this article. Juan Undurraga has served as a consultant for Johnson & Johnson. Michael Bauer has received research grants by the Deutsche Forschungsgemeinschaft (DFG), Bundesministerium für Bildung und Forschung (BMBF), Gemeinsamer Bundesausschuss- Innovationsausschuss, European Commission, Sächsisches Staatsministerium für Wissenschaft, Kultur und Tourismus (SMWK) and served as consultant, adviser or speaker for Biogen, Janssen-Cilag, GH Research, Livanova Deutschland GmbH, Novartis, Sunovion, Takeda, neuraxpharm, Shire International GmbH, Aristo, Servier Deutschland GmbH and Hexal AG. Allan H. Young has received honoraria for lectures and advisory boards for all major pharmaceutical companies with drugs used in affective and related disorders with no financial or other relationship relevant to the subject of this article.Eduard Vieta has received research support from or served as consultant, adviser or speaker for AB-Biotics, Abbott, Abbvie, Adamed, Angelini, Biogen, Celon, Dainippon Sumitomo Pharma, Ferrer, Gedeon Richter, GH Research, Glaxo SimthKline, Janssen, Lundbeck, Organon, Otsuka, Rovi, Sage pharmaceuticals, Sanofi-Aventis, Shire, Sunovion, Takeda, and Viatris, out of the submitted work. The other authors do not report any financial or other relationship relevant to the subject of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The supplementary file contains the complete survey answered by the participantsof the study about psychiatrists’ personal concepts, opinions and experiences on the clinical use of lithium in the maintenance treatment of bipolar disorders. For each survey section, the question, instructions to respond, and count of the responses to each possible answer are shown.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hidalgo-Mazzei, D., Mantingh, T., Pérez de Mendiola, X. et al. Clinicians’ preferences and attitudes towards the use of lithium in the maintenance treatment of bipolar disorders around the world: a survey from the ISBD Lithium task force. Int J Bipolar Disord 11, 20 (2023). https://doi.org/10.1186/s40345-023-00301-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40345-023-00301-y